Abstract
This chapter reports on the prevalence of social anxiety disorder (SAD) and social fears in Western and non-Western countries, onset and course characteristics, mental and physical comorbidities, as well as risk factor constellations based on findings from clinical and population-based samples in children, adolescents, and adults. SAD represents one of the most common mental disorders: About one-fifth of the population reports unreasonably strong social fears, ranging from pervasive shyness to more or less isolated social fears; another 13 % of the population meets the diagnostic criteria for social anxiety disorder at some point in their life. Childhood and adolescence have emerged as developmentally sensitive time windows for first onset, with considerable persistence but also substantial fluctuations in symptom severity around the diagnostic threshold up to adulthood. Remission is rare, posing affected youth at risk for secondary complications such as depressive and substance use disorders and somatic conditions. Risk factors that have been implicated in the development of SAD include deficits in social skills and negative peer status, as well as family-related factors such as parental psychopathology, heritability estimates and temperament, anxiogenic parenting, and transmission of interpretation bias. Future studies may benefit from such a family-oriented perspective to depict the divergent developmental sequence, to provide a comprehensive model in promoting epidemiological understanding of SAD, and to delineate targeted prevention and early interventions.
Contribution upon request for Ranta, K., La Greca, A. M., Garcia-Lopez, L.-J., Marttunen, M., (eds). Social Anxiety and Phobia in Adolescents: Development, Manifestation and Intervention Strategies. Springer.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Prevalence of Social Anxiety Disorder and Social Fears in Western and Non-Western Countries
Social anxiety includes a spectrum of phenomena that may range from shyness to more or less isolated social fears up to the clinically relevant diagnostic prototype of SAD, sometimes also extending to avoidant or anxious personality disorder. Social fears may occur in only one or two situations but may also be more pervasive in a wider range of situations. They include performance fears such as fear of public speaking or speaking in front of others or taking tests and fears of being observed by others while writing in public, reading aloud, or eating and/or drinking in public. Other social fears relate to social interactions such as initiating and/or maintaining a conversation, talking to or dealing with others, using public restrooms, or going to (social) activities or participating in social events (APA 2000, 2013).
Social Anxiety Disorder (SAD)
Social anxiety disorder (SAD) or social phobia is the most frequent anxiety disorder and the second most common of all DSM-IV disorders (Kessler et al. 2005b). Rates are higher in adults as compared to adolescents and children, but as implicated in the studies shown here, the differences between adults and adolescents are at least in part explained by methodological artifacts and the remaining differences are small.
About 13 % of the population meet the diagnostic criteria for SAD at some point in their life (Beesdo et al. 2007; Kessler et al. 1994), and mean lifetime prevalence is estimated at 6.7 % in European (Fehm et al. 2005) and up to 12.1 % in US samples (NCS-R; Kessler et al. 2005a). Twelve-month prevalence rates for SAD range from 0.4 (Neufeld et al. 1999) to 6.8 % (Chavira et al. 2004). Prevalence estimates generally vary across studies due to sampling and assessment strategies (screening tools or self-report measurements vs. standardized or structured interviews, please see Chap. 6), applied diagnostic criteria (DSM vs. ICD), or culture-bound forms of social anxiety such as taijin kyofusho (Kleinknecht et al. 1997) or hikikomori (Nagata et al. 2013). Lifetime rates range between 15.3 and 32.4 % in clinical samples (Last et al. 1992; Lépine et al. 1993; Zhang et al. 2004) and between 2.5 and 24.0 % in community samples (Fehm et al. 2005).
There is a lack of comparable studies in children and adolescents in non-Western countries, specifically East-Asian regions. However, studies among East-Asian adults have yielded lower SAD estimates ranging between 0.5 and 1.2 % according to DSM or ICD (Hwu et al. 1989; Tsuchiya et al. 2009; Kleinknecht et al. 1997; Lee et al. 2009). Of note, culture-specific forms of social anxiety are typically more frequent in the respective culture than DSM-defined social anxiety (Dinnel et al. 2002; Vriends et al. 2013; Lee et al. 2006). Hence, ethnic differences on self-reported social anxiety are likely attenuated when assessments consider views of the self that are typically associated with Western cultures (Hong and Woody 2007; Heinrichs et al. 2006; Essau et al. 2012) and when culture-specific assessment formats and evaluations of impairment are used (Hsu and Alden 2007). Lifetime prevalence estimates in childhood and adolescence are somewhat lower than for adults in Europe and the United States, where rates are up to 10 % (Merikangas et al. 2011; Beesdo et al. 2007; Feehan et al. 1994). Again, reported rates are higher in adolescents than in children and higher in girls than in boys. For example, the overall rate for SAD was 3.9 % in Turkish children and adolescents; 1.8 and 3.5 % for boys and girls aged 9 to 10 years, respectively; and 3.2 and 6.4 % for boys and girls aged 11–13 years (Demir et al. 2013). In Finnish adolescents aged 12–17 years who were drawn from the general population, the 12-month prevalence was 3.2 % for SAD with a further 4.6 % with subclinical SAD (Ranta et al. 2009b). Finally, the prevalence has been found to be 5.5 % in Spanish adolescents (13–18 years) and 5.8 % (12–18-year-old) who were also drawn from the general population (Garcia-Lopez et al. 2014; Garcia-Lopez 2015b, respectively).
Social Fears
The most common social fear both in adolescents and in adults is fear of public speaking (Stein et al. 1994; Faravelli et al. 2000; Magee et al. 1996; Kessler et al. 1994). However, isolated or pure social fears occur rarely, as the majority report at least one other social fear (Kessler et al. 1998; Wittchen et al. 1999b). For the recently introduced specifier for DSM-5 social anxiety disorder, namely, “performance only,” reliable prevalence estimates are still rare (Garcia-Lopez et al. 2015a, 2015b; Kerns et al. 2013). Unreasonably strong social fears were found in 22.3 % of male and in 32.2 % of female adolescents and young adults aged 14–24 years (Wittchen et al. 1999b). Similarly, at least one-fifth of adults reported unreasonable strong social fears (Fehm et al. 2008). In a community sample of adolescents and young adults, 20.0, 11.6, and 11.7 % of respondents reported fear of one, two, three or more social situations, respectively, and among individuals with DSM-IV SAD, rates were 24.2, 18.7, and 57.1 % (Knappe et al. 2011). Among Spanish adolescents, the highest anxiety-provoking social situation was speaking in public (11 %), followed by being observed by others (9.7 %), being in an embarrassing situation (9.3 %), and being rejected (9 %) (Garcia-Lopez et al. 2008).
Further, a substantial proportion of adolescents and young adults reported social fears that may not necessarily meet the criteria for the diagnostic threshold of SAD: 23.1 % reported symptomatic SAD, i.e., positively affirmed a diagnostic stem question for “ever having a persistent, irrational fear of, and compelling desire to avoid a situation in which the respondent attended social affairs, like going to a party or meeting,” and another 18.4 % met all but one diagnostic criteria for SAD according to the DSM-IV (Knappe et al. 2009a). Of note, the direct and indirect economic and individual costs associated with SAD are substantial, and those of subthreshold SAD approach those of the full-threshold disorder (Acaturk et al. 2009).
Onset, Natural Course, and Persistence
Onset
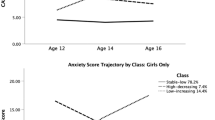
Retrospective reports of clinical populations have located the age of SAD onset in late adolescence and adulthood (Keller 2006; Wittchen and Fehm 2001), likely reflecting the point in life at which symptoms have led to severe impairment requiring treatment, after the disorder has been present for a considerable proportion of years. In contrast, prospective-longitudinal studies in youth preponed first onset of SAD toward childhood and adolescence between ages 10 and 16.6 years (Wittchen and Fehm 2001; Magee et al. 1996). Specifically, the core high-risk period spans from 9 years of age to the third decade of life (Beesdo et al. 2007). New onsets after the age of 20 are probably rare, though further peaks of incidence may not be strictly excluded. For clinicians, it is worth knowing that most adults with SAD fail to recall the first onset of SAD symptoms or to remember a time when SAD did not affect their daily life – probably because of the early onset in childhood and adolescence (Wittchen and Fehm 2001) (Figs 3.1 and 3.2).
Duration and Course Patterns
The mean duration of SAD symptoms ranges from 19 to 21 years in clinical studies and from 19 to 25 years in community studies (Fehm et al. 2008; Wittchen and Fehm 2001).
Little is however known about the natural course of SAD, and the majority of findings are based on adult samples. Studies are needed that cover the high-risk period for SAD onset as well as tracking subsequent chronification vs. alleviation of SAD symptoms. Prospective examinations in adult clinical samples and primary care patients indicate a chronic, i.e., long-lasting, course with enduring symptom load (Chartier et al. 1998; Beard et al. 2010). One small retrospective cross-sectional study of 39 socially anxious adults (Chartier et al. 1998) revealed four patterns of course: “worsening” (8 %), “stability” (33 %), “slight improvement” (21 %), and “remission” (38 %) of symptoms across an average illness duration of 29 years (± 2.7 years). Notably, all respondents reported to meet DSM-IV diagnostic criteria of SAD continuously during the course of the disorder, with the exception of the remission pattern, which was associated with a marked improvement of social anxiety, none or a minimal level of distress, lack of avoidance, and interference. Larger, predominantly community studies indicate, however, that meeting the disorder criteria continuously over long time periods is rare. Comparing the ratios of the 12-month to lifetime rate (90.9 %) with 30-day to 12-month prevalence rate of SAD (55.7 %) in the cross-sectional NCS-A, Kessler and colleagues concluded that persistence of SAD is better characterized by recurrences than by constant chronicity (Kessler et al. 2012). In accordance, prospective-longitudinal examinations have revealed considerable persistence of SAD, but also substantial fluctuations of symptom severity. In the 15-year prospective multi-wave Zurich Cohort Study (Angst and Vollrath 1991), no individual with SAD was diagnosed continuously at each follow-up assessment after the disorder had manifested (Merikangas et al. 2002). Thus, diagnostic stability of SAD is presumed to be low, consistent with findings that stability rates of threshold SAD (defined as meeting the full DSM-IV criteria again at a subsequent assessment) ranged between 7.1 and 15.1 % in a prospective-longitudinal study (Beesdo-Baum et al. 2012), depending on the assessment times that were considered and the follow-up periods. Rates increase to 56.7 % when also symptomatic and subthreshold SAD is taken into account. These stability rates for SAD may appear rather moderate, but SAD at each time point was associated with a considerably increased risk to also have the disorder or signs and symptoms of the disorder at later points in time, compared to the rates for those without SAD. In fact, a substantial proportion of SAD cases reported at least some significant SAD symptoms (21.5 %) or subthreshold SAD (19.7 %) at subsequent waves (Beesdo-Baum et al. 2012), indicating an oscillating course of SAD (i.e., waxing and waning) around the diagnostic threshold (Wittchen et al. 1999a). Stability of social anxiety symptomatology has been found to be moderate in adolescents after 6 months reassessment (Garcia-Lopez et al. 2008).
Remission, Recovery, and Relapse
Few studies have considered the natural course of SAD among young people, so available findings may lead to misinterpretations and underestimations of disorder severity. We have therefore first drawn on studies with adult populations, where more extensive data is available. Generally, the course of SAD in adults is considered to be less favorable in clinical than in primary care or community samples (27 % vs. 40 % recovery rate after 5 years) (Steinert et al. 2013). Between 45 and 56 % of patients who underwent routine treatment in outpatient care centers experienced at least partial remission from their symptoms over 6–8 years (Alnaes and Torgersen 1999; Keller 2003), while in the community this rate was 77 % after 3 years (Steinert et al. 2013). In a female community sample, 64 % of SAD cases were at least partially recovered, and 36 % showed full recovery 1.5 years later, i.e., no longer experienced any of the DSM-IV criteria of social phobia (Vriends et al. 2007). Roughly estimated, less than half of affected adults experience spontaneous remissions or full recovery (Sibrava et al. 2013; Keller 2006; Bruce et al. 2005; Alnaes and Torgersen 1999).
As noted, few studies have examined natural remission among children, adolescents, and young people with SAD. However, one study with a clinical population (many of whom received treatment) reported remission of SAD and other anxiety disorders in 80 % of children aged 5–18 years (Last et al. 1996), but 30 % of the cases reported another anxiety disorder 3–4 years later. In a community sample of adolescents and young adults, the rate of full remission of SAD was 15.1 % (Beesdo-Baum et al. 2012), that is, they revealed neither SAD symptoms nor other disorders across a time period of up to 10 years. Hence, even though the frequency or intensity of SAD symptoms may decrease over time, the risk for other mental problems (disorders) increases (Essau et al. 2002).
Mental and Physical Comorbidity
Comorbidity with Other Mental Disorders
Co-occurrence of other anxiety and mental disorders with SAD is frequent in adolescence and adulthood and is the rule rather than the exception (Wittchen and Fehm 2001). In general, comorbidity rates range from between about 69 and 99 % (Steinert et al. 2013; Schneier et al. 1992) depending on the study sample, setting, and assessments. The most frequent comorbid mental conditions in adolescents and adults are other anxiety disorders, depressive disorders, substance use, and somatoform disorders (Coles et al. 2006; Fu et al. 2007; Rogers et al. 1996; Beesdo-Baum and Knappe 2012), as well as personality disorders in adults (Massion et al. 2002; Lampe et al. 2003; Cox et al. 2009). Compared to non-SAD cases, an increased risk for suicidal ideation but not for suicide attempts was reported in both cross-sectional and longitudinal analyses of NEMESIS data drawn from adults (Sareen et al. 2005a).
Among the anxiety disorders, SAD most commonly co-occurs with specific phobias, agoraphobia, panic disorder, and generalized anxiety disorder (e.g., Alonso et al. 2004; Kessler et al. 2005b; Lampe et al. 2003; Merikangas et al. 2002). Prospective epidemiological studies indicate that children and adolescents meeting the criteria for SAD or any other anxiety disorder are at high risk for meeting the criteria for the same or comorbid disorders also in adulthood (Costello et al. 2003), and vice versa, adults with SAD or other anxiety disorders reported that the same or comorbid disorder was already present in childhood and adolescence (Gregory et al. 2007; Kim-Cohen et al. 2003; Rutter et al. 2006). Compared to unaffected individuals, higher rates of SAD have also been observed in adult patients with obsessive-compulsive disorders (e.g., Assuncao et al. 2012). Among individuals with anorexia nervosa, elevated rates for SAD were observed relative to those without anorexia, though findings are yet inconclusive (Godart et al. 2002; Swinbourne and Touyz 2007); lifetime and current prevalence rates for SAD in threshold or subsyndromal bulimia nervosa are significantly higher than in nonclinical controls (Godart et al. 2002).
Comorbidity with Physical Disorders
Elevated rates of SAD have also been found to be associated with physical problems, specifically sleep problems and insomnia (Stein et al. 1993; Johnson et al. 2006), diabetes, thyroid disease, lupus, or other autoimmune disease (Sareen et al. 2005b). Findings are however limited to adults. For adolescents, a history of early language impairment was associated with a greater likelihood to meet diagnostic criteria for DSM-IV SAD by the age of 19 years (Voci et al. 2006) (Table 3.1).
SAD as a Risk Factor for Incident Conditions
While acknowledging the variability in definitions and applied assessment methods, analyses of comorbidity can inform understanding of shared and non-shared risk factors for SAD and can help delineate hypotheses about underlying pathogenic mechanisms. The most basic assumptions about the co-occurrence (comorbidity) of mental and/or physical conditions are probably that co-occurrence is either at random or that two or more conditions overlap or even represent the same underlying clinical phenomenon. Comorbidity may also be due to the fact that one condition temporally precedes the other, potentially as a (causal) risk factor for the other condition. In this regard, SAD is presumed to serve as a risk factor for a cascade of secondary psychopathology. Because longitudinal data (starting in childhood or adolescence and with sufficient follow-up periods) are needed to resolve these questions, findings from studies in adolescents and young adults up to the third decade of life are presented. Therein, longitudinal studies have provided evidence for the role of SAD as a putative causal risk factor for depressive disorders (Beesdo et al. 2007; Stein et al. 2001b; Pine et al. 1998), substance use disorders (Buckner et al. 2006, 2008; Sonntag et al. 2000; Sareen et al. 2006; Zimmerman et al. 2004), and, in some studies, psychosis (Schutters et al. 2011; Rietdijk et al. 2013).
SAD as a Risk Factor for Substance Use
While depressive disorders may be considered a consequence of SAD, it is widely assumed that the consumption of alcohol or other substances as a form of coping or safety behavior bears the risk for alcohol-related problems (Schry and White 2013) and/or other substance use disorders. Consumption of alcohol or other substances prior or during social situations is expected to reduce self-perceived social anxiety but also to affect attentional processes such as preferential processing of external stimuli and physical symptoms such as facial blushing (Stevens et al. 2014). In addition, findings in college student samples point to the role of different drinking motives; that is, alcohol may be consumed in order to reduce social anxiety in situations where intake of alcohol is deemed socially acceptable but fear of cognitive performance deficits may also reduce the motivation for alcohol intake, particularly in performance-related situations (Cludius et al. 2013). Similar observations were made in relation to smoking and nicotine dependence and social anxiety; that is, socially anxious individuals, in particular females, who use cigarettes to cope with feelings of loneliness or social rejection may be particularly vulnerable to more severe nicotine dependence (Buckner and Vinci 2013). Here, the potential mediating role of depression also needs to be considered.
SAD as a Risk Factor for Psychosis
Research on early signs and prodromal states of psychosis in adolescents and young adults has pointed to SAD (Schutters et al. 2011) and social anxiety (Rietdijk et al. 2013) as a useful screener for paranoid symptoms in help-seeking individuals at high risk for psychosis. Again, the associations between SAD and psychosis may relate to shared and non-shared risk factors and to the temporal sequence of these two conditions.
Risk Factors for SAD Onset and Course
A range of correlates and putative risk factors for SAD conditions have been examined. The findings are sometimes unclear as studies focus on selected factors and use cross-sectional designs with diverging assessment strategies and outcome criteria. For descriptive purposes, we will consider factors relevant for SAD onset and SAD course.
Female Gender
Community samples have identified that females across all ages are about twice as often affected by SAD as males (Demir et al. 2013; DeWit et al. 2005; De Graaf et al. 2002; Merikangas et al. 2011; Ruscio et al. 2008; Wittchen et al. 1999b). In contrast, an equal gender distribution has been observed in clinical samples or even slightly higher rates for men (Fehm et al. 2005). This may be due to the difference in social expectations between genders that is still influential in many societies. Of note, though some studies on convenience samples have suggested differences in the prevalence of social fears between males and females, effect sizes were low (Garcia-Lopez et al. 2008) but appear to increase with advanced puberty (Deardoff et al. 2007).
In relation to the course of SAD, females report higher rates of comorbid anxiety and depressive disorders (MacKenzie and Fowler 2013), whereas males more often report comorbid externalizing disorders and substance use (Xu et al. 2012).
Peer Status and Social Skills
Mixed results have been found regarding the causal relationship of peer status and social skills on SAD. There is ample evidence that negative peer status during childhood and adolescence is linked with higher levels of social anxiety (Erath et al. 2008; La Greca et al. 1988; La Greca and Stone 1993; Ranta et al. 2009a; Rao et al. 2007; Siegel et al. 2009; Storch et al. 2005; Tillfors et al. 2012; Vernberg et al. 1992), and both adolescents and adults with SAD are more likely to report a history of peer victimization than their healthy counterparts or patients with other anxiety disorders (Gren-Landell et al. 2011; McCabe et al. 2003; Roth et al. 2002; Garcia-Lopez et al. 2011; Ranta et al. 2009a, 2013). However, some studies show that the variable with the largest impact in predicting prospective anxiety symptoms is the self-report of victimization and the reaction to these negative experiences (i.e., personal perceptions of the incident) (Bouman et al. 2012; Levinson et al. 2013). Since many existing studies rely on retrospective accounts and lack objective peer ratings, measurement issues need to be considered when comparing specific results.
The relationship between peer rejection and heightened social anxiety is likely to be bidirectional (Tillfors et al. 2012). Thus, children and adolescents with elevated social anxiety behave in a reserved way toward their peers, and their peers tend to evaluate these children negatively. Negative evaluation from others may then reinforce children’s fear of social situations, making the child more reluctant to interact with his or her peers (Rapee and Spence 2004).
Whether the reserved social behaviors shown by children with social anxiety reflect a lack of social skills is a matter of ongoing debate. Early studies by Spence and colleagues (Spence et al. 2000) and Beidel et al. (1999) showed that SAD is associated with not only lower subjective ratings of social skills but also lower observer ratings on behavioral measures. Many subsequent studies have replicated these findings in both clinical and nonclinical samples (Alfano et al. 2006; Beidel et al. 2014; Inderbitzen-Nolan et al. 2007; Morgan and Banerjee 2006) and thus have provided the basis for the application of social skills training in child and adolescent social anxiety intervention programs (e.g., Beidel et al. 2000; Spence et al. 2000). However, evaluating social skills in situations where children are anxious makes it difficult to ascertain whether group differences reflect social communication skill deficits or a lack of social confidence. For example, Cartwright-Hatton and colleagues (Cartwright-Hatton et al. 2003; Cartwright-Hatton et al. 2005) recruited a group of non-referred school children and assessed their performance in a speech/conversation task and found that, although more anxious children had more negative perceptions of their performance, micro-behaviors and global impression of the performance did not differ significantly between anxious and non-anxious children. The authors concluded that socially anxious children may benefit from cognitive interventions that focus on maladaptive beliefs about how they appear to others during social encounters.
One approach to teasing apart social skills deficits and a lack of social confidence is to consider the social communication difficulties that may underlie restricted social behaviors. For example, Banerjee and Henderson (2001) reported that community children with high levels of social anxiety were rated by teachers as being less skilled in social tasks that involved insight into others’ mental states, compared to their low-anxious peers. Consistent with this finding are recent reports that clinically referred children with anxiety disorders have inflated levels of traits of autistic spectrum disorders (van Steensel et al. 2013) and that this is particularly the case among children with SAD (Halls et al. 2014). Whether similar patterns are found among adolescents with social anxiety requires investigation given findings that adolescents show less impairment in behavioral measures of social skills than younger children (Rao et al. 2007).
Clearly, more research is needed to clarify the causal relationship between peer status, social skills, and SAD. However, existing evidence strongly suggests that interpersonal relationships during the adolescent years shape subjective image of the social self, and this image has a lasting impact which persists into adulthood. Social skills training on the part of the individual as well as classwide prevention and early intervention programs to change the environmental factors within the school may have a synergistic effect for both anxious and non-anxious adolescents. For example, reactions from classmates moderate anxious adolescents’ performance level in social tasks (Blöte et al. 2007), and children’s risk for peer difficulties is moderated by classroom emotional climate (Gazelle 2006; Avant et al. 2011).
Familial Load and Parental Psychopathology
Family and high-risk studies strongly indicate that SAD aggregates in families, that is, offspring are at increased risk for SAD when parents are affected themselves (Knappe et al. 2009c; Lieb et al. 2000; Bandelow et al. 2004; Elizabeth et al. 2006; Merikangas et al. 2003; Stein et al. 2001a). Associative family studies however do not provide information on the mechanisms of intergenerational transmission, i.e., whether, when, and to which degree genetic factors, environmental factors, or a combination thereof contribute to offspring SAD. The vast majority of literature has demonstrated that both gene and environmental influences and their interaction contribute to SAD.
Findings are mixed with regard to specificity of the parent-to-offspring transmission. The Reading longitudinal study recruited mothers during pregnancy on the basis of their meeting diagnostic criteria for SAD (n = 96), generalized anxiety disorder (n = 58), or having no history of an anxiety disorder (n = 94). At the most recent assessment (age 4–5 years), inflated levels of internalizing difficulties and SAD (15 %), specifically, were already apparent among the offspring of mothers with SAD compared to those with generalized anxiety disorder (2 %) and those with no history of anxiety disorder (0 %) (Murray et al. 2014). These findings are consistent with early diagnostic specificity in transmission, at least in the case of SAD.
However, epidemiological data with adolescent or adult populations indicate parental SAD, but also other parental anxiety, depressive, and alcohol use disorders confer risk to offspring SAD above and below the diagnostic threshold and to other offspring disorders as well (Knappe et al. 2009a, b; Lieb et al. 2000). Interestingly, SAD cases with isolated performance-related fears had substantially lower rates of parents with SAD or alcohol use disorders than SAD cases who reported fears in interaction or both interaction or performance-related social situations (Knappe et al. 2011). In addition, different risks for the development of social anxiety disorder may be associated with different developmental phases. For example, increased social fears have been documented among infant and toddler offspring of parents with social anxiety disorder (Murray et al. 2007, 2008; Akatr et al. 2014), indicating that infancy and early childhood are sensitive time windows for learning social fears through observation of parental behaviors.
Heritability and Candidate Genes
Heritability estimates specifically for SAD based on twin samples are modest, range from 0.20 to 0.50 across studies (Knappe et al. 2010), and are generally comparable across ages (McGrath et al. 2012). However, it has been suggested that men and women differ in the extent to which genetic and environmental factors contribute to SAD. Specifically, twin resemblance was best explained by (non-shared) family-environment factors in females and by (shared) genetic factors in males (Kendler et al. 2002). It is likely that there are common genetic risk factors underlying many of the childhood anxiety disorders and traits, although the magnitude of overlap differs depending on the age of the sample, measures used, and disorders or traits considered (for reviews cf. Gregory and Eley 2007; McGrath et al. 2012). For example, overlap in familial and non-shared environmental factors was observed between specific phobia and SAD (Eley et al. 2008). Particularly for SAD, there is some evidence for developmental dynamics; that is, genetic contributions to SAD in childhood are different from those in adolescence and adulthood, indicating only a limited degree of genetic continuity across time. Compared to other phobias, the genetic effects on SAD were observed to dramatically change in adolescence and young adulthood, when new and substantial genetic influences contributed to the course of SAD and the development of comorbid conditions (Kendler et al. 2008).
With regard to potential candidate genes, the focus has been on specific genes encoding components of serotonergic (5-HT) and dopaminergic pathways (Domschke et al. 2009; Gelernter et al. 2004) without notable results for SAD. Progress in this field is slow and limited given that multiple genes of small effect size are likely to contribute to SAD as well as to other anxiety-related conditions (Gregory and Eley 2007) and because of a range of methodological issues such as small or heterogeneous samples with broad age ranges, diverse comorbidity profiles, false-positive results that do not hold up for replication, and vague thresholds to differentiate between normative and pathological (social) anxiety conditions (McGrath et al. 2012). Similarly, genome-wide association studies (GWAS), including both linkage and association designs, have mostly focused on anxiety-related traits, the broader category of anxiety disorders in general, or predominantly panic disorder (for an overview, cf. McGrath et al. 2012; Domschke and Deckert 2012). Genetic polymorphisms are of further interest in understanding and predicting outcomes related to SAD treatment, though findings are not yet convincing (Andersson et al. 2013). For more details on genetics and heritability in SAD, refer to Tillfors et al. (2012), and Chap. 4 of this book.
Behavioral Inhibition and Other Temperamental and Personality Factors
A further potential mechanism underlying the familial and genetic factors that are associated with SAD is behavioral inhibition (BI). BI is a temperamental trait that has been consistently associated with an increased risk for SAD. Originally derived from laboratory-based direct observation, BI is defined as a chronic tendency to “show an initial avoidance of or behavioral restraint to novelty” (Kagan et al. 1988a). Behavioral signs of BI in children include “long latencies to interact with unfamiliar adults, retreat from unfamiliar objects, cessation of play and vocalization, and long periods remaining proximal to the mother” (Kagan et al. 1988b). In recent years, it has been shown that BI is a heritable trait that has a strong neurophysiological basis (DiLalla et al. 1994; Kagan et al. 1987; Matheny 1989; Robinson et al. 1992).
Early studies by Kagan et al. (1988a, b) found that children with extreme BI tendencies at age 2 showed stable social avoidance and withdrawal behavior at ages 4, 5.5, and 7.5. In diagnostic terms, a follow-up study of this same cohort at age 13 showed higher rates of SAD for children with BI (Schwartz et al. 1999). Similar results have been obtained using retrospective self-reports in SAD patients (Van Ameringen et al. 1998) and adolescents (Hayward et al. 1998). Results from a recent meta-analysis (Clauss and Blackford 2012) indicate that BI is associated with a greater than sevenfold increase in risk for developing SAD. This association remained significant after considering study differences in temperament assessment, control group, parental risk, age at temperament assessment, and age at anxiety diagnosis. Collectively, it is well established that BI has the strongest relationship with SAD above all other mental disorders.
There is an ongoing controversy regarding whether BI is a distinct construct from SAD. Some researchers regard BI on a quantitative continuum from shyness to SAD (e.g., McNeil 2001). However, for the most part, BI is conceptualized as a temperamental vulnerability that is linked to the later development of anxiety disorders. Cultural differences in the manifestation of BI (Chen et al. 1998) and interactions with parenting variables (e.g., Natsuaki et al. 2013) are some areas of future research that may clarify such distinctions.
Biological Factors
Central to adolescent development are hormonal changes associated with growth and puberty. As part of normative functional changes, morphological and neural maturations significantly impact on cognition and information processing (Haller et al. 2014; Blakemore 2008). The rapid increase of studies using structural and functional imaging procedures with special interest in limbic and prefrontal brain areas has contributed tremendously to our understanding of social anxiety and SAD, though most findings are based on young adult samples between ages 20 and 35. Structural data indicate enlarged amygdala and left hippocampal regions (Machado-de-Sousa et al. 2014), increased thickness of the left inferior temporal cortex, and reduced thickness of the right rostral anterior cingulate cortex (Frick et al. 2013) in socially anxious young adults relative to controls. Some of these brain areas are associated with dysfunctional regulation and processing of emotions in SAD which is further supported by functional imaging studies.
Functional imaging studies in SAD focus on face perception, social cue processing, and processing and inhibition of social threat stimuli as neural correlates for SAD-relevant cognitive distortions and bias (Anderson et al. 2013; Pejic et al. 2013; Gentili et al. 2009), as well as emotional hyperreactivity and ineffective emotion regulation. For example, Goldin and colleagues (Goldin et al. 2009) examined neural correlates of emotional reactivity and cognitive regulation during processing of harsh facial expressions (i.e., social threat) and violent scenes (physical threat) in 15 adults with SAD and matched unaffected controls. As a result, viewing social threat resulted in greater emotion-related neural responses and reduced cognitive and attention regulation-related neural activation in patients than controls, with social anxiety symptom severity related to activity in a network of emotion- and attention-processing regions only in patients (Goldin et al. 2009). For more details on the neurobiological factors, regions, and processes in SAD (see Chap. 4 ).
Family Environment
Given the early onset of SAD in childhood and adolescence, the strong familial aggregation, and the importance of the family for the social, emotional, and cognitive development of an individual, diverse family processes have been hypothesized to promote the onset or persistence or to affect the treatment of SAD (for a comprehensive overview, see Knappe et al. 2010), such as insecure attachment (Stevenson-Hinde and Shouldice 1990; Eng et al. 2001; van Brakel et al. 2006), higher levels of expressed emotion (Suveg et al. 2005; Garcia-Lopez et al. 2009, 2014), excessive family cohesion (Peleg-Popko and Dar 2001), and disturbed family functioning (Ballash et al. 2006; Bögels and Brechmann-Toussaint 2006; Tamplin and Goodyer 2001). It should be noted though that some of these concepts have been linked with anxiety disorders, but their specific association with social anxiety disorder has rarely been examined. An exception is Garcia-Lopez et al.’s (2009) study revealing that parental psychopathology (parents with high expressed emotion, EE) should be taken into consideration to prevent poor treatment outcomes for socially anxious adolescent. More recently, Garcia-Lopez et al. (2014) have found that the inclusion of parent training to reduce EE in a treatment program designed to address social anxiety in adolescents had a positive effect on their improvement, particularly when the parents’ EE status changed from high to low expressed emotion after treatment. In addition, different roles for maternal and paternal behavior in the development of child anxiety have been suggested (Bögels et al. 2011; Bögels and Perotti 2011; Teetsel et al. 2014), for example, that fathers’ parenting behavior may have a particularly important role in encouraging the child to playfully test limits, approach new situations, and actively cope with fears (Majdandzic et al. 2014), whereas maternal parenting behavior may be particularly critical for teaching social wariness (Bögels et al. 2011). Few studies to date have distinguished between maternal and paternal behaviors; however, this is clearly a priority for future research. In fact, awareness and investigations of the father’s role for SAD and other anxiety disorders in offspring are increasing (i.e., Majdandzic et al. 2014; Aktar et al. 2014; Bögels and Perotti 2011; Bögels and Phares 2008).
“Anxiogenic” Parenting
It is likely that parents who are anxious, depressed, or stressed display potentially anxiogenic parenting behaviors and that offspring with SAD elicit adverse parenting. Prospective evaluations are limited, but findings so far point to independent as well as accumulated contributions of parental psychopathology and parental rearing to offspring SAD.
Parenting styles and behaviors characterized by expressed anxiety, overcontrol, and low warmth have been implicated in the development and maintenance of childhood anxiety disorders (e.g., Murray et al. 2009), with most consistent support from both questionnaire and observational assessments of overcontrol (McLeod et al. 2007; Wood et al. 2003). It has been suggested that negative parenting behaviors may be particularly pertinent to the development of SAD, where sensitivity to negative evaluation from others is a core feature (Gulley et al. 2014). Results of a recent prospective study using observational methods have implicated parental overcontrol in the development of social anxiety symptoms and disorder, particularly among children with a stable history of high levels of behavioral inhibition (Lewis-Morrarty et al. 2012). However, few studies have examined associations between parental behaviors and SAD specifically (i.e., in contrast to other anxiety disorders). A notable exception is a prospective-longitudinal study in adolescents and young adults, in which offspring-reported dysfunctional parental rearing (rejection, overprotection, and lack of emotional warmth) was associated with offspring threshold SAD and, albeit less strong and less consistently, also with subthreshold SAD (Knappe et al. 2009a). Here, the constellation of higher paternal rejection and lower paternal (but not maternal) emotional warmth and higher maternal (but not paternal) overprotection was observed in offspring SAD but not in other offspring anxiety disorders, suggesting that there may be specificity in parenting factors associated with offspring SAD and that particular patterns of behaviors of mothers and fathers may have distinct functions (Knappe et al. 2012).
Whether parenting behaviors account for the intergenerational transmission of SAD has also received little empirical investigation. Notably, in the prospective-longitudinal study described above, associations between offspring-reported parenting behaviors and offspring SAD did not change after controlling for parental psychopathology and vice versa, suggesting that both risk factors may contribute independently to offspring SAD (Knappe et al. 2009a, c). However, offspring-reported parenting on questionnaire measures may be subject to biases and may not pick up on situationally specific parenting responses. Murray et al. (2012), for example, found that differences in parenting behaviors (specifically increased passivity and reduced encouragement and warmth) between mothers with SAD or GAD and non-anxious mothers were principally evident in the context of disorder-specific challenge. In line with these findings, parents with SAD have demonstrated less warmth and more criticism and doubts of child competency than parents with other anxiety disorders when observed with their child conducting two performance tasks, although notably no differences were found in parental overcontrol or autonomy granting (Budinger et al. 2013).
In addition to particular parental responses being more likely to occur in the context of parental anxiety, depression, or stress, child experiences and characteristics are likely to elicit particular parental responses. For example, natal complications have been found to relate to later overprotection and low emotional warmth, with a trend toward serious health problems predicting unfavorable parenting (Knappe et al. 2012). Furthermore, adverse experiences or particular child characteristics may provoke particular parenting styles more readily among more anxious parents. Consistent with this suggestion, Hirshfeld et al. (1997) found that maternal criticism of the child was a function of a significant interaction between child behavioral inhibition and maternal anxiety disorder status: Within the group of anxious mothers, 65 % of those with inhibited children were critical compared to 18 % of those with non-inhibited children. Similarly Murray et al. (2008) reported that mothers with SAD showed low levels of encouragement to their infants to engage with a stranger only when the infant was behaviorally inhibited. Together these findings highlight the likely complex reciprocal and interacting relationships between child and parent characteristics and behaviors.
Information Processing Biases
Biases in information processing have been emphasized in theories of the development and maintenance of anxiety disorders in both adults (Beck et al. 1985) and children (Kendall 1985) and in models of social anxiety disorder specifically (Clark and Wells 1995; Rapee and Heimberg 1997). Central to these theories are the hypotheses that anxiety is reinforced by a tendency to (1) selectively or preferentially respond to threat and (2) to interpret ambiguous information in a negative or threatening manner. However, Spence et al. (1999) suggested that negative expectancies about social situations may not be a key factor in the development of social anxiety in children, but may initially be a response to a lack of social success, which then later maintains anxiety by promoting avoidance of social situations. Findings to date have not yet been able to fully evaluate this possibility, although, in contrast, there is some evidence that infants at risk of SAD (by virtue of having a parent with SAD) differ from low-risk infants (with non-socially anxious parents) in their looking responses to emotional faces (Creswell et al. 2008) and that this is associated with later anxiety symptoms (Creswell et al. 2011). In a similar vein, compared to children of non-anxious mothers, 4 to 5-year-old children of mothers with SAD were significantly more likely to give negative responses to school-based scenarios presented in a doll-play format prior to the child starting school (Pass et al. 2012). Furthermore, negative doll play predicted teacher reported anxious-depressed and social worry problems at the end of the child’s first term at school. Despite these intriguing findings which might suggest a developmental role of information processing biases, cross-sectional studies that have examined associations between information processing biases and SAD in children have failed to deliver a clear pattern of results in relation to the maintenance of SAD.
Associations between attention biases and anxiety in children and adolescents have varied across studies, with some finding that anxiety is associated with attention toward threat (e.g., Roy et al. 2008) but others finding attention away from (or avoidance of) threat (e.g., Monk et al. 2006). Differences in findings may be explained by methodological and sample characteristics, for example, the specific anxiety disorder subtypes that make up the sample (Waters et al. 2014). Specific associations between social anxiety and attention bias in children and adolescents have received little attention; however, Stirling, Eley, and Clark (2006) reported that social anxiety symptoms (and not general anxiety symptoms) in a community population of 8–11-year-olds were significantly associated with a bias away from negative facial expressions. In contrast, Gulley, Oppenheim, and Hankin (2014) recently reported a bias toward angry faces among children (9–15 years) with higher symptoms of social anxiety in both a community and a psychiatrically enriched sample. Of particular note, the association between observed authoritarian and negative parenting and child social anxiety was mediated by attention to angry faces in the community sample. These cross-sectional findings provide preliminary support for the hypothesis that environmental factors (such as parenting) may present a risk for SAD by virtue of their influence on emerging information processing styles. These findings are fascinating, but the lack of consistency in reported results to date emphasizes the need for caution and further examination of the role of attentional biases in the development and maintenance of SAD in childhood and adolescence.
Although a number of studies have demonstrated that children with anxiety disorders interpret ambiguous situations in a more negative manner than non-anxious children (e.g., Barrett et al. 1996; Creswell et al. 2005), there has been little examination of disorder-specific associations. The studies that have considered this have provided inconsistent findings, with some finding no SAD-specific associations when compared to children with other anxiety disorders (Barrett et al. 1996) or non-anxious controls (Creswell et al. 2014), but with one recent study reporting higher fear and threat ratings in response to ambiguous situations in children with SAD compared to both other anxious and non-anxious children (Alkozei et al. 2014). These discrepancies may be accounted for by methodological and sample characteristics, and further clarification is required. In addition, little is known about the role of interpretation biases in SAD in adolescence. On the basis of Spence et al.’s (1999) proposal, prospective studies are clearly required that follow children into adolescence to examine the potentially changing association between interpretation biases, social functioning, and social anxiety over time.
Although studies with children and adolescents have focused predominantly on attention and interpretation biases, adult models of the maintenance of SAD emphasize other information processing biases, such as recall biases, self-focused attention, and the tendency to view anxiety symptoms as having negative consequences (e.g., Clark and Wells 1995; Rapee and Heimberg 1997). Accordingly, consideration of broader indices of information processing in relation to SAD is required with adolescent populations. One such recent example reported that adolescents with SAD were more likely to recall information that they had been instructed to forget than non-anxious children (Gómez-Ariza et al. 2013). These findings are consistent with the hypothesis that young people with SAD may be particularly likely to hold on to negative or unhelpful memories (e.g., relating to social failure), and that this may underlie negative expectancies when entering novel social situations.
Given the limited available evidence and lack of consistency found in relation to information processing biases and SAD in adolescents, replication of positive findings is required, as are prospective and experimental methods to establish the directional nature of associations at different stages in development.
Predictors for SAD Course and Persistence
In contrast to the substantial literature reporting on correlates and (risk) factors for SAD or SAD onset, data on risk factors for the (natural) course of SAD, (i.e., with regard to remission or persistence of SAD symptoms), are limited. Again, findings vary between retrospective and clinical studies and prospective samples with varying follow-up periods and whether SAD or anxiety disorders in general are examined as outcomes. Most studies are based on adult samples. Among distal factors, in a study of adolescents and young adults, presence of parental psychopathology was unrelated to persistence of offspring SAD, but higher levels of parental overprotection were associated with higher persistence of offspring SAD (Knappe et al. 2009c). Also cumulative effects were suggested; that is, lack of emotional warmth and disturbed family functioning predicted higher SAD persistence, particularly when parents were affected by a mental disorder themselves (Knappe et al. 2009c). Distal vulnerability characteristics such as parental SAD and depression, behavioral inhibition, and harm avoidance predicted SAD persistence and also, but less consistently, diagnostic stability of SAD (Beesdo-Baum et al. 2012).
Among proximal factors, clinical characteristics of onset patterns and early course are of interest (Noyes et al. 2005), with early age of onset (de Menezes et al. 2005; Lim et al. 2013; but see Crippa et al. 2007), degree of impairment (Davidson et al. 1994), or symptom severity (DeWit et al. 1999), as well as comorbid conditions (Yonkers et al. 2003; Massion et al. 2002), being associated with an unfavorable outcome. One study in young women did not find that SAD symptom severity or duration predicted recovery 1.5 years later (Vriends et al. 2007), while other studies with longer follow-up periods and including both genders reported that baseline severity (van Beljouw et al. 2010), a longer duration of SAD, comorbid panic disorder with agoraphobia, and lower psychosocial functioning predicted lower rates of recovery from SAD (Beard et al. 2010). Blanco et al. (2011) recorded treatment seeking in the past 12 months to predict an unfavorable course. In contrast, being employed, no lifetime depression, fewer than three lifetime psychiatric disorders, less anxiety sensitivity, and fewer daily hassles were associated with recovery from SAD (Vriends et al. 2007). In adolescents and young adults, predominantly clinical features in terms of early onset, generalized subtype, more anxiety cognitions, severe avoidance and impairment, and co-occurring panic attacks were associated with SAD persistence (Beesdo-Baum et al. 2012).
A Heuristic Framework for the Epidemiology of SAD
In parallel to a number of psychological models for SAD (Hughes et al. 2006; Clark and Wells 1995; Hoffman 2002; Christensen et al. 2003; Morrison and Heimberg 2013), clinical-epidemiological research focusing on natural course patterns as well as identification of correlates and risk factors and their interplay has stimulated a diathesis-stress model (vulnerability stress model) linking societal, biological, and psychological vulnerabilities with environmental stressors. This heuristic approach may help to delineate hypotheses about multiple factors relevant for the onset and course of SAD, as well as putative mechanisms and processes and their occurrence within sensitive developmental periods. In the past decade, a range of studies have provided findings in line with this approach (for a review, cf. Brook and Schmidt 2008). Childhood and adolescence have emerged as a sensitive time window for first SAD onset, though indicators and early signs for SAD may already be observed in infancy. The observed familial aggregation of SAD and the importance of the family and environment (in addition or combination with genetics) for the societal, emotional, and cognitive development of the offspring may denote a more family-oriented approach for targeted prevention and early intervention (Knappe et al. 2010; Elizabeth et al. 2006). However, dissection of the complex interplay of risk factors, correlates, and consequences is warranted to also understand underlying mechanisms and, more specifically, to identify moderators and mediators for SAD onset and course.
Summary and Conclusions
SAD is a debilitating condition that affects a large number of children and adolescents in both Western and non-Western countries. Most patients report an onset age of 20 years or younger, and symptoms tend to be persistent, although considerable fluctuations are seen over time. High co-occurrence is found with other mental problems, such as other anxiety disorders, depressive disorders, bulimia nervosa, substance use and somatoform disorders, and even psychosis. In addition, individuals with SAD are at increased risk for physical disorders, including insomnia, diabetes, and autoimmune diseases. In light of these facts, early intervention and prevention of SAD are a research imperative.
A wide range of risk factors have been identified to heighten incidence rates of SAD. Demographic variables include female gender and parental history of psychopathology. Low peer status and social skills and maladaptive familial environment and parenting are some typical psychological risk factors. Biological and physiological factors as represented by behavioral inhibition also play an important role in the manifestation and maintenance of symptoms. In recent years, cognitive factors such as information processing bias have received increased attention in relation to the etiology of SAD. These risk factors do not function independently, but rather constitute a complex interplay underpinning multiple trajectories to the onset of the disorder.
Current literature has come a long way since SAD was described as a “neglected anxiety disorder” (Liebowitz et al. 1985). However, information regarding temporal alteration and the longitudinal course of the disorder is very limited. Future studies may benefit from a family-oriented perspective to depict the divergent developmental sequence, to provide a comprehensive model in promoting epidemiological understanding of SAD, and to delineate targeted prevention and early interventions.
References
Acaturk C, Smit F, De Graaf R, van Straten A, Ten Have M, Cuijpers P (2009) Economic costs of social phobia: a population-based study. J Affect Disord 115:421–429
Aktar M, Majdandzic M, De Vente W, Bogels SM (2014) Parental social anxiety disorder prospectively predicts toddlers’ fear/avoidance in a social referencing paradigm. J Child Psychol Psychiatry 55:77–87
Alfano CA, Beidel DC, Turner SM (2006) Cognitive correlates of social phobia among children and adolescents. J Abnorm Child Psychol 34:189–201
Alkozei A, Cooper P, Creswell C (2014) Emotional reasoning and anxiety sensitivity: associations with social anxiety disorder in childhood. J Affect Disord 152–154:219–228
Alnaes R, Torgersen S (1999) A 6-year follow-up study of anxiety disorders in psychiatric outpatients: development and continuity with personality disorders and personality traits as predictors. Nord J Psychiatry 53:409–416
Alonso J, Angermeyer C, Bernert S (2004) 12-month comorbidity patterns and associated factors in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand 109:28–37
American Psychiatric Association (2000) DSM-IV-TR. Diagnostic and statistical manual of mental disorders (Text revision). Author, Washington, DC
American Psychiatric Association (2013) DSM-5. Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Anderson EC, Dryman MT, Worthington J, Hoge EA, Fischer LE, Pollack MH, Barrett LF, Simon NM (2013) Smiles may go unseen in generalized social anxiety disorder: evidence from binocular rivalry for reduced visual consciousness of positive facial expressions. J Anxiety Disord 27:619–626
Andersson E, Ruck C, Lavebratt C, Hedman E, Schalling M, Lindefors N, Eriksson E, Carlbring P, Andersson G, Furmark T (2013) Genetic polymorphisms in monoamine systems and outcome of cognitive behavior therapy for social anxiety disorder. PLoS One 8
Angst J, Vollrath M (1991) The natural history of anxiety disorders. Acta Psychiatr Scand 84:446–452
Assuncao MC, Costa DLD, De Mathis MA, Shavitt RG, Ferrao YA, Do Rorsario MC, Miguel EC, Torres AR (2012) Social phobia in obsessive-compulsive disorder: prevalence and correlates. J Affect Disord 143:138–147
Avant TS, Gazelle H, Faldowski R (2011) Classroom emotional climate as a moderator of anxious solitary children’s longitudinal risk for peer exclusion: a child x environment model. Dev Psychol 6:1711–1727
Ballash NG, Pemble MK, Usui WM, Buckley AF, Woodruff-Borden J (2006) Family functioning, perceived control, and anxiety: a mediational model. J Anxiety Disord 20:486
Bandelow B, Torrente AC, Wedekind D, Broocks A, Hajak G, Rüther E (2004) Early traumatic life events, parental rearing styles, family history of mental disorders, and birth risk factors in patients with social anxiety disorder. Eur Arch Psychiatr Clin Neurosci 254:397–405
Banerjee R, Henderson L (2001) Social-cognitive factors in childhood social anxiety: a preliminary investigation. Social Develop 10:558–572
Barrett PM, Rapee RM, Dadds MR, Ryan ND (1996) Family enhancement of cognitive style in anxious and aggressive children. J Abnorm Child Psychol 24:187–203
Beard C, Moitra E, Weisberg RB, Keller MB (2010) Characteristics and predictors of social phobia course in a longitudinal study of primary care patients. Depress Anxiety 27:839–845
Beck AT, Emery G, Greenberg RL (1985) Anxiety disorders and phobias: a cognitive perspective. Basic Books, New York
Beesdo K, Bittner A, Pine DS, Stein MB, Höfler M, Lieb R, Wittchen H-U (2007) Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Arch Gen Psychiatry 64:903–912
Beesdo-Baum K, Knappe S (2012) Developmental epidemiology of anxiety disorders. Child Adolesc Psychiatr Clin N Am 21:457–478
Beesdo-Baum K, Knappe S, Fehm L, Höfler M, Lieb R, Hofmann SG, Wittchen H-U (2012) The natural course of social anxiety disorder among adolescents and young adults. Acta Psychiatr Scand 126:411–425
Beidel DC, Turner SM, Morris TL (1999) Psychopathology of childhood social phobia. J Am Acad Child Adolesc Psychiatry 38:643–650
Beidel DC, Turner SM, Morris TL (2000) Behavioral treatment of childhood social phobia. J Consult Clin Psychol 68:1072–1080
Beidel DC, Alfano CA, Kofler MJ, Rao, PA, Scharfstein L, Sarver, NW (2014). The impact of social skills training for social anxiety disorder: A randomized controlled trial. 28:908–918
Blakemore S-J (2008) The social brain in adolescence. Nat Rev Neurosci 9:267–277
Blanco C, Xu Y, Schneier FR, Okuda M, Liu SM, Heimberg GRG (2011) Predictors of persistence of social anxiety disorder: a national study. J Psychiatr Res 45:1557–1563
Blöte AW, Kint MJW, Westenberg PM (2007) Peer behavior towards socially anxious adolescents: classroom observations. Behav Res Ther 45:2773–2779
Bögels SM, Brechmann-Toussaint ML (2006) Family issues in child anxiety: attachment, family functioning, parental rearing and beliefs. Clin Psychol Rev 26:834–856
Bögels SM, Perotti EC (2011) Does father know best? A formal model of the paternal influence on childhood social anxiety. J Child Fam Stud 20:171–181
Bögels SM, Phares V (2008) Fathers’ role in the etiology, prevention and treatment of child anxiety: a review and new model. Clin Psychol Rev 28:539–558
Bögels S, Stevens J, Majdandzic M (2011) Parenting and social anxiety: fathers’ versus mothers’ influence on their children’s anxiety in ambiguous social situations. J Child Psychol Psychiatry 52:599–606
Bouman T, van der Meulen M, Goossens FA, Olthof T, Vermande MM, Aleva EA (2012) Peer and self-reports of victimization and bullying: their differential association with internalizing problems and social adjustment. J Sch Psychol 50:759–774
Brook CA, Schmidt LA (2008) Social anxiety disorder: a review of environmental risk factors. Neuropsychiatr Dis Treat 4:123–143
Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano ME, Shea MT, Keller MB (2005) Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry 162:1179–1187
Buckner JD, Vinci C (2013) Smoking and social anxiety: the roles of gender and smoking motives. Addict Behav 38:2388–2391
Buckner JD, Schmidt NB, Bobadilla L, Taylor J (2006) Social anxiety and problematic cannabis use: evaluating the moderating role of stress reactivity and perceived coping. Behav Res Ther 44:1007–1015
Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM (2008) Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res 42:230–239
Budinger MC, Drazdowski TK, Ginsburg GS (2013) Anxiety-promoting parenting behaviors: a comparison of anxious parents with and without social anxiety disorder. Child Psychiatr Human Developt 44:412–418
Cartwright-Hatton S, Hodges L, Porter J (2003) Social anxiety in childhood: the relationship with self and observer rated social skills. J Clin Psychol Psychiatry 44:737–742
Cartwright-Hatton S, Tschernitz N, Gomersall H (2005) Social anxiety in children: social skills deficit, or cognitive distortion? Behavr Res Ther 43(1):131–141
Chartier MJ, Hazen AL, Stein MB (1998) Lifetime patterns of social phobia: a retrospective study of the course of social phobia in a nonclinical population. Depress Anxiety 7:113–121
Chavira DA, Stein MB, Bailey K, Stein MT (2004) Child anxiety in primary care: prevalent but untreated. Depress Anxiety 20:155–164
Chen X, Hastings PD, Rubin KH, Chen H, Cen G, Stewart SL (1998) Child-rearing attitudes and behavioral inhibition in Chinese and Canadian toddlers: a cross-cultural study. Dev Psychol 34:677–686
Christensen PN, Stein MB, Means-Christensen A (2003) Social anxiety and interpersonal perception: a social relations model analysis. Behav Res Ther 41:1355–1371
Clark DM, Wells A (1995) A cognitive model of social phobia. In: Heimberg RG, Liebowitz M, Hope DA, Schneier FR (eds) Social phobia: diagnosis, assessment, and treatment. Guilford, New York
Clauss JA, Blackford JU (2012) Behavioral inhibition and risk for developing social anxiety disorder: A meta-analytic study. J Am Acad Child Adolesc Psychiatry 51:1066–1075
Cludius B, Stevens S, Bantin T, Gerlach AL, Hermann C (2013) The motive to drink due to social anxiety and its relation to hazardous alcohol use. Psychol Addict Behav 27:806–813
Coles ME, Philipps BM, Menard W, Pagano ME, Fay C, Weisberg RB, Stout RL (2006) Body dysmorphic disorder and social phobia: cross-sectional and prospective data. Depress Anxiety 23:26–33
Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60:837–844
Cox BJ, Pagura J, Stein MB, Sareen J (2009) The relationship between generalized social phobia and avoidant personality disorder in a national mental health survey. Depress Anxiety 26:354–362
Creswell C, Schniering CA, Rapee RM (2005) Threat interpretation in anxious children and their mothers: comparison with nonclinical children and the effects of treatment. Behav Res Ther 43:1375–1381
Creswell C, Woolgar M, Cooper P, Giannakakis A, Schofield E, Young AW, Murray L (2008) Processing of faces and emotional expressions in infants at risk of social phobia. Cogn Emot 22:437–458
Creswell C, Cooper P, Giannakakis A, Schofield E, Woolgar M, Murray L (2011) Emotion processing in infancy: specificity in risk for social anxiety and associations with two year outcomes. J Exp Psychopathol 2:490–508
Creswell C, Murray G, Cooper P (2014) Interpretation and expectation in childhood anxiety disorders: age effects and social specificity. J Abnorm Child Psychol 42:453–465
Crippa JAS, Loureiro SR, Bapista CA, Osorio F (2007) Are there differences between early- and late-onset social anxiety disorder? Revista Brasileira De Psiquiatria 29:195–196
Davidson JRT, Hughes DC, George LK, Blazer DG (1994) The boundary of social phobia: exploring the threshold. Arch Gen Psychiatry 51:975–983
De Graaf R, Bijl RV, Smit F, Vollebergh WAM, Spijker J (2002) Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: findings from the Netherlands Mental Health Survey and Incidence Study. Am J Psychiatry 159(4):620–629
De Menezes GB, Fontenelle LF, Versiani MR (2005) Early-onset social anxiety disorder in adults: Clinical and therapeutic features. Rev Bras Psiquiatr 27:32–36
Deardorff J, Hayward C, Wilson KA, Bryson S, Hammer LD, Agras S (2007) Puberty and gender interact to predict social anxiety symptoms in early adolescence. J Adolesc Health 41(1):102–124
Demir T, Karacetin G, Demir DE, Uysal O (2013) Prevalence and some psychosocial characteristics of social anxiety disorder in an urban population of Turkish children and adolescents. Eur Psychiatry 28:64–69
Dewit DJ, Ogborne A, Offord DR, MacDonald K (1999) Antecedents of the risk of recovery from DSM-III-R social phobia. Psychol Med 29:569–582
Dewit DJ, Chandler-Coutts M, Offord DR, King G, McDougall J, Specht J, Stewart S (2005) Gender differences in the effects of family adversity on the risk of onset on DSM III-R social phobia. J Anxiety Disord 19:479–502
DiLalla LF, Kagan J, Reznick JS (1994) Genetic etiology of behavioral inhibition among 2-year-old children. Infant Behav Dev 17:405–412
Dinnel DL, Kleinknecht RA, Tanaka-Matsumi J (2002) A cross-cultural comparison of social phobia symptoms. J Psychopathol Behavl Assess 24:75–84
Domschke K, Deckert J (2012) Genetics of anxiety disorders – status Quo and quo vadis. Curr Pharm Des 18:5691–5698
Domschke K, Stevens S, Beck B, Baffa A, Hohoff C, Deckert J, Gerlach AL (2009) Blushing propensity in social anxiety disorder: influence of serotonin transporter gene variation. J Neural Transm 116:663–666
Eley TC, Rijsdijk FV, Perrin S, O'Connor TG, Bolton D (2008) A multivariate genetic analysis of specific phobia, separation anxiety and social phobia in early childhood. J Abnorm Child Psychol 36:839–848
Elizabeth J, King N, Ollendick TH, Gullone E, Tonge B, Watson S, Macdermott S (2006) Social anxiety disorder in children and youth: a research update on aetiological factors. Couns Psychol Q 19:151–163
Eng W, Heimberg RG, Hart TA, Schneier FR, Liebowitz MR (2001) Attachment in individuals with social anxiety disorder: the relationship among adult attachment styles, social anxiety, and depression. Emotion 1
Erath SA, Flanagan KS, Biedermann KL (2008) Early adolescent school-adjustment: associations with friendship and peer victimization. Soc Devel 17:853–870
Essau CA, Conradt J, Petermann F (2002) Course and outcome of anxiety disorders in adolescents. J Anxiety Disord 16:67–81
Essau CA, Sasagawa S, Ishikawa S, Okajima I, O’Callaghan J, Bray D (2012) A Japanese form of social anxiety (taijin kyofusho): frequency and correlates in two generations of the same family. Int J Soc Psychiatry 58:635–642
Faravelli C, Zucchi T, Viviani B, Salmoria R, Perone A, Paionni A, Scarpato A, Vigliaturo D, Rosi S, D'Adamo D, Bartolozzi D, Cecchi C, Abrardi L (2000) Epidemiology of social phobia: a clinical approach. Eur Psychiatry 15:17–24
Feehan M, McGee R, Raha SN, Williams SM (1994) DSM-III-R disorders in New Zealand 18-year-olds. Aust N Z J Psychiatry 28:87–99
Fehm L, Pelissolo A, Furmark T, Wittchen H-U (2005) Size and burden of social phobia in Europe. Eur Neuropsychopharmacol 15:453–462
Fehm L, Beesdo K, Jacobi F, Fiedler A (2008) Social anxiety disorder above and below the diagnostic threshold: prevalence, comorbidity and impairment in the general population. Soc Psychiatry Psychiatr Epidemiol 43:257–265
Frick A, Howner K, Fischer H, Eskildsen SF, Kristiansson M, Furmark T (2013) Cortical thickness alterations in social anxiety disorder. Neurosci Lett 536:52–55
Fu C-W, Tan AW, Sheng F, Luan R-S, Zhan S-Y, Chen W-Q et al (2007) The prevalence of anxiety symptoms and depressive symptoms in patients with somatic disorders in urban China: a multi-center cross-sectional study. Int J Psychiatry Med 37:185–199
Garcia-Lopez LJ, Ingles C, Garcia-Fernandez JM (2008) Exploring the relevance of gender and age differences in the assessment of social fears in adolescence. Soc Behav Personal 36:385–390
Garcia-Lopez LJ, Beidel DC, Hidalgo MD, Olivares J, Turner S (2008a) Brief form of the Social Phobia and Anxiety Inventory (SPAI-B) for adolescents. Eur J Psychol Assess 24:150–156
Garcia-Lopez LJ, Muela JA, Espinosa-Fernández L, Diaz-Castela MM (2009) Exploring the relevance of expressed emotion to the treatment of social anxiety disorder in adolescence. J Adolesc 32:1371–1376
Garcia-Lopez LJ, Irurtia MJ, Caballo VE, Díaz-Castela MM (2011) Ansiedad social y abuso psicológico [Social anxiety and psychological abuse]. Behav Psycholy 19:223–236
Garcia-Lopez LJ, Diaz-Castela MM, Muela-Martinez JA, Espinosa-Fernandez L (2014) Can parent training for parents with high levels of expressed emotion have a positive effect on their child’s social anxiety improvement? J Anxiety Disord 28:812–822
Garcia-Lopez LJ, Moore H (2015a) The Mini-Social Phobia Inventory: psychometric properties in an adolescent general and clinical population. PLOS One (in press)
Garcia-Lopez LJ, Saez-Castillo A, Beidel DC, La Greca AM (2015b) Brief measures to screen for social anxiety in adolescents. Manucript submitted for publication
Gazelle H (2006) Class climate moderates peer relations and emotional adjustment in children with an early history of anxious solitude: a child x environment model. Dev Psychol 42:1179–1192
Gelernter J, Page GP, Stein MB, Woods SW (2004) Genome-wide linkage scan for loci predisposing to social phobia: evidence for a chromosome 16 risk locus. Am J Psychiatry 161:59–66
Gentili C, Ricciardi E, Gobbini MI, Santarelli MF, Haxby JV, Pietrini P, Guazzelli M (2009) Beyond amygdala: default Mode Network activity differs between patients with social phobia and healthy controls. Brain Res Bull 79:409–413
Godart N, Flament M, Perereau F, Jeammet P (2002) Co-morbidity between eating disorders and anxiety disorders: a review. Int J Eat Diosrd 32:253–270
Goldin PR, Manber T, Hakimi S, Canli T, Gross JJ (2009) Neural bases of social anxiety disorder. Emotional reactivity and cognitive regulation during social and physical threat. Arch Gen Psychiatry 66:170–180
Gómez-Ariza CJ, Iglesias-Parro S, Garcia-Lopez LJ, Díaz-Castela MM, Espinosa-Fernández L, Muela JA (2013) Selective intentional forgetting in adolescents with social anxiety disorder. Psychiatry Res 208:151–155
Gregory AM, Eley TC (2007) Genetic Influences on anxiety in children: what we’ve learned and where we’re heading. Clin Child Fam Psychol 10:199–212
Gregory AM, Caspi A, Moffitt TE, Koenen K, Eley TC, Poulton R (2007) Juvenile mental health histories of adults with anxiety disorders. Am J Psychiatry 164:301–308
Gren-Landell M, Aho N, Andersson G, Svedin CG (2011) Social anxiety disorder and victimization in a community sample of adolescents. J Adolesc 34:569–577
Gulley LD, Oppenheimer CW, Hankin BL (2014) Associations among negative parenting, attention bias to anger, and social anxiety among youth. Dev Psychol 50(2):577–585
Haller SPW, Kadosh KC, Lau JYF (2014) A developmental angle to understanding the mechanisms of biased cognitions in social anxiety. Front Hum Neurosci 7:846
Halls G, Cooper PJ, Creswell C (2015) Social communication deficits: specific associations with Social Anxiety Disorder. J Affect Disord 172:38–42
Hayward C, Killen JD, Kraemer HC, Taylor CB (1998) Linking self-reported behavioral inhibition to adolescent social phobia. J Am Acad Child Adolesc Psychiatry 27:1308–1316
Heinrichs N, Rapee RM, Alden LA, Bögels S, Hofmann SG, Ja Oh K, Sakano Y (2006) Cultural differences in perceived social norms and social anxiety. Behav Res Ther 44:1187–1197
Hirshfeld DR, Biederman J, Brody L, Faraone SV, Rosenbaum JF (1997) Expressed emotion toward children with behavioral inhibition: associations with maternal anxiety disorder. J Am Acad Child Adolesc Psychiatry 36:910–917
Hoffman SO (2002) Die Psychodynamik der Sozialen Phobien (The psychodynamics of social anxiety disorder). Forum der Psychoanalyse 18:51–71
Hong JJ, Woody SR (2007) Cultural mediators of self-reported social anxiety. Behav Res Ther 45:1779–1789
Hsu L, Alden L (2007) Social anxiety in Chinese- and European-heritage students: the effect of assessment format and judgments of impairment. Behav Ther 38:120–131
Hughes AA, Heimberg RG, Coles ME, Gibb BE, Liebowitz MR, Schneier FR (2006) Relations of the factors of the tripartite model of anxiety and depression to types of social anxiety. Behav Res Ther 44:1629–1641
Hwu HG, Yeh EK, Chang LY (1989) Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule. Acta Psychiatr Scand 79:136–147
Inderbitzen-Nolan HM, Anderson ER, Johnson HS (2007) Subjective versus objective behavioral ratings following two analogue tasks: a comparison of socially phobic and non-anxious adolescents. J Anxiety Disord 21:76–90
Johnson EO, Roth T, Breslau N (2006) The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res 40(8):700–708
Kagan J, Reznick JS, Snidman N (1987) The physiology and psychology of behavioral inhibition in children. Child Dev 58:1459–1473
Kagan J, Reznick JS, Snidman N (1988a) Biological bases of childhood shyness. Science 240:167–171
Kagan J, Reznick JS, Snidman N, Gibbons J, Johnson MO (1988b) Childhood derivates of inhibition and lack of inhibition to the unfamiliar. Child Dev 59:1580–1589
Keller MB (2003) The lifelong course of social anxiety disorder: a clinical perspective. Acta Psychiatr Scand 108:85–94
Keller MB (2006) Social anxiety disorder clinical course and outcome: Review of Harvard/Brown Anxiety Research Project (HARP) findings. J Clin Psychiatry 67:14–19
Kendall PC (1985) Toward a cognitive-behavioral model of child psychopathology and a critique of related interventions. J Abnorm Child Psychol 13:357–372
Kendler KS, Prescott CA, Jacobson K, Myers J, Neale MC (2002) The joint analysis of personal interview and family history diagnoses: evidence for validity of diagnosis and increased heritability estimates. Psychol Med 32:829–845
Kendler KS, Gardner CO, Annas P, Lichtenstein P (2008) The development of fears from early adolescence to young adulthood: a multivariate study. Psychol Med 38:1759–1769
Kerns CE, Comer JS, Pincus DB, Hofmann SG (2013) Evaluation of the proposed social anxiety disorder specifier change for DSM-5 in a treatment-seeking sample of anxious youth. Depress Anxiety 30:709–715.
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Study. Arch Gen Psychiatry 51:8–19
Kessler RC, Stein MB, Berglund P (1998) Social phobia subtypes in the national comorbidity survey. Am J Psychiatry 155:613–619
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005a) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602
Kessler RC, Chui WT, Demler O, Merikangas KR, Walters EE (2005b) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:617–627
Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He JP, Koretz D, McLaughlin KA, Petukhova M, Samspon NA, Zaslavsky AM, Merikangas KR (2012) Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry 69:372–380
Kim-Cohen J, Caspi A, Moffitt TE, Harrington HL, Milne BJ, Poulton R (2003) Prior juvenile diagnosis in adults with mental disorders: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 60:709–717
Kleinknecht RA, Dinnel DL, Kleinknecht EE, Hiruma N (1997) Cultural factors in social anxiety: a comparison of social phobia symptoms and Taijin Kyofusho. J Anxiety Disord 11:157–177
Knappe S, Beesdo K, Fehm L, Lieb R, Wittchen H-U (2009a) Associations of familial risk factors with social fears and social phobia: evidence for the continuum hypothesis in social anxiety disorder ? J Neural Transm 116:639–648
Knappe S, Lieb R, Beesdo K, Fehm L, Low NCP, Gloster AT, Wittchen H-U (2009b) The role of parental psychopathology and family environment for social phobia in the first three decades of life. Depress Anxiety 26:363–370
Knappe S, Beesdo K, Fehm L, Höfler M, Lieb R, Wittchen H-U (2009c) Do parental psychopathology and unfavorable family environment predict the persistence of social phobia? J Anxiety Disord 23:986–994
Knappe S, Beesdo-Baum K, Wittchen H-U (2010) Familial risk factors in social anxiety disorder: calling for a family-oriented approach for targeted prevention and early intervention. Eur Child Adolesc Psychiatry 19:857–871
Knappe S, Beesdo K, Fehm L, Stein MB, Lieb R, Wittchen HU (2011) Social fear and social phobia types among community youth: differential clinical features and vulnerability factors. J Psychiatr Res 45:111–120
Knappe S, Beesdo-Baum K, Fehm L, Lieb R, Wittchen H-U (2012) Characterizing the association between parental rearing and adolescent social phobia. J Anxiety Disord 26:608–616
La Greca AM, Stone WL (1993) Social anxiety scale for children-revised: factor structure and concurrent validity. J Clin Child Psychol 22:17–27
La Greca AM, Dandes SK, Wick P, Shaw K (1988) Development of the social anxiety scale for children: reliability and concurrent validity. J Clin Child Psychol 17:84–91
Lampe L, Slade T, Issakidis C, Andrews G (2003) Social phobia in the Australian National Survey of Mental Health and Well-Being (NSMHWB). Psychol Med 33:637–646
Last CG, Perrin S, Hersen M, Kazdin AE (1992) DSM-III-R anxiety disorders in children: sociodemographic and clinical characteristics. J Am Acad Child Adolesc Psychiatry 31:1070–1076
Last CG, Perrin S, Hersen M, Kazdin AE (1996) A prospective study of childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry 35:1502–1510
Lee MR, Okazaki S, Yoo HC (2006) Frequency and intensity of social anxiety in Asian Americans and European Americans. Cultu Divers Ethnic Minor Psychol 12:291–305
Lee S, Ng KL, Kwok KPS, Tsang A (2009) Prevalence and correlates of social fears in Hong Kong. J Anxiety Disord 23:327–332
Lépine J-P, Wittchen H-U, Essau CA (1993) Lifetime and current comorbidity of anxiety and depressive disorders: results from the International WHO/ADAMHA CIDI Field Trials. Int J Methods Psychiatr Res 3:67–78
Levinson CA, Langer JK, Rodebaugh TL (2013) Reactivity to social exclusion prospectively predicts social anxiety symptoms in young adults. Behav Ther 44
Lewis-Morrarty E, Degnan KA, Chronis-Tuscano A, Rubin KH, Cheah CS, Pine DS, Henderon HA, Fox NA (2012) Maternal over-control moderates the association between early childhood behavioral inhibition and adolescent social anxiety symptoms. J Abnorm Child Psychol 40(8):1363–1373
Lieb R, Wittchen H-U, Höfler M, Fuetsch M, Stein MB, Merikangas KR (2000) Parental psychopathology, parenting styles and the risk of social phobia in offspring: a prospective-longitudinal community study. Arch Gen Psychiatry 57:859–866
Liebowitz MR, Gorman JM, Fyer AJ, Klein DF (1985) Social phobia: review of a neglected anxiety disorder. Arch Gen Psychiatry 42:729
Lim SW, Ha J, Shin YC, Shin DW, Bae SM, Oh KS (2013) Clinical differences between early- and late-onset social anxiety disorders. Early Interv Psychiatry 7:44–50
Machado-de-Sousa JP, Osorio FD, Jackowski AP, Bressan RA, Chagas MHN, Torro-Alves N, Depaula ALD, Crippa JAS, Hallak JEC (2014) Increased amygdalar and hippocampal volumes in young adults with social anxiety. PLoS One 9(2):e88523
MacKenzie MB, Fowler KF (2013) Social anxiety disorder in the Canadian population: exploring gender differences in sociodemographic profile. J Anxiety Disord 27:427–434
Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC (1996) Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry 53:159–168
Majdandzic M, Moller EL, de Vente W, Bogels SM, van den Boom DC (2014) Fathers’ challenging parenting behavior prevents social anxiety development in their 4-year-old children: a longitudinal observational study. J Abnorm Child Psychol 42:301–310
Massion AO, Dyck IR, Shea MT, Phillips KA, Warshaw MG, Keller MB (2002) Personality disorders and time to remission in generalized anxiety disorder, social phobia, and panic disorder. Arch Gen Psychiatry 59:434–440
Matheny AP (1989) Children’s behavioral inhibition over age and across situations: genetic similarity for a trait during change. J Pers 57:215–235
McCabe RE, Antony MM, Summerfeldt LJ, Liss A, Swinson RP (2003) Preliminary examination of the relationship between anxiety disorders in adults and self-reported history of teasing. Cogn Behav Ther 32:187–193
McGrath LM, Weill S, Robinson EB, MacRae R, Smoller JW (2012) Bringing a developmental perspective to anxiety genetics. Dev Psychopathol 24:1179–1193
McLeod BD, Wood JJ, Weisz JR (2007) Examining the association between parenting and childhood anxiety: a meta-analysis. Clin Psychol Rev 27:155–172
McNeil DW (2001) Terminology and evolution of constructs in social anxiety and social phobia. In: Hofmann SG, Dibartolo PM (eds) From social anxiety to social phobia. Allyn & Bacon, Needham Heights
Merikangas KR, Avenevoli S, Acharyya S, Zhang H, Angst J (2002) The spectrum of social phobia in the Zurich cohort study of young adults. Biol Psychiatry 51:81–91
Merikangas KR, Lieb R, Wittchen H-U, Aveneoli S (2003) Family and high-risk studies of social anxiety disorder. Acta Psychiatr Scand 108:28–37
Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui LH, Benjet C, Georgiades K, Swendsen J (2011) Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 49:980–989
Monk CS, Nelson EE, McClure EB, Mogg K, Bradley BP, Leibenluft E, Blair RJ, Chen G, Charney DS, Ernst M, Pine DS (2006) Ventrolateral prefrontal cortex activation and attentional bias in response to angry faces in adolescents with generalized anxiety disorder. Am J Psychiatry 163:1091–1097
Morgan J, Banerjee M (2006) Social anxiety and self-evaluation of social performance in a nonclinical sample of children. J Clin Child Adolesc Psychol 35:292–301
Morrison AS, Heimberg RG (2013) Social anxiety and Social anxiety disorder. Annu Rev Clin Psychol 9(9):249–274
Murray L, Cooper P, Creswell C, Schofield E, Sack C (2007) The effects of maternal social phobia on mother-infant interactions and infant social responsiveness. J Child Psychol Psychiatry 48:45–52
Murray L, de Rosney M, Pearson J, Bergeron C, Schofield E, Royal-Lawson M, Cooper PJ (2008) Intergenerational transmission of social anxiety: the role of social referencing processes in infancy. Child Dev 79:1049–1064
Murray L, Creswell C, Cooper PJ (2009) The development of anxiety disorders in childhood: an integrative review. Psychol Med 39:1413–1423
Murray L, Lau PY, Arteche A, Creswell C, Russ S, Zoppa LD, Muggeo M, Stein A, Cooper P (2012) Parenting by anxious mothers: effects of disorder subtype, context and child characteristics. J Child Psychol Psychiatry 53:188–196
Murray L, Pella J, De Pascalis L, Arteche A, Pass L, Percy R, Creswell C, Cooper P (2014) Socially anxious mothers’ narratives to their children, and their relation to child representations and adjustment. Dev Psychopathol 26(4 Pt 2):1531–1546
Nagata T, Yamada H, Teo AR, Yoshimura C, Nakajima T, van Vliet I (2013) Comorbid social withdrawal (hikikomori) in outpatients with social anxiety disorder: clinical characteristics and treatment response in a case series. Int J Soc Psychiatry 59:73–78
Natsuaki MN, Leve LD, Neiderhiser JM, Shaw DS, Scaramella LV, Ge X, Reiss D (2013) Intergenerational transmission of risk for social inhibition: the interplay between parental responsiveness and genetic influences. Dev Psychopathol 25:261–274
Neufeld KJ, Swartz KL, Bienvenu OJ, Eaton WW, Cai G (1999) Incidence of DIS/DSM-IV social phobia in adults. Acta Psychiatr Scand 100:186–192
Noyes R, Holt CS, Woodman CL (2005) Natural course of anxiety disorders. In: Mavissakalian MR, Prien RF (eds) Long-term treatment of anxiety disorders. American Psychiatric Press, Inc, Washington, DC
Pass L, Arteche A, Cooper P, Creswell C, Murray L (2012) Doll Play narratives about starting school in children of socially anxious mothers, and their relation to subsequent child school-based anxiety. J Abnormal Child Psychol 40(8):1375–1384
Pejic T, Hermann A, Vaitl D, Stark R (2013) Social anxiety modulates amygdala activation during social conditioning. Soc Cogn Affect Neurosci 8:267–276
Peleg-Popko O, Dar R (2001) Marital quality, family patterns, and children's fears and social anxiety. Contemp Fam Ther: Int Jl 23:465–487
Pine DS, Cohen P, Gurley D, Brook J, Ma Y (1998) The risk for early adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 55:56–64
Ranta K, Kaltiala-Heino R, Pelkonen M, Marttunen M (2009a) Associations between peer-victimization, self-reported depression and social phobia among adolescents: the role of comorbidity. J Adolesc 32:77–93
Ranta K, Kaltiala-Heino R, Rantanen P, Marttunen M (2009b) Social phobia in Finnish general adolescent population: Prevalence, comorbidity, individual and family correlates, and service use. Depress Anxiety 26:528–236
Ranta K, Kaltiala-Heino R, Fröjd S, Marttunen M (2013) Peer victimization and social phobia: a follow-up study among adolescents. Soc Psychiatry Psychiatr Epidemiol 48:533–544
Rao PA, Beidel DC, Turner SM, Ammerman RT, Crosby LE, Sallee FR (2007) Social anxiety disorder in childhood and adolescence: descriptive psychopathology. Behav Res Ther 45:1181–1191
Rapee RM, Heimberg RG (1997) A cognitive-behavioral model of anxiety in social phobia. Behav Res Ther 35:741–756
Rapee RM, Spence SH (2004) The etiology of social phobia: empirical evidence and an initial model. Clin Psychol Rev 24:737–767
Rietdijk J, Ising HK, Dragt S, Klaassen R, Nieman D, Wunderink L, Cuijpers P, Linszen D, van der Gaag M (2013) Depression and social anxiety in help-seeking patients with an ultra-high risk for developing psychosis. Psychiatry Res 209:309–313
Robinson JL, Kagan J, Reznick JS, Corley R (1992) The heritability of inhibited and uninhibited behavior: a twin study. Dev Psychol 28:1030–1037
Rogers MP, Weinshenker NJ, Warshaw MG, Goisman RM, Rodriguez-Villa FJ, Fierman EJ, Keller MB (1996) Prevalence of somatoform disorders in a large sample of patients with anxiety disorders. Psychosomatics: J Consult Liaison Psychiatry 37:17
Roth DA, Coles ME, Heimberg RG (2002) The relationship between memories for childhood teasing and anxiety and depression in adulthood. J Anxiety Disord 16(2):149–164
Roy AK, Vasa RA, Bruck M, Mogg K, Bradley BP, Sweeney M, Bergman RL, McClure-Tone EB, Pine DS (2008) Attention bias toward threat in pediatric anxiety disorders. J Am Acad Child Adolesc Psychiatry 47:1189–1196
Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC (2008) Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychol Med 38:15–28
Rutter M, Kim-Cohen J, Maughan B (2006) Continuities and discontinuities in psychopathology between childhood and adult life. J Child Psychol Psychiatry 47:276–295
Sareen J, Cox BJ, Afifi TO, de Graaf R, Asmundson GJG, ten Have M, Stein MB (2005a) Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry 62:1249–1257
Sareen J, Cox BJ, Clara I, Asmundson GJG (2005b) The relationship between anxiety disorders and physical disorders in the U.S. National Comorbidity Survey. Depress Anxiety 21:193–202
Sareen J, Chartier MJ, Paulus MP, Stein MB (2006) Illicit drug use and anxiety disorders: findings from two community surveys. Psychiatry Res 142:11–17
Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM (1992) Social phobia: comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry 49:282–288
Schry AR, White SW (2013) Understanding the relationship between social anxiety and alcohol use in college students: a meta-analysis. Addict Behav 38:2690–2706
Schutters SIJ, Dominguez MD, Knappe S, Lieb R, van Os J, Schruers KRJ, Wittchen HU (2011) The association between social phobia, social anxiety cognitions and paranoid symptoms. Acta Psychiatr Scand 125:213–227
Schwartz CE, Snidman N, Kagan J (1999) Adolescent social anxiety as an outcome of inhibited temperament in childhood. J Am Acad Child Adolesc Psychiatry 38:1008–1015
Sibrava NJ, Beard C, Bjornsson AS, Moitra E, Weisberg RB, Keller MB (2013) Two-year course of generalized anxiety disorder, social anxiety disorder, and panic disorder in a longitudinal sample of African American adults. J Consult Clin Psychol 81:1052–1062
Siegel RS, La Greca AM, Harrison HM (2009) Peer victimization and social anxiety in adolescents: prospective and reciprocal relationships. J Youth Adolesc 38
Sonntag H, Wittchen HU, Höfler M, Kessler RC, Stein MB (2000) Are social fears and DSM IV social anxiety disorder associated with smoking and nicotine dependence in adolescents and young adults? Eur Psychiatry 15:67–74
Spence SH, Donovan C, Brechman-Toussaint M (1999) Social skills, social outcomes, and cognitive features of childhood social phobia. J Abnorm Psychol 108:211–221
Spence SH, Donovan C, Brechman-Toussaint M (2000) The treatment of childhood social phobia: the effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. J Child Psychol Psychiatry 41:713–726
Stein MB, Kroft CDL, Walker JR (1993) Sleep impairment in patients with social phobia. Psychiatry Res 49:251–256
Stein MB, Walker JR, Forde DR (1994) Setting diagnostic thresholds for social phobia. Considerations from a community survey of social anxiety. Am J Psychiatry 151:408–412
Stein MB, Chavira DA, Jang KL (2001a) Bringing up a bashful baby: developmental pathways to social phobia. Psychiatr Clin North Am 24:661–675
Stein MB, Fuetsch M, Müller N, Höfler M, Lieb R, Wittchen H-U (2001b) Social anxiety disorder and the risk of depression: a prospective community study of adolescents and young adults. Arch Gen Psychiatry 58:251–256
Steinert C, Hofmann M, Leichsenring F, Kruse J (2013) What do we know today about the prospective long-term course of social anxiety disorder? A systematic literature review. J Anxiety Disord 27:692–702
Stevens S, Cludius B, Bantin T, Hermann C, Gerlach AL (2014) Influence of alcohol on social anxiety: an investigation of attentional, physiological and behavioral effects. Biol Psychol 96:126–133
Stevenson-Hinde J, Shouldice A (1990) Fear and attachment in 2,5 year olds. Br J Dev Psychol 8:319–333
Stirling LJ, Eley TC, Clark DM (2006) Preliminary evidence for an association between social anxiety symptoms and avoidance of negative faces in school-age children. J Clin Child Adolesc Psychol 35:431–439
Storch EA, Masia-Warner C, Crisp H, Klein RG (2005) Peer victimization and social anxiety in adolescence: a prospective study. Aggress Behav 31:437–452
Suveg C, Zeman J, Flannery-Schroeder E, Cassano M (2005) Emotion socialization in families of children with an anxiety disorder. J Abnorm Child Psychol 33:145
Swinbourne JM, Touyz SW (2007) The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev 15:253–274
Tamplin A, Goodyer IM (2001) Family functioning in adolescents at high and low risk for major depressive disorder. Eur Child Adolesc Psychiatry 10:170–179
Teetsel RN, Ginsburg GS, Drake KL (2014) Anxiety-promoting parenting behaviors: a comparison of anxious mothers and fathers. Child Psychiatry Hum Dev 45:133–142
Tillfors M, Persson S, Willen M, Burk WJ (2012) Prospective links between social anxiety and adolescent peer relations. J Adolesc 35:1255–1263
Tsuchiya M, Kawakami N, Ono Y, Nakane Y, Nakamura Y, Tachimori H, Wata N, Uda H, Nakane H, Watanabe M, Naganuma Y, Furukawa TA, Hata Y, Kobayashi M, Miyake Y, Takeshima T, Kikkawa T, Kessler RC (2009) Lifetime comorbidities between phobic disorders and major depression in Japan. Results from the World Mental Health Japan 2002-2004 Survey. Depress Anxiety 26:949–955
Van Ameringen M, Mancini C, Oakman JM (1998) The relationship of behavioral inhibition and shyness to anxiety disorder. J Nerv Mental Dis 186:425–431
van Beljouw IMJ, Verhaak PFM, Cuijpers P, van Marwijk HWJ, Penninx B (2010) The course of untreated anxiety and depression, and determinants of poor one-year outcome: a one-year cohort study. BMC Psychiatry 10:86
van Brakel AML, Muris P, Bögels SM, Thomassen C (2006) A multifactorial model for the etiology of anxiety in non-clinical adolescents: main and interactive effects of behavioral inhibition, attachment and parental rearing. J Child Fam Stud 15:569–579
Van Steensel FJ, Bögels SM, Wood JJ (2013) Autism spectrum traits in children with anxiety disorders. J Autism Dev Disord 43:361–370
Vernberg EM, Abwender DA, Ewell KK, Beery SH (1992) Social anxiety and peer relationships in early adolescence: a prospective analysis. J Clin Child Psychol 21:189–196
Voci SC, Beitchman JH, Brownlie EB, Wilson B (2006) Social anxiety in late adolescence: the importance of early childhood language impairment. J Anxiety Disord 20:915–930
Vriends N, Becker ES, Meyer A, Williams SL, Lutz R, Margraf J (2007) Recovery from social phobia in the community and its predictors: data from a longitudinal epidemiological study. J Anxiety Disord 21:320–337
Vriends N, Pfaltz MC, Novianti P, Hadiyono J (2013) Taijin kyofusho and social anxiety and their clinical relevance in Indonesia and Switzerland. FrontPsychol 4:3
Waters AM, Bradley BP, Mogg K (2014) Biased attention to threat in paediatric anxiety disorders (generalized anxiety disorder, social phobia, specific phobia, separation anxiety disorder) as a function of ‘distress’ versus ‘fear’ diagnostic categorization. Psychol Med 44:607–616
Wittchen H-U, Fehm L (2001) Epidemiology, patterns of comorbidity and associated disabilities of social phobia. Psychiatr Clin North Am 24:617–641
Wittchen H-U, Lieb R, Schuster P, Oldehinkel AJ (1999a) When is onset? Investigations into early developmental stages of anxiety and depressive disorders. In: Rapoport JL (ed) Childhood onset of “adult” psychopathology, clinical and research advances. American Psychiatric Press, Washington
Wittchen HU, Stein MB, Kessler RC (1999b) Social fears and social phobia in a community sample of adolescents and young adults: prevalence, risk factors and comorbidity. Psychol Med 29:309–323
Wood JJ, McLeod BD, Sigman M, Hwang W-C, Chu BC (2003) Parenting and childhood anxiety: theory, empirical findings, and future directions. J Child Psychol Psychiatry 44:134–151
Xu Y, Schneier F, Heimberg RG, Princisvalle K, Liebowitz MR, Wang S, Blanco C (2012) Gender differences in social anxiety disorder: results from the national epidemiologic sample on alcohol and related conditions. J Anxiety Disord 26:12–19
Yonkers KA, Bruce SE, Dyck IR, Keller MB (2003) Chronicity, relapse, and illness – course of manic disorder, social phobia, and generalized anxiety disorder: findings in men and women from 8 years of follow-up. Depress Anxiety 17:173–179
Zhang W, Ross J, Davidson JRT (2004) Social anxiety disorder in callers to the Anxiety Disorders Association of America. Depress Anxiety 20:101–106
Zimmerman G, Pin MA, Krenz S, Bouchat A, Favrat B, Besson J, Zullino DF (2004) Prevalence of social phobia in a clinical sample of drug dependent patients. J Affect Disord 83:83–87
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Knappe, S., Sasagawa, S., Creswell, C. (2015). Developmental Epidemiology of Social Anxiety and Social Phobia in Adolescents. In: Ranta, K., La Greca, A., Garcia-Lopez, LJ., Marttunen, M. (eds) Social Anxiety and Phobia in Adolescents. Springer, Cham. https://doi.org/10.1007/978-3-319-16703-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-16703-9_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16702-2
Online ISBN: 978-3-319-16703-9
eBook Packages: MedicineMedicine (R0)