Abstract
For the past 25 years, academics and practitioners have raised concerns on the measurement of environmental sustainability performance. Addressing these issues has become paramount for organizations worldwide. In the healthcare sector, especially in hospitals, measuring environmental performance relates to the reduction of environmental impact and continuous improvements in the quality of processes and outcomes. Considering this context, the study seeks to identify how concerns on environmental sustainability and performance measurement have pervaded the healthcare operations management literature. A two-tier systematic review of literature included: (1) a literature review on performance measurement, environmental sustainability and healthcare operations management; (2) a bibliometric review of literature, which evaluated published studies (1988–2013), focusing on citation numbers, country of origin, main journals, authors and themes. The study highlighted concerns on the lack of strategic focus of performance indicators, relevance and robustness of metrics and difficulties for the deployment of measures within different hierarchical levels. Furthermore, the bibliometric review emphasized the scarcity of published research addressing the environmental performance measurement in the healthcare setting, especially in the context of developing countries. New frameworks are necessary to define relevant and meaningful indicators for monitoring and assessing environmental performance if healthcare systems and operations are to be improved.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
For the last 25 years, organizations have been urged to internalize concerns related to the use of their productive resources and how to rationalize the impact of their processes on the environment (Kleindorfer et al. 2005). Environmental sustainabilityFootnote 1 has become an important competitive factor that influences strategies, demanding the adoption of ‘best practices’. Developing robust performance measurement frameworks to evaluate environmental sustainability has become a continuous learning process. Sustainable development indicators translate sustainability issues into quantifiable environmental performance measures. Using meaningful indicators to evaluate performance allows monitoring and reflection on the measurement process (Bourne et al. 2000), since their main goal is to assist with the search and achievement of superior performance (Scerri 2010).
According to Porter (2010), enhanced improved performance in any sector depends on the existence of a common goal for the activities and interests of different stakeholders. In the healthcare sector, this goal is associated with the definition of value represented by the patients’ health outcomes by the unit of currency invested in the process. If this value is improved, patients, managers, service providers and suppliers can benefit from it while the sustainability of the healthcare system is also improved (Porter 2010).
Performance measures also encompass concerns on the quality of healthcare services (Kanji and Sá 2003). Quality improvements may lead to less waste of resources, improved patient satisfaction and medical care effectiveness (Maki et al. 2008). In the past, the incineration of waste in local hospitals was common practice (Department of Environment (DoE) 1990). New regulations have forced these organizations to solve this problem through a more systematic and selective manner (Tudor et al. 2005) to promote environmental sustainability. Nowadays, healthcare services providers should consider an efficient mobilization of resources in their blueprints (Vilaça and Oliveira 2008). A healthcare system includes activities and structures, whose primary purpose is influencing health. The health of the population is determined by several factors and among these factors is the provision of healthcare services. Healthcare organizations that ‘embrace’ environmental sustainability tend to gain significant performance improvements and decrease costs related to waste disposal (Jarousse 2012). Efforts to improve sustainability indicators may also raise awareness and generate consistent attitudes to preserve resources.
Healthcare indicators correspond to measurable and explicitly defined items related to the structures, processes and outcomes of the provision of services (Campbell et al. 2001). They represent statistical instruments that monitor performance, analyzing the resources deployment within these systems without necessarily judging value on quality.
The combination of the internalization of concerns on environmental sustainability, the importance of an efficient management of resources and the improvement in service quality raise questions such as:
-
How have the concerns on environmental sustainability pervaded the healthcare operations management?
-
What are the main environmental performance measurement frameworks used within healthcare organizations?
-
What are the main themes being discussed in the context of healthcare organizations?
The study seeks these answers through a systematic review of literature. The paper is divided in five main sections. Section 2 discusses the research methods and strategy adopted in the study. Section 3 analyzes the application of performance measurement frameworks and metrics/indicators used to address environmental sustainability within the healthcare context. The Brazilian legal framework related to healthcare and current practices are also briefly evaluated. Section 4 presents the results of the bibliometric review of literature. Section 5 summarizes final considerations on the study findings while approaching the next steps of the research.
2 Research Methods
Initially, a literature review on performance measurement, environmental sustainability and healthcare operations management was conducted. The main objective was to identify essential terms that convey knowledge across published studies (Krauthammer and Nenadic 2004). Moreover, the literature review indicates what has been learned about the topics and where research gaps are present (Webster and Watson 2002). After this initial step, the bibliometric technique was chosen as research strategy. Bibliometric methods indicate research impact (Wallin 2005; Van Raan 1996; Van Raan and Van Leeuwen 2002). Four databases were selected for the search: Web of Science®, Medline Complete® (EBSCO), Wiley Online Library® and Scopus® (Elsevier). Web of Science was chosen due its multidisciplinary and comprehensive nature. It includes Science Citation Index Expanded (SCI-EXPANDED), Social Sciences Citation Index (SSCI), Arts & Humanities Citation Index (A&HCI), Conference Proceedings Citation Index-Science (CPCI-S) and Conference Proceedings Citation Index—Social Science and Humanities (CPCI-SSH). Medline complete was selected for two reasons: (a) focus on Health Sciences/Biomedical publications that cover healthcare operations; (b) consistent reputation by being associated with the US National Library of Medicine. Wiley Online was chosen mainly because of its comprehensiveness; it is regarded as the world’s ‘broadest multidisciplinary resources’. Finally, Scopus was selected because of the emphasis placed on the peer-review process of its resources and the inclusion of articles in press and conference proceedings.
The searches were conducted between January and March of 2013. The combination of terms found in the literature review guided these searches. The following terms were combined: ‘Hospital’, ‘Operations’, ‘Environment*’ (the asterisk symbol was used to obtain results that included environment and environmental), ‘Indicators’, ‘Performance’, ‘Sustain*’ (the asterisk symbol was used to obtain results that included sustainable and sustainability), ‘Framework’, ‘Quality’, ‘Health’ and ‘Care’ (the terms were combined in the searches, since both Healthcare and Health Care are found in literature). Papers/articles published between 1988 and 2013 were included (25 years), since the publication of ‘Our Common Future’ (1987) represents an important milestone that defined terms currently used to approach concerns on the environment and raise awareness on the importance of the issue (Atkinson 2000; Kleindorfer et al. 2005; Linton et al. 2007). The combinations of terms were used as topics to be found in the Abstracts of the articles.
In order to avoid researcher bias, two independent searches took place: one by the first author and another by one of the co-authors. The coding of different themes followed the rationale: Title of the article→Abstract→Keywords. To avoid bias, the coding process followed the same strategy with two independent analyses. Similar results were obtained in both cases.
3 The Measurement of Environmental Performance in Healthcare Organizations
3.1 Performance Measurement and Environmental Sustainability
The first step for the measurement process refers to the conception of performance measures. According to Medori and Steeple (2000), Gomes et al. (2004) and Neely (2004), several frameworks have been proposed in literature:
-
The performance measurement matrix (Keegan et al. 1989);
-
The SMART model (Cross and Lynch 1989);
-
Performance measurement for World Class Manufacturing created by Maskell (1989);
-
The performance measurement questionnaire (Dixon et al. 1990);
-
The framework proposed by Beischel and Smith (1991);
-
The model based in services of Fitzgerald et al. (1991);
-
The Balanced Scorecard (Kaplan and Norton 1992);
-
The Business Excellence Model developed by the European Foundation for Quality Management (EFQM 2013);
-
The model of organizational macro processes proposed by Brown (1996);
-
The dynamic integrated performance measurement system (Ghalayini et al. 1997);
-
The performance measurement record sheet (Neely et al. 1997); and
-
The performance PRISM (Neely et al. 2002).
Even though a number of performance measurement frameworks can be found, a gap between the application and validation of the concepts within these models has been observed (Pinheiro De Lima et al. 2013). Gomes et al. (2004) found, after an extensive review of literature on performance measurement, little evidence that these measures are formalized and connected with organizational strategy and efficiency. Kaplan and Norton (2004) highlight the need for a correlation between strategy and performance measurement. Only through a consistent connection among these elements, strategies can be translated into actions to achieve strategic goals (Kaplan and Norton 2004; Otley 1999; Wongrassamee et al. 2003) could not find any specification as how to formulate these goals within known models.
Feng and Joung (2011) searched for an appropriate model to evaluate the three dimensions of sustainability in manufacturing organizations: economic, social and environmental. In their study, Feng and Joung (2011) found that the focus tends to be on the perception of external stakeholders (reporting) rather than in getting required information for the decision-making to improve performance. Table 1 presents some of these models. The information contained in Table 1 was complemented with additional frameworks reviewed by the authors of the present paper.
In addition to the models mentioned in Table 1, researchers have suggested the combination of existing frameworks. For instance, Nikolaou and Tsalis (2013) combined the Balanced Scorecard rationale with the indicators proposed within the Global Reporting Initiative (GRI). Nonetheless, after reviewing the frameworks, some difficulties reported in literature can be cited:
-
Deployment of performance measures: studies on sustainable performance measurement reveal difficulties in considering context-specific features in terms of the definition of indicators and deployment of performance measures for each hierarchical level within the organization;
-
Prevalence of subjective judgements: in general, the delineation of performance measures is associated with a significant subjective component. Measures that are useful for one type of organization may be superfluous for another;
-
Scoring methods: Feng and Joung (2011) highlighted the excessive simplicity of scoring methods proposed in the models. Essential aspects related to corporate strategy, changes that may occur in the strategic path of a company/business unit and required trade-offs are consistently disregarded.
3.2 Healthcare Operations and Performance Measurement
Bertrand and De Vries (2005) indicate that a number of characteristics differentiate healthcare operations from manufacturing settings. Healthcare operations are regarded as complex and employing performance evaluation techniques used in manufacturing is described as troublesome. Bertrand and De Vries (2005) highlight the delicate balance of power among different stakeholders: managers, medical experts and nurses. Each group has different expectations on organizational performance goals. Service providers are highly trained professionals, who give instructions and received instructions from final consumers (patients). Healthcare services are not commodities that can be stored; they are associated with the management of limited resources. As healthcare organizations are included in more complex healthcare systems containing hospitals, private clinics, hospices and carers, the performance measurement task is also magnified (Curtright et al. 2000). Table 2 summarizes some of these differences.
Yearly, the United Kingdom National Health Service (NHS) produces 600.000 tons of clinical, pharmaceutical, infectious and domestic waste at a cost of 42 million pounds (approx. 64 million dollars) (Coote 2002). The healthcare sector has been urged to demonstrate efficiency and effectiveness in service provision (Weir et al. 2009). Healthcare (hospitals, private clinics, etc.) is an open system, which is subject to several influences: social, economic, political and technological that can benefit or negatively affect their services (Oliveira 2003). People undergoing treatment, materials and equipment, specialized healthcare services and supporting activities such as laundry, maintenance, Information Technologies represent the inputs of this system. The process is composed by the diagnosis and treatment of patients, that is, activities performed for the provision of medical services. Treated/cured people, the knowledge acquired through research and process wastes represent the outputs (Oliveira 2003). In the healthcare sector, the provision of public and private healthcare services coexists. Healthcare service providers represent ‘the intermediate’ between those who finance the healthcare system and those who pay and use these services (Swayne et al. 2006). These organizations are responsible for managing resources on behalf of those who utilize their services. Nonetheless, as healthcare operations evolve, much attention has been paid to the ‘healthcare business’ instead of focusing on quality improvements (Swayne et al. 2006). Growing pressures for cost reduction and quality improvement have been associated with stricter rules and regulations. This has forced healthcare professionals and managers to reexamine the way performance is evaluated (Castañeda-Méndez et al. 1998).
3.3 Difficulties in Measuring Sustainability—Metrics and Indicators
In spite of the efforts related to obtaining environmental sustainability in the healthcare sector, the outcomes of these initiatives have been unsatisfactory (Phillips et al. 2002). Volumes of waste generated in the healthcare have progressively risen (Woolridge et al. 2005). Several policy weaknesses have been highlighted. Tudor et al. (2008) conclude that a more effective participation in the recycling and waste management in the healthcare sector can be achieved through the incorporation of sustainability concepts into the organizational policies; a comprehensive communication plan; training programs and professional development; and emphasis on the benefits from sustainable practices.
A profusion of frameworks have tried to overcome the complexity of the performance measurement process. Difficulties related to the quantification of information and disregard for performance measurement systems already in place have been reported by the literature. A multiple stakeholder perspective is indicated as one of the most important characteristics that contribute to the success of the application of performance evaluation models given the complexity of the healthcare operations (Tawfik-Shukor et al. 2007).
In addition to existing frameworks, other tools have been proposed for the evaluation of environmental sustainability. Paju et al. (2010) suggested the use of the Sustainable Manufacturing Mapping (SMM), which is a combination of Value Stream Mapping (VSM), Discrete Event Simulation (DES) and Life Cycle Assessment (LCA). The US Environmental Protection Agency has introduced a set of evaluation tools that aimed to improve the environmental performance of American companies (Environmental Protection Agency 2007). Hardi and Pinter (1995) show that indicators that aggregate heterogeneous dimensions are not readily available to be considered in the decision-making process. Indicators currently used by organizations aggregate dimensions that are not comparable and, when they are, the evaluation based on the perception of stakeholders should be careful. Moreover, a process for the selection of indicators focused on specific issues may not compose a balanced view of sustainability issues (Hardi and Pinter 1995). Organizational decision processes guided by a reduced set of indicators may require substantial structural changes. This restrictive process may lead to the selection of indicators related to very specific, less meaningful and non-representative targets. Performance indicators should have specific characteristics to measure performance and represent a source for benchmarking and strategy planning (Feng and Joung 2011). Such characteristics include:
-
Measurability: an indicator should be capable of measuring quantitatively or qualitatively multidimensional perspectives;
-
Relevance: an indicator should be present an useful meaning for the evaluation processes;
-
Clarity: an indicator should be easily understood by the community, especially those that are not experts;
-
Reliability: information proposed by an indicator should be reliable and useful;
-
Data accessibility: an indicator should be based on accessible data;
-
Opportunity: the measurement of an indicator should happen with the frequency that allows an informed and well-timed decision making process;
-
Long term view: an indicator should be compatible with an open pattern that supports the need for recorded information for future generations.
Moreover, the definition of performance indicators depends on the answers to three fundamental questions (Weir et al. 2009):
-
Who should be involved in the development of performance indicators?
-
Who is the audience for the performance indicators (stakeholders)?
-
What level of performance should be measured?
For instance, despite the wide scope of indicators proposed in the applications of the BSC in healthcare organizations, environmental performance indicators are not usually declared. When environmental measures are present, they tend to refer to existing regulations and/or sustainability programs. These concerns are then associated with the framework with no changes/adaptations. In specific cases in Brazil, some environmental indicators were proposed as reported by Campos and Selig (2002):
-
Number of complaints related to the environmental aspect and placed by the community (NGOs, neighborhood, supplier, third-parties, etc.);
-
Number of complaints related to any environmental factors made by a visitor divided by the number of visitors per days (percentage);
-
Water consumption per person (monthly water consumption divided by the number of people, including visitors, employees and third-parties);
-
Electricity consumption per person (monthly consumption divided by the number of people per month, including visitors, employees and third-parties);
-
All legal parameters of discharge of effluents required by legislation;
-
Percentage of inert waste sent to landfills (tons of inert/generated waste);
-
Number of legal non-conformities registered per year (fines, contaminations, violations).
Metrics are vital elements to measure performance, since potential difficulties can be indicated by the gap metric-standard (Melnyk et al. 2004), especially regarding issues related to sustainability (Gunasekaran et al. 2001). Nonetheless, the existence of a framework that deals with the deployment of measures and metrics in strategic, tactical and operational levels to include tangible, intangible, financial and non-financial aspects is questioned in the literature (Gunasekaran and Spalanzani 2012). Metrics mentioned by Zhu and Sarkis (2004) include reductions of air emissions and waste of water, increased investments in training and ‘green’ purchases, and reduced costs with waste treatment and energy consumption.
Two perspectives should be present to define performance measures: resources and value (Fiksel et al. 1999). Resources are represented by energy, materials, water, land, waste, cost and human capital. Value corresponds to the functional performance of resources such as information content, client satisfaction, environmental quality, business competence, human health and social well-being. BP Amoco™, for instance, uses the production process water discharge as a resource indicator. Volvo™ evaluates how many managers include lifecycle tools in the product development process (value).
Townend and Cheeseman (2009) proposed detailed recommendations on how to measurement environmental performance in healthcare organizations based on (a) general management; (b) social issues; (c) health and safety; (d) energy and water use; (e) purchasing and supply; (f) waste management (responsibility, segregation, storage and packaging); (g) waste transport; (h) recycling and re-use; (i) waste treatment; and (j) final disposal.
Veleva et al. (2003) used the hierarchy of indicators established by the Lowell Center of the University of Massachusetts in their study in the pharmaceutical industry. Level 1 indicators are managed by voluntary initiatives or based on regulations (ISO and others). The eco-efficiency measures (Level 2) translate the connection between the environmental performance and savings of financial resources. The standards and methods for the definition of Level 3 indicators (environmental impact) have been developed only recently. Organizations tend to avoid establishing connections between the indicators and competitive advantage, according to the authors. The reduced influence of the government and stakeholders in a wider adoption of these indicators was highlighted. Levels 4 and 5 refer, respectively, to the availability of data on the supply chain participants and collaborations with entities outside the organization (Veleva et al. 2003).
Kaplan and Norton (1992) developed the Balanced Scorecard, using four perspectives to measure performance: (a) financial, (b) client, (c) internal processes and (d) learning and growth. Gurd and Gao (2008) studied the adaptation of the Balanced Scorecard indicators to measure performance in hospitals and clinics. Some examples can be cited:
-
Financial perspective: profit growth indicators, productivity indicators;
-
Client perspective: patient retention, patient acquisition, patient satisfaction indicators;
-
Internal processes perspective: patient satisfaction, safety and health, productivity, innovation indicators;
-
Learning and growth perspective: human capital, information capital, continuous innovation, organizational capital.
However, considering 22 cases reported in their study, only 77 % included the client or patient perspective. Health does not seem the central focus of these BSC applications, the researchers concluded. In the healthcare sector in the US, Mannion and Davies (2002) recognize the existence of scorecards, service provider profile evaluation and medical professional profile. A sufficient number of metrics represents another concern in the performance measurement in hospitals. Multiple aspects are present in a hospital and trying to measure every single aspect of a complex system may emphasize metrics instead of concerns on the quality of the patients and system (Forrest et al. 2006). Regarding environmental performance measurement in healthcare, it is important to point out the existence of common indicators from either practice or current legislation. Table 3 presents some of these common indicators.
McGlynn (Paju et al. 2010) discusses six actions that are necessary to measure performance in healthcare:
-
1.
Identify the perspectives of the system stakeholders;
-
2.
Develop a framework of responsibilities;
-
3.
Establish explicit criteria on how the system will be evaluated;
-
4.
Select a subset of indicators for periodical reports;
-
5.
Minimize conflicts between financial and non-financial incentives and quality goals in healthcare;
-
6.
Facilitate the development of information systems to support quality monitoring.
Indicators should satisfy one or more stakeholder groups (McGlynn 1997). Learning is a dimension needed in the performance measurement process (Wilcock and Campion-Smith 1998). Scientific soundness and applicability should be achieved. It relates to three aspects: reliability, validity and adjustability. Reliability means that replication of the measurement will produce the same results. Validity refers to the measurement of quality related to healthcare. And adjustability involves the use of other factors apart from quality that will influence the measurement final result. Applicability refers to a consistent choice by managers, covering a number of areas and services. It involves parsimony and comprehensiveness (Wilcock and Campion-Smith 1998).
Although a profusion of models and indicators to measure environmental performance have been proposed in literature, initiatives related to the environmental sustainability tend to lack strategic focus. The main purpose behind these initiatives has been connected with rules and regulations, accreditation requirements and elements pertaining to quality programs (e.g. ISO, The Business Excellence Model). As a consequence of the lack of strategic focus and use of standard measures, the deployment of measures in different hierarchical levels has become troublesome (Fiksel et al. 1999). In developing countries such as Brazil, healthcare operations face major challenges such as the high cost of healthcare services, limited existence of productive resources, inadequate infrastructure/structure (e.g. access to clean water, electricity), lack of public investments and strategically focused governmental policies, which underline the difficulties associated with the measurement of sustainability in healthcare operations.
3.4 The Brazilian Regulatory Framework
In Brazil, nine normative documents deal directly or indirectly with the control and disposal of hospital waste. The evaluation of organizations that provide healthcare services, NA2 Rev. 01 of 6 March 2006, is necessary to acquire Hospital Accreditation with the National Organization for Accreditation (ONA, abbreviation in Brazilian Portuguese). The National Environment Council (CONAMA) and the National Health Surveillance Agency (ANVISA) have specific resolutions. While the Brazilian Technical Standards Association (ABNT) issued six standards on hospital waste. The CONAMA Resolution nº 358 (29 April 2005) approaches the need to treat and dispose of waste from healthcare services. The ANVISA Resolution nº 306 (7 December 2004) addresses the management of waste from these services. The ABNT legislates on:
-
Waste transport (NBR 14652, 11 July 2013);
-
Methods for the collection of perforating/cutting materials (NBR 13853, de 30 June 1997);
-
Internal and external collection of waste under hygienic and safe conditions (NBR 12810, 1 April 1993);
-
Classification of materials and definition of terms (NBR 12808, 1 April 1993, and NBR 12807 of 15 June 2013, respectively);
-
Required procedures for the intra-establishment management of healthcare services waste (NBR 12809 of 19 May 2013).
Despite the existence of a legal framework, Da Silva et al. (2005) concluded from a study on 91 healthcare facilities, including hospitals (2), health centers (48) and clinical laboratories (22) that in Brazil the practices in most cases do not comply with current legislation. According to Nazar et al. (2005), the mere existence of regulations does not guarantee the success of environmental initiatives. In Brazil, a scarcity of regulations that define the consumption of other resources such as water, electricity and fuel is noteworthy. Recently, some initiatives have tried to address the disposal of liquid waste (part of the solid waste category) by creating Eco-centers and Effluents Treatment Facilities (Vieira and Rodrigues 2013). Concerns on measurement environmental performance are regarded as insufficient and limited due to a number of issues (La Forgia and Couttolenc 2008).
3.5 Environmental Performance Measurement Frameworks Used in Brazil
The United Kingdom public healthcare system (NHS) represents one of the most recognizable performance measurement frameworks described in literature. In the case of the NHS, a national model of performance evaluation has been applied. A set of 51 indicators (2002) is divided and classified in the following dimensions: health improvement, fair access, effective provision of health, efficiency, patient/carer experience and health outcomes (Woolridge et al. 2005). The environmental sustainability indicators, in this case, are designed from current government policies. The EPA 90 (Environmental Protection Act) constitutes the integrative program, which guides these initiatives. Local initiatives are also implemented to promote a sustainable behavior. These programs had a central objective to improve waste management, establishing goals and indicators for recycling and recovery. Clinical waste was classified and a number of strategies were developed to motivate the separation of items. Alternative treatment technologies were proposed whereas risks for the health of human beings had been observed (Tudor 2007). Potential benefits from the separation and recycling of waste have been emphasized by hospitals and other institutions within the British healthcare system. This promoted new initiatives for efficiency and effectiveness improvements (Tudor 2007).
Regarding solid waste, indicators such as Kilograms per solid waste by patient bed/day or Kilograms of solid waste per appointment and per day have been suggested (Oliveira 2003). Indicators are obtained through sampling. There is an apparent consensus found in literature that it is impossible to define a single indicator of sustainable development. A substantial number of indicators are necessary to capture all the important aspects of a particular system (Becker 1997; Bossel 1999). Performance indicators should perform as an integrated information network and should not be analyzed individually. There are knots that connect or relate to information and data that can assist in the analysis of a particular system (Becker 1997; Bossel 1999). These knots are represented by the performance indicators (factors) built from a referential model proposed for the analysis. Those with greater importance (more weight/importance according to stakeholders) can be prioritized in the management actions (Silva et al. 2008). Performance indicators raise awareness and understanding on issues; inform the decision making process; and measure the achievement of established goals (Ventura et al. 2010).
The Syrian Lebanese Hospital (HSL) case represents an environmental performance measurement framework based on quality programs. Launched in 1998, the hospital’s environmental management program includes the hospital hygiene service, selective collection of waste and different maintenance solutions. Its main goal is to save resources such as water, electricity and gas. Since its launching, the program generated yearly savings of one million cubic meters of water and 679 tons of paper; 19 tons of glass, 23 tons of aluminum and 101 tons of plastic have been recycled (Bio2 Sustentabilidade 2012). In the hospital, the environmental management project focuses on two primary objectives: a better utilization of input material such as water, electricity and gas and the management of waste and reuse of produced waste. The model developed by the hospital is part of the organization’s ‘Quality Management Plan’ constituted by five items: patient safety, health programs accreditation, integrated management system for workers, campaigns/projects and the Joint International Commission (accreditation organization on international quality criteria). The indicators developed for the model focus on waste generation and consumption of process inputs. Communication and monitoring through sustainability reports are regarded as crucial for its success.
The ‘Global Green and Healthy Hospitals Agenda’ represents another example of framework applied in Brazil. The model was created by the coalition ‘Salud Sin Daño’ (Health Care without Harm), composed by an international network of healthcare systems, hospitals, communities, unions and environmental organizations. Its main goal is to transform the worldwide healthcare service without negatively affecting patient care. It seeks environmental sustainability so that the healthcare sector is no longer a source of losses for people and environment. The framework has ten main objectives related to leadership, chemical substances, waste, electricity, transport, food, pharmaceutical products and facilities (GGHHA 2012). According to numbers related to the initiative, the Brazilian hospitals use large amounts of electricity that represent more than 10 % of the total of the commercial energy consumption in the country. By comparison, the UK NHS carbon footprint represents more than 18 million tons of CO2 per year, which is equivalent to 25 % of the total of public sector emissions (GGHHA 2012). The global agenda of the framework presents a comprehensive list of objectives and actions that can be implemented in the search for performance improvement, but does not present guidelines on how to find specific indicators. There are recommendations for the development and implementation of measures from documents that report experiences of hospitals, governmental entities and research in the field. These documents are available in their website and labelled as ‘Tools and Resources’.
Current legislation has also been used to compose frameworks for the healthcare sustainability measurement. That is the case with the Manual of Hospital Accreditation (Ministry of Health (MS) 2002). The document was inspired by the Latin America and Caribbean Hospital Accreditation Manual (Novaes and Paganini 1992). The manuscript, however, represents a very incipient guide to present meaningful indicators and/or metrics adjusted to the healthcare environmental measurement. Three main aspects are controlled: general maintenance, waste and water potability. The existence of indicators is recommended without systematic guidance.
The framework provided by ISO 14001 (ISO 14031 for performance evaluation) constitutes another model used in the healthcare services in Brazil. The standard offers some principles that are periodically verified and evaluated for the re-accreditation. ISO 14001 aims to promote the environmental accreditation of organizations. The Environmental Failure Mode and Effects Analysis (EFMEA) methodology is regarded as a traditional option for the search for flaws in product and/or process projects within ISO (Zambrano and Martins 2007). Regarding the standard and environmental sustainability, it corresponds to the calculation of the risk of the occurrence of a flaw through the multiplication of severity, occurrence and detection indices. Aspects such as the pollution of waters, lands and air are considered. In an industrial environmental, for instance, these aspects are considered: the inputs and outputs of the productive process, the types of flaws that can happen and existing controls. At the end of the process, the more prevalent risks and actions are identified. Brazilian Hospital Albert Einstein (HIAE) with its five units located in São Paulo represents a certified organization. In the organization, the creation and use of an Environmental Management System has built commitment to environmental issues; a more rational use of water, electricity and resources has been noticed. There has been an acknowledgement of the organization and its employees’ environmental responsibility (Sociedade Beneficente Israelita Brasileira (SBIB) 2012).
The Global Reporting Initiative (GRI) methodology is based on a voluntary initiative to standardize sustainability reports. Indicators related to the three dimensions of sustainability are suggested within its guidelines that are also adopted by HIAE. Regarding the environmental dimension, indicators are listed and goals are monitored in terms of (1) materials, (2) energy, (3) water, (4) biodiversity, (5) emissions (6) effluents and waste, (7) products and services, (8) compliance, (9) transport, (10) overall (expenditure and in investments in environmental initiatives), (11) supplier environment assessment and (12) environmental grievance mechanisms. As reported by Morhardt et al. (2002), the indicators proposed by GRI encompass essential aspects of environmental performance. Moreover, GRI guidelines have been promoted by the United Nations Environment Programme (UNEP). The framework is regarded as the most prominent reporting guide due to its focus that goes beyond the environment performance measurement to include a balanced approach of financial (economic) and social issues leading to sustainability.
Considering the current use of the five frameworks previously mentioned, that is, the Balanced Scorecard (BSC), Global Green and Healthy Hospitals Agenda (GGHHA), the standard established by ISO (ISO 14031) and the Hospital Accreditation Manual (HAM) for the measurement of environmental performance, a comparison between these models was made. Table 4 lists key aspects highlighted in literature as crucial for a meaningful measurement of environmental performance while looking for a correspondence in these frameworks.
As per the discussion on metrics of environmental sustainability performance and the analysis of current frameworks, a gap in research can be perceived. Performance metrics should be relevant and incorporate certain characteristics necessary to measure performance in healthcare organizations. The troublesome deployment of measures and indicators within the strategic, tactical and operational levels is also underlined. Moreover, two perspectives should be present while developing measures: resource and value. Resources refer to the evaluation of the use of productive resources: increase and decrease. Value corresponds to the functional performance of each resource within its measure. Furthermore, the way performance data is validated has been discussed. It should involve stakeholders in the development of metrics to improve understanding and emphasize the importance of the measurement. Multiple points of view should be considered to define a sufficient number of performance indicators and metrics. Finally, the robustness of indicators/metrics is a vital milestone for the performance measurement process. Such robustness encompasses three main components: reliability, validity and adjustability. Section 4 describes the main findings of the bibliometric review of literature.
4 The Bibliometric Review
4.1 Search and Analysis Strategy
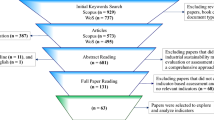
As previously stated, four databases were selected for the search: Web of Science, Medline Complete (EBSCO), Wiley Online Library and Scopus (Elsevier). The following terms were combined and sought in the Abstracts: ‘Hospital’, ‘Operations’, ‘Environment*’, ‘Indicators’, ‘Performance’, ‘Sustain*’, ‘Framework’, ‘Quality’, ‘Health’ and ‘Care’. These terms were used due to their high occurrence identified in the initial literature review. The study analyzed published work between 1988 and 2013, i.e., 25 years since the publication of the Brundtland Report (Barkemeyer et al. 2014). Figure 1 represents the search and analysis strategy.
The combination of the terms: ‘Health’, ‘Care’, ‘Performance’, ‘Indicators’, ‘Environment’, ‘Sustain*’ produced 49 articles that given their comprehensiveness and focus were regarded as suitable for a more in-depth content analysis. After removing duplicates, 35 papersFootnote 2 were selected.
It is important to underline studies that appeared in more than one combination of terms: (Chen et al. 2013; Joiner and Coleman 2012; Klazinga et al. 2011; Wakai et al. 2013) and Gajewski and Dunton (2013) were found twice. Lin et al. (2013), Tanaka et al. (2013) were found three and four times, respectively.
By revealing impact of research, citation numbers have been considered as important indications of quality (Bornmann et al. 2008). Four main aspects were analyzed: (a) country of origin; (b) citation numbers; (c) publication outlets (journals, conferences); (d) main themes associated with environmental performance measurement of healthcare organizations. Table 5 shows the number of results obtained for each combination of terms (10 in total).
Regarding country of origin, a certain prevalence of collaborative studies was noticed. The UK, the US and Turkey are present in more than two occasions. Nonetheless, the review of the papers does not present sufficient data for an account of prevalence of a country or research center. Table 6 displays the information on country of origin.
Given the reduced number of citations found in the first search within Web of Science, a new data collection effort was made through Google Scholar®. This search mechanism is regarded as comprehensive by including peer-reviewed papers, theses, books, abstracts and academic papers published by professional organizations, pre-publication libraries, universities and other academic entities. Figure 2 describes the results of both searches.
After comparing the results, a significant increase was perceived. Nevertheless, the most cited papers remained the same: Mutemwa (2005), Klazinga et al. (2011), Aitken et al. (2011), Andrade et al. (2012). Mutemwa (2005) investigates the effectiveness of Information Systems for healthcare management in Zambia. The study was associated with the Centre for AIDS Research of the University of Southampton in the United Kingdom. It does not, however, address environment sustainability; it focuses on the economic and social impact of technology to forge sustainability.
The paper by Klazinga et al. (2011) listed a number of themes related to the quality of healthcare results. The need for more valid and reliable performance indicators was pointed out in the research. Aitken et al. (2011) focused on human resources and the internal environment of hospitals in terms of their role to achieve sustainability. Andrade et al. (2012) explored the physical and social environment of four Portuguese hospitals: two old units and two recently renovated hospitals. The main purpose behind the study was to develop quality evaluation mechanisms for internal settings.
The publication outlets were also analyzed. In only three cases, publications were cited more than once within the list. Two papers were published within BMC Public Health (Impact Factor: 2.32); two articles were published in the International Journal of Quality in Health Care (Impact Factor: 1.584) and two papers were published within Water Resources Management (Impact Factor: 2.463). The information on Impact Factors was collected from their websites. Two of the analyzed articles were published in conference proceedings: (Freitas et al. 2011; Tchouaket et al. 2012). Table 7 lists the papers by publication outlet.
As previously stated, the bibliometric review also aimed to analyze the main themes being discussed in the context of the healthcare organizations. Figure 3 represents the analysis on emerging themes. The coding of different themes followed the sequence: Paper title-Abstract-Keywords. Nine main themes were coded in the analysis. Three studies focused on the development of quality indicators based on benchmarking. Four papers emphasized the importance of ‘best practices’ in terms of quality improvement in the internal environment of hospitals. Six articles focused on strategies to improve economic/social efficiency of healthcare organizations (based on the Balanced Scorecard). One study focused on cleaner production in general. Economic development, especially at country and city level, was evaluated in three of the studies. Five papers reported on initiatives to improve efficiency in healthcare, mainly connected with cost reduction and economic savings of hospital units. One paper discussed Hospital Accreditation. Two of the studies were related to the role/impact of Information Systems to improve healthcare performance and quality. And ten of the articles reported on indicators of the preservation of natural resources, biodiversity and reduction of solid waste.
5 Final Considerations and Further Research
The literature has shown that there is scarce evidence on the formalization of performance measures across organizations. In many cases, the systems already in place are ignored when new metrics are established. Regarding performance measurement frameworks, the lack of guidelines on the development and selection of performance indicators was also identified in the study. A consistent concern on the external public was indicated while internally the sustainability indicators are often composed by dimensions that are not comparable, restrict, and even insignificant. As a result, the application of frameworks for the environmental sustainability measurement has been far from satisfactory. Considering the importance of performance measurement for the healthcare sector, especially in developing countries, and the significant impact of its operations, there is a clear need for more robust/systematic frameworks guided by practice. New models are necessary to define relevant indicators for monitoring and performance evaluation in the sector. The search for measures that can raise awareness, continuous improvement and innovation in organizational processes has just begun. The study represents a starting point in proposing a meaningful framework to measure environmental sustainability in hospitals within the Brazilian setting.
Notes
- 1.
The terms environmental and sustainability are used interchangeably and in combination in the study.
- 2.
It is important to indicate that the set of 35 papers is listed at the end of the list of references and arranged alphabetically (Abou-Ali and Abdelfattah 2013; Aitken et al. 2011; Andrade et al. 2012; Boriani et al. 2013; Boyer et al. 2012; Braithwaite et al. 2012; Brown et al. 2013; Chen et al. 2013; El-Jardali et al. 2011; Freitas et al. 2011; Gajewski and Dunton 2013; Gimelli and Muccillo 2013; Hao et al. 2012; Harmancioglu et al. 2013; Iacone et al. 2012; Joiner and Coleman 2012; Klazinga et al. 2011; Koutkias et al. 2012; Lin et al. 2013; Mears et al. 2011; Menikpura et al. 2012; Mutale et al. 2013; Mutemwa 2005; Olafsdottir et al. 2011; Peterson et al. 2013; Santana-Medina et al. 2013; Seke et al. 2013; Sulku 2012; Tanaka et al. 2013; Tchouaket et al. 2012; Townend 1996; Tseng 2013; Wakai et al. 2013; Yi and Ma 2010; Yildiz and Demirors 2013). Within the text, the format author(s) name/year of publication was adopted for easiness.
References
Atkinson G (2000) Measuring corporate sustainability. J Environ Plann Manage 43(2):235–252
Barkemeyer R, Holt D, Preuss Lutz, Tsang S (2014) What happened to the development in sustainable development? Business guidelines two decades after brundtland. Sustain Dev 22(1):15–32 (First published 2011)
Beischel ME, Smith KR (1991) Linking the shop floor to the top floor. Manag Account 73(4):25
Becker B (1997) Sustainability assessment: a review of values. Concepts and Methodological Approaches, World Bank, Washington, DC
Bertrand W, De Vries G (2005) Lessons to be learned from operations management. Health Operations Management: patient flow logistics in health care, London, Routledge
Bossel H (1999) Indicators for Sustainable development: theory, method, applications: a report to the balaton group. IISD, Winnipeg
Bio2 Sustentabilidade (2012) Projeto de Gestão Ambiental—Hospital Sírio Libanês. Available at http://www.agendasustentavel.com.br/Case.aspx?id=555. Accessed 1 March 2012
Bornmann L, Mutz R, Neuhaus C, Daniel HD (2008) Citation counts for research evaluation: standards of good practice for analyzing bibliometric data and presenting and interpreting results. Ethics Sci Environ Politics 8(1):93–102
Bourne M, Mills J, Wilcox M, Neely A, Platts K (2000) Designing, implementing and updating performance measurement systems. Int J Oper Prod Manag 20(7):754–771
Brown MG (1996) Keeping score: using the right metrics to drive world-class performance. Quality Recourses, New York
Castañeda-Méndez K, Mangan K, Lavery AM (1998) The Role and application of the balanced scorecard in healthcare quality management. J Healthc Qual 20(1):10–13
Campbell B, Sayer JA, Frost P, Vermeulen S, Ruiz-Pérez M, Cunningham A, Prabhu R (2001) Assessing the performance of natural resource systems. Conservation Ecology 5 (2), 22, [online]. Available at http://www.consecol.org/vol5/iss2/art22/. Accessed 1 April 2012
Campos LMS, Selig PM (2002) SGADA—Sistema de gestão e avaliação do desempenho ambiental: a aplicação de um modelo de SGA que utilize o Balanced Scorecard (BSC). Revista Eletrônica de Administração (REAd) 8(6):1–23
Cross K, Lynch R (1989) Accounting for competitive performance. J Cost Manag 3(1):20–28
Curtright JW, Stolp-Smith S, Edell ES (2000) Strategic performance management: development of a performance measurement system at the Mayo Clinic. J Healthc Manag 45(1):58–68
Coote A (2002) Claiming the Health Dividend. King’s Fund, London
Da Silva CE, Hoppe AE, Ravanello MM, Mello N (2005) Medical wastes management in the south of Brazil. Waste Manag 25(6):600–605
Department of Environment (DoE) (1990) The Environmental Protection Act. HMSO London
Dixon JR, Nanni AJ, Vollmann TE (1990) The new performance challenge: measuring operations for world-class competition. Dow Jones-Irwin, Homewood, Illinois
EFQM (2013) European Foundation for Quality Management. In: Fundamental Concepts. Available at http://www.efqm.org/efqm-model/fundamental-concepts. Accessed 10 Sep 2013
Environmental Protection Agency (2007) The lean and environment toolkit. Environmental Protection Agency, USA. Available at http://www.epa.gov/lean/toolkit/LeanEnviroToolkit.pdf. Accessed 1 July 2012
Feng SC, Joung CB (2011) A measurement infrastructure for sustainable manufacturing. Int J Sustain Manufact 2(2):204–211
Fiksel J, McDaniel J, Mendenhall C (1999) Measuring progress towards sustainability principles, process and best practices. Battelle Memorial Institute, Ohio
Fitzgerald L, Brignall S, Silvestro R, Voss C (1991) Performance measurement in service businesses. Chartered Institute of Management Accountants, London
Forrest CB, Villagra VV, Pope JE (2006) Managing the metric vs managing the patient: the physician’s view of pay for performance. The Am J Managed Care 12(2):83–85
GGHHA (2012) Global green and healthy hospitals agenda. Available at http://hospitalesporlasaludambiental.net/. Accessed 1 July 2012
Ghalayini AM, Noble JS, Crowe TJ (1997) An integrated dynamic performance measurement system for improving manufacturing competitiveness. Int J Prod Econ 48(3):207–225
Gomes CF, Yasin MM, Lisboa JV (2004) A literature review of manufacturing performance measures and measurement in an organizational context: a framework and direction for future research. J Manufact Technol Manag 15(6):511–530
Gunasekaran A, Patel C, Tirtiroglu E (2001) Performance measures and metrics in a supply chain environment. Int J Oper Prod Manag 21(1/2):71–87
Gunasekaran A, Spalanzani A (2012) Sustainability of manufacturing and services: investigations for research and applications. Int J Prod Econ 140(1):35–47
Gurd B, Gao T (2008) Lives in the balance: an analysis of the balanced scorecard (BSC) in healthcare organizations. Int J Prod Perform Manag 57(1):6–21
Hardi P, Pinter L (1995) Models and methods of measuring sustainable development performance. International Institute for Sustainable Development (IISD), Winnipeg, 301 p
Jarousse LA (2012) Environmental sustainability programs for hospitals. Hosp Health Netw 86(1):33–40
Kanji GP, Sá PM (2003) Sustaining healthcare excellence through performance measurement. Total Qual Manag Bus Excellence 14(3):269–289
Kaplan RS, Norton DP (1992) The balanced scorecard—measures that drive performance. Harvard Bus Rev 70(1):71–79
Kaplan RS, Norton DP (2004) The strategy map: guide to aligning intangible assets. Strategy Leadersh 32(5):10–17
Keegan DP, Eiler RG, Jones CR (1989) Are your performance measures obsolete? Manag Account 70(12):45–50
Kleindorfer PR, Singhal K, Van Wassenhove LN (2005) Sustainable Operations Management. Prod Oper Manag 14(4):482–492
Krauthammer M, Nenadic G (2004) Term identification in the biomedical literature. J Biomed Inform 37(6):512–526
La Forgia GM, Couttolenc BF (2008) Hospital Performance in Brazil: the search for excellence. World Bank Publications, Washington DC
Linton JD, Klassen R, Jayaraman V (2007) Sustainable supply chains: an introduction. J Oper Manag 25(6):1075–1082
Maki J, Qualls M, White B, Kleefield S, Crone R (2008) Health impact assessment and short-term medical missions: a methods study to evaluate quality of care. BMC Health Service Research 8:121–128
Mannion R, Davies HTO (2002) Reporting health care performance: learning from the past, prospects for the future. J Eval Clin Pract 8(2):215–228
Maskell B (1989) Performance measures of world class manufacturing. Manag Account 67(5):32–33
McGlynn EA (1997) Six challenges in measuring the quality of health care. Health Aff 16(3):7–21
Medori D, Steeple D (2000) A framework for auditing and enhancing performance measurement systems. Int J Oper Prod Manag 20(5):520–533
Melnyk SA, Stewart DM, Swink M (2004) Metrics and performance measurement in operations management: dealing with the metrics maze. J Oper Manag 22(3):209–218
Ministry of Health (MS) (2002) Manual Brasileiro de Acreditação Hospitalar. Brazilian Manual of Hospital Accreditation, Series A, Standards and Technical Manuals 117, 3rd Edition, Reviewed and Updated, 109p
Morhardt JE, Baird S, Freeman K (2002) Scoring corporate environmental and sustainability reports using GRI 2000, ISO 14031 and other criteria. Corp Soc Responsib Environ Manag 9(4):215–233
Nazar MW, Pordeus IA, Werneck MAF (2005) Gerenciamento de resíduos sólidos de odontologia em postos de saúde da rede municipal de Belo Horizonte, Brasil. Revista Panamericana Salud Publica 17(4):237–242
Neely A (ed) (2004) Business performance measurement: theory and practice. Cambridge University Press, Cambridge, 2002 (2004 edition)
Neely AD, Adams C, Kennerley M (2002) The performance prism: the scorecard for measuring and managing business success. Prentice Hall Financial Times, London
Neely A, Richards H, Mills J, Platts K, Bourne M (1997) Designing performance measures: a structured approach. Int J Oper Prod Manag 17(11):1131–1152
Nikolaou IE, Tsalis TA (2013) Development of a sustainable balanced scorecard framework. Ecol Ind 34:76–86
Novaes HM, Paganini JM (1992) Garantia de qualidade: acreditação de hospitais para a América Latina e o Caribe. Pan American Health Organization, Series Silos nº, Washington, DC 13
Oliveira JM (2003) A questão dos resíduos de serviços de saúde na administração hospitalar. EnANPAD 27, Atibaia/SP, Proceedings
Otley D (1999) Performance management: a framework for management control systems research. Manag Account Res 10(4):363–382
Porter ME (2010) What is value in health care? The N Engl J Med 363(26):2477–2481
Pinheiro De Lima E, Gouvea Da Costa SE, Angelis JJ, Munik J (2013) Performance measurement systems: a consensual analysis of their roles. Int J Prod Econ 146(2):524–542
Phillips PS, Holley K, Bates MP, Freestone NP (2002) Corby waste not: an appraisal of the UK’s largest holistic waste minimisation project. Resour Conserv Recycl 36(1):1–31
Paju M, Heilala J, Hentula M, Heikkila A, Johansson B, Leong S, Lyons K (2010) Framework and indicators for a sustainable manufacturing mapping methodology. In: Simulation Conference (WSC), Proceedings of the 2010 IEEE Winter: 3411-3422
Scerri A (2010) Accounting for sustainability: implementing a residential emissions reduction strategy using an approach that combines qualitative and quantitative ‘indicators’ of sustainability. Manag Environ Qual Int J 21(1):122–135
Swayne L, Duncan WJ, Ginter PM (2006) Strategic management of health care organizations, 5th edn. Blackwell Publishing, Pastow 869p
Silva SRA, Gonçalves MA, Siqueira PC, Silveira CAC (2008) As decisões de investimento na Fundação Hospitalar de Minas Gerais e seus reflexos nos indicadores de qualidade. RAHIS—Revista de Administração Hospitalar e Inovação em Saúde, Belo Horizonte, 1(1):46–57
Sociedade Beneficente Israelita Brasileira (SBIB) (2012) Programa Einstein de Sustentabilidade, Einstein Sustainability Program. Available at http://www.einstein.br/sobre-a-sociedade/sustentabilidade/Paginas/programa-de-sustentabilidade.aspx. Accessed 3 June 2012
Tawfik-Shukor AR, Klazinga NS, Arah OA (2007) Comparing health system performance assessment and management approaches in the Netherlands and Ontario, Canada. BMC Health Serv Res 7:25–37
Townend WK, Cheeseman C, Edgar J, Tudor T (2009) Factors driving the development of healthcare waste management in the United Kingdom over the past 60 years. Waste Manage Res 27:362–373
Tudor TL (2007) Towards the development of a standardized measurement unit for healthcare waste generation. Resour Conserv Recycl 50:319–333
Tudor TL, Noonan CL, Jenkin LET (2005) Healthcare waste management: a case study from the National health service in Cornwall. Waste Manag 25(6):606–615
Tudor TL, Barr SW, Gilg AW (2008) A novel conceptual framework for examining environmental behavior in large organizations: a case study of the Cornwall National Health Service (NHS) in the United Kingdom. Environ Behav 40(3):426–450
Van Raan AFJ (1996) Advanced bibliometric methods as quantitative core of peer review based evaluation and foresight exercises. Scientometrics 36(3):397–420
Van Raan AFJ, Van Leeuwen TN (2002) Assessment of the scientific basis of interdisciplinary, applied research: application of bibliometric methods in nutrition and food research. Res Policy 31(4):611–632
Ventura KS, Reis LFR, Takayanagui AMM (2010) Avaliação do gerenciamento de resíduos de serviços de saúde por meio de indicadores de desempenho. Engenharia Sanitária e Ambiental 15(2):167–176
Veleva V, Hart M, Greiner T, Crumbley C (2003) Indicators for measuring environmental sustainability: a case study of the pharmaceutical industry. Benchmarking: an Int J 10(2):107–119
Vieira DS, Rodrigues SS (2013) Picoli RL (2013) Gestão Ambiental e Resíduos Hospitalares: Uma análise sobre a legislação vigente e a viabilidade de implantação dos Econcentros e ECTE no Distrito Federal. IV Congresso Brasileiro de Gestão Ambiental, Salvador/BA, pp 25–28
Vilaça WPT, Oliveira MM (2008) Sustentabilidade e Comunicação no contexto hospitalar: estabelecendo a necessária conscientização. IX Congreso Latinoamericano de Investigación De La Comunicación, México, October
Webster J, Watson RT (2002) Analyzing the past to prepare for the future: writing a literature review. Manag Inf Syst Q 26(2):3
Wallin JA (2005) Bibliometric methods: pitfalls and possibilities. Basic Clin Pharmacol Toxicol 97(5):261–275
Weir E, D’Entremont N, Stalker S, Kurji K, Robinson V (2009) Applying the balanced scorecard to local public health performance measurement: deliberations and decisions. BMC Public Health 8(9):127–134
Wongrassamee S, Gardiner PD, Simmons JEL (2003) Performance measurement tools—the balanced scorecard and the EFQM excellence model. Measuring Bus Excellence 7(1):14–29
Woolridge A, Morrissey A, Phillips PS (2005) The development of strategic and tactical tools, using systems analysis for waste management in large, complex organisations: a case study in UK Health Care. Res Conserv Policy 44(2):115–137
Wilcock PM, Campion-Smith C (1998) Never mind the quality: feel the improvement. Qual Health Care: QHC 7(4):181
Zambrano TF, Martins MF (2007) Utilização do método FMEA para avaliação do risco ambiental. Gestão & Produção [online] 14(2):295–309
Zhu Q, Sarkis J (2004) Relationships between operational practices and performance among early adopters of green supply chain management practices in Chinese manufacturing enterprises. J Oper Manag 22(3):265–289
References—Bibliometric Review
Abou-Ali H, Abdelfattah YM (2013) Integrated paradigm for sustainable development: a panel data study. Econ Model 30:334–342. ISSN 0264–9993
Aitken LM, Hackwood B, Crouch S, Clayton S, West N, Carney D, Jack L (2011) Creating an environment to implement and sustain evidence based practice: a developmental process. Aust Crit Care 24(4):244–254. ISSN 1036–7314
Andrade C, Lima ML, Fornara F, Bonaiuto M (2012) Users’ views of hospital environmental quality: validation of the Perceived Hospital Environment Quality Indicators (PHEQIs). J Environ Psychol 32(2):97–111. ISSN 0272–4944
Boriani E, Benfenati E, Baderna D, Thomsen M (2013) Application of ERICA index to evaluation of soil ecosystem health according to sustainability threshold for chemical impact. Sci Total Environ 443:134–142. ISSN 0048–9697
Boyer KK, Gardner JW, Schweikhart S (2012) Process quality improvement: an examination of general vs. outcome-specific climate and practices in hospitals. J Oper Manag 30(4):325–339. ISSN 0272–6963
Braithwaite J, Shaw CD, Moldovan M, Greenfield D, Hinchcliff R, Mumford V, Kristensen MB, Westbrook J, Nicklin W, Fortune T, Whittaker S (2012) Comparison of health service accreditation programs in low-and middle-income countries with those in higher income countries: a cross-sectional study. Int J Qual Health Care 24(6):568–577. ISSN 1353–4505
Brown NW, Malmqvist T, Bai W, Molinari M (2013) Sustainability assessment of renovation packages for increased energy efficiency for multi-family buildings in Sweden. Build Environ 61:140–148. ISSN 0360–1323
Chen HC, Chang TC, Lin YT, Cheng HY, Chang TL (2013) Application of DMAIC process to enhance health effects in caring institution. Qual Quant47(4):2065–2080. ISSN 0033–5177
El-Jardali F, Saleh S, Ataya N, Jamal D (2011) Design, implementation and scaling up of the balanced scorecard for hospitals in Lebanon: policy coherence and application lessons for low and middle income countries. Health Policy 103(2):305–314. ISSN 0168–8510
Freitas A, Costa T, Marques B, Gaspar J, Gomes J, Lopes F, Lema I (2011) A framework for the production and analysis of hospital quality indicators. In Information Technology in Bio-and Medical Informatics, Springer, Berlin, pp 96–105. ISSN 0302–9743
Gajewski BJ, Dunton N (2013) Identifying Individual Changes in Performance With Composite Quality Indicators While Accounting for Regression to the Mean. Medical Decision Making 33 (3):396–406. ISSN 0272-989X
Gimelli A, Muccillo M (2013) Optimization criteria for cogeneration systems: multi-objective approach and application in an hospital facility. Appl Energy 104:910–923. ISSN 0306–2619
Hao T, Du PF, Gao Y (2012) Water environment security indicator system for urban water management. Frontiers Environ Sci Eng 6(5):678–691. ISSN 2095–2201
Harmancioglu NB, Barbaros F, Cetinkaya CP (2013) Sustainability issues in water management. Water Resour Manag 27(6):1867–1891. ISSN 0920–4741
Iacone F, Martin S, Siciliani L, Smith PC (2012) Modelling the dynamics of a public health care system: evidence from time-series data. Appl Econ 44(23):2955–2968. ISSN 0003–6846
Joiner KA, Coleman DL (2012) Perspective: key indicators in academic medicine: a suggested framework for analysis. Acad Med 87(2):230–235. ISSN 1040–2446
Klazinga N, Fischer C, Asbroek A (2011) Health services research related to performance indicators and benchmarking in Europe. J Health Serv Res Policy 16:38–47. ISSN 1355–8196
Koutkias V, Kilintzis V, Stalidis G, Lazou K, Niès J, Durand-Texte L, McNair P, Beuscart R, Maglaveras N (2012) Knowledge engineering for adverse drug event prevention: on the design and development of a uniform, contextualized and sustainable knowledge-based framework. J biomed inform 45(3):495–506. ISSN 1532–0464
Lin QL, Liu L, Liu HC, Wang DJ (2013) Integrating hierarchical balanced scorecard with fuzzy linguistic for evaluating operating room performance in hospitals. Expert Syst Appl, 40(6):1917–1924. ISSN 0957–4174
Mears A, Vesseur J, Hamblin R, Long P, Den Ouden L (2011) Classifying indicators of quality: a collaboration between dutch and english regulators. Int J Qual Health Care 23(6):637–644. ISSN 1353–4505
Menikpura SNM, Gheewala SH, Bonnet S (2012) Framework for life cycle sustainability assessment of municipal solid waste management systems with an application to a case study in Thailand. Waste Manag Res 30(7):708–719. ISSN 0734–242X
Mutale W, Godfrey-Fausset P, Mwanamwenge MT, Kasese N, Chintu N, Balabanova D, Spicer N, Ayles H (2013) Measuring health system strengthening: application of the balanced scorecard approach to rank the baseline performance of three rural districts in Zambia. PloS one 8(3):e58650. ISSN 1932–6203
Mutemwa RI (2005) HMIS and decision-making in Zambia: re-thinking information solutions for district health management in decentralized health systems. Health Policy Plann 21(1):40–52. ISSN 0268–1080
Olafsdottir AE, Reidpath DD, Pokhrel S, Allotey P (2011) Health systems performance in sub-Saharan Africa: governance, outcome and equity. BMC public health 11(1):237. ISSN 1471–2458
Peterson HM, Nieber JL, Kanivetsky R, Shmagin B (2013) Water resources sustainability indicator: application of the watershed characteristics approach. Water resour manag 27(5):1221–1234. ISSN 0920–4741
Santana-Medina N, Franco-Maass S, Sánchez-Vera E, Imbernon J, Nava-Bernal G (2013) Participatory generation of sustainability indicators in a natural protected area of Mexico. Ecol Ind 25:1–9. ISSN 1470–160X
Seke K, Petrovic N, Jeremic V, Vukmirovic J, Kilibarda B, Martic M (2013) Sustainable development and public health: rating European countries. BMC public health 13(1):77. ISSN 1471–2458
Sulku SN (2012) The health sector reforms and the efficiency of public hospitals in Turkey: provincial markets. Eur J Public Health 22(5):634–638. ISSN 1101–1262
Tanaka M, Lee J, Ikai H, Imanaka Y (2013) Development of efficiency indicators of operating room management for multi‐institutional comparisons. J eval clin prac 19(2):335–341. ISSN 1356–1294
Tchouaket ÉN, Lamarche PA, Goulet L, Contandriopoulos AP (2012) Health care system performance of 27 OECD countries. The Int J Health Plann Manag, 27(2):104–129. ISSN 0749–6753
Townend B (1996) The implications of sustainable development and the zero option for health care waste. 7th Iswa International Congress, Proceedings II:II74–II81
Tseng ML (2013) Modeling sustainable production indicators with linguistic preferences. J Cleaner Prod 40:46–56. ISSN 0959–6526
Wakai A, O’Sullivan R, Staunton P, Walsh C, Hickey F, Plunkett PK (2013) Development of key performance indicators for emergency departments in Ireland using an electronic modified-Delphi consensus approach. Eur J Emerg Med 20(2):109–114. ISSN 0969–9546
Yi R, Ma ZX (2010) Research on the comprehensive evaluation of small town sustainable development based on DEA. Adv Manag Technol Pt 1:264–270. ISBN 978-1-921712-08-1
Yildiz O, Demirors O (2013) Measuring healthcare process quality: applications in public hospitals in Turkey. Inform Health Soc Care 38(2):132–149. ISSN 1753–8157
Acknowledgment
The researchers would like to acknowledge the support of ‘UNIDAVI’ through a PhD scholarship provided to Mrs. Blass.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Blass, A.P., da Costa, S.E.G., de Lima, E.P., Borges, L.A. (2015). The Measurement of Environmental Performance in Hospitals: A Systematic Review of Literature. In: Chiarini, A. (eds) Sustainable Operations Management. Measuring Operations Performance. Springer, Cham. https://doi.org/10.1007/978-3-319-14002-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-14002-5_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14001-8
Online ISBN: 978-3-319-14002-5
eBook Packages: Business and EconomicsBusiness and Management (R0)