Abstract
Chemotherapy is the mainstay in the treatment of various cancers for several decades; however, it suffers several clinical limitations. For example, anticancer drugs are often nonselective and are taken up by all forms of cells. Non-selectivity of the agents usually results in significant toxicity to normal cells, thus resulting in poor prognosis for patients. Hence, to improve the therapeutic efficacy of chemotherapy, improving the selectivity of anticancer drug is highly desired. Prodrug conjugation is one of the most beneficial strategies to enhance selectivity and efficacy of a chemotherapy drug. The classical prodrug approach is to overcome physicochemical (e.g., solubility, chemical instability) or biopharmaceutical problems (e.g., bioavailability, toxicity) associated with common anticancer drugs via a simple chemical modification. On the other hand, here we discuss targeted prodrug systems for delivering anticancer agents specifically to tumor cells, thereby sparing normal cells. This chapter focuses on various synthetic strategies in designing targeted prodrug conjugates and its rationale for cancer treatment. Various tumor-targeting ligands that are currently being explored are critically discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Polymeric prodrug conjugates
- Targeted drug delivery systems
- Anticancer drugs
- Peptide and proteins and antibody
1 Introduction
The primary dearth of treatment in chemotherapy is lack of molecular selectivity and severe toxicity associated from an anticancer drug. In general, chemotherapeutic drugs responds through anti-proliferative mechanisms; or by preventing cell cycle at a specific phases rather than producing a toxic effect to particular site or types of cancer cells [1]. Hence, for the effective anticancer therapy, polymeric prodrug conjugation methodology represents one of the most promising approaches in achieving selective chemotherapy. Many efforts in reducing the systemic toxicity of chemotherapeutic moieties have been clinically explored (Fig. 11.1). In particular, polymeric prodrug conjugate is a chemical modification of a biologically inert component which is transformed to its active form, in vivo [2, 3]. Polymeric forms (e.g., poly(ethylene glycol) (PEG)) commonly referred in literature as “PEGylation ” is a polymeric prodrug approach, offering an important tool to enhance the pharmacodynamics (PD) of the active pharmacologic component via a simple chemical alteration. Traditional prodrug design aims to offer: (1) enhanced aqueous solubility, chemical stability, brain permeability, and oral or local absorption of a drug; and (2) reduced undesired pre-systemic metabolism, and toxicity [4, 5].
Advances in drug delivery systems representing varied architectures, physicochemical traits such as size, shape, and surface charge (modified from [6])
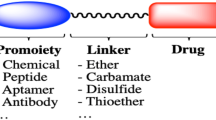
An ideal polymeric prodrug conjugate system typically consists of multiple components as represented in Fig. 11.2.
-
1.
A polymer as a drug delivery vehicle
-
2.
Drug, protein or peptide as a biological active component
-
3.
A spacer molecule and targeting moiety
Following approaches are generally used to target anticancer prodrugs to the tumor or cancer cells [7, 8]: (1) Passive Drug targeting and (2) Active Drug targeting.
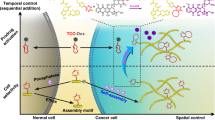
Passive Drug Targeting: In passive targeting, drug is delivered to the targeted site by conjugating it with polymer which releases the drug outside the targeted site due to altered environmental conditions as represented in Fig. 11.3a. The general features of tumors and many inflamed areas of body include leaky blood vessels and poor lymphatic drainage which passively provides increased retention of macromolecules into tumor [9–12]. This phenomenon is commonly referred to as Enhanced Permeability and Retention (EPR) effect [9]. EPR effect is primarily a passive targeting due to the accumulation of prodrug, into the tumor. The phenomenon mainly occurs owing to hampered lymphatic drainage which allows them to release the drug into the tumor milieu. However, passive targeting approach has several limitations. This is because targeting of the cancer cells is not always achieved as the diffusion of some drugs is insufficient and the random chemical approach makes it difficult to control the process. The lack of control is expected to lead into multiple-drug resistance (MDR). This situation results in resistance of cancer cells towards one or more drugs, thereby leading to failure of chemotherapy treatments. Moreover, it is known that certain tumors do not show the EPR effect, and the permeability of vessels is unpredictable throughout tumor which further limits the passive targeting approach [13]. On the other hand, the more efficient way to obtain targeting is by “active targeting” process.
(a) Active and passive targeting approaches though prodrug system, (b) (1) prodrug is docked at cell surface by ligand–receptor interaction and then internalized by tumor cells through receptor-mediated endocytosis , (2) transport of prodrug in membrane limited organelles, (3) fusion with lysosomes, (4) finally, drug is released intracellularly on exposure to lysosomal enzymes or lower pH (pH 6.5 to <4.0) [15, 16]
Active Drug Targeting : Active targeting approach involve interactions between specific biological systems, e.g., ligand–receptor, antigen–antibody, enzyme–substrate (Fig. 11.3a [14]). Active targeting is achieved by targeting ligand molecules that may interact with specific receptors on the cell surfaces—along with the bioactive prodrug system (Fig. 11.3b), designed by variety of synthetic conjugation methods. Most commonly used targeting components are small organic molecules, antibodies (mAbs), peptide ligands, sugar residues, aptamers (specific to particular receptors), selectins, antigens, and mRNAs overexpressed in targeted cells or organs. It is imperative that the targeting moiety binds with high selectivity to molecular receptors that are uniquely overexpressed on the cell surface.
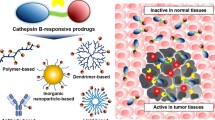
2 Prodrug Systems for Targeted Drug Delivery
The critical requirements for achieving selective targeting of prodrug to tumors are as follows: (1) it should be highly stable in blood circulation, (2) higher bio-distribution to the targeted site, (3) adequate contact time with the target, (4) sufficient retention by the target, (5) retention of drug potency, and (6) adequate clearance fate of non-targeted compound [17]. Polymer therapeutics with various polymeric architectures have been reported to achieve cellular targetability and EPR effect (Fig. 11.4). Similarly, Table 11.1 shows different types of targeting through ligands, and their specific targets through various drug delivery systems. Furthermore, to target specific biological molecules (e.g., enzymes, peptide transporters, antigens) that are overexpressed in tumor cells in comparison to normal cells, new promising anticancer prodrugs can be designed which includes:
(a-e) Different polymer therapeutics with various architectures for delivering biological actives (reproduced from [3])
-
1.
Enzyme-activated prodrugs—antibody-directed enzyme prodrug therapy (ADEPT) and gene-directed enzyme prodrug therapy (GDEPT) [17].
-
2.
Targeting-ligand conjugated prodrugs—antibody–drug conjugates, peptide–drug conjugates, aptamer–drug conjugates, and folic acid–drug conjugates [18].
-
3.
Enzyme-cleavable prodrugs.
-
4.
Membrane transporter-associated prodrugs.
-
5.
Polymeric prodrug conjugates.
The section below describes the classification and mechanisms of targeting.
3 Type of Targeting Moieties
Targeting agents can be classified broadly as proteins (mainly antibodies and their fragments), nucleic acids (aptamers), or other receptor ligands (peptides, vitamins, and carbohydrates) as shown in Fig. 11.5.
(a) Various targeting molecules such as a monoclonal antibody or antibodies’ fragments, non-antibody ligands, and aptamers. (b) Affinity and selectivity can be increased by dimerization of ligand or by screening for conformation-sensitive targeting agents such as intact antibodies and their fragments as well as antibodies, avimers and nanobodies (reproduced from [19])
4 Implications of Molecular Targeting in Anticancer Therapy (e.g., CDK Inhibitors, mTOR, IGFR, VEGF)
The implementation of targeted cancer therapy for individual patient has revolutionized the existing ways for cancer therapy. There is an increasing importance of targeted therapy in the treatment of several cancer entities (e.g., colon, NSCLC, breast, lymphoma, and malignant melanoma) and its molecular targets such as human epidermal growth factor 2 (HER2) [22], epidermal growth factor receptor (EGFR) [23], cyclin-dependent kinase inhibitors (CDK inhibitor) [24], vascular endothelial growth factor (VEGF), etc. [25, 26]. However, the key issue in implementing targeted therapy may only be effective when the tumor carry certain molecular features; otherwise they can be ineffective or can create unwanted side effects. For example, panitumumab is active against colon cancer only when the tumor is Kirsten rat sarcoma viral oncogene (KRAS) wild type [27].
In order to avoid such limitations and designing diagnostic analysis of solid and hematological tumors, identifying target genes is an essential step. In order to have an identification process, the laboratories explore high-end techniques, such as FISH assay, PCR, HPLC, protein arrays, DNA/RNA-array technology which are used to precisely detect the genetic alterations in the diseased state. For example, breast cancer is characterized by overexpression of HER2 which has been known to be more aggressive disease progression and a poorer prognosis [28, 29]. Hence, many researchers have focused on HER2 inhibitors as potential anticancer target which is achieved through gene therapy or by using drugs as Trastuzumab [30]. However, patients with HER2 positive breast cancer developed resistance towards the first FDA-approved therapeutic antibody for metastatic breast cancer “Trastuzumab” through hyperactivation of the phosphatidylinositol 3-kinase (PI3K)/Akt/mTOR signaling pathway [31]. The PI3K/Akt/mTOR signaling cascade has important regulatory functions in normal and oncogenic cellular growth, survival, proliferation, migrations and metabolism [32]. Several studies have shown that second mutations in this signaling pathway confers resistance mechanism to HER2-targeted therapies and direct inhibition of PI3K/Akt/mTOR signaling cascade may overcome trastuzumab resistance [33, 34]. Hence, combination of Trastuzumab and Anastrozole is targeted towards MAPK pathways and Akt pathway [35]. Likewise, inhibition of mTOR with drug Everolimus is efficacious when combined with Trastuzumab [36]. Recently, US FDA has approved Trastuzumab with Emtansine as a first antibody-drug conjugate for treating HER2-positive metastatic breast cancer [20]. In addition to many other molecular targets, sialic acid, a derivative of neuraminic acid, is one of the major targets in developing therapeutic treatment in cancer patients as hypersialylation has been shown to contribute cancer cell progression and metastasis [37]. However, till date, there is no therapeutic drug developed to interfere with sialic acid synthesis which might offer better treatment approach for cancer patients. Sialic acid as a targeting moiety with PEGylated doxorubicin (Dox) targeted prodrug conjugate demonstrated significant antitumor activity compared to free Dox and non-targeted conjugate counterpart. This significant effect is achieved by enhancing the permeation and prodrug uptake by cancer cells and cytotoxicity of the prodrug [38].
5 Role of Antibodies in Targeted Therapy
In 1975, Köhler and Milstein developed methods to recover antibodies in large amount which can be directed against specific antigens . Since then monoclonal have emerged as most important ligands for delivering contrast agents and chemotherapeutics for several different malignancies [39]. Monoclonal antibody are stable in blood and typically have nanomolar affinities for their target. The binding and non-binding domains of mAb are separated physically; hence, they could impart substitution with other chemical agents like, contrast agents and chemotherapeutics. Three targeting moieties, whole mAb, Fab′, and single chain variable fragment (scFv) were evaluated for targeting the same B-cell antigen CD19 [18]. The Fab′ immunoliposomes even though exhibited the most prolonged circulation times, exhibited statistically insignificant numbers of long-term survivors [18]. While, in B-cell model, the anti-CD19 Fab′ immunoliposomes demonstrated increased circulation time and higher survival rates for Namalwa-bearing SCID mice as compared to the anti-CD19 mAb immunoliposome treatment [40].
More recently, the fragments of antibody containing only the variable region of the antibody are used for active targeting of therapeutics because they retain the specificity for their target [36]. In addition, they prevent complement activation due to the lack of constant Fc effector region or undesirable interaction with other cells. Furthermore, the smaller sizes of antibody fragments are important factor in the development of an actively targeting nanoparticle. Moreover, using antibody fragments can also help in efficient cell permeability [41]. Therapeutic agents must cross various biological barriers as well as the high interstitial pressure to reach their target cells. Towards this antibody fragments such as scFv and Fab are known to represent higher efficiency in penetrating tumor cells compared to intact antibody.
Immunogenicity caused by these antibodies is yet another important factor in using them for therapeutic targeting. Animal originated antibodies are obviously identified as foreign agents resulting in strong immune responses. However, genetic engineering tools can now design chimeric mouse-human mAbs. For example the anti-CD20 mAb rituximab (Rituxan) has revolutionized lymphoma treatment. On the other hand, humanized antibodies, containing only the binding regions of the mouse antibodies combined with a human antibody, exhibit reduction in immunogenicity [42]. However, they have shown reduced affinity in some cases. Further, antibodies could lose activity when translated into a conjugated form. Therefore, novel chemical strategies are essential to retain their potency even after the conjugation and at the same time are able to release the cytotoxic agent, either after binding to the cancer cell surface or after endocytosis into the cell. An example of such a conjugation is that of calicheamicin, a cytotoxic drug, conjugated to a tumor-targeting mAb through an amide linkage. The conjugate accumulates in the tumor but shows no appreciable cytotoxicity [43]. However, when calicheamicin is conjugated using a pH-sensitive bifunctional linker that permits its release intracellularly (Fig. 11.6), the conjugate shows potent antitumor activity [44].
Cleavable bifunctional linker for the conjugation of calicheamicin to monoclonal antibodies (reproduced from [17])
The prodrug was designed by coupling calicheamicin to various hydrazide bearing spacers through a disulfide bond, and the resulting moiety was conjugated to humanized anti-CD33 monoclonal antibody (clone P67.6) hinge region. Monoclonal antibody conjugated calicheamicin was then coupled to aldehyde-bearing oxidized carbohydrates, through hydrazone bonds [44]. In vivo study showed that active prodrugs rapidly cleaved at pH 4.5 whereas, they were stable at pH 7.4. On the other hand the efficacy of the prodrug system was found to be far less when calicheamicin was conjugated with a linker encompassing a non-pH-labile amide bond to mAb. This conjugate although had the same affinity for CD33 as Mylotarg, the system was found to be hundreds of times less cytotoxic in vitro and considerably less active in vivo and ex vivo [44]. In this system, the release of calicheamicin was believed to be due to intracellular oxidation of a hindered disulfide bond. This clearly indicated that the importances of linker chemistry for effective intracellular activation of calicheamicin–mAb conjugate.
6 Protein and Peptide Based Carrier Systems
Peptide ligands are being explored against a tumor-specific antigen or a peptide transporter that is overexpressed in cancer cells [40]. Peptide ligands can be directly conjugated to chemotherapy drugs to achieve a targeted delivery to cancer cells. Compared to antibody, peptides are more suitable targeting moieties because of (1) low molecular weight, (2) exceptional cell permeability, (3) ease in chemical conjugation, and (4) simple to produce [45].
The main approach in identifying appropriate peptide ligands is to screen peptide libraries produced by either phage display [46] or by chemical synthesis process [47, 48]. Phage display assists in identifying peptides that target a specific receptor, or certain cell types even if the receptors are unidentified [49]. Till date, various types of receptors or cells, have been discovered such as integrin receptors [50, 51], thrombin receptors [52], tumor cells [53–55], cardiomyocytes [56], and pancreatic β cells [57]. Tumor-targeting peptides have been effectively used in delivery vehicles for targeting small molecule drugs, oligonucleotides, liposomes, imaging agents, and inorganic nanoparticles to tumors. Furthermore, peptidomimetic self-assembled nanoparticles and peptide aptamers, which are peptide-related nanoparticles, also have shown great promise in targeted drug delivery. The former have wider applications in tumor imaging, tumor targeting delivery and vaccination [58], whereas the latter are directly used as drugs interfering with the function of receptors [59]. The use of these peptides has assisted in enhancing the specificity and efficacy of drug delivery with reduced side effects [60, 61]. The current discoveries of tumor lymphatic vessel targeting peptides present another route for targeted drug delivery for tumors [62–64].
Transferrin (Tf), a serum non-heme iron binding glycoprotein is a very pertinent targeting agent for cancer therapeutics due to overexpressed Tf receptors (TfR+) on malignant cells compared to normal cells because of the higher demand for faster cell growth and division. We and many others have demonstrated use of Tf for targeting TfR+ in cancer therapeutics and diagnostics [65]. Tf is also extensively reported in human clinical trials with adriamycin [66], cisplatin [67], and diphtheria toxin [68].
An important study to demonstrate Tf mediated targeting was explored using 0.05 % PEG-AD containing Tf formulation [69]. The formulation was compared against AD-PEG-particles (with 0.0 % Tf-PEG-AD) using cells K562 for gene delivery. Tf-PEG-AD demonstrated a fourfold increase in transfection mainly due to Tf mediated uptake. However, presence of excess Tf added to 0.05 % Tf-PEG-AD particles eliminated the transfection enhancement [69].
An important characteristic of Tf ligand for targeting TfR+ is the iron-binding efficiency. Transferrin ligand with low iron-binding efficiency resulted in a lower efficiency in binding to the TfR [68]. This was revealed from the flow cytometry study involving fluorescein-labeled transferrin (Tf-fluor) and holo-transferrin (holo-Tf, native transferrin), Tf-PEG-AD, or Tf-(PEGAD)2. The Tf-PEG-AD and Tf-(PEG-AD)2 showed lower binding affinities, while holo-Tf treatment showed the highest binding affinity mainly due to their oxidized state. As a result, a different synthesis route for Tf-PEG-AD was designed to improve the binding affinity to the Tf receptor. The synthesized Tf-PEG-AD nanoparticles (250 nM Tf-fluor/75 nM Tf-PEG-AD nanoparticles) showed a 15 % reduction in fluorescence compared to Tf-PEG-AD conjugates (250 nM Tf-fluor/75 nM Tf-PEG-AD in conjugate form) revealing high binding. The difference in receptor binding was mainly due to multiple interactions between each ligand-modified particle and cell surface receptors.
Davis et al. have also performed a novel study of small interfering RNA (siRNA) delivery in nonhuman primates using Tf-conjugated liposomes [70]. The efficacy of these Tf-conjugated liposomes had been proven effective in metastatic mouse models of Ewing’s sarcoma, and consequently, the safety of the administration of these particles in nonhuman primates was the focus of this study [71, 72].
Interestingly, Tf-conjugated liposomes co-encapsulating Dox and verapamil (Tf-L-DOX/VER) have been shown to effectively overcome multi-drug resistance [73]. Cellular uptake of Tf-L-DOX/VER was 5.2 and 2.8 times greater with cytotoxicity (IC50 = 4.18 μM) than non-targeted liposomes having Dox and verapamil (IC50 = 21.7 μM) and Tf-conjugated liposomes loaded with Dox alone (IC50 = 11.5 μM) in a chronicmyelogenous leukemia cell line (K562 cells). In addition, the difference in cytotoxicity between the targeted and non-targeted liposomes was diminished within the presence of 2 mg/mL free Tf. This exhibits the effectiveness of the Tf moiety for cellular uptake and cytotoxicity [72].
We have recently shown that Tf conjugated multicomponent magneto-dendritic nanosystem (MDNS) can be efficiently used for rapid tumor cell targeting, isolation, and high-resolution imaging by a facile bioconjugation approach [65]. The bio-functionalized MDNS designed by combining multiple components such as Tf, iron oxide (Fe3O4) nanoparticles, fourth generation (G4) dendrimers, cyanine 5 NHS (Cy5) fluorescent NIR dye and glutathione (GSH) was able to capture TfR overexpressed cancer cells from an artificial circulating tumor cell (CTC)-like suspension (Fig. 11.7). The MDNS platform exhibited rapid capture (~5 min) of TfR-overexpressing (TfR+) cancer cells at clinically relevant concentrations (approximately 1 CTC per 105 blood cells) [65].
Cellular targeting of a bio-functionalized Magneto-Dendritic Nano System (MDNS). (a) Magnified image of a cell showing localization of MDNS particles on the cell membrane after 5 min of incubation. (b) Left image shows Tf+ MDNS particles attached to the HCT116 cells, whereas, hardly any Tf- MDNS particles present on the cell surface as shown in right image. (c) After 60 min of exposure only the Tf+ MDNS were present in large numbers on the cells revealing target specificity of MDNS interaction remains intact even after long exposure (reproduced from [65])
Choi and his coworkers showed that Tf decorated PEGylated gold nanoparticles accumulations in the tumors and other organs are independent of Tf (Fig. 11.8) [74]. However, the nanoparticle localizations within a particular organ are influenced by the Tf content. They also demonstrated that in tumor tissue, the content of targeting ligands significantly influenced the number of nanoparticles localized within the cancer cells. Most nanoparticles remain in nonparenchymal cells, however, small amount of nanoparticles resided in hepatocytes due to higher Tf content [74].
Schematic of Tf-PEG-AuNPs. Unmodified 50-nm AuNPs (I) were reacted with excess mPEG-SH to form PEG-AuNPs (II) as untargeted particles or first were reacted with various amounts of Tf-PEG-SH and later excess mPEG-SH to form Tf-PEG-AuNPs (III: 2 Tf per particle; IV: 18 Tf per particle; V: 144 Tf per particle) (reproduced from [74])
Similarly, Lutenizing Hormone Releasing Hormone (LHRH) peptide-conjugated prodrug has shown promising results for cancer therapy [75, 8]. Khandare et al. conjugated LHRH peptide using PEG as the spacer to camptothecin (CPT), a cytotoxic drug [75, 8] (Fig. 11.9). The LHRH peptide-conjugated prodrug demonstrated higher efficacy with minimized side effects on healthy organs. In addition, the prodrug system showed targeting potential for both solid tumor tissue as well as a single tumor cell. Hence, this prodrug can effectively target tumor cells with a low toxicity to normal tissues [75]. Neamati and coworkers conjugated paclitaxel, an antimicrotubule agent commonly used in the treatment of metastatic breast cancer to a cyclic peptide E[c(RGDyK)]2 (RGD). In vivo studies showed a specific tumor uptake of the RGD-paclitaxel system at 4 h post administration [76].
Schematic of targeted multivalent anticancer prodrug . The prodrug conjugate system was designed with (a) bis-PEG polymer as a carrier- one, two, or three copies of CPT as an anticancer drug; and one, two, or three copies of LHRH peptide as a targeting agent. (b) α,ω-bis-PEG3000-CA conjugate (3) was designed by conjugation of bis(2-carboxyethyl) PEG (1) with CA (2). (c) The bis-PEG-CA conjugate (3) was conjugated with CPT (4) to obtain α,ω-bis(2-carboxyethyl) PEG-CA-CPT conjugates (5, 6, and 7). (d) α,ω-bis(2-carboxyethyl) PEG-CA-CPT-LHRH conjugates (d, 5a, 6a, and 7a) having one, two, and three copies of CPT (4) and LHRH (8)were synthesized by conjugating LHRH (8) with 5, 6, and 7 (reproduced from [75])
Similarly, Yoneda et al. have explored targeted delivery of paclitaxel and doxorubucin by using glucose-regulated protein 78 (GRP78) as a tumor-specific antigen [77]. GRP78 is overexpressed on many tumor cells, including skin, prostate, colon, and breast cancers. On the other hand, its expression on normal tissues is very small [78]. Pep42, a cyclic 13-meroligopeptide (CTVALPGGYVRVC), internalizes through the GRP78 receptor-mediated endocytosis after specifically binding to GRP78 and then trafficked to the lysosome that contains protease cathepsin B. Therefore, Val-Cit motif, a cleavable linker, was used to link Pep42 to anticancer drugs. The Val-Cit linker is reasonably stable in the plasma, but cathepsin B in the cancer cells can cleave [79]. Both Pep42-paclitaxel and Pep42-Dox showed an enhanced toxicity in comparison to the free drug when cytotoxicity of the Pep42-prodrug was estimated in osteosarcoma cells, SJSA-1 [77].
7 Folic Acid-Drug Conjugate
Folic acid (FA) is a member of the vitamin B family and is one of the most commonly used targeting moiety for specific delivery of various imaging agents, therapeutic agents, and nano-scaled systems to tumor cells. It is known to bind with a very high affinity (K d 0.1–1 nM) to folate receptor (FR). Folate receptor is overexpressed on the surface of many malignant cells including breast, lung, kidney, ovarian, and endometrial cancers [80]. On the other hand, the expression of FR on other normal tissues is low and restricted to some epithelial cells. Folic acid conjugated prodrugs enter cells via receptor mediated endocytosis after binding to folate receptors. In addition, FA has a low immunogenicity and relatively simple chemistry compared to other targeting moieties such as antibody, peptide, and aptamer [80–82]. For targeting tumor cells, a range of anticancer drugs have been conjugated with FA.
To enhance the specificity to tumor cells Dox was conjugated to FA [83]. Dox is an anthracyclinic drug used for a wide variety of cancers. However, poor solubility, extremely high toxicity and short half-life limit its therapeutic efficacy. D-α-Tocopheryl polyethylene glycol succinate (TPGS) was conjugated, to the FA modification, to Dox to enhance the solubility and drug permeability across cell membrane. The TPGS-Dox-FA prodrug exhibited enhanced half-life, high antitumor efficacy (45-fold more effective than the unmodified Dox), and less accumulation in the heart, which is the major organ affected by Dox’s side effects [83].
Philip et al. demonstrated that FA on conjugation to campothecin, a poor water-soluble and highly toxic chemotherapy agent, via a hydrophilic peptide containing a disulfide bond [81]. They showed increase in specificity of the prodrug, while the cleavable spacer increased the solubility of campothecin and also provides an efficient release of camptothecin within tumor cells via the disulfide reduction [81].
8 Conclusions
Polymeric prodrug conjugate systems offer a potent and versatile tool for improving the therapeutic potential of low-molecular-weight drugs and proteins. Although considerable progress has been made in the field of prodrugs in clinic, prodrug systems consisting a targeting component still remains only as a perspective. There are numerous scientific challenges to overcome this goal, such as advanced biomaterials, molecular tunability, physicochemical strategies, immunogenicity, cell permeability, and cell specificity in clinically relevant targeted drugs. However, several prodrug systems having anticancer agents are currently under clinical trials. Towards this direction, in next few years many other anticancer conjugates could get regulatory approvals. In the future, requirement for advance drug delivery strategies such as targeted prodrugs will become more important since the discovery of new anticancer drugs will become increasingly challenging and expensive [1].
Abbreviations
- ADCC:
-
Antibody-dependent cellular cytotoxicity
- ADEPT:
-
Antibody-directed enzyme prodrug therapy
- AuNP:
-
Gold nanoparticles
- BCR:
-
Breakpoint cluster region protein
- BTK:
-
Bruton’s tyrosine kinase
- CDK inhibitor:
-
Cyclin-dependent kinase inhibitors
- CLL:
-
Chronic lymphocytic leukemia
- CPT:
-
Camptothecin
- CTC:
-
Circulating tumor cells
- Dox:
-
Doxorubicin
- DTC:
-
Disseminated tumor cells
- EGFR:
-
Epidermal growth factor receptor
- EPR:
-
Enhanced permeability and retention
- ERK:
-
Extracellular signal-regulated kinases
- FISH:
-
Fluorescence in-situ hybridization
- FOL:
-
Folic acid
- FR:
-
Folate Receptor
- GDEPT:
-
Gene-directed enzyme prodrug therapy
- GnRH:
-
Gonadotropin-releasing hormone
- GRP78:
-
Glucose-regulated protein 78
- HCC:
-
Hepatocellular carcinoma
- HER2:
-
human epidermal growth factor 2
- HPLC:
-
High-performance liquid chromatography
- IGFR:
-
Insulin-like growth factor receptor
- KRAS:
-
Kirsten rat sarcoma
- LHRH:
-
Luteinizing hormone releasing hormone
- mAb:
-
Monoclonal antibodies
- MAPK:
-
Mitogen-activated protein kinases
- MCL:
-
Mantle cell lymphoma
- mCRC:
-
Metastatic colorectal cancer
- MDNS:
-
Magneto-Dendritic Nano System
- MDR:
-
Multiple-drug resistance
- mRNA:
-
Messenger ribonucleic acid
- mTOR:
-
Mammalian target of rapamycin
- NSCLC:
-
Non-small-cell lung cancer
- PCR:
-
Polymerase chain reaction
- PDGFRβ:
-
Platelet-derived growth factor receptor
- PI3K:
-
Phosphatidylinositol 3-kinase
- PIGF:
-
Placental growth factor
- RCC:
-
Renal cell carcinoma
- RET:
-
Rearranged during transfection
- RGD:
-
Arginine-glycine-aspartic acid
- SCCHN:
-
Squamous cell carcinoma of the head and neck
- scFv:
-
Single chain variable fragment
- siRNA:
-
Small interfering RNA
- Tf:
-
Transferrin
- Tf-PEG-AD:
-
Transferrin-conjugated poly (ethylene glycol)-adamantane
- TfR:
-
Transferrin receptor
- TPGS:
-
D-α-Tocopheryl polyethylene glycol succinate
- US FDA:
-
United States Food and Drug administration
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
References
Knox RJ, Connors TA (1997) Prodrugs in cancer chemotherapy. Pathol Oncol Res 3(4):309–324
Rautio J, Kumpulainen H, Heimbach T, Oliyai R, Oh D, Jarvinen T, Savolainen J (2008) Prodrugs: design and clinical applications. Nat Rev Drug Discov 7(3):255–270. doi:10.1038/nrd2468
Duncan R (2003) The dawning era of polymer therapeutics. Nat Rev Drug Discov 2(5):347–360. doi:10.1038/nrd1088
Singh Y, Palombo M, Sinko PJ (2008) Recent trends in targeted anticancer prodrug and conjugate design. Curr Med Chem 15(18):1802–1826
Muller CE (2009) Prodrug approaches for enhancing the bioavailability of drugs with low solubility. Chem Biodivers 6(11):2071–2083. doi:10.1002/cbdv.200900114
Minko T, Khandare JJ, Vetcher AA, Soldatenkov CA, Garbuzenko OB, Saad M, Pozharov VP (2008) Multifunctional nanotherapeutics for cancer. In: Torchilin VP (ed) Multifunctional pharmaceutical nanocarriers. Springer, New York, pp 309–336
Minko T (2004) Drug targeting to the colon with lectins and neoglycoconjugates. Adv Drug Deliv Rev 56(4):491–509. doi:10.1016/j.addr.2003.10.017
Dharap SS, Wang Y, Chandna P, Khandare JJ, Qiu B, Gunaseelan S, Sinko PJ, Stein S, Farmanfarmaian A, Minko T (2005) Tumor-specific targeting of an anticancer drug delivery system by LHRH peptide. Proc Natl Acad Sci U S A 102(36):12962–12967. doi:10.1073/pnas.0504274102
Maeda H, Wu J, Sawa T, Matsumura Y, Hori K (2000) Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release 65(1–2):271–284
Mariano WA, Stella VJ (2007) Macromolecular prodrugs of small molecules. In: Stella V, Borchardt R, Hageman M, Oliyai R, Maag H, Tilley J (eds) Prodrugs, challenges and rewards part 1, vol 1. Springer-AAPS, New York, pp 289–321. doi:10.1007/978-0-387-49785-3
Greish K (2007) Enhanced permeability and retention of macromolecular drugs in solid tumors: a royal gate for targeted anticancer nanomedicines. J Drug Target 15(7–8):457–464. doi:10.1080/10611860701539584
Haag R, Kratz F (2006) Polymer therapeutics: concepts and applications. Angew Chem Int Ed Engl 45(8):1198–1215. doi:10.1002/anie.200502113
Jain RK (1994) Barriers to drug delivery in solid tumors. Sci Am 271(1):58–65
Minko T, Dharap SS, Pakunlu RI, Wang Y (2004) Molecular targeting of drug delivery systems to cancer. Curr Drug Targets 5(4):389–406
Choksi A, Sarojini KV, Vadnal P, Dias C, Suresh PK, Khandare J (2013) Comparative anti-inflammatory activity of poly(amidoamine) (PAMAM) dendrimer-dexamethasone conjugates with dexamethasone-liposomes. Int J Pharm 449(1–2):28–36. doi:10.1016/j.ijpharm.2013.03.056
Banerjee SS, Aher N, Patil R, Khandare J (2012) Poly(ethylene glycol)-prodrug conjugates: concept, design, and applications. J Drug Deliv 2012:103973. doi:10.1155/2012/103973
Maison W, Frangioni JV (2003) Improved chemical strategies for the targeted therapy of cancer. Angew Chem Int Ed 42(39):4726–4728. doi:10.1002/anie.200301666
Khandare J, Minko T (2006) Polymer–drug conjugates: progress in polymeric prodrugs. Prog Polym Sci 31(4):359–397. doi:http://dx.doi.org/10.1016/j.progpolymsci.2005.09.004
Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R (2007) Nanocarriers as an emerging platform for cancer therapy. Nat Nanotechnol 2(12):751–760. doi:10.1038/nnano.2007.387
Administration USFDA (2014) Hematology/Oncology (Cancer) Approvals & Safety Notifications. http://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm279174.htm. Accessed 23 March 2014
Collins I, Workman P (2006) New approaches to molecular cancer therapeutics. Nat Chem Biol 2(12):689–700. doi:10.1038/nchembio840
Park JW, Hong K, Kirpotin DB, Meyer O, Papahadjopoulos D, Benz CC (1997) Anti-HER2 immunoliposomes for targeted therapy of human tumors. Cancer Lett 118(2):153–160
Baselga J (2001) The EGFR as a target for anticancer therapy—focus on cetuximab. Eur J Cancer 37(Suppl 4):S16–S22
Fischer PM, Gianella-Borradori A (2003) CDK inhibitors in clinical development for the treatment of cancer. Expert Opin Investig Drugs 12(6):955–970. doi:10.1517/13543784.12.6.955
Ellis LM, Hicklin DJ (2008) VEGF-targeted therapy: mechanisms of anti-tumour activity. Nat Rev Cancer 8(8):579–591. doi:10.1038/nrc2403
Dietel M, Johrens K, Laffert M, Hummel M, Blaker H, Muller BM, Lehmann A, Denkert C, Heppner FL, Koch A, Sers C, Anagnostopoulos I (2013) Predictive molecular pathology and its role in targeted cancer therapy: a review focussing on clinical relevance. Cancer Gene Ther 20(4):211–221. doi:10.1038/cgt.2013.13
Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ, Juan T, Sikorski R, Suggs S, Radinsky R, Patterson SD, Chang DD (2008) Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol 26(10):1626–1634. doi:10.1200/jco.2007.14.7116
Gilcrease MZ, Woodward WA, Nicolas MM, Corley LJ, Fuller GN, Esteva FJ, Tucker SL, Buchholz TA (2009) Even low-level HER2 expression may be associated with worse outcome in node-positive breast cancer. Am J Surg Pathol 33(5):759–767. doi:10.1097/PAS.0b013e31819437f9
Hudziak RM, Schlessinger J, Ullrich A (1987) Increased expression of the putative growth factor receptor p185HER2 causes transformation and tumorigenesis of NIH 3T3 cells. Proc Natl Acad Sci U S A 84(20):7159–7163
Hudis CA (2007) Trastuzumab—mechanism of action and use in clinical practice. N Engl J Med 357(1):39–51. doi:10.1056/NEJMra043186
Morrow PK, Wulf GM, Ensor J, Booser DJ, Moore JA, Flores PR, Xiong Y, Zhang S, Krop IE, Winer EP, Kindelberger DW, Coviello J, Sahin AA, Nunez R, Hortobagyi GN, Yu D, Esteva FJ (2011) Phase I/II study of trastuzumab in combination with everolimus (RAD001) in patients with HER2-overexpressing metastatic breast cancer who progressed on trastuzumab-based therapy. J Clin Oncol 29(23):3126–3132. doi:10.1200/jco.2010.32.2321
Vivanco I, Sawyers CL (2002) The phosphatidylinositol 3-kinase AKT pathway in human cancer. Nat Rev Cancer 2(7):489–501. doi:10.1038/nrc839
Berns K, Horlings HM, Hennessy BT, Madiredjo M, Hijmans EM, Beelen K, Linn SC, Gonzalez-Angulo AM, Stemke-Hale K, Hauptmann M, Beijersbergen RL, Mills GB, van de Vijver MJ, Bernards R (2007) A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell 12(4):395–402. doi:10.1016/j.ccr.2007.08.030
Nagata Y, Lan KH, Zhou X, Tan M, Esteva FJ, Sahin AA, Klos KS, Li P, Monia BP, Nguyen NT, Hortobagyi GN, Hung MC, Yu D (2004) PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell 6(2):117–127. doi:10.1016/j.ccr.2004.06.022
Damodaran S, Olson EM (2012) Targeting the human epidermal growth factor receptor 2 pathway in breast cancer. Hosp Pract 40(4):7–15. doi:10.3810/hp.2012.10.997
Jerusalem G, Fasolo A, Dieras V, Cardoso F, Bergh J, Vittori L, Zhang Y, Massacesi C, Sahmoud T, Gianni L (2011) Phase I trial of oral mTOR inhibitor everolimus in combination with trastuzumab and vinorelbine in pre-treated patients with HER2-overexpressing metastatic breast cancer. Breast Cancer Res Treat 125(2):447–455. doi:10.1007/s10549-010-1260-x
Bull C, Boltje TJ, Wassink M, de Graaf AM, van Delft FL, den Brok MH, Adema GJ (2013) Targeting aberrant sialylation in cancer cells using a fluorinated sialic acid analog impairs adhesion, migration, and in vivo tumor growth. Mol Cancer Ther 12(10):1935–1946. doi:10.1158/1535-7163.mct-13-0279
Khandare JJ, Wang Y, Singh AP, Vorsa N, Minko T (2007) Targeted sialic acid-doxorubicin prodrugs for intracellular delivery and cancer treatment. Pharm Res 24(11):2120–2130. doi:10.1007/s11095-007-9406-1
Cheng WW, Allen TM (2008) Targeted delivery of anti-CD19 liposomal doxorubicin in B-cell lymphoma: a comparison of whole monoclonal antibody, Fab' fragments and single chain Fv. J Control Release 126(1):50–58. doi:10.1016/j.jconrel.2007.11.005
Sapra P, Moase EH, Ma J, Allen TM (2004) Improved therapeutic responses in a xenograft model of human B lymphoma (Namalwa) for liposomal vincristine versus liposomal doxorubicin targeted via anti-CD19 IgG2a or Fab' fragments. Clin Cancer Res 10(3):1100–1111
Chapman AP (2002) PEGylated antibodies and antibody fragments for improved therapy: a review. Adv Drug Deliv Rev 54(4):531–545
Maloney DG, Grillo-Lopez AJ, White CA, Bodkin D, Schilder RJ, Neidhart JA, Janakiraman N, Foon KA, Liles TM, Dallaire BK, Wey K, Royston I, Davis T, Levy R (1997) IDEC-C2B8 (Rituximab) anti-CD20 monoclonal antibody therapy in patients with relapsed low-grade non-Hodgkin’s lymphoma. Blood 90(6):2188–2195
Chan SY, Gordon AN, Coleman RE, Hall JB, Berger MS, Sherman ML, Eten CB, Finkler NJ (2003) A phase 2 study of the cytotoxic immunoconjugate CMB-401 (hCTM01-calicheamicin) in patients with platinum-sensitive recurrent epithelial ovarian carcinoma. Cancer Immunol Immunother 52(4):243–248. doi:10.1007/s00262-002-0343-x
Hamann PR, Hinman LM, Hollander I, Beyer CF, Lindh D, Holcomb R, Hallett W, Tsou HR, Upeslacis J, Shochat D, Mountain A, Flowers DA, Bernstein I (2002) Gemtuzumab ozogamicin, a potent and selective anti-CD33 antibody-calicheamicin conjugate for treatment of acute myeloid leukemia. Bioconjug Chem 13(1):47–58
Tai W, Mahato R, Cheng K (2010) The role of HER2 in cancer therapy and targeted drug delivery. J Control Release 146(3):264–275. doi:10.1016/j.jconrel.2010.04.009
Marasco D, Perretta G, Sabatella M, Ruvo M (2008) Past and future perspectives of synthetic peptide libraries. Curr Protein Pept Sci 9(5):447–467
Koivunen E, Arap W, Rajotte D, Lahdenranta J, Pasqualini R (1999) Identification of receptor ligands with phage display peptide libraries. J Nucl Med 40(5):883–888
Smith GP, Petrenko VA (1997) Phage display. Chem Rev 97(2):391–410
Brown KC (2000) New approaches for cell-specific targeting: identification of cell-selective peptides from combinatorial libraries. Curr Opin Chem Biol 4(1):16–21
Pasqualini R, Koivunen E, Ruoslahti E (1997) Alpha v integrins as receptors for tumor targeting by circulating ligands. Nat Biotechnol 15(6):542–546. doi:10.1038/nbt0697-542
Koivunen E, Wang B, Ruoslahti E (1995) Phage libraries displaying cyclic peptides with different ring sizes: ligand specificities of the RGD-directed integrins. Biotechnology (N Y) 13(3):265–270
Doorbar J, Winter G (1994) Isolation of a peptide antagonist to the thrombin receptor using phage display. J Mol Biol 244(4):361–369. doi:10.1006/jmbi.1994.1736
Oyama T, Sykes KF, Samli KN, Minna JD, Johnston SA, Brown KC (2003) Isolation of lung tumor specific peptides from a random peptide library: generation of diagnostic and cell-targeting reagents. Cancer Lett 202(2):219–230
Oyama T, Rombel IT, Samli KN, Zhou X, Brown KC (2006) Isolation of multiple cell-binding ligands from different phage displayed-peptide libraries. Biosens Bioelectron 21(10):1867–1875. doi:10.1016/j.bios.2005.11.016
McGuire MJ, Samli KN, Chang YC, Brown KC (2006) Novel ligands for cancer diagnosis: selection of peptide ligands for identification and isolation of B-cell lymphomas. Exp Hematol 34(4):443–452. doi:10.1016/j.exphem.2005.12.013
McGuire MJ, Samli KN, Johnston SA, Brown KC (2004) In vitro selection of a peptide with high selectivity for cardiomyocytes in vivo. J Mol Biol 342(1):171–182. doi:10.1016/j.jmb.2004.06.029
Samli KN, McGuire MJ, Newgard CB, Johnston SA, Brown KC (2005) Peptide-mediated targeting of the islets of Langerhans. Diabetes 54(7):2103–2108
Baines IC, Colas P (2006) Peptide aptamers as guides for small-molecule drug discovery. Drug Discov Today 11(7–8):334–341. doi:10.1016/j.drudis.2006.02.007
Jabbari E (2009) Targeted delivery with peptidomimetic conjugated self-assembled nanoparticles. Pharm Res 26(3):612–630. doi:10.1007/s11095-008-9802-1
Curnis F, Gasparri A, Sacchi A, Longhi R, Corti A (2004) Coupling tumor necrosis factor-alpha with alphaV integrin ligands improves its antineoplastic activity. Cancer Res 64(2):565–571
Ellerby HM, Arap W, Ellerby LM, Kain R, Andrusiak R, Rio GD, Krajewski S, Lombardo CR, Rao R, Ruoslahti E, Bredesen DE, Pasqualini R (1999) Anti-cancer activity of targeted pro-apoptotic peptides. Nat Med 5(9):1032–1038. doi:10.1038/12469
Laakkonen P, Akerman ME, Biliran H, Yang M, Ferrer F, Karpanen T, Hoffman RM, Ruoslahti E (2004) Antitumor activity of a homing peptide that targets tumor lymphatics and tumor cells. Proc Natl Acad Sci U S A 101(25):9381–9386. doi:10.1073/pnas.0403317101
Laakkonen P, Porkka K, Hoffman JA, Ruoslahti E (2002) A tumor-homing peptide with a targeting specificity related to lymphatic vessels. Nat Med 8(7):751–755. doi:10.1038/nm720
Zhang L, Giraudo E, Hoffman JA, Hanahan D, Ruoslahti E (2006) Lymphatic zip codes in premalignant lesions and tumors. Cancer Res 66(11):5696–5706. doi:10.1158/0008-5472.can-05-3876
Banerjee SS, Jalota-Badhwar A, Satavalekar SD, Bhansali SG, Aher ND, Mascarenhas RR, Paul D, Sharma S, Khandare JJ (2013) Transferrin-mediated rapid targeting, isolation, and detection of circulating tumor cells by multifunctional magneto-dendritic nanosystem. Adv Healthc Mater 2(6):800–805. doi:10.1002/adhm.201200164
Faulk WP, Taylor CG, Yeh CJ, McIntyre JA (1990) Preliminary clinical study of transferrin-adriamycin conjugate for drug delivery to acute leukemia patients. Mol Biother 2(1):57–60
Head JF, Wang F, Elliott RL (1997) Antineoplastic drugs that interfere with iron metabolism in cancer cells. Adv Enzyme Regul 37:147–169
Rainov NG, Soling A (2005) Technology evaluation: transMID, KS Biomedix/Nycomed/Sosei/PharmaEngine. Curr Opin Mol Ther 7(5):483–492
Bellocq NC, Pun SH, Jensen GS, Davis ME (2003) Transferrin-containing, cyclodextrin polymer-based particles for tumor-targeted gene delivery. Bioconjug Chem 14(6):1122–1132. doi:10.1021/bc034125f
Heidel JD, Yu Z, Liu JY, Rele SM, Liang Y, Zeidan RK, Kornbrust DJ, Davis ME (2007) Administration in non-human primates of escalating intravenous doses of targeted nanoparticles containing ribonucleotide reductase subunit M2 siRNA. Proc Natl Acad Sci U S A 104(14):5715–5721. doi:10.1073/pnas.0701458104
Hu-Lieskovan S, Heidel JD, Bartlett DW, Davis ME, Triche TJ (2005) Sequence-specific knockdown of EWS-FLI1 by targeted, nonviral delivery of small interfering RNA inhibits tumor growth in a murine model of metastatic Ewing's sarcoma. Cancer Res 65(19):8984–8992. doi:10.1158/0008-5472.can-05-0565
Pun SH, Tack F, Bellocq NC, Cheng J, Grubbs BH, Jensen GS, Davis ME, Brewster M, Janicot M, Janssens B, Floren W, Bakker A (2004) Targeted delivery of RNA-cleaving DNA enzyme (DNAzyme) to tumor tissue by transferrin-modified, cyclodextrin-based particles. Cancer Biol Ther 3(7):641–650
Wu J, Lu Y, Lee A, Pan X, Yang X, Zhao X, Lee RJ (2007) Reversal of multidrug resistance by transferrin-conjugated liposomes co-encapsulating doxorubicin and verapamil. J Pharm Pharm Sci 10(3):350–357
Choi CH, Alabi CA, Webster P, Davis ME (2010) Mechanism of active targeting in solid tumors with transferrin-containing gold nanoparticles. Proc Natl Acad Sci U S A 107(3):1235–1240. doi:10.1073/pnas.0914140107
Khandare JJ, Chandna P, Wang Y, Pozharov VP, Minko T (2006) Novel polymeric prodrug with multivalent components for cancer therapy. J Pharmacol Exp Ther 317(3):929–937. doi:10.1124/jpet.105.098855
Chen X, Plasencia C, Hou Y, Neamati N (2005) Synthesis and biological evaluation of dimeric RGD peptide-paclitaxel conjugate as a model for integrin-targeted drug delivery. J Med Chem 48(4):1098–1106. doi:10.1021/jm049165z
Yoneda Y, Steiniger SC, Capkova K, Mee JM, Liu Y, Kaufmann GF, Janda KD (2008) A cell-penetrating peptidic GRP78 ligand for tumor cell-specific prodrug therapy. Bioorg Med Chem Lett 18(5):1632–1636. doi:10.1016/j.bmcl.2008.01.060
Shin BK, Wang H, Yim AM, Le Naour F, Brichory F, Jang JH, Zhao R, Puravs E, Tra J, Michael CW, Misek DE, Hanash SM (2003) Global profiling of the cell surface proteome of cancer cells uncovers an abundance of proteins with chaperone function. J Biol Chem 278(9):7607–7616. doi:10.1074/jbc.M210455200
Dubowchik GM, Firestone RA (1998) Cathepsin B-sensitive dipeptide prodrugs. 1. A model study of structural requirements for efficient release of doxorubicin. Bioorg Med Chem Lett 8(23):3341–3346
Shangguan D, Li Y, Tang Z, Cao ZC, Chen HW, Mallikaratchy P, Sefah K, Yang CJ, Tan W (2006) Aptamers evolved from live cells as effective molecular probes for cancer study. Proc Natl Acad Sci U S A 103(32):11838–11843. doi:10.1073/pnas.0602615103
Henne WA, Doorneweerd DD, Hilgenbrink AR, Kularatne SA, Low PS (2006) Synthesis and activity of a folate peptide camptothecin prodrug. Bioorg Med Chem Lett 16(20):5350–5355. doi:10.1016/j.bmcl.2006.07.076
Aronov O, Horowitz AT, Gabizon A, Gibson D (2003) Folate-targeted PEG as a potential carrier for carboplatin analogs. Synthesis and in vitro studies. Bioconjug Chem 14(3):563–574. doi:10.1021/bc025642l
Anbharasi V, Cao N, Feng SS (2010) Doxorubicin conjugated to D-alpha-tocopheryl polyethylene glycol succinate and folic acid as a prodrug for targeted chemotherapy. J Biomed Mater Res A 94(3):730–743. doi:10.1002/jbm.a.32734
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Controlled Release Society
About this chapter
Cite this chapter
Banerjee, S., Todkar, K., Chate, G., Khandare, J. (2015). Prodrug Conjugate Strategies in Targeted Anticancer Drug Delivery Systems. In: Devarajan, P., Jain, S. (eds) Targeted Drug Delivery : Concepts and Design. Advances in Delivery Science and Technology. Springer, Cham. https://doi.org/10.1007/978-3-319-11355-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-11355-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-11354-8
Online ISBN: 978-3-319-11355-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)