Abstract
ACE inhibitors are commonly used to treat hypertension and congestive heart failure.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Congestive Heart Failure
- Angiotensin Convert Enzyme
- Angiotensin Convert Enzyme Inhibitor
- Vascular Malformation
- Mucosal Edema
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
43.1 Uses
ACE inhibitors are commonly used to treat hypertension and congestive heart failure.
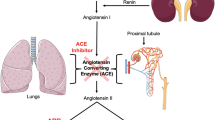
43.2 Mechanism
ACE inhibitors are believed to result in angioedema through increased bradykinin activity, which causes transient vasodilation and extravasation of fluid into the extracellular space, resulting in soft tissue edema. ACE inhibitor-induced angioedema is a class effect and is not dose dependent.
43.3 Discussion
The use of ACE inhibitors is believed to be the most common cause of angioedema, comprising approximately 35 % of all cases of angioedema. Conversely, angioedema occurs in approximately 0.1–1 % of patients treated with ACE inhibitors. ACE inhibitor-induced angioedema is primarily localized in the head and neck, especially in the face, mouth, tongue, lips, and larynx. The distribution of involvement tends to be diffuse and bilateral (Fig. 43.1), although focal or unilateral lingual and peritonsillar edema have been reported (Fig. 43.2). Patients with suspected angioedema are typically assessed clinically and via laryngoscopy, but may present for radiological imaging. The edema of the affected tissues appears as relatively low attenuation on CT and as low T1 and high T2 signal on MRI, without much abnormal enhancement. Patients often present shortly after initiating ACE inhibitors, but can sometimes develop angioedema many years after starting the medication. The severity of angioedema can also vary considerably from benign facial swelling to severe airway obstruction. Treatment consists of stopping the medication, instituting steroids and antihistamines, and supportive care for airway protection, which may require intubation or tracheotomy.
43.4 Differential Diagnosis
Several other drugs, such as rituximab, alteplase, fluoxetine, laronidase, lepirudin, and tacrolimus, can also cause angioedema. Otherwise, the imaging differential diagnosis for angioedema includes infection, longus coli calcific tendonitis, vascular malformations (Fig. 43.5), and neoplasms (Fig. 43.6).
-
Phlegmon appears as ill-defined areas of hypoattenuation and swelling on CT, while abscess is characterized by a rim-enhancing fluid collection (Fig. 43.3). Clinical parameters, such as fever and elevated white blood cell count, are typically present.
-
Longus colli calcific tendonitis can present with prevertebral space edema. Identifying a calcification on CT along the course of the tendon helps to make the diagnosis (Fig. 43.4). Patients can present with neck pain and fever.
-
Vascular malformations, such as lymphatic malformations (Fig. 43.5), can present as focal or diffusely infiltrative trans-spatial lesions. These lesions are often initially diagnosed in children or young adults. Patients may present acutely due to hemorrhage within such a lesion.
-
Neoplasms, such as squamous cell carcinoma (refer to Chaps. 1, 2, and 8), can present as an infiltrative mass in the oral cavity or pharynx. Tumors typically demonstrate enhancement, but may contain areas of necrosis that do not enhance.
-
Radiation therapy for head and neck cancers of the aerodigestive track often produces diffuse pharyngeal mucosal edema (Fig. 43.6). This is generally mild and chronic and may be accompanied by other changes, such as subcutaneous fat reticulation.
Suggested Reading
Al-Khudari S, Loochtan MJ, Peterson E, Yaremchuk KL. Management of angiotensin-converting enzyme inhibitor-induced angioedema. Laryngoscope. 2011;121(11):2327–34.
Chiu AG, Newkirk KA, Davidson BJ, Burningham AR, Krowiak EJ, Deeb ZE. Angiotensin-converting enzyme inhibitor-induced angioedema: a multicenter review and an algorithm for airway management. Ann Otol Rhinol Laryngol. 2001;110(9):834–40.
Ee YS, Sow AJ, Goh BS. Unilateral tongue angioedema caused by angiotensin-converting enzyme inhibitor. J Laryngol Otol. 2010;124(12):1337–9.
Raman SP, Lehnert BE, Pruthi S. Unusual radiographic appearance of drug-induced pharyngeal angioedema and differential considerations. AJNR Am J Neuroradiol. 2009;30(1):77–8.
Winters ME, Rosenbaum S, Vilke GM, Almazroua FY. Emergency department management of patients with ACE-inhibitor angioedema. J Emerg Med. 2013;45:775–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ginat, D.T., Johnson, J.M. (2015). Angiotensin Converting Enzyme (ACE) Inhibitors. In: Ginat, D., Small, J., Schaefer, P. (eds) Neuroimaging Pharmacopoeia. Springer, Cham. https://doi.org/10.1007/978-3-319-12715-6_43
Download citation
DOI: https://doi.org/10.1007/978-3-319-12715-6_43
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-12714-9
Online ISBN: 978-3-319-12715-6
eBook Packages: MedicineMedicine (R0)