Abstract
Ablation therapy is proving to be a major tool in the anti-cancer armamentarium. The superb diagnostic capabilities of CT, US, and MRI, along with IR techniques, have combined to allow percutaneous tumor ablation to become fairly widespread in availability at major centers. The fundamental concept of ablation is that the extremes of temperature kill cancer. Thus both heating and freezing methods are effectively tumoricidal. Heating options are via radiofrequency, laser, and microwave. The former is utilized most frequently, laser least, and microwave is in its early clinical experience. Other primary methods of percutaneous tumor ablation include cryotherapy (CRYO) and direct chemical injection. While various agents have been injected for direct percutaneous injection into tumors, alcohol ablation is most effective, and has been utilized most frequently. The efficacy of radiofrequency ablation (RFA) is related to the size of the liver tumor. It is accepted that the lesion should not exceed 2.5–3.0 cm to obtain complete necrosis. It has been reported that certain microwave ablation (MWA) devices may allow successful treatment of lesions as large as 5 cm with an acceptable margin of safety. Notwithstanding, RFA commonly is utilized for lesions greater than 3 cm in diameter, occasionally for palliative debulking rather than cure. Guidelines may assist in the selection and use of the more widely used thermal technologies to provide optimal Predictive, Preventive and Personalized Medicine (PPPM). To achieve maximal effectiveness for cure, basic treatment precepts must be understood and adhered to, including: (1) proper patient selection; (2) treatment of the entire lesion; (3) providing adequate tumor margins.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Personalized medicine
- Hepatocellular carcinoma
- Locoregional therapy
- Treatment
- Radiofrequency ablation (RFA)
- Microwave ablation (MWA)
- Cryotherapy (CRYO)
- Alcohol ablation
9.1 Introduction
Ablation therapy is proving to be a major tool in the anti-cancer armamentarium. The superb diagnostic capabilities of CT, US, and MRI, along with IR techniques, have combined to allow percutaneous tumor ablation to become fairly widespread in availability. Ablation also may be performed at open surgery or laparoscopically.
The fundamental concept of ablation is that the extremes of temperature kill cancer [1]. Thus both heating and freezing methods are effectively tumoricidal. Heating options are via radiofrequency, laser, and microwave. The former is utilized most frequently, laser least, and microwave is in its early clinical experience.
Other primary methods of percutaneous tumor ablation include cryotherapy (CRYO) and direct chemical injection. The former currently uses argon as the freezing agent and helium for warm-up. While various agents have been injected for direct percutaneous injection into tumors, alcohol ablation, first described by Livraghi [2], is most effective, and has been utilized most frequently.
9.1.1 Mechanisms and Instrumentation for RFA
The mechanisms of tissue destruction differ with the various heating modalities. For radiofrequency ablation (RFA), the mechanism is ionic agitation that causes frictional heating. Tissue death occurs at 60 °C, but in clinical use, the probes generate over 90 °C temperatures. Care must be taken not to overheat, as this can cause charring which is counterproductive to heat therapy, and actually impedes heat propagation and eventual tumor killing. Probes are connected into a generator to disperse the heat effect.
Several type probes and systems exist. Each has features that attempt more complete killing for larger tumors. Thus systems have umbrella type tines, cooling mechanisms to decrease charring, multiple probes (similar to CRYO), different shapes, and variable flexibility to help tailor ablations. Various feedback systems from the different vendors are incorporated into the generators and monitors to guide the operator during the procedures.
9.1.2 Pre-Procedure Requirements
The procedure itself may be performed under US, CT, or MRI guidance. In the United States, CT is utilized most frequently. Contrast enhancement helps depict active tumor, areas of necrosis, and adjacent structures to be avoided. A pre-procedure biopsy is performed at the same setting (with quick stain pathology analysis) if not obtained previously. Coagulation parameters must be normalized prior to RFA. We use general anesthesia and antibiotics, although both are controversial; some operators prefer conscious sedation, and not all interventionalists prescribe prophylactic antibiotics.
9.1.3 The Procedure
Patients are positioned appropriately with access to the tumor entry site, without arms and metal or other artifacts to compromise the imaging appearances of the tumors. Probes must be placed such that, for cure, the entire tumor and a 1 cm circumferential safety margin of kill in normal liver tissue are obtained. Multiple tumors can be ablated in one or more sessions. Results are best with masses 3 cm or less in diameter, and with 3 tumors or fewer in number. Nonetheless, palliative killing of larger or multiple tumors can be an option as well. In the latter case, combination therapy may include ablation along with chemotherapy, radiation therapy, and/or surgery.
Alcohol may be infused by a percutaneous 22 g needle prior to RFA. A synergistic effect of the two ablation mechanisms has been documented [3]. In addition, alcohol may be used to “clean up” small areas of persistent or recurrent tumor [4]. The RFA is continued until the desired effective coagulation necrosis is achieved. Impedance and temperature are end points, depending on the various vendor algorithms. Typically on removal of the probes, cauterization of the tract is performed. This may diminish the likelihood of bleeding post-ablation.
Once the ablation is complete, general anesthesia is reversed, and the patient is observed in the recovery room. Patients are hospitalized overnight routinely, and discharged the following day if no major complications ensue and once they have recovered well; the vast majority of patients do go home the day after RFA.
9.1.4 Applicability
RFA knows virtually no limits in tumor killing. Thus, the spectrum of tumor cell types is nearly universal to the tumoricidal effects of RFA. Similarly, all varieties of carcinoma, sarcoma, and benign tumors may be treated with RFA. (RFA is not utilized for lymphoma typically, because of the diffuse multisystemic nature of the tumor, and the superiority of other treatment methods.) RFA is applicable in a wide spectrum of organs, as well. Very few sites in the body have not had RFA applied for tumor killing. (Cardiac ablation techniques are anti-arrhythmic, not anti-oncologic.)
A wide variety of liver lesions, histopathologically, has been successfully treated by RFA in our experience, and includes primary and metastatic tumors, vascular and sarcomatous cancers, as well as benign tumors. The latter typically are not treated unless symptoms (such as pain) prompt the need for therapy [5].
RFA can be effective treatment for pain related to tumor masses. Studies have documented the efficacy of RFA to treat pain in bones, soft tissues, and even internal viscera [6].
9.1.5 Complications
In most respects, the complications of RFA are those of biopsy or needle/catheter insertion in general. Thus, bleeding, infection, perforation of the gastrointestinal tract, pneumothorax, and death are potential generic complications that might occur with almost any interventional radiology (IR) procedure.
Several specific complications may result from RFA. An annoying, but non-life threatening complication from RFA is termed, “the Post Ablation Syndrome”. Presumably the Syndrome results from ablated necrotic tumors with resultant circulating toxins that cause a flu-like syndrome that may affect muscles, joints, and the overall wellness of the patient. The Syndrome likely correlates with the volume of killed tumor. While treatment is supportive, as with the “flu”, prevention may be achieved by performing ablation on large tumors in more than one session so as not to overload the tumoricidal effects on the body. The Syndrome can be more noxious in elderly patients, another caveat for prevention.
A second specific issue with RFA that is preventable is the unwanted effects of heat (similar for cryotherapy) on structures that need to be preserved; most importantly is the gastrointestinal (GI) tract that can be perforated or fistulized by the undesirable properties of the intense heat. Similarly the kidney, gallbladder, and diaphragm may be injured by the heat of RFA. Preventively, the technique of hydrodissection has been developed [7,8]. The goal of hydrodissection is to infuse sterile water or dextrose to displace structures protectively from the tumor being targeted by RFA. Most commonly, various GI structures (e.g. colon, duodenum, stomach) are protected by displacement from the masses. Buffer areas of 1 cm or greater by sterile water or dextrose may be created similarly to protect the gallbladder, pancreas, kidney, and diaphragm. Saline is not used, as it actually further conducts heat.
9.1.6 Follow-Up
Clinical follow-up is of course essential for ablation. How the patient responds, whether or not significant complications occur, overall morbidity and mortality from the procedure, underlying diagnoses, symptom control, recurrent disease, and eventual lifespan all are metrics to assess effectiveness of RFA. In addition, imaging follow-up offers important insights into many factors: prognosis, need for further therapy, complications, recurrent and/or persistent disease.
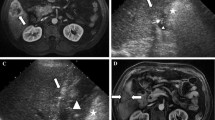
CT predominantly, along with PET/CT and MRI, provides the bulwark of imaging follow-up information. The hallmark of effective ablation is lack of contrast enhancement within the tumor, as well as a 1 cm circumferential safety margin around the entire mass. Nodular enhancement, irregular inhomogeneous enhancement, or vessels seen within the mass, indicate persistent or eventual recurrent disease.
9.1.7 Results of RFA and Other Forms of Ablation Therapy
The role of ablation technologies in the management of hepatocellular carcinoma has been well described in the literature, with numerous review articles available [2, 9–12]. However, to date no large randomized clinical trials have been performed that provide the treating clinician, or the patient, precise information in determining the best form of therapy for any given situation. It has been reported that at this time, percutaneous RFA may offer complete tumor kill in patients with lesions up to 3 cm in diameter, and it has comparable survival rates with partial hepatectomy and with fewer complications [10]. It has to be remembered that, in general, cancer control, but not cancer cure, is offered to cirrhotic patients because they have greater than a 10 % chance annually of developing new lesions once one tumor occurs. If tumor control is achieved, the outcome is defined by the progression of the liver disease [10].
The efficacy of RFA is related to the size of the liver tumor. It is accepted that the lesion should not exceed 2.5–3.0 cm to obtain complete necrosis [13]. It has been reported that certain microwave ablation (MWA) devices may allow successful treatment of lesions as large as 5 cm with an acceptable margin of safety [13]. Notwithstanding, RFA commonly is utilized for lesions greater than 3 cm in diameter, occasionally for palliative debulking rather than cure.
As stated above, the fundamental concept of ablation is that the extremes of temperature kill cancer. All of the commercially available devices are capable of achieving the required temperatures. The overall success of an ablation device in the clinical setting depends on how well the device can fulfill all of the treatment requirements in a given patient, as well as in a population of patients, with all of their similarities and unique features.
Guidelines may assist in the selection and use of the more widely used thermal technologies: RFA, MWA, and CRYO. To achieve maximal effectiveness for cure, basic treatment precepts analogous to those in surgery, must be understood and adhered to, including: (1) proper patient selection; (2) treatment of the entire lesion; and, (3) providing adequate tumor margins. For ablation therapies, certain additional considerations include: (1) avoidance of anatomic structures that influence effective deposition of energy, such as blood vessels that divert energy from the tumor (“heat sink” or “cold sink”); (2) avoiding tissue alterations that could influence energy deposition, such as too rapid increase in tissue impedance, tissue charring, and creation of microscopic gas bubbles; (3) ensuring complete coverage when overlapping zones of treatment are required so that no gaps of inadequately treated tumor cells remain; and, (4) ensuring an adequate treatment margin when the tumor is in proximity to sensitive or vital structures (e.g. GI tract or myocardium).
It is also important that when we evaluate the results of ablation that we recognize recurrent tumor as treatment failure and distinguish that from the presence of new tumor, especially in patients with hepatitis B and C. It is also important that the efficacy of ablation therapy is best evaluated by the presence or absence of contrast enhancement of viable tumor on contrast-enhanced CT (modified or mRECIST criteria), and that traditional RECIST/WHO criteria rely on decrease in tumor size. It is important to note that post ablation edema, tissue reaction and blood may give the appearance of “enlargement of the tumor” on CT, when it is rather the effect of successful ablation. Methods of combining evaluation techniques are being developed [12].
Conclusion
Ablation therapies are now an integral part of the menu of therapy for HCC. RFA procedures are generally safe and effective, with caveats and guidelines, and are at the time of this writing still considered the gold standard for percutaneous ablation. Alternative technologies, such as MWA, CRYO, interstitial laser thermotherapy (ILT), and percutaneous ethanol ablation are in use, with MWA showing promise for future development.
References
Cheung L, van Sonnenberg E, Morrison P et al (2005) Radiofrequency ablation therapy. CDR 28:1–6
Livraghi T (2011) Radiofrequency ablation of hepatocellular carcinoma. Surg Oncol Clin N Am 20:281–299
Shankar S, van Sonnenberg E, Morrison PR et al (2004) Combined radiofrequency and alcohol injection for percutaneous hepatic tumor ablation. Am J Roentgenol 183:1425–1429
Mamlouk MD, van Sonnenberg E, Morrison PR et al (2009, November 29) Indications and uses of alcohol in the RF/Cryo ablation era. Paper presented at RSNA, Chicago
Hedayati P, van Sonnenberg E, Shamos R, Gillespie T (2010) Treatment of a symptomatic focal nodular hyperplasia by percutaneous radiofrequency ablation. J Vasc Interv Radiol 21:582–585
Nair R, van Sonnenberg E, Shankar S et al (2008) Radiofrequency and alcohol ablation for pain relief in visceral and soft tissue tumors. Radiology 248:1067–1076
Goodacre BW, Savage C, Zwischenberger JB et al (2002) Salinoma window technique for mediastinal lymph node biopsy. Ann Thorac Surg 74:276–277
Brown S, van Sonnenberg E, Morrison P, Diller L, Shamberger R (2005) CT-guided radiofrequency ablation of pediatric Wilms tumor in a solitary kidney. Pediatr Radiol 35:923–928
Abrams P, Marsh JW (2010) Current approach to hepatocellular carcinoma. Surg Clin North Am 90:803–816
Guimaraes M, Uflacker R (2011) Locoregional therapy for hepatocellular carcinoma. Clin Liver Dis 15:395–421
Aronsohn A, Mohanty SR (2010) Current treatment strategies for hepatocellular carcinoma. Curr Cancer Ther Rev 6:199–206
Curley SA, Stuart KE, Schwartz JM, Carithers RL Jr (2012) Up-to-date. http://www.uptodate.com/contents/nonsurgical-therapies-for-localized-hepatocellular-carcinoma-radiofrequency-ablation-percutaneous-ethanol-injection-thermal-ablation-and-cryoablation/. Accessed 10 June 2012
Livraghi T, Meloni F, Solbiati L, Zanus G (2012) For the collaborative Italian group using AMICA system complications of microwave ablation for liver tumors: results of a multicenter study. Cardiovasc Intervent Radiol 35:868–874
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
van Sonnenberg, E., Berliner, L. (2015). Minimally Invasive Therapies for Hepatocellular Cancer: Ablation Therapies. In: Berliner, L., Lemke, H. (eds) An Information Technology Framework for Predictive, Preventive and Personalised Medicine. Advances in Predictive, Preventive and Personalised Medicine, vol 8. Springer, Cham. https://doi.org/10.1007/978-3-319-12166-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-12166-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-12165-9
Online ISBN: 978-3-319-12166-6
eBook Packages: MedicineMedicine (R0)