Abstract
The importance of the spinal cord collateral network and its physiology have been extensively studied over the last few decades, and a detailed description of the anatomy of the vasculature and its structural changes in response to diminished input after extensive aortic repair—open or endovascular—has led to a better understanding and adjustments in treatment. The continuing advances in endovascular techniques call for new approaches to prevent paraplegia. A staged approach, temporary aneurysm sac perfusion (TASP), and endovascular coiling of intercostal and lumbar arteries—segmental arteries (SAs)—are all believed to minimize the risk of this devastating complication by stimulating the development of a denser collateral vasculature with many interconnections not only within the spinal cord, but also within the paraspinous muscles, with inflow from the subclavian and hypogastric arteries. By the time the thoracoabdominal aorta is repaired—during which a substantial number of SAs are sacrificed—the collateral network has been enhanced enough to compensate for the loss of direct inflow, and protect the cord from ischemic damage.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Spinal cord ischemia
- Thoracoabdominal aortic aneurysm
- Endovascular
- Paraplegia
- Coiling
- Segmental arteries
- TASP
- TEVAR
- Collateral network
- Remodeling
Introduction
Endovascular repair of aortic aneurysms has evolved as the primary treatment strategy for many patients suffering from infrarenal aortic pathologies, and already represents an alternative treatment for patients with aortic aneurysms involving the thoracic and visceral segment of the aorta. With the implementation of fenestrated and branched stent grafts, we are now facing different complications than were usually encountered after open repair, but certain issues remain unsolved. Among these, paraplegia as a consequence of spinal cord ischemic damage has an incidence as high as 30 % in some reports, is the most devastating complication to patients and most dreaded by surgeons. Paraplegia results in dramatic life changes and often in early mortality, encouraging us in the quest for ways to minimize its risk.
Background
Anatomy
To understand the anatomy of the spinal cord vasculature and its physiological mechanisms as a reaction to critical changes in spinal cord perfusion is a vital first step toward improved treatment. The spinal cord is nourished by three major arteries: the anterior spinal artery (ASA ) feeds the anterior two-thirds of the spinal cord, and two posterior spinal arteries provide blood flow to the posterior third. Arising from the aorta, intercostal and lumbar arteries give off branches to the spinal arteries: the anterior and posterior radicular–medullary arteries (ARMA, Fig. 7.1).
High-resolution CT scan of the vasculature. The aorta (1) gives rise to the segmental arteries (2), which run around the vertebral bodies and connect to the anterior spinal artery (3) through the anterior radicular–medullary arteries (4), and give off branches to the epidural arcades (5). Its connections with the dense vasculature within the paraspinous muscles can also be seen (6). Reprinted from The Journal of Thoracic and Cardiovascular Surgery, 144(6), Geisbusch S, Schray D, Bischoff S, Lin HM, Griepp RB, Di Luozzo G, Imaging of vascular remodeling after simulated thoracoabdominal aneurysm repair, 1471–8, Copyright 2012, with permission from Elsevier
The traditional teaching that there exists one dominant artery which feeds the spinal cord, the artery of Adamkiewicz, has dominated the thinking of surgeons seeking to safeguard spinal cord perfusion, and many attempts have been made to identify and preserve this elusive vessel preoperatively and intraoperatively, recently using high-resolution computed tomographic angiography (CTA ). Unfortunately, however, valiant attempts to re-implant SAs associated with prominent radicular arteries have been frustrated by lack of improvement in paraplegia rates. We have shown in a review of hundreds of TAAA resections that there is no unique SA whose interruption results in cord ischemia [1, 2]. Lazorthes et al. were among the first to question the idea of a single dominant artery, and they described the importance of additional inflow into the spinal cord circulation provided by the subclavian and hypogastric arteries [3–5]. The occlusion of a large number of segmental arteries when replacing a long segment of the aorta by open or endovascular means results in immediate loss of blood flow to the cord through intercostal and lumbar arteries, and this immediate ischemia results in recruitment and development of additional sources.
Pathophysiology
Serial examination of spinal cord blood flow (SCBF ) using fluorescent microspheres in experimental pig studies has shown that the lowest flow occurs within 5 h after extensive SA ligation, at a time when sham-operated pigs demonstrate hyperemia. Pigs that recover from SA ligation with normal hind limb function show a return to baseline SCBF at the 5-h time point, whereas those that suffer paraplegia do not reach baseline until 72 h after SA sacrifice (Fig. 7.2) [6].
Spinal cord blood flow (SCBF ) drops after sacrifice of all thoracoabdominal segmental arteries and returns to baseline 5 h after the operation in pigs that recover without impairment of hind limb function. In paraparetic pigs, it takes up to 72 h to return to baseline levels. By permission of Mayo Foundation for Medical Education and Research. All rights reserved
Monitoring of the actual spinal cord perfusion pressure (SCPP ) via a catheter inserted in the stump of a ligated SA confirms that the most severe drop in pressure occurs also at 5 h, with recovery even in paraplegic animals by 72 h (Fig. 7.3). In patients as in pigs, SCPP is a fraction of mean arterial pressure (MAP ): in hypertensive patients, MAP must be maintained at preoperative levels during and after operation in order to avoid spinal cord ischemic injury [7, 8].
The explanation for the physiological patterns of spinal cord perfusion after sacrifice of SAs has been provided by several anatomic studies. The blood supply to the spinal cord is part of an extensive network of vessels within and surrounding the cord and the vertebrae, extending into the paraspinous muscles, which is interconnected with major arteries: the subclavian, hypogastric, and internal thoracic. The most surprising finding of our initial anatomic studies—carried out using acrylic casts of the vascular system in the pig—is the dominance of the vasculature of the paraspinal muscles over the much less extensive arterial supply of the spinal cord (Fig. 7.4) [9].
Casting of the vasculature using acrylic resin revealed a dense network within the paraspinous muscles. Reprinted from The Journal of Thoracic and Cardiovascular Surgery, 141(4), Etz CD, Kari FA, Mueller CS, Silovitz D, Brenner RM, Lin HM, et al., The collateral network concept: a reassessment of the anatomy of spinal cord perfusion, 1020–8, Copyright 2011, with permission from Elsevier
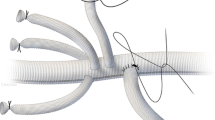
There are multiple longitudinal interconnections between the blood supply of the muscles, an extensive epidural system, and the anterior spinal artery, with numerous anastomoses at every thoracic and lumbar level between these various components of the network. A reconstruction based on several casts of the paraspinal and intrathecal vessels is shown in Fig. 7.5 [9].
Following sacrifice of all SAs from level T4 to S1 through simulated TAAA repair in a pig model, an increase in the diameter of the ASA can be seen already at 24 h after operation. By 48 h and especially 120 h, there is also a significant increase in the volume and diameter of the epidural arteries, and evidence of proliferation of small arterioles within the muscles surrounding the cord as well as enlargement of those which were present before SA ligation [1, 9].
The proliferation of small vessels as well as enlargement of major collateral arteries after SA ligation has been confirmed by studies using a barium latex infusion viewed by means of CT scanning [1]. One of the most striking findings is the extensive anterior-posterior collateralization, which develops between the internal thoracic and intercostal arteries. The dramatic proliferation of the network is easily appreciated visually, and can be confirmed by morphometric studies. Figure 7.6 shows a native pig compared with a pig 24 h and 5 days after complete SA ligation. The latex-barium method permits analysis of the vessels in situ, in contrast with the need for digestion of the tissue around the acrylic vascular cast, a process, which destroys many small and fragile vessels.
High-resolution CT scans of a native pig, and pigs 48 and 120 h after complete SA sacrifice (simulated TAAA repair ). It can easily be appreciated that a dense network of collaterals develops, and that an increase in vessel diameter occurs as early as 48 h after the operation. Reprinted from The Journal of Thoracic and Cardiovascular Surgery, 144(6), Geisbusch S, Schray D, Bischoff S, Lin HM, Griepp RB, Di Luozzo G, Imaging of vascular remodeling after simulated thoracoabdominal aneurysm repair, 1471–8, Copyright 2012, with permission from Elsevier
Histological findings have made it clear that necrosis of the spinal cord neurons is most prominently seen in the lower thoracic region (T9-T13), the part of the cord where input from cranial and caudal sources is limited when direct blood flow through SAs is interrupted (Fig. 7.7) [10].
In experimental studies, the ischemic damage within the spinal cord was graded on an 8-point scale after complete SA sacrifice from T4–S1. Necrosis was most prominently seen from T9 to T13, the region farthest away from supportive cranial and caudal input when direct inflow is interrupted. By permission of Mayo Foundation for Medical Education and Research. All rights reserved
After simulated TAAA repair in experimental models, there is also a striking reorientation of vessels within the musculature, from a random pattern (top) to one more parallel to the cranio-caudal axis (bottom), suggesting that this is a mechanism to augment flow along the longitudinal axis and provide both cranial and caudal input to the central region of a spinal cord which has been deprived of its direct blood supply (Fig. 7.8) [11].
The reorientation of the smallest vessels within the collateral network, most likely to direct flow to the central region of the cord. Reprinted from The Journal of Thoracic and Cardiovascular Surgery, 141(4), Etz CD, Kari FA, Mueller CS, Brenner RM, Lin HM, Griepp RB, The collateral network concept: remodeling of the arterial collateral network after experimental segmental artery sacrifice, 1029–36, Copyright 2011, with permission from Elsevier
The Impact of the Collateral Network on Endovascular Repair
Although its incidence is gradually diminishing, paraplegia following repair of aortic aneurysms is a formidable complication and continues to be disturbingly high even in the hands of experts, especially in cases where the aneurysm spans most of the thoracic and thoracoabdominal aorta. The number of SAs to be sacrificed during an operation—equivalent to the extent of the aneurysm—and the presence of additional compromise of input resulting from previous or concomitant occlusion of the subclavian or hypogastric arteries are the major factors in assessing the risk of paraplegia or paraparesis [12–14]. Current surgical strategies to reduce the risk of cord ischemia include reimplantation of SAs and use of cardiopulmonary bypass to increase intraoperative flow, and deep hypothermia to decrease the nutritional demand of the spinal cord, but these techniques are of limited relevance in endovascular repair, where intraoperative cord ischemia is much less of a problem. Other surgical adjuncts, such as drainage of cerebrospinal fluid (CSF) and maintenance of mean arterial pressure (MAP ) at high normal levels, are part of the routine perioperative management in both surgical and endovascular repair to assure adequate SCPP . In addition, monitoring tools such as motor-evoked potentials (MEPs) or somatosensory-evoked potentials (SSEPs ) help to immediately detect changes and adjust treatment in anaesthetized patients, but are not feasible once they awaken, making us rely on clinical assessments of spinal cord function.
The impact of the collateral network on recovery from endovascular aortic repair becomes apparent when we look at results of clinical as well as experimental studies in which extensive aortic replacement has been carried out in two stages. There is an undeniable decrease in the incidence of postoperative paraplegia after staged repair [15–17], notwithstanding the ongoing controversy over the impact of previous aortic repair as a risk factor for paraplegia: the detrimental effect of previous surgery may well be a consequence of hypogastric or subclavian artery sacrifice. Experiments in which various numbers of SAs T4–S1 were sacrificed have shown that the incidence of spinal cord ischemia corresponds to the number of sacrificed vessels. Further studies have shown that pigs in which the subclavian and/or the hypogastric arteries had been ligated prior to SA sacrifice had a worse outcome than those in which these other sources of blood flow were intact: in the absence of an intact subclavian or hypogastric blood supply, fewer SAs could be sacrificed without spinal cord injury [18].
Taking into account what we have learned about spinal cord anatomy and physiology, it is likely that the first step of a two-stage procedure provides an ischemic stimulus which stimulates the collateral network to develop small new vessels (angiogenesis ) and to transform existing small vessels into larger ones (arteriogenesis) and to reorient them. All of these changes serve to augment spinal cord blood flow to compensate for diminished direct SA input. Patients in whom recruitment of collateral input sources is compromised by previous occlusion of subclavian or hypogastric vessels are therefore at higher risk of spinal cord ischemia following SA sacrifice during aneurysm repair.
With constant improvement of endovascular strategies including fenestrated and branched stent grafts, innovative concepts to prevent spinal cord ischemia after complete endovascular repair have been developed, with the idea of promoting enhancement of the collateral network before occlusion of all segmental vessels. First published in 2010, temporary aneurysm sac perfusion (TASP ) after branched thoracic endovascular aortic repair (bEVAR) is a technique which involves leaving two or more branches open at the time of initial repair, and performing side branch completion in a second stage procedure days to weeks later. TASP has shown promising results in a case report and two series of 10 and 40 patients [19–22]. Although spinal cord perfusion is dramatically reduced by implanting a thoracoabdominal stent graft, leaving some branches open seems to assure sufficient cord perfusion until the collaterals have had time to develop, while placing the stent graft immediately reduces the risk of rupture by minimizing flow into the aneurysm sac.
Endovascular occlusion of a number of SAs prior to simulated TAAA repair has shown excellent results in an experimental study: no paraplegia in pigs that had coil occlusion of two or more SAs 1 week prior to sacrifice of all SAs, in contrast to a 60 % rate of spinal cord injury in controls without pretreatment [10]. The first clinical cases report successful application in patients at high risk [23]. Coiling of a few SAs seems to stimulate collateral development prior to subsequent simulated TAAA endovascular repair in healthy pigs without being harmful to spinal cord integrity: histologic ischemic damage, quantified as necrosis of grey and white matter, was significantly reduced after preparatory coiling (p = 0.001) (Fig. 7.9).
As opposed to the pattern of spinal cord necrosis after simulated TAAA repair (blue bars), the extent of ischemic cell damage is marginal in the T9-T13 region after coiling of two or more SAs in this region of the cord (red bars), p = 0.001. The ischemic stimulus likely activates the dilatation of existing vessels and the development of small new vessels that compensate for the loss of inflow after subsequent TAAA repair [10]. By permission of Mayo Foundation for Medical Education and Research. All rights reserved
TASP and coiling of SAs seem to have real potential clinical utility, although some issues pose concerns. In patients with degenerative aneurysms, some of the SAs may already be occluded by thrombus, and so the coiling of additional arteries could then itself lead to spinal cord ischemia [19]. Test balloon occlusion in the awake patient may be a way of dealing with this problem: in the absence of neurological symptoms, permanent coils could be placed, or implantation of the branch to complete bEVAR could be performed. In addition, catheter manipulation during the coiling procedure carries a risk of atheroembolization from plaque and mural thrombus and should be performed by an experienced interventionalist or surgeon. The imaging of patent intercostal arteries and thrombus formation by angiography, CT or MRI is a helpful tool in planning the procedure [24, 25].
Revascularization of the left subclavian artery via a bypass graft should be considered in each patient in whom coverage of the artery with a stent graft is inevitable, and when additional risk factors—such as previous aortic repair with sacrifice of the hypogastric artery—are present.
Finally, it should be pointed out that some patients are not eligible for a two-stage procedure, TASP or coiling: those with symptoms or imminent rupture, rapid aneurysm progression over a short period of time, or large aneurysm diameters. For these patients, the risk of paraplegia with extensive aneurysm repair remains high, and should be minimized using careful monitoring and supportive adjuncts during the first few days following the endovascular procedure.
In summary, minimally invasive endovascular repair of complex extensive aortic pathologies still carries a high risk of postoperative paraplegia, but innovative endovascular strategies in combination with currently accepted management may improve outcome and reduce paraplegia to a rare complication.
References
Geisbusch S, Schray D, Bischoff S, Lin HM, Griepp RB, Di Luozzo G. Imaging of vascular remodeling after simulated thoracoabdominal aneurysm repair. J Thorac Cardiovasc Surg. 2012;144(6):1471–8 [Research Support, N.I.H., Extramural].
Etz CD, Halstead JC, Spielvogel D, Shahani R, Lazala R, Homann TM, et al. Thoracic and thoracoabdominal aneurysm repair: is reimplantation of spinal cord arteries a waste of time? Ann Thorac Surg. 2006;82(5):1670–7.
Lazorthes G, Gouaze A, Zadeh JO, Santini JJ, Lazorthes Y, Burdin P. Arterial vascularization of the spinal cord. Recent studies of the anastomotic substitution pathways. J Neurosurg. 1971;35(3):253–62 [Review].
Lazorthes G, Poulhes J, Bastide G, Roulleau J, Chancholle AR. [Research on the arterial vascularization of the medulla; applications to medullary pathology]. Bull Acad Natl Med. 1957;141(21–23):464–77.
Lazorthes G, Poulhes J, Bastide G, Roulleau J, Chancholle AR. Arterial vascularization of the spine; anatomic research and applications in pathology of the spinal cord and aorta. Neurochirurgie. 1958;4(1):3–19.
Etz CD, Homann TM, Luehr M, Kari FA, Weisz DJ, Kleinman G, et al. Spinal cord blood flow and ischemic injury after experimental sacrifice of thoracic and abdominal segmental arteries. Eur J Cardiothorac Surg. 2008;33(6):1030–8.
Etz CD, Zoli S, Bischoff MS, Bodian C, Di Luozzo G, Griepp RB. Measuring the collateral network pressure to minimize paraplegia risk in thoracoabdominal aneurysm resection. J Thorac Cardiovasc Surg. 2010;140(6 Suppl):S125–30. [Research Support, N.I.H., Extramural]; discussion S42–S46.
Etz CD, Di Luozzo G, Zoli S, Lazala R, Plestis KA, Bodian CA, et al. Direct spinal cord perfusion pressure monitoring in extensive distal aortic aneurysm repair. Ann Thorac Surg. 2009;87(6):1764–73; discussion 73–4.
Etz CD, Kari FA, Mueller CS, Silovitz D, Brenner RM, Lin HM, et al. The collateral network concept: a reassessment of the anatomy of spinal cord perfusion. J Thorac Cardiovasc Surg. 2011;141(4):1020–8 [Research Support, N.I.H., Extramural].
Geisbusch S, Stefanovic A, Koruth JS, Lin HM, Morgello S, Weisz DJ, et al. Endovascular coil embolization of segmental arteries prevents paraplegia after subsequent thoracoabdominal aneurysm repair: an experimental model. J Thorac Cardiovasc Surg. 2014;147(1):220–6 [Research Support, N.I.H., Extramural].
Etz CD, Kari FA, Mueller CS, Brenner RM, Lin HM, Griepp RB. The collateral network concept: remodeling of the arterial collateral network after experimental segmental artery sacrifice. J Thorac Cardiovasc Surg. 2011;141(4):1029–36 [Research Support, N.I.H., Extramural].
Czerny M, Eggebrecht H, Sodeck G, Verzini F, Cao P, Maritati G, et al. Mechanisms of symptomatic spinal cord ischemia after TEVAR: insights from the European Registry of Endovascular Aortic Repair Complications (EuREC). J Endovasc Ther. 2012;19(1):37–43 [Multicenter Study].
Eagleton MJ, Shah S, Petkosevek D, Mastracci TM, Greenberg RK. Hypogastric and subclavian artery patency affects onset and recovery of spinal cord ischemia associated with aortic endografting. J Vasc Surg. 2014;59(1):89–94 [Clinical Trial Research Support, Non-U.S. Gov’t].
Zoli S, Roder F, Etz CD, Brenner RM, Bodian CA, Lin HM, et al. Predicting the risk of paraplegia after thoracic and thoracoabdominal aneurysm repair. Ann Thorac Surg. 2010;90(4):1237–44; discussion 45.
Zoli S, Etz CD, Roder F, Brenner RM, Bodian CA, Kleinman G, et al. Experimental two-stage simulated repair of extensive thoracoabdominal aneurysms reduces paraplegia risk. Ann Thorac Surg. 2010;90(3):722–9.
Etz CD, Zoli S, Mueller CS, Bodian CA, Di Luozzo G, Lazala R, et al. Staged repair significantly reduces paraplegia rate after extensive thoracoabdominal aortic aneurysm repair. J Thorac Cardiovasc Surg. 2010;139(6):1464–72.
Bischoff MS, Scheumann J, Brenner RM, Ladage D, Bodian CA, Kleinman G, et al. Staged approach prevents spinal cord injury in hybrid surgical-endovascular thoracoabdominal aortic aneurysm repair: an experimental model. Ann Thorac Surg. 2011;92(1):138–46. [Comparative Study Research Support, N.I.H., Extramural]; discussion 46.
Strauch JT, Spielvogel D, Lauten A, Zhang N, Shiang H, Weisz D, et al. Importance of extrasegmental vessels for spinal cord blood supply in a chronic porcine model. Eur J Cardiothorac Surg. 2003;24(5):817–24.
Harrison SC, Agu O, Harris PL, Ivancev K. Elective sac perfusion to reduce the risk of neurologic events following endovascular repair of thoracoabdominal aneurysms. J Vasc Surg. 2012;55(4):1202–5.
Kasprzak PM, Gallis K, Cucuruz B, Pfister K, Janotta M, Kopp R. Editor’s choice—temporary aneurysm sac perfusion as an adjunct for prevention of spinal cord ischemia after branched endovascular repair of thoracoabdominal aneurysms. Eur J Vasc Endovasc Surg. 2014;48(3):258–65.
Lioupis C, Corriveau MM, Mackenzie KS, Obrand DI, Steinmetz OK, Ivancev K, et al. Paraplegia prevention branches: a new adjunct for preventing or treating spinal cord injury after endovascular repair of thoracoabdominal aneurysms. J Vasc Surg. 2011;54(1):252–7 [Case Reports].
Reilly LM, Chuter TA. Reversal of fortune: induced endoleak to resolve neurological deficit after endovascular repair of thoracoabdominal aortic aneurysm. J Endovasc Ther. 2010;17(1):21–9 [Case Reports Research Support, Non-U.S. Gov’t].
Etz CD, Debus ES, Mohr FW, Kolbel T. First-in-man endovascular preconditioning of the paraspinal collateral network by segmental artery coil embolization to prevent ischemic spinal cord injury. J Thorac Cardiovasc Surg. 2015;149(4):1074–9.
Schurink GW, Nijenhuis RJ, Backes WH, Mess W, de Haan MW, Mochtar B, et al. Assessment of spinal cord circulation and function in endovascular treatment of thoracic aortic aneurysms. Ann Thorac Surg. 2007;83(2):S877–81; discussion S90–2.
Williams GM, Roseborough GS, Webb TH, Perler BA, Krosnick T. Preoperative selective intercostal angiography in patients undergoing thoracoabdominal aneurysm repair. J Vasc Surg. 2004;39(2):314–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Mayo Foundation for Medical Education and Research
About this chapter
Cite this chapter
Geisbüsch, S., Di Luozzo, G., Griepp, E.B., Griepp, R.B. (2017). The Spinal Cord Collateral Network: Implications for Endovascular Aortic Repair. In: Oderich, G. (eds) Endovascular Aortic Repair. Springer, Cham. https://doi.org/10.1007/978-3-319-15192-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-15192-2_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-15191-5
Online ISBN: 978-3-319-15192-2
eBook Packages: MedicineMedicine (R0)