Abstract
Overnutrition characterized by overconsumption of food rich in fat and carbohydrates is a significant contributor to hypertension, type 2 diabetes, and the cardiorenal syndrome (CRS). Obesity, insulin resistance, and diabetes mellitus are associated with a substantially increased prevalence of arterial disease (AD), which is involved in the risk of coronary, cerebral, and peripheral atherosclerosis and the clinical consequences of myocardial infarction, stroke, limb ischemia, and death. Although the underlying mechanisms and mediators of AD are not well understood, accumulating evidence supports the role of dysregulation of VSMCs, ECs, and vascular extracellular matrix in pathogenesis of AD. Risk factors related to CRS and misregulation of adaptive metabolic responses develop a complex network and contribute to the progression of AD. In this review, we will focus on the interaction of metabolic risk factors, adaptive metabolic response, and AD, highlighting pathophysiology and molecular mechanisms, as well as the contemporary understanding of potential therapeutic strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cardiorenal metabolic syndrome
- Arterial disease
- Insulin resistance
- Vascular smooth muscle cells
- Endothelial cells
- Extracellular matrix
1 Introduction
The main cause of arterial disease (AD) is hardening of the arteries or atherosclerosis due to a thickening of the artery lining from fatty deposits or plaques. There are several different symptoms, depending on the location of the AD. It most commonly affects the arteries in the heart, brain, and legs [1]. Diabetes is associated with a two- to fourfold increase in the risk of developing coronary artery disease (CAD). Diabetic patients presenting with unstable angina are more likely to develop myocardial infarction. The mortality caused by myocardial infarction in diabetic patients is more than in nondiabetic individuals [2]. Similarly, diabetes increases the risk of stroke and stroke-related mortality [3]. Meanwhile, diabetes is a major risk factor for the development of peripheral arterial disease, which is typically caused by progressive narrowing of the arteries in the lower extremities [4]. Thus, AD is the major cause of mortality and significant morbidity in diabetes and cardiorenal metabolic syndrome (CRS).
Epidemiologic evidence supports the hypothesis that diabetes adds to the impact of individual risk factors, such as hypertension and hyperlipidemia, for the prediction of excess AD [3]. It was suggested that integrative effects of elevated glucose, insulin, and triglycerides may have a considerable impact on AD and play an important role in the early pathophysiology of AD in patients with type 2 diabetes [5]. In individuals with the CRS and those with clinical diabetes, AD has been observed in all age groups, including children. Indeed, obese children prematurely manifest signs of AD [6]. In individuals 40 years and older, multiple logistic and linear regression analyses from a total of 2,188 individuals demonstrated that AD was independently associated with insulin resistance (IR) in middle-aged adults [7]. In elderly people without diabetes mellitus, the Rotterdam study found that impaired fasting glucose was associated with increased AD [8]. Therefore, glycemic control, low-density cholesterol-lowering therapy, blood pressure lowering, and comprehensive approaches targeting multiple metabolic risk factors to reduce cardiovascular risk may therefore account for the clinical beneficial effects in obese and diabetic patients with AD. In the present review, we will discuss the roles of metabolic factors in the pathogenesis of AD and provide a better understanding of potential therapeutic strategies.
2 Risk Factors for AD in CRS
Several metabolic risk factors such as hyperglycemia, IR, dyslipidemia, obesity, fructose, and uric acid may initiate and accelerate artery impairment (Fig. 8.1).
Proposed the interaction of metabolic risk factors, adaptive metabolic response, and AD in CRS. Risk factors for AD such as hyperglycemia, insulin resistance, dyslipidemia, fructose, and uric acid induce the adaptive metabolic responses including mitochondria dysfunction, ROS, inflammation response, sympathetic activity, RAAS, PTH, and TG2, resulting in the pathophysiological abnormalities in ECs, VSMCs, and extracellular matrix on CRS. Abbreviations: AD arterial disease, RAAS renin–angiotensin–aldosterone system, PTH Parathyroid hormone, AGE advanced glycation end products, TG2 tissue transglutaminase, ROS reactive oxygen species, IL interleukin, TNF tumor necrosis factor, NO nitric oxide, ONOO – peroxynitrite, ET-1 endothelin-1, Ang II angiotensin II, TxA2 thromboxane A2, MCP-1 monocyte chemotactic protein-1, CRP C-reactive protein, MMP matrix metalloproteinase
2.1 Hyperglycemia and IR
Hyperglycemia, a hallmark of diabetes, has been implicated in the development of vascular cell dysfunction including vascular smooth muscle cells (VSMCs) and endothelial cells (ECs) via mechanisms of protein kinase C (PKC) activation, activation of the hexosamine, and advanced glycation end products (AGEs). These pathways are believed to mediate vascular dysfunction through the unifying mechanism of reactive oxygen species (ROS) overproduction, most notably increases in O2 − [9]. Studies have also shown that elevated glucose concentration may activate the tissue renin–angiotensin–aldosterone system (RAAS), and this plays an important role in the pathogenesis of vascular complications of diabetes [10, 11]. In vivo exposure of healthy human subjects to an acute glucose load leads to attenuated endothelium-dependent vascular relaxation [12]. This impaired endothelial relaxation is associated with increased oxidative stress, adhesion molecule expression, vascular permeability, and plasma levels of plasminogen activator inhibitor-1 [12]. In vitro, both high glucose and angiotensin II (Ang II) induced a progressive increase in Ang II receptor type 1 receptor 1 (AT-1R) expression on the cultured human ECs. Furthermore, high glucose enhanced Ang II-mediated peroxisome proliferation-activated receptor-γ inactivation and expression of pro-inflammatory adhesion molecules via signaling through the AT-1R [13]. With chronic exposure to elevated plasma glucose, the resulting glucotoxicity may activate mitogen-activated protein kinase (MAPK) thus increasing secretion of inflammatory cytokines and inhibiting phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt) signaling leading to reduced nitric oxide (NO) production and endothelial dysfunction [13].
IR, a metabolic risk factor in patients with normal glucose tolerance and even after adjustment for known risk factor such as low-density lipoprotein (LDL), triglycerides (TG), high-density lipoprotein cholesterol (HDL), and systolic blood pressure, is frequently present in obesity, hypertension, dyslipidemia, and AD [14]. In nonobese subjects without diabetes, IR predicted the development of cardiovascular disease (CVD) independently of other known risk factors. In another group of subjects without diabetes or impaired glucose tolerance, patients with IR had a 2.5-fold increase in CVD risk. These data indicate that IR itself promotes atherogenesis [15]. Our study has found that abnormal insulin metabolic signaling is an important contributor to AD. In this regard, IR is typically accompanied by reduced PI3K-NO pathway and heightened MAPK-endothelin-1 (ET-1) pathway [16].
2.2 Dyslipidemia and Obesity
Lipid abnormalities play an important part in raising the cardiovascular risk in patients with diabetes. The main components of diabetic dyslipidemia are increased plasma TG, low concentration of HDL, preponderance of small dense LDL, and excessive postprandial lipemia [17]. Small, dense LDL, the elevation in remnant TG-rich lipoprotein particles, and the low HDL are the most powerful atherogenic components. The coexistence of these factors strongly aggravates the lipid accumulation in the arterial wall and the formation of atherosclerotic plaques. Small, dense LDL particles are held to be more atherogenic than their larger, buoyant counterparts because they are more liable to oxidation and may more readily adhere to and subsequently invade the arterial wall. The atherogenicity of LDL may also be enhanced by nonenzymatic glycation [18]. Thus, the benefits of statin therapy in type 2 diabetics can no longer be questioned.
Obesity has a strong association with atherogenic dyslipidemia. In a large series of 26,000 overweight children, concentrations of one or more of the lipids were abnormal in 32 %, total cholesterol in 14.1 %, LDL-C in 15.8 %, HDL-C in 11.1 %, and TG in 14.3 % of those in whom data were available [19]. Indeed, overweight and obesity are associated with development of CRS which is a constellation of risk factors, such as IR, dyslipidemia, and high blood pressure [16]. The development of AD in obese patients can be attributed to a number of factors including pro-inflammatory cytokines, inappropriate activation of RAAS, vasoconstriction from increased sympathetic nervous system (SNS) activation, and dysregulation in adipokine production and secretion [20]. These data suggest that obesity and dyslipidemia are involved in AD in CRS.
2.3 Fructose and Uric Acid
The increasing fructose consumption has led to a rise in obesity from 13 to 34 % since 1960 and the subsequent rise in diagnosed type 2 diabetes from 5 to 8 % since 1988 [21]. In children, the intake of artificially sweetened beverages was found to be positively associated with adiposity [22]. A prospective cohort analyses of nondiabetic women in the Nurses’ Health Study II concluded that higher consumption of sugar-sweetened beverages is associated with greater magnitude of weight gain and an increased risk for the development of type 2 diabetes [22]. In the Framingham Heart Study, the relationship between soft drink consumption and cardiovascular risk factors was evaluated in 6,039 participants; consumption of more than one can of soft drink per day was significantly associated with the prevalence of CRS [23]. Thus, fructose has been implicated in promoting obesity and CRS by altering appetite, inducing leptin resistance, and resulting in increased food intake. Recently, The Third National Health and Nutrition Examination Survey (NHANES III) report has indicated that consumption of sugar-sweetened beverages is significantly associated with plasma uric acid concentrations [23]. Thus, a novel hypothesis has been proposing to link fructose intake, hyperuricemia, and AD in CRS.
3 EC Dysfunction Initiates AD
Forming a vast interface between blood and surrounding tissues, the endothelium forms a monolayer comprising the innermost lining of blood vessels. The arterial endothelium provides a continuous barrier between the elements of blood and the arterial wall and is a critical component to vascular homeostasis, actively responding to biochemical and physical stimuli through the release of a diverse set of vasoactive substances [24]. Endothelial damage and thickening of the intima-media layers induced by risk factors we discussed above are early events in the AD process. For example, LDL particles invade the endothelium and become oxidized, creating risk for a subsequent inflammatory response and ultimately CVD. Monocytes enter the artery wall from the bloodstream with platelets adhering to the area of insult, differentiate into macrophages, and eventually form foam cells. Foam cells die and further propagate the inflammatory process [25] (Fig. 8.1).
NO, a most significant endothelium-derived mediator, plays multiple roles in preventing AD. NO diffuses into neighboring VSMCs, activating guanylyl cyclase and producing cyclic guanosine monophosphate (cGMP) and activating kinases responsible for vascular relaxation [16]. NO also inhibits platelet aggregation, smooth muscle cell proliferation, and nuclear transcription of leukocyte-adhesion molecules including vascular cell adhesion molecule (VCAM) and intercellular adhesion molecule (ICAM) [9]. Indeed, vascular homeostasis is tightly controlled by EC secreting the vasodilatory substances, such as NO, endothelium-derived hyperpolarizing factor (EDHF), prostacyclin (PGI2), and vasoconstrictory substances, such as ET-1, Ang II, and thromboxane A2 (TxA2) [26]. These EC-secreting vasoactivity substances have been proposed to mediate the AD in CRS, including continued activation of the SNS; increased production and activity of vasoconstrictors, such as ET-1, Ang II, and TxA2; and impaired endothelium-dependent relaxation [27]. Thus, endothelial dysfunction has been suggested as a common underlying mechanism in AD with IR, hyperinsulinemia, and CRS.
4 Dysregulation of VSMCs and Vascular Extracellular Matrix Promotes AD
Following the EC dysfunction, the metabolic abnormalities that characterize diabetes, hyperglycemia, free fatty acids, and IR provoke the impairment of the function and structures in blood vessels include VSMC and extracellular vascular matrix (Fig. 8.1).
4.1 VSMC Dysfunction
The impact of CRS on vascular function is not only limited to the ECs but also to VSMCs, which are the predominant cell type found in the arterial wall and are essential for the structural and functional integrity of the vessel. Diabetes increases PKC activity, NF-kappaB (NF-κΒ) production, and generation of oxygen-derived free radicals in VSMCs and heightens migration of VSMCs into atherosclerotic lesions, where they replicate and produce extracellular matrix—important steps in mature lesion formation [28]. Dysregulation of VSMC function is exacerbated by impairments in SNS function. Studies from the Zucker obese insulin-resistant rat have shown that VSMCs from these rats manifested greater concentrations of ROS and impaired activation of the NO/cGMP/protein kinase G (PKG) pathway when compared to VSMC from the lean, insulin-sensitive Zucker rats [29]. Our recent data also showed excessive serine phosphorylation of insulin receptor substrate (IRS-1) as a key mechanism underlying cellular IR in VSMCs. Furthermore, after treatment with aldosterone or Ang II, VSMCs show increased activation of p70 S6 kinase 1 signaling pathway, increased proteasome degradation of IRS-1, and attenuated insulin-induced Akt phosphorylation and glucose uptake [30]. These observations provide a biochemical basis to the IR in VSMCs in the development of AD.
4.2 VSMC Calcification
Studies conducted in the United States have revealed that calcium deposits in arterial walls are reported in nearly 30 % of Americans over 45 years of age [31]. Vascular calcification risk factors are similar to those of atherosclerosis including hypertriglyceridemia, increased LDL, decreased HDL, obesity, and hypertension. It has also been shown that diabetes and renal failure contribute significantly to higher risk of accumulation of calcium depositions in the vessel wall [32]. Calcification of vessels reduces their elasticity, affecting hemodynamic parameters of the cardiovascular system. Vascular calcification is an active and complex process that involves numerous mechanisms responsible for calcium deposits in arterial walls. They lead to an increase in arterial stiffness and in pulse wave velocity, which in turn increases CVD morbidity and mortality. We have known that VSMCs can differentiate from a quiescent, contractile phenotype to a proliferative, synthetic phenotype following arterial injury and in atherosclerotic diseases [33]. Indeed, VSMCs are capable of osteoblast transdifferentiation in calcifying arteries [34]. Epidemiological data have shown that higher insulin levels in diabetes can independently predicate arterial calcification [35]. The mechanisms of insulin involved in arterial calcification in these clinical settings are still controversial. Furthermore, it has been demonstrated that insulin enhances the calcification of VSMCs in vitro [36]. In this regard, insulin promotes alkaline phosphatase activity, osteocalcin expression, and the formation of mineralized nodules in VSMCs by increased receptor expression of NF-κB ligand (RANKL) through extracellular signal-regulated protein kinases 1 and 2 (Erk ½) activation [37]. However, others suggest that insulin attenuated VSMC calcification induced by high phosphate conditions [38]. These contradictory results may be explained by different cell types or different experimental conditions.
4.3 Elastin, Collagen, and Advanced Glycation End Products
Elastin is the most abundant protein in the walls of the arteries, which are subjected to pulsatile pressure generated by cardiac contraction. Matrix metalloproteinases (MMPs) have an important role in the degradation of elastin [39]. Recently, it was reported that in the arterial vasculature from chronic kidney disease patients, the presence of diabetes markedly upregulated MMP-2 and -9, and this adaption is strongly associated with elastic fiber degradation and AD. The increase in MMPs in diabetic vessels was also accompanied by pronounced generation of angiostatin, and the reduction of microvascular density was associated with impaired vasorelaxation [40]. In addition, the degradation of elastin also induces the overexpression of transforming growth factor beta (TGF-β). TGF-β1 not only plays an important role in osteoblast differentiation but also accelerates the calcification of VSMCs [39]. Meanwhile, hyperglycemia may cause changes in the type or structure of elastin and/or collagen in the arterial wall through nonenzymatic glycosylation of proteins that generate AGE. AGE may form irreversible cross-links between long-lived proteins such as collagen, leading to accumulation of stiffer molecules that are less susceptible to hydrolytic turnover [41]. These data confirm that the interaction among MMPs, elastin, collagen, and AGE plays a key role in the development of AD with CRS.
5 Misregulation of Adaptive Metabolic Responses Aggravate to the Progression of AD
Misregulation of an adaptive metabolic response contributes to the risk factors related CRS and dysfunction of ECs, VSMCs, and extracellular vascular matrix in AD (Fig. 8.1).
5.1 Mitochondria Dysfunction and ROS
Mitochondria are essential for intermediary metabolism as well as energy production and normally provide more than 90 % of the cellular energy [42]. It has been established that mitochondrial respiratory chain function is responsible for energy metabolism and adenosine triphosphate (ATP) production through the tricarboxylic acid (TCA) cycle, coupling of oxidative phosphorylation (OXPHOS), and electron transfer [43]. Mitochondria dysfunction is recognized as playing a central role in the development of various abnormalities, including disturbed glucose homeostasis, IR, abdominal fat accumulation, dyslipidemia, hypertension, and associated cardiac and renal pathology. ROS production occurs mainly at complex I and complex III in mitochondria [44]. Under conditions of glucose and fatty acid overnutrition, nutrient overflow into cells prompts electrons transferring to oxygen without ATP production and further favors a state of increased ROS, which potentially leads to oxidative damage within mitochondria [45]. Therefore, ROS generated from mitochondria damages proteins, DNA, and lipid in membrane components, which result in mitochondrial dysfunction. Although this review is concerned with mitochondrial ROS, it should be recognized that the considerable amount of ROS is derived from outside of mitochondria, such as oxygen radicals from peroxisomal β-oxidation of fatty acids, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, xanthine oxidase, arachidonic acid metabolism, microsomal P-450 enzymes, and prooxidant heme molecule [46].
5.2 Adaptive Immunity and Inflammation Response
Atherosclerosis is a chronic inflammatory disease of the arterial wall characterized by an innate and adaptive immune system, which is composed of diverse cellular components including granulocytes, mast cells, monocytes, macrophages, dendritic cells (DCs), and natural killer cells [47]. Upon activation, partly in response to immunological stimuli from the local microenvironment as well as systemic circulation, macrophages polarize into classical (M1) or alternative (M2) phenotypes [48]. M1 macrophages are found in advanced lesions where they accumulate a large amount of lipids, which promotes their differentiation into foam cells. Meanwhile, M1 macrophages secrete tumor necrosis factor alpha (TNF-α), interleukin (IL)-6, and metalloproteinases, which exacerbate and destabilize lesion development. However, M2 macrophages predominate in the early stages of atherosclerosis and are characterized by IL-10 secretion and smaller amounts of accumulated lipids; these events are atheroprotective and can reduce plaque development [49].
DC precursors or monocytes are recruited to lesions where they differentiate into DCs. The DC population is heterogeneous and can be divided into four major categories: conventional DCs (cDCs), plasmacytoid DCs (pDCs), monocyte-derived DCs, and Langerhans cells [50]. DC accumulation in regions prone to AD suggests that their recruitment accounts for an initial inflammatory or immune activation. The exact localization and origin of vascular DCs, however, is still under debate [51]. In general, immature and semimature DCs uptake lipids and other intimal antigens, thus preventing them from eliciting pro-inflammatory signaling in other artery wall cells. Toll-like receptor (TLR) ligation by ligands such as oxLDL induces DC maturation. Under hyperlipidemic conditions, lipid uptake and efferocytosis likely lead to DC-foam cell formation, and mature DCs and foam cells emigrate from the vessel wall in a C-C chemokine receptor type 7 (CCR7)-dependent manner, clearing inflammatory cells, lipids, and apoptotic cell debris from the intimal space and preventing necrosis and persistent inflammation. Mature CD11b+ DCs likely expand regulatory T cells (Tregs) and CD4+ effector T cells within the artery wall [52]. CD4+CD25+Foxp3+ Tregs can protect the pro-inflammatory activation of vascular cells. The mechanisms by which Tregs protect against inflammation are thought to be mediated, at least in part, by directing cell-to-cell interactions as well as through the secretion of soluble anti-inflammatory cytokines, including IL-10 TGF-β [53]. Thus, further studies are required to understand the role of adaptive immunity and inflammation response in AD with CRS.
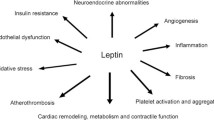
5.3 Sympathetic Activity
The role of increased SNS activity in IR with CRS is increasingly recognized. Individuals with central obesity show increased sympathetic nervous activity. Increased sympathetic outflow has been reported in obese nonhypertensive individuals with the determination of circulating catecholamines, urinary norepinephrine (NE), and muscle sympathetic nerve activity (MSNA) [54]. Multiple neurohumoral mechanisms can activate the SNS in patients with CRS including direct activation of the SNS in response to the activation of higher cerebral nuclei and renal afferent nerve activation mediated by perirenal fat accumulation and kidney compression [55]. Sympathetic activation can also be triggered by reflex mechanisms such as arterial baroreceptor impairment, psychological stress, oxidative stress, obstructive sleep apnea, inflammation, and metabolic factors and dysregulated production and secretion of adipokines from visceral fat with a particular important role of leptin [20]. Although enhanced activation of SNS is an important component in IR, it is often related to activation of RAAS since the RAAS system causes sustained sympathetic overactivity by modulating central neurons in the subfornical organ of the forebrain [49]. The link between sympathetic nervous activity and AD offers new clues to identify AD and may allow for development of novel-targeted therapeutic interventions.
5.4 Renin–Angiotensin–Aldosterone System and Parathyroid Hormone
There is evidence that RAAS activation plays an important role in the pathogenesis of AD. In the course of RAAS-induced vascular injury, Ang II binds to its type 1 receptor to induce oxidative stress, mainly mediated by NADPH oxidase. Our study has also found that Ang II increased serine phosphorylation of IRS-1 and inhibited the insulin-stimulated phosphorylation of endothelial NO synthase through activation of S6 kinase (S6K) signaling pathway [30]. Recent data also suggests that increased mineralocorticoid receptor (MR) is associated with IR. Studies have demonstrated a relationship between MR activation and decreased insulin sensitivity in animal models and humans. For example, patients with primary hyperaldosteronism were found to have IR suggesting the contribution of MR signaling to IR [56]. Spironolactone, a blocker of the MR, has been shown to decrease local inflammation and vascular stiffness in rodent models of hypertension and IR [57, 58]. These observations suggest that inhibition of MR might be a beneficial therapeutic approach for preventing AD in diet-induced obesity and IR [58]. Thus, enhanced RAAS activation may represent a link between obesity, hypertension, dyslipidemia, and IR, features present in the AD with CRS [59]. Moreover, cross-talk between Ang II and aldosterone signaling underscores the importance of Ang II–aldosterone interactions in the development of IR, vascular dysfunction, and AD.
Parathyroid hormone (PTH) is secreted from parathyroid glands and increases the concentration of calcium in the blood. Recent research suggests that PTH is implicated in regulating RAAS which is proposed to regulate PTH hormones [60]. Ang II seems to be an acute modulator of PTH, potentially through direct stimulation of PTH release via the AT-1R. In contrast, aldosterone may be involved in the modulation of PTH in the chronic setting via indirect and direct mechanisms [61]. PTH may increase sensitization towards Ang II and directly stimulate aldosterone synthesis by binding to the PTH-related protein receptor, voltage-gated calcium channels, and the adrenocorticotropic hormone receptor [62]. Therefore, the interaction of PTH and RAAS plays a key role in the pathogenesis of AD.
5.5 Tissue Transglutaminase
Tissue transglutaminase (TG2) is a multifunctional protein that plays an important role in vascular function, including remodeling of resistance vessels, increased aortic stiffness with age, and arterial calcification [63]. TG2 is a link between IR and AD because of its regulation by NO availability. A study has found that bioavailability of NO impaired by inflammation cytokines and RAAS is associated with decreased TG2 S-nitrosylation [63, 64]. Thus, increased secretion of TG2 to the cell surface and extracellular matrix and enhanced cross-linking activity in isolated endothelial, smooth muscle, and fibroblast cells resulted in AD in CRS [65]. In addition, increased vascular TG2 activity was also associated with AD in high fat-fed mice that preceded hypertension [66], thereby suggesting TG2 activation and AD as an early vent in the long-term effects of obesity on the vasculature.
6 Conclusion
AD increases the risk of developing coronary, cerebrovascular, and peripheral arterial disease and is a major cause of disability and death in patients with diabetes mellitus and CRS. The pathophysiology of AD in diabetes and CRS involves abnormalities in ECs, VSMCs, elastin, collagen, and AGE products, which increase the risk of the adverse cardiovascular events. Elucidation of mechanisms leading to the pathophysiological alterations in vasculature will enable us to specifically target therapeutic interventions since currently available cardiovascular medications fall short at reducing AD. Future therapeutic strategies should emphasize the need to achieve control of hyperglycemia, dyslipidemia, blood pressure, obesity, and cigarette smoking, in addition to exercise therapy. A better understanding of the mechanisms leading to vascular dysfunction may unmask new strategies to reduce disability and death in these patients.
References
Krentz AJ (2003) Lipoprotein abnormalities and their consequences for patients with type 2 diabetes. Diabetes Obes Metab 5:S19–S27
Lüscher TF, Creager MA, Beckman JA, Cosentino F (2003) Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Circulation 108:1655–1661
Sowers JR (2013) Diabetes mellitus and vascular disease. Hypertension 61:943–947
Jia G, Sowers JR (2014) New thoughts in an old player: role of nitrite in the treatment of ischemic revascularization. Diabetes 63:39–41
Salomaa V, Riley W, Kark JD et al (1995) Non-insulin-dependent diabetes mellitus and fasting glucose and insulin concentrations are associated with arterial stiffness indexes. The ARIC Study. Atherosclerosis Risk in Communities Study. Circulation 91:1432–1443
Tounian P, Aggoun Y, Dubern B et al (2001) Presence of increased stiffness of the common carotid artery and endothelial dysfunction in severely obese children: a prospective study. Lancet 358:1400–1404
Ho CT, Lin CC, Hsu HS et al (2011) Arterial stiffness is strongly associated with insulin resistance in Chinese–a population-based study (Taichung Community Health Study, TCHS). J Atheroscler Thromb 18:122–130
van Popele NM, Elizabeth Hak A, Mattace-Raso FU et al (2006) Impaired fasting glucose is associated with increased arterial stiffness in elderly people without diabetes mellitus: the Rotterdam Study. J Am Geriatr Soc 54:397–404
Roberts AC, Porter KE (2013) Cellular and molecular mechanisms of endothelial dysfunction in diabetes. Diab Vasc Dis Res 10:472–482
Daemen MJ, Lombardi DM, Bosman FT, Schwartz SM (1991) Angiotensin II induces smooth muscle cell proliferation in the normal and injured rat arterial wall. Circ Res 68:450–456
Sodhi CP, Kanwar YS, Sahai A (2003) Hypoxia and high glucose upregulate AT1 receptor expression and potentiate ANG II-induced proliferation in VSM cells. Am J Physiol Heart Circ Physiol 284:H846–H852
Reusch JE, Wang CC (2011) Cardiovascular disease in diabetes: where does glucose fit in? J Clin Endocrinol Metab 96:2367–2376
Min Q, Bai YT, Jia G et al (2010) High glucose enhances angiotensin-II-mediated peroxisome proliferation-activated receptor-gamma inactivation in human coronary artery endothelial cells. Exp Mol Pathol 88:133–137
Shanik MH, Xu Y, Skrha J et al (2008) Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Diabetes Care 31:S262–S268
Du X, Edelstein D, Obici S et al (2006) Insulin resistance reduces arterial prostacyclin synthase and eNOS activities by increasing endothelial fatty acid oxidation. J Clin Invest 116:1071–1080
Bender SB, McGraw AP, Jaffe IZ, Sowers JR (2013) Mineralocorticoid receptor-mediated vascular insulin resistance: an early contributor to diabetes-related vascular disease? Diabetes 62:313–319
Carmena R, Betteridge DJ (2004) Statins and diabetes. Semin Vasc Med 4:321–332
Arca M, Pigna G, Favoccia C (2012) Mechanisms of diabetic dyslipidemia: relevance for atherogenesis. Curr Vasc Pharmacol 10:684–686
Raj M (2012) Obesity and cardiovascular risk in children and adolescents. Indian J Endocrinol Metab 16:13–19
Canale MP, Manca di Villahermosa S, Martino G et al (2013) Obesity-related metabolic syndrome: mechanisms of sympathetic overactivity. Int J Endocrinol 2013:865965
Masterjohn C, Park Y, Lee J et al (2013) Dietary fructose feeding increases adipose methylglyoxal accumulation in rats in association with low expression and activity of glyoxalase-2. Nutrients 5:3311–3328
Khitan Z, Kim DH (2013) Fructose: a key factor in the development of metabolic syndrome and hypertension. J Nutr 2013:682673
Tappy L, Lê KA (2010) Metabolic effects of fructose and the worldwide increase in obesity. Physiol Rev 90:23–46
Muniyappa R, Sowers JR (2012) Endothelial insulin and IGF-1 receptors: when yes means NO. Diabetes 61:2225–2227
Zhang Y, Sowers JR, Ren J (2012) Pathophysiological insights into cardiovascular health in metabolic syndrome. Exp Diabetes Res 2012:320534
Mudau M, Genis A, Lochner A, Strijdom H (2012) Endothelial dysfunction: the early predictor of atherosclerosis. Cardiovasc J Afr 23:222–231
Tran LT, Yuen VG, McNeill JH (2009) The fructose-fed rat: a review on the mechanisms of fructose-induced insulin resistance and hypertension. Mol Cell Biochem 332:145–159
Creager MA, Lüscher TF, Cosentino F, Beckman JA (2003) Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Circulation 108:1527–1532
Doronzo G, Russo I, Mattiello L et al (2004) Insulin activates vascular endothelial growth factor in vascular smooth muscle cells: influence of nitric oxide and of insulin resistance. Eur J Clin Invest 34:664–673
Kim JA, Jang HJ, Martinez-Lemus LA, Sowers JR (2012) Activation of mTOR/p70S6 kinase by ANG II inhibits insulin-stimulated endothelial nitric oxide synthase and vasodilation. Am J Physiol Endocrinol Metab 302:E201–E208
Karwowski W, Naumnik B, Szczepański M, Myśliwiec M (2012) The mechanism of vascular calcification – a systematic review. Med Sci Monit 18:RA1–RA11
Townsend RR, Wimmer NJ, Chirinos JA et al (2010) Aortic PWV in chronic kidney disease: a CRIC ancillary study. Am J Hypertens 23:282–289
Speer MY, Yang HY, Brabb T et al (2009) Smooth muscle cells give rise to osteochondrogenic precursors and chondrocytes in calcifying arteries. Circ Res 104:733–741
Johnson RC, Leopold JA, Loscalzo J (2006) Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res 99:1044–1059
Blaha MJ, DeFilippis AP, Rivera JJ et al (2011) The relationship between insulin resistance and incidence and progression of coronary artery calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 34:749–751
Olesen P, Nguyen K, Wogensen L et al (2007) Calcification of human vascular smooth muscle cells: associations with osteoprotegerin expression and acceleration by high-dose insulin. Am J Physiol Heart Circ Physiol 292:H1058–H1064
Yuan LQ, Zhu JH, Wang HW et al (2011) RANKL is a downstream mediator for insulin-induced osteoblastic differentiation of vascular smooth muscle cells. PLoS One 6:e29037
Wang CC, Sorribas V, Sharma G et al (2007) Insulin attenuates vascular smooth muscle calcification but increases vascular smooth muscle cell phosphate transport. Atherosclerosis 195:e65–e75
Mizobuchi M, Towler D, Slatopolsky E (2009) Vascular calcification: the killer of patients with chronic kidney disease. J Am Soc Nephrol 20:1453–1464
Chung AW, Yang HH, Sigrist MK (2009) Matrix metalloproteinase-2 and -9 exacerbate arterial stiffening and angiogenesis in diabetes and chronic kidney disease. Cardiovasc Res 84:494–504
Ganne S, Winer N (2008) Vascular compliance in the cardiometabolic syndrome. J Cardiometab Syndr 3:35–39
Gao L, Laude K, Cai H (2008) Mitochondrial pathophysiology, reactive oxygen species, and cardiovascular diseases. Vet Clin North Am Small Anim Pract 38:137–155
Nisoli E, Clementi E, Carruba MO, Moncada S (2007) Defective mitochondrial biogenesis: a hallmark of the high cardiovascular risk in the metabolic syndrome? Circ Res 100:795–806
Whaley-Connell A, Sowers JR (2011) Indices of obesity and cardiometabolic risk. Hypertension 58:991–993
Liu J, Shen W, Zhao B et al (2009) Targeting mitochondrial biogenesis for preventing and treating insulin resistance in diabetes and obesity: hope from natural mitochondrial nutrients. Adv Drug Deliv Rev 61:1343–1352
Sivitz WI, Yorek MA (2010) Mitochondrial dysfunction in diabetes: from molecular mechanisms to functional significance and therapeutic opportunities. Antioxid Redox Signal 12:537–577
Chávez-Sánchez L, Espinosa-Luna JE, Chávez-Rueda K et al (2014) Innate immune system cells in atherosclerosis. Arch Med Res 45:1–14
Aroor A, McKarns S, Nistala R et al (2013) DPP-4 inhibitors as therapeutic modulators of immune cell function and associated cardiovascular and renal insulin resistance in obesity and diabetes. Cardiorenal Med 3:48–56
Aroor AR, McKarns S, Demarco VG et al (2013) Maladaptive immune and inflammatory pathways lead to cardiovascular insulin resistance. Metabolism 62:1543–1552
Legein B, Temmerman L, Biessen EA, Lutgens E (2013) Inflammation and immune system interactions in atherosclerosis. Cell Mol Life Sci 70:3847–3869
Döring Y, Zernecke A (2012) Plasmacytoid dendritic cells in atherosclerosis. Front Physiol 3:230
Alberts-Grill N, Denning TL, Rezvan A, Jo H (2013) The role of the vascular dendritic cell network in atherosclerosis. Am J Physiol Cell Physiol 305:C1–C21
He S, Li M, Ma X, Lin J, Li D (2010) CD4+CD25+Foxp3+ regulatory T cells protect the proinflammatory activation of human umbilical vein endothelial cells. Arterioscler Thromb Vasc Biol 30:2621–2630
Huang CJ, Webb HE, Zourdos MC, Acevedo EO (2013) Cardiovascular reactivity, stress, and physical activity. Front Physiol 7:4–314
Xiong XQ, Chen WW, Zhu GQ (2014) Adipose afferent reflex: sympathetic activation and obesity hypertension. Acta Physiol (Oxf) 210:468–478
Underwood PC, Adler GK (2013) The Renin angiotensin aldosterone system and insulin resistance in humans. Curr Hypertens Rep 15:59–70
Wada T, Kenmochi H, Miyashita Y et al (2010) Spironolactone improves glucose and lipid metabolism by ameliorating hepatic steatosis and inflammation and suppressing enhanced gluconeogenesis induced by high-fat and high-fructose diet. Endocrinology 151:2040–2049
Benetos A, Lacolley P, Safar ME (1997) Prevention of aortic fibrosis by spironolactone in spontaneously hypertensive rats. Arterioscler Thromb Vasc Biol 17:1152–1156
Garg R, Adler GK (2012) Role of mineralocorticoid receptor in insulin resistance. Curr Opin Endocrinol Diabetes Obes 19:168–175
Tomaschitz A, Ritz E, Pieske B, Rus-Machan J et al (2014) Aldosterone and parathyroid hormone interactions as mediators of metabolic and cardiovascular disease. Metabolism 63:20–31
Brown JM, Williams JS, Luther JM et al (2014) Human interventions to characterize novel relationships between the renin-angiotensin-aldosterone system and parathyroid hormone. Hypertension 63:273–280
Tomaschitz A, Ritz E, Pieske B et al (2012) Aldosterone and parathyroid hormone: a precarious couple for cardiovascular disease. Cardiovasc Res 94:10–19
Jung SM, Jandu S, Steppan J et al (2013) Increased tissue transglutaminase activity contributes to central vascular stiffness in eNOS knockout mice. Am J Physiol Heart Circ Physiol 305:H803–H810
Thomas WG (2005) Double trouble for type 1 angiotensin receptors in atherosclerosis. N Engl J Med 352:506–508
Santhanam L, Tuday EC, Webb AK et al (2010) Decreased S-nitrosylation of tissue transglutaminase contributes to age-related increases in vascular stiffness. Circ Res 107:117–125
Weisbrod RM, Shiang T, Al Sayah L et al (2013) Arterial stiffening precedes systolic hypertension in diet-induced obesity. Hypertension 62:1105–1110
Acknowledgments
The authors would like to thank Brenda Hunter for her editorial assistance. This research was supported by NIH (R01 HL73101, R01 HL107910) and the Veterans Affairs Merit System (0018) for JRS. The authors have no conflict of interest associated with this manuscript.
Disclosure
The authors have no conflict of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Jia, G., Aroor, A.R., Sowers, J.R. (2015). Role of Metabolic Factors: Lipids, Glucose/Insulin Intolerance. In: Berbari, A., Mancia, G. (eds) Arterial Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-14556-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-14556-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14555-6
Online ISBN: 978-3-319-14556-3
eBook Packages: MedicineMedicine (R0)