Abstract
This chapter reviews radiologic imaging of posterior cruciate ligament (PCL) and coexistent injuries, primarily focusing on the magnetic resonance imaging (MRI). Examples of normal ligamentous anatomy and injury are provided for comparison. The injuries are reviewed by compartment, with the goal of providing the orthopedic surgeon with pertinent information so that a comprehensive surgical plan can be determined prior to repair and/or reconstruction.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Posterior cruciate ligament (PCL)
- Posteromedial corner
- Medial collateral ligament (MCL)
- Lateral collateral ligament (LCL)
- Magnetic resonance (MR) imaging (MRI)
- Posterolateral corner
- Radiology
- Knee ligament injury
Introduction
Imaging is complementary to the history and physical examination in confirming suspected injuries. Imaging is especially valuable when the clinical examination is limited by large body habitus, guarding, and in the setting of complex injuries. Imaging, furthermore, decreases the chance of unsuspected and thus undiagnosed injuries, which if untreated may result in instability, repair failure, and early osteoarthritis [1]. Radiographic imaging provides evaluation of osseous injuries, both large and small. Radiographs should be scrutinized for small avulsion fractures not only because they are often unapparent on magnetic resonance imaging (MRI) but also that they alert us to other more substantial injuries. MRI evaluates directly for ligamentous injury and evaluates for coexistent injuries of the articular cartilage and menisci. MRI evaluation of the posterior cruciate ligament (PCL) as well as the medial and lateral stabilizers is the focus of this chapter.
Initial Radiographic Evaluation
Imaging protocols vary depending on preference, but at our institution this typically includes standing anteroposterior (AP) views of both knees, a tunnel view, 30° flexion lateral view, and sunrise view of the patella. Radiographs may demonstrate indirect and direct signs of PCL tear, for example, radiographic posterior drawer and PCL avulsion fracture [2] (Figs. 6.1 and 6.12b respectively). The “reverse Segond” fracture is a subtle avulsion fracture on X-ray, and is associated with PCL tear [3] (Fig. 6.2). The “arcuate sign” is an osseous avulsion of the fibular head involving some combination of the arcuate complex (arcuate ligament, fabellofibular, popliteofibular ligaments) and/or the conjoined insertion of fibular collateral ligament (FCL)/biceps femoris. Both injuries have a high association with PCL tears [4–6] (Fig. 6.3).
MRI
When evaluating the dynamic and static knee stabilizers, the obtained MRI should be of high resolution. Optimally, imaging should be on a 1.5-Tesla magnet or higher, with small field-of-view (FOV) images of the knee, and should be tailored to evaluate ligaments, tendons, and cartilage. That is to say, large FOV images that cover from the mid femur through the mid tibia result in lower-resolution images, and potentially missed pathology. A high-quality exam is important to accurately evaluate the large stabilizers, but it is even more important to evaluate the complex, blending medial and lateral capsular stabilizers, subtle coexistent meniscal tears, and articular cartilage defects. MRI should be performed in the acute setting, because as normal healing progresses and edema resolves, injuries may become less conspicuous.
PCL
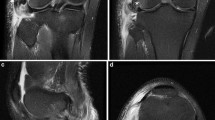
The knee is typically imaged in extension, where the anterior cruciate ligament (ACL) is taut and straight, and the PCL is lax and curved. This position is comfortable for the patient, and allows for the technologist to utilize a knee coil for high-resolution MR images. Unlike the ACL, the normal PCL is homogeneously low signal on both T2 and proton density (PD) weighted sequences, lacking internal striations that may be seen in the normal ACL [7, 8] (Fig. 6.4). The knee is not typically imaged in flexion, because a knee coil cannot be utilized, resulting in lower resolution images. However, when imaged in flexion, the PCL appears taut and remains homogeneously low in signal (Fig. 6.5). The normal PCL should measure 6 mm or less, when measured from anterior to posterior in the sagittal plane [9]. Like the ACL, the PCL has two functional bundles, the posteromedial bundle (PMB) and anterolateral bundle (ALB), named according to their femoral attachments [10]. In the axial plane, the separate bundles can often be distinguished from one another (Fig. 6.6). The meniscofemoral ligaments can often be seen coursing adjacent to the PCL, with the posterior meniscofemoral ligament (Wrisberg) being more common than the anterior meniscofemoral ligament (Humphey). Not uncommonly both meniscofemoral ligaments are present [11].
a and b Normal PCL. Sagittal PD nonfat-suppressed image and sagittal T2 fat-suppressed image demonstrate normal appearance of PCL. The PCL is not taut like ACL when imaged in extension and thus has curved rather than straight morphology. The normal PCL is hypointense on PD and T2 weighted images. PCL posterior cruciate ligament, PD proton density, ACL anterior cruciate ligament
a and b Normal PCL in flexion. Coronal PD nonfat-suppressed and T2 fat-suppressed image shows knee imaged in mild flexion without a knee coil. PCL is taut in flexion rather than usual curved appearance in extension. Note lower quality images due to imaging without a knee coil. PCL posterior cruciate ligament, PD proton density
MRI is the radiologic study of choice in diagnosing acute PCL tears [7]. The sagittal MRI sequences quickly screen for PCL injury and determine the site of failure at the femoral attachment, midsubstance, or tibial attachment. MRI readily demonstrates acute high-grade injuries to the PCL (Figs. 6.7, 6.8, 6.9). However, unlike ACL tears, PCL tears are more commonly partial rather than complete [7]. In the sagittal plane, partially torn PCL tears often demonstrate a “stretched” appearance with thickening greater than 6 mm and intrasubstance signal changes, the latter of which may be seen only on PD sequence but not on T2 weighted sequences [9]. There are two potential pitfalls if one relies only on the sagittal plane when evaluating PCL tears. First, partial tears may be interpreted as complete tears. Second, mucoid degeneration may mimic a PCL tear in the setting of a functionally stable ligament. In this regard, we have found that the axial plane is complementary to the sagittal plane and can safeguard against the aforementioned pitfalls.
Complete PCL tear. a Complete midsubstance disruption with intact femoral and tibial attachments intact. Note subjacent Humphries ligament (arrow). b Axial image shows empty notch (star) other than ACL (arrow), consistent with complete PCL tear involving PM and AL bundles. PCL posterior cruciate ligament, ACL anterior cruciate ligament, PM posteromedial, AL Anterolateral
Complete PCL tear. a Fat-suppressed T2 sagittal demonstrates complete proximal disruption of PCL. Note overlying Wrisburg ligament (arrow). b Axial image shows empty notch (star) other than ACL (arrow), consistent with complete tear involving PM and AL bundles. PCL posterior cruciate ligament, ACL anterior cruciate ligament, PM posteromedial, AL anterolateral
In the axial plane, the anterolateral and PMBs are often apparent and side by side, so we can better determine if the tear is partial or complete, depending on if one or both bundles are torn (compare Figs. 6.7 and 6.10 respectively). Mucoid degeneration of the ACL has been described as a pitfall resulting in false positive ACL tears on MRI [12]. More recently, mucoid degeneration of the PCL was described [13]. Both mucoid degeneration and partial PCL tears may demonstrate thickening and intrasubstance signal changes in the sagittal plane. The axial images help us to distinguish mucoid degeneration from PCL tear, because the former demonstrates the “tram-track” sign. The tram-track sign is defined as a single, linear striation in the PCL that does not surface, so is surrounded by low signal in all planes [13] (Fig. 6.11). In contradistinction, incomplete PCL tears demonstrate multiple heterogeneous internal striations that extend to the outer surface somewhere along the course of the ligament in the sagittal and/or axial planes (compare Figs. 6.10 and 6.11).
Partial PCL tear. a Sagittal and axial T2 fat-suppressed images showing moderate grade midsubstance PCL injury. Intrasubstance striated signal changes with no visualization of tibial attachment. b Arrow shows normal ACL. PCL is diminutive with intact AL bundle (arrowhead) and fluid signal at expected location of torn PM bundle (star). PCL posterior cruciate ligament, ACL anterior cruciate ligament, AL anterolateral, PM posteromedial
PCL mucoid degeneration. a Nonfat-suppressed proton density (PD) image demonstrates mild linear intrasubstance fluid bright signal changes. b Axial T2 fat-suppressed image midsubstance of PCL. Signal changes do not reach the surface of the ligament on sagittal or axial sequences. Femoral and tibial attachments are intact. Note Humphries ligament (arrowhead). PCL posterior cruciate ligament
Osseous avulsion of PCL. a Nonfat-suppressed PD images show intact PCL with osseous avulsion of PCL at tibial attachment (arrows). b Corresponding X-ray shows osseous avulsion as well. Note hypointense fracture margins on MRI and sclerotic fracture margins on X-ray, consistent with chronic rather than acute injury. PCL posterior cruciate ligament, PD proton density, MRI magnetic resonance imaging
Although chronic PCL injuries may be apparent on MRI (Figs. 6.12 and 6.13), MRI is not as sensitive in diagnosing chronic compared to acute PCL tears [14, 15]. Furthermore, MRI may appear normal as soon as 3 months following low- to moderate-grade PCL injuries [16]. Stress radiograph s, such as the Telos system, are accurate in their ability to evaluate for functional instability of the PCL [17, 18]. Given the above challenges in diagnosing chronic partial PCL tears on MRI, stress radiographs are useful to evaluate functional stability of the PCL in the presence of an indeterminate MRI that demonstrates mild PCL thickening and/or mild PCL signal changes (Fig. 6.14).
Two patients with high-grade chronic tears. a T2 fat-suppressed image shows remote, complete nonosseous avulsion of PCL at tibial attachment with proximal retraction. b PD nonfat-suppressed images show marked attenuation of PCL with nonvisualization of femoral attachment, consistent with chronic tear. PCL posterior cruciate ligament, PD proton density
a and b Stress radiographs of both knees with history of remote injury and only mildly thickened PCL on MRI (MRI not shown). Note posterior displacement of the right tibia on the femur in right knee with stress, with ~ 10-mm corrected side: side differential compared to normal left knee. PCL posterior cruciate ligament, MRI magnetic resonance imaging
Lateral and Posterolateral Corner Stabilizers
The large lateral stabilizers such as the iliotibial band (ITB), FCL, biceps tendon, and the conjoined insertion of biceps and FCL are well seen on MRI , and hence injuries are accurately characterized. MRI evaluation of the smaller ligamentous and capsular structures, such as the popliteofibular ligament and capsular ligaments, are challenging due to their diminutive size, oblique course relative to traditional imaging planes, and anatomic variation [1].
The FCL courses obliquely from anterior to posterior in the lateral and posterolateral aspect of the knee. The obliquely oriented biceps femoris courses from posterior to anterior. These two structures converge to form a “conjoined tendon insertion” as they insert onto the lateral aspect of the fibular head [19, 20]. Both structures are homogeneously low in signal on all pulse sequences, with the exception of their conjoined insertion, which we note often demonstrates faint, thin striations (Fig. 6.15). Injuries to the biceps, FCL, and their conjoined insertion are relatively straightforward due to the size of these structures. Figures 6.16, 6.17, and 6.18 demonstrate various injuries to the FCL.
Normal FCL, biceps, and popliteus origin on coronal T2 fat-suppressed images. a Normal FCL (arrowheads) and partially imaged biceps tendon at their conjoined insertion (arrow). Note popliteus origin as well (circle). b Normal biceps tendon insertion is striated (arrow), which does not indicate pathology. FCL fibular collateral ligament
Complete disruption of FCL. Coronal T2 fat-suppressed image with nonvisualization of FCL (arrowheads) with the exception of edematous distal fibers at conjoined insertion, consistent with high-grade injury. Partially imaged biceps insertion was intact (arrow). Popliteus origin and popliteofibular ligament were intact (not shown). FCL fibular collateral ligament
The popliteus tendon and popliteofibular ligament are strong stabilizers of the PLC of the knee. The origin of the popliteus tendon is intra-articular from a sulcus on the lateral femoral condyle, inferior and anterior to the proximal attachment of the FCL [19, 20]. As the popliteus tendon wraps posteromedially, it become extra-articular at the meniscal hiatus and gives off a branch that acts as a pulley; this popliteofibular ligament courses laterally and inserts on the medial aspect of the fibular styloid process, medial to the attachment of the fabellofibular ligament and arcuate ligament [19–21].
The popliteus origin is consistently seen on MRI (Fig. 6.15a). Although it is generally a low signal on all pulse sequences, we often see mild signal changes and striations in the absence of injury. The normal popliteofibular ligament is consistently present [22], but can be difficult to visualize on MRI [19, 23]. The popliteofibular ligament courses on average approximately 40° to the horizontal plane [24] and is best seen on coronal sequences (Fig. 6.19). At times, fat surrounding the ligament makes it more conspicuous on traditional nonfat-suppressed PD or T2 weighted sequences (Fig. 6.20). Complicating the evaluation of this ligament is that there is known anatomic variation, whereas at times the popliteofibular ligament may have a more vertical course, and multiple bands have been described [17, 19, 20, 25].
Injury to the popliteus complex may occur throughout its course (Figs. 6.21, 6.22, 6.23, 6.24, 6.25, 6.26). An empty popliteus notch is indicative of tear (Fig. 6.21). An injury may occur in isolation, but multiligament involvement is common. A torn tendon may be retracted far proximally and become entrapped in the joint (Fig. 6.22). Despite the difficulties in visualizing the noninjured popliteofibular ligament, injury to the popliteofibular ligament is often apparent because the surrounding edema makes the ligament more conspicuous. Injuries run the gamut from low-grade sprains with mild surrounding edema to complete avulsion (Figs. 6.24, 6.25, 6.26). If no edema is present posterolaterally, acute injury to the popliteus and posterior capsule (discussed below) is unlikely, despite nonvisualization of these structures on MRI .
High-grade posterolateral corner injury. Coronal T2 fat-suppressed image showing popliteus avulsion from the femoral attachment, displaced into the lateral joint (arrowhead), partially obscured by the superimposed lateral meniscus (star). Nonvisualized FCL and conjoined insertion, completely torn at femoral attachment (arrows). FCL fibular collateral ligament
The mid-lateral capsule is specifically the anterior oblique band (AOB), which is formed by contributions from the ITB and FCL [26]. The normal mid-lateral capsule is located in the interval between the ITB and FCL, and is low signal and relatively thin (Fig. 6.27). Figure 6.28 demonstrates injury to the mid-lateral capsule. Avulsion fracture at the tibial attachment of the AOB is termed the Segond fracture [26] (Fig. 6.29).
Segond fracture. Coronal T2 fat-suppressed image showing Segond fracture, which is osseous avulsion of the AOB at its tibial attachment (arrow). Also, note injury to superficial and deep MCL (circle) with osseous avulsion at meniscofemoral ligament attachment. AOB anterior oblique band, MCL medial collateral ligament
The posterolateral capsule is formed by a number of structures, most notably the fabellofibular and arcuate ligaments, with contributions from the popliteus and lateral gastrocnemius. These smaller capsular structures are not consistently present in dissection, vary in size and thickness, and can be present alone or in combination [20, 22, 27–30]. An injury to the posterolateral capsule is challenging to characterize due to the anatomic variation in this region, the small size of these structures, and location that is not well evaluated with traditional imaging planes [1]. Knowledge of the insertional geometry of the popliteofibular ligament and arcuate complex onto the fibular head is instrumental to accurate diagnosis [31]. In the setting of PLC injury, marrow edema may be present in the fibular head, and the surrounding soft tissue edema is helpful in highlighting the normal anatomy (Fig. 6.30). Soft tissue edema, disorganization of fibers, and fluid tracking posterior to the popliteus tendon are indicative of moderate to high-grade injury of the posterolateral capsule [27] (Fig. 6.31).
Lateral capsule on coronal and sagittal T2 fat-suppressed images respectively. a Edema surrounding and thus highlighting thin V shape of medial and lateral limbs of arcuate ligament complex (arrowheads). Note adjacent biceps (arrow). b Edema does not track posterior to popliteofibular ligament insertion to fibular styloid process on lateral view (circle), so post capsule is intact
Moderate- to-high-grade injury to the popliteofibular ligament on coronal and sagittal T2 fat-suppressed images, respectively. a Note disorganization of fibers of the posterior capsule on coronal image (circle). b There is fluid signal posterior to the fibular head on sagittal image (circle), consistent with high-grade posterolateral capsule injury
Medial and Posteromedial Stabilizers
Warren initially described three layers stabilizing the medial knee, which includes the sartorius fascia, superficial medial collateral ligament (MCL), and deep MCL [32]. The prominent superficial component of the MCL in the middle third of the knee is traditionally referred to as the MCL, which, due to its size, is well seen in all planes and on all sequences. The more superficial sartorius fascia is thin, so is best seen without fat suppression, and may be inconspicuous on T2 fat-suppressed sequence. The deep MCL is likewise thin, but is located just deep to the MCL. The deep MCL forms the capsule in the middle third of the knee, and is made up of the meniscotibial (MT) and meniscofibular (MF) ligaments [32, 33]. The deep MCL is best seen when fluid signal or fat is interposed between the superficial and deep MCL (Fig. 6.32). If the deep MCL is flush against the larger overlying MCL, it may be hard to distinguish (Fig. 6.33).
Low-grade MCL sprain. Coronal T2 fat-suppressed image showing fluid/edema superficial to MCL displaces the overlying sartorius fascia (arrows). As is often the case, the meniscofemoral and meniscotibial ligaments are taut against and therefore blend with and are indistinguishable from overlying superficial MCL. MCL Medial collateral ligament
The imaging criteria utilized for all other ligamentous injuries are also used for the medial stabilizers [34, 35]. Low-grade injuries demonstrate periligamentous signal changes (edema and/or hemorrhage) without internal signal changes or fiber discontinuity. Moderate-grade injuries demonstrate intrasubstance signal changes in addition to periligamentous signal changes, sometimes with areas of partial discontinuity. High-grade tears demonstrate complete fiber discontinuity, often exemplified by a wavy ligament. Care should be taken as to which layers of the MCL are torn, as well as describing the location of injury (i.e., at the femoral attachment, tibial attachment, or midsubstance). Figures 6.34, 6.35, 6.36, 6.37, and 6.38 demonstrate various MCL injuries and descriptions of these injuries. Of note, atraumatic edema from osteoarthritis and/or meniscal tear may mimic low-grade MCL tear [36, 37].
Moderate to high-grade MCL injury. Coronal T2 fat-suppressed image showing focal disruption of superficial MCL near the femoral attachment (arrow) and osseous avulsion of MF ligament (arrowhead). Tibial attachment of superficial MCL and meniscotibial ligament are both intact. MF meniscofibular, MCL medial cruciate ligament
When one moves from the middle third to the posterior third of the knee, the deep MCL blends with the posterior oblique ligament (POL) and capsule. The posteromedial capsule is further reinforced by contributions from fibers of the medial gastrocnemius as well as the semimembranosus [27, 32, 33, 38]. The POL is well visualized on MRI and, like the deep MCL, has MF and MT components (Fig. 6.39). Injury to the POL is graded similar to the MCL, and may be diffuse (Fig. 6.40), may occur to the meniscofemoral or meniscotibial components (Fig. 6.41), may strip off the meniscus (meniscocapsular separation; Fig. 6.42), or may pull off the periphery of the meniscus in the form of a longitudinal vertical tear (Fig. 6.43). The POL serves as a bridge between the meniscus and the semimbranosus tendon, and this coupling of the meniscus to the semimembranosus provides motor function to the meniscus via its capsular attachments, resulting in meniscal retraction during knee flexion [39, 40]. Tear in any of the above locations has the potential to decouple the meniscus and semimembranosus tendon, increasing risk of meniscal tear.
Normal POL ligament. Coronal T2 fat-suppressed image showing normal POL stabilizing the medial meniscus (arrows). The appearance is similar to MF and MT ligaments seen in middle 1/3 of knee, but is located posteriorly, and there is no overlying MCL. MF meniscofemoral, MT meniscotibial, POL posterior oblique ligament, MCL medial collateral ligament
Conclusion
High-quality radiographs and MRI accurately evaluate the normal anatomy and acute injuries of the PCL , medial knee, and lateral knee. X-rays complement MRI by evaluating for fractures, gross ligamentous injury, and can pick up tiny avulsion fractures that may be subtle or missed on MRI. MRI not only confirms clinically suspected injuries but helps to diagnose unsuspected injuries as well. MRI is complementary, but less accurate in the evaluation of chronic injuries, and may be supplemented with functional imaging in this setting. Imaging studies combined with history and clinical exam and functional studies together provide a precise diagnosis to plan the complex ligamentous repair and reconstruction.
References
Malone WJ, Verde F, Weiss D, Fanelli GC. MR imaging of knee instability. Magn Reson Imaging Clin N Am. 2009 vi–vii;17(4):697–724.
Gottsegen CJ, Eyer BA, White EA, Learch TJ, Forrester D. Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics. 2008;28(6):1755–70.
Escobedo EM, Mills WJ, Hunter JC. The “reverse Segond” fracture: association with a tear of the posterior cruciate ligament and medial meniscus. AJR Am J Roentgenol. 2002;178(4):979–83.
Huang GS, Yu JS, Munshi M, Chan WP, Lee CH, Chen CY, et al. Avulsion fracture of the head of the fibula (the “arcuate” sign): MR imaging findings predictive of injuries to the posterolateral ligaments and posterior cruciate ligament. AJR Am J Roentgenol. 2003;180(2):381–87.
Juhng SK, Lee JK, Choi SS, Yoon KH, Roh BS, Won JJ. MR evaluation of the “arcuate” sign of posterolateral knee instability. AJR Am J Roentgenol. 2002;178(3):583–8.
Shindell R, Walsh WM, Connolly JF. Avulsion fracture of the fibula: the ‘arcuate sign’ of posterolateral knee instability. Nebr Med J. 1984;69(11):369–71.
Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME. MR imaging of the posterior cruciate ligament: normal, abnormal, and associated injury patterns. Radiogr : Rev Publ Radiolog Soc N Am Inc. 1995;15(3):551.
Roberts CC, Towers JD, Spangehl MJ, Carrino JA, Morrison WB. Advanced MR imaging of the cruciate ligaments. Magn Reson Imaging Clin N Am. 2007;15(1):73–86.
Rodriguez W, Jr, Vinson EN, Helms CA, Toth AP. MRI Appearance of Posterior Cruciate Ligament Tears. Am J Roentgenol. 2008;191(4):W155–9.
Amis AA, Gupte CM, Bull AMJ, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2006;14(3):257–63.
Bintoudi A, Natsis K, Tsitouridis I. Anterior and posterior meniscofemoral ligaments: MRI evaluation. Anat Res Int 2012;2012:839724–5.
Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol. 2004;182(5):1283–7.
Vinson EN, Helms CA. Imaging for evaluation of posterolateral corner injury. J Knee Surg. 2005;18(2):151–6.
Tewes DP, Fritts HM, Fields RD, Quick DC, Buss DD. Chronically injured posterior cruciate ligament: magnetic resonance imaging. Clin Orthop Relat Res. 1997;335:224–32.
Christopher TJS, James PR, Neil PT. The accuracy of magnetic resonance imaging in diagnosing chronic posterior cruciate ligament injury. The Knee. 2004;11(4):265–70.
Shelbourne KD, Jennings RW, Vahey TN. Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg. 1999;12(4):209–13.
Stäubli HU, Birrer S. The popliteus tendon and its fascicles at the popliteal hiatus: gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy. 1990;6(3):209–20.
Schulz MS, Steenlage ES, Russe K, Strobel MJ. Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Joint Surg Am. 2007;89(2):332–8.
Munshi M, Pretterklieber ML, Kwak S, Antonio GE, Trudell DJ, Resnick D. MR imaging, MR arthrography, and specimen correlation of the posterolateral corner of the knee: an anatomic study. AJR Am J Roentgenol. 2003;180(4):1095–101.
Diamantopoulos A, Tokis A, Tzurbakis M, Patsopoulos I, Georgoulis A. The posterolateral corner of the knee: evaluation under microsurgical dissection. Arthroscopy. 2005;21(7):826–33.
Brinkman JM, Schwering PJ, Blankevoort L, Kooloos JG, Luites J, Wymenga AB. The insertion geometry of the posterolateral corner of the knee. J Bone Joint Surg Br. 2005;87(10):1364–8.
Watanabe Y, Moriya H, Takahashi K, Yamagata M, Sonoda M, Shimada Y, Tamaki T. Functional anatomy of the posterolateral structures of the knee. Arthroscopy. 1993;9(1):57–62.
De Maeseneer M, Shahabpour M, Vanderdood K, De Ridder F, Van Roy F, Osteaux M. Posterolateral supporting structures of the knee: findings on anatomic dissection, anatomic slices and MR images. Eur Radiol. 2001;11(11):2170–7.
LaPrade RF, Ly TV, Wentorf FA, Engebretsen L. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31(6):854–60.
Ullrich K, Krudwig WK, Witzel U. Posterolateral aspect and stability of the knee joint. I. Anatomy and function of the popliteus muscle-tendon unit: an anatomical and biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2002;10(2):86–90.
Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, Yu J, Resnick D. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219(2):381–6.
De Maeseneer M, Van Roy P, Shahabpour M, Gosselin R, De Ridder F, Osteaux M. Normal anatomy and pathology of the posterior capsular area of the knee: findings in cadaveric specimens and in patients. AJR Am J Roentgenol. 2004;182(4):955–62.
Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982;64(4):536–41.
Maynard MJ, Deng X, Wickiewicz TL, Warren RF. The popliteofibular ligament. Rediscovery of a key element in posterolateral stability. Am J Sports Med. 1996;24(3):311–6.
Sudasna S, Harnsiriwattanagit K. The ligamentous structures of the posterolateral aspect of the knee. Bull Hosp Jt Dis Orthop Inst. 1990;50(1):35–40.
Lee J, Papakonstantinou O, Brookenthal KR, Trudell D, Resnick DL. Arcuate sign of posterolateral knee injuries: anatomic, radiographic, and MR imaging data related to patterns of injury. Skeletal Radiol. 2003;32(11):619–27.
Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61(1):56–62.
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000–10.
Schweitzer ME, Tran D, Deely DM, Hume EL. Medial collateral ligament injuries: evaluation of multiple signs, prevalence and location of associated bone bruises, and assessment with MR imaging. Radiology. 1995;194(3):825–9.
Stoller DW. Magnetic resonance imaging in orthopaedics and sports medicine. 3rd ed. Baltimore: Lippincott Williams & Wilkins; 2007. pp. 553–4.
Bergin D, Keogh C, O’Connell M, Rowe D, Shah B, Zoga A, et al. Atraumatic medial collateral ligament oedema in medial compartment knee osteoarthritis. Skeletal Radiol. 2002;31(1):14–8.
Bergin D, Hochberg H, Zoga AC, Qazi N, Parker L, Morrison WB. Indirect soft-tissue and osseous signs on knee MRI of surgically proven meniscal tears. AJR Am J Roentgenol. 2008;191(1):86–92.
Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55(5):923–40.
Hughston JC. Knee ligaments:injury and repair. St. Louis: Mosby Year-Book; 1993.
Sims WF, Jacobson KE. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med. 2004;32(2):337–45.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Malone, W., Stuelke, S., Snowden, R., Salesky, J. (2015). MRI of PCL, Posteromedial, and Posterolateral Corner Injuries of the Knee. In: Fanelli, MD, G. (eds) Posterior Cruciate Ligament Injuries. Springer, Cham. https://doi.org/10.1007/978-3-319-12072-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-12072-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-12071-3
Online ISBN: 978-3-319-12072-0
eBook Packages: MedicineMedicine (R0)