Abstract
The elderly population is growing rapidly, and the prevalence of anemia is approximately 11 % in the elderly. Observational data demonstrates poor outcome in patients with even mild anemia, but this may reflect the patients’ underlying disease rather than the anemia itself. Clinical trials evaluating transfusion thresholds in the elderly suggest that a restrictive transfusion approach is safe in most clinical settings. Transfusion guidelines do not recommend specific transfusion thresholds in the elderly but rather focus on the hemoglobin level in relation to patients’ comorbidities; thus, transfusion decisions may be affected by the higher prevalence of underlying medical problems in the elderly but not by age itself.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic Kidney Disease
- Transfusion Strategy
- High Hemoglobin Level
- Oxyhemoglobin Dissociation Curve
- Unexplained Anemia
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
7.1 Introduction
The demographic landscape is changing at a rapid pace. Due to increases in life expectancy, the number of people aged 65 years or older is expected to rise precipitously over the next several decades. According to a 2010 report by the World Health Organization entitled “Global Health and Aging,” the worldwide elderly population is projected to rise from approximately 524 million in 2010 to almost 1.5 billion by 2050. The United States is no exception to this trend; by the year 2030, an estimated 1 in 5 Americans will be elderly, representing about 72 million people. Approximately 89 million Americans will be aged 65 or older by the year 2050, more than doubling the elderly population in 2010.
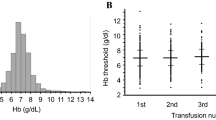
Anemia is a common condition in the elderly, and thus an important consideration in the medical care of the aging population. According to the NHANES III study, the largest and most comprehensive analysis of the prevalence of anemia in the elderly, 10.6 % of community-dwelling elderly people were found to be anemic (defined as a hemoglobin level <13 g/dL in men and <12 g/dL in women; see Fig. 7.1) [1]. The percentage of anemia in elderly men was slightly higher when compared to that of women (11.0 % vs. 10.2 %).
Furthermore, the prevalence of anemia increases steadily with age; in persons older than age 85, about one-quarter of men and one-fifth of women were anemic. These findings are similar to those of other large studies of the community-dwelling elderly population [2–4]. NHANES III also found significant differences in anemia rates in the elderly based on race and ethnicity. Non-Hispanic whites constitute the lowest prevalence (9.0 %), while non-Hispanic blacks constitute the highest (27.8 %).
Clinical data involving institutionalized elderly persons is less robust but indicates a much higher prevalence of anemia. Robinson and colleagues analyzed the charts of 6,200 nursing home residents with a mean age of 83 years old and found a 60 % prevalence of anemia [5]. Additionally, Artz et al. performed a retrospective chart review of 900 skilled nursing facility residents with a median age of 82 years old and found a mean hemoglobin of 12.9 g/dL for men and 11.9 for women [6]. The overall 6-month point prevalence of anemia was 48 %. The discrepancy in prevalence between these two studies is likely due to variations in the patient population studied, but clearly anemia is very common in the institutionalized elderly.
7.2 Etiology of Anemia in the Elderly
The causes of anemia in the elderly are generally divided into the following four categories: (1) nutrient deficiency, (2) chronic disease/inflammation, (3) chronic kidney disease, and (4) unexplained cause. NHANES III showed nearly a one-third split in prevalence between nutrient deficiencies (34 %), anemia of chronic disease (32 %), and unexplained anemia in the elderly (34 %). Half of the cases of nutrient deficiencies were due to iron deficiency (17 % of the total anemic population). Folate and vitamin B12 deficiency each accounted for about 6 % of all anemia. Eight percent of the cases of anemia of chronic disease were deemed secondary to chronic kidney disease. The authors theorized that the large proportion of unexplained anemia was related to the study design in that only a limited laboratory evaluation was performed in the study participants. Etiologies such as hypothyroidism, multiple myeloma, myelodysplastic syndrome, and thalassemia minor were thought to account for a significant portion of the unexplained cases.
A smaller but more intensive study performed by Price and colleagues enrolled 190 elderly patients with anemia from a hematology clinic [7]. All patients underwent a history, physical, laboratory evaluation (including a complete blood count with red cell indices, iron studies, erythropoietin level, and assessment of renal and thyroid function), and review of blood smears. Any further testing was left to the discretion of the treating physician and recorded for inclusion in the study when available. As examples, a serum protein electrophoresis was performed in 87 % of the patients, and a bone marrow biopsy was performed in 17 % of the patients. See Table 7.1 below for their results.
Despite a more thorough hematologic evaluation by Schrier et al., a similar rate of unexplained anemia was found as compared to that of NHANES III. However, the more thorough evaluation allowed for identification of several other key causes of anemia in the elderly, including hematologic malignancy and therapy for non-hematologic malignancy. A striking difference emerged between the prevalence of nutritional deficiencies between the two studies, likely due to a more stringent and accurate definition of nutritional deficiencies by Schrier et al. While the NHANES III study looked merely at blood levels of folate and vitamin B12 to make the diagnosis of deficiency, Schrier et al. went a step further in their definition by also requiring a hematologic response to folate or vitamin B12 supplementation.
7.3 Physiologic Response to Anemia in the Elderly
The human body is capable of several adaptive mechanisms in response to anemia [8]. Perhaps most importantly, the adrenergic system is ramped up in order to increase cardiac output and redirect this cardiac output to vital organs via selective arterial vasoconstriction. The renin-angiotensin-aldosterone axis is also stimulated to retain water and sodium. It is reasonable to consider that both of these hemodynamic alterations are vulnerable to attenuation with age. The incidence of heart failure increases with age, growing from about 20 per 1,000 persons between the ages of 65 and 69 to about 80 per 1,000 by age 85 or older [9]. Accordingly, the elderly may be less likely to adequately compensate to anemia by increasing cardiac output. Similar trends in rates of hypertension and peripheral vascular disease are seen with age [10], potentially making increases in vasomotor tone more difficult. This may result in reduced redirection of blood from skeletal, splanchnic, and superficial vessels to cerebral and coronary vessels that is seen in a normal compensation to anemia. All in all, elderly persons may not be able to achieve the hemodynamic changes necessary to fully compensate for anemia.
Several other age-related phenomena have been proposed as mechanisms of increased rates of anemia in the elderly. These mechanisms may also provide insight into the high rates of unexplained anemia seen in the studies mentioned above. Makipour et al. theorized that the following factors may contribute to anemia in the elderly [11]:
-
1.
Age-related decline in renal function, resulting in decreased erythropoietin levels.
-
2.
Age-related decline in androgen levels, which has been shown to correlate with a decrease in hemoglobin. For instance, the InCHIANTI study found an association between low testosterone and anemia in an elderly Italian population without cancer or chronic kidney disease [12].
-
3.
Increased prevalence of chronic inflammatory conditions in the elderly, such as cancer, arthritis, atherosclerosis, and others.
-
4.
Though still under investigation, there is growing evidence that hematopoietic stem cells lose proliferative and regenerative function over time [13, 14].
It is worthy to note that another major compensation for anemia is a shift to the right in the oxyhemoglobin dissociation curve. This is made possible by increased production of 2,3-diphosphoglycerate in red blood cells, which results in increased oxygen delivery to tissues at a given partial pressure of oxygen. After a literature search, no recent studies were found that specifically address the effect of aging on the oxyhemoglobin dissociation curve.
7.4 Consequences of Anemia in the Elderly
A review of the literature of the adverse consequences of anemia in the elderly can be broadly divided by the outcomes that were studied. Functional ability, cognitive function, and mortality are three of the most common outcomes studied in this population and are reviewed below. It is important to note that in studies that found worse outcomes in anemic elderly patients, it remains unknown if the anemia itself or the underlying cause of the anemia and/or associated comorbidities is the culprit. We suspect that the underlying cause and comorbidity are responsible for worse outcomes rather than anemia itself.
A number of studies found an association between anemia in the elderly and poor functional status [15–18]. Penninx et al. studied a cohort of 1,146 anemic elderly patients by assessing various markers of physical performance, including a standing balance test, a timed 8-foot walk, and a timed test of 5 chair rises [17]. After adjustment for patients’ baseline performance scores, age, sex, cigarette smoking, blood pressure, and comorbid conditions, anemia was associated with a statistically significant decline in physical performance when compared to a control group. Additionally, separate studies by Penninx et al. showed decreased handgrip and knee extension strength [18] and a higher risk of falls [19] in the anemic elderly.
In addition to its effect on physical performance, anemia in the elderly has been shown to impact cognitive function as well. The Women’s Health and Aging Study showed an association between mild anemia (hemoglobin 10–12 g/dL) and lower executive function in high-functioning, community-dwelling elderly women [20]. In the “Health and Anemia” study, researchers found that anemic elderly persons performed worse on a host of cognitive testing but, after adjustment for possible cofounders, only selective attention remained statistically significant [21]. Hong and colleagues utilized the Health, Aging, and Body Composition study, a prospective cohort of community-dwelling persons aged 70–79, to study the association between anemia and the risk of dementia [22]. Out of 2,552 study participants with available hemoglobin levels, 393 (15 %) were diagnosed with anemia. After 11 years of follow-up, dementia was diagnosed in 23 % of the anemic patients versus 17 % on non-anemic controls. These results remained statistically significant after adjustment for several variables including comorbid conditions. Two earlier studies found similar results with smaller groups of patients and a shorter follow-up period [23, 24].
The most important question is whether anemia in the elderly affects mortality rates. In a study of 755 persons aged 85 and above, risk of mortality was 1.60 (95 % confidence interval, 1.24–2.06; P < .001) in women with anemia and 2.29 (95 % confidence interval, 1.60–3.26; P < .001) in men with anemia after 5 years of follow-up, a finding that remained similar after adjustment for known diseases at baseline [25]. Higher mortality due to malignant neoplasms and infections was found in the anemic cohort. Of note, there was no difference in mortality found from years 5 to 10 of the study.
Mortality in relation to anemia in the elderly was also analyzed using the Cardiovascular Health Study, a cohort of 5,888 community-dwelling elderly persons [4]. After about 11 years of follow-up, mortality rates for those with and without anemia were 57 and 39 %, respectively (P < 0.001). Similarly, the Populations for Epidemiologic Studies of the Elderly cohort was used to show a relative risk of death of 1.61 (95 % confidence interval, 1.34–1.93) when comparing 451 elderly anemic persons to non-anemic persons after adjustment for demographics and baseline comorbidities. This finding remained statistically significant after excluding all patients with certain chronic medical conditions at the onset of the study [26].
7.5 Randomized Controlled Trials of Blood Transfusion in the Elderly
Few large, randomized controlled trials exist on blood transfusions in the elderly. The FOCUS trial by Carson et al., a study of blood transfusions in the postoperative period, provides insight into this question in that nearly all the patients in the study were elderly [27]. This multicenter randomized clinical trial enrolled 2,016 patients aged 50 years or older who underwent surgical repair of a hip fracture with a postoperative hemoglobin level of less than 10 g/dL. Only patients with cardiovascular disease (i.e., history of ischemic heart disease, congestive heart failure, transient ischemic attack, stroke, or peripheral vascular disease or electrocardiographic evidence of a previous myocardial infarction) or cardiovascular risk factors (i.e., hypertension, diabetes mellitus, tobacco history, or a creatinine level above 2.0 mg/dL) were included in the study.
Participants were randomized to either the liberal-strategy or the restrictive-strategy group. In the liberal-strategy group, patients were transfused with blood until their hemoglobin level reached 10 g/dL. Patients in the restrictive-strategy group received blood transfusions at the discretion of the treating physicians to maintain a hemoglobin level above 8 g/dL or for symptoms consistent with anemia (e.g., cardiac chest pain, hypotension, tachycardia, and congestive heart failure). Transfusion was permitted at any time regardless of the hemoglobin level if blood transfusion was deemed necessary to treat active bleeding.
The primary outcome of the FOCUS trial was mortality or an inability to walk 10 ft without human assistance at 60 days. Secondary outcomes included a composite of in-hospital myocardial infarction, unstable angina, or death from any reason. Baseline characteristics were similar between the two groups. The mean age of the study population was 81.6 years. Cardiovascular disease was present in 63 % of the participants, including 40 % with coronary artery disease and about 17 % with congestive heart failure. The median number of units of blood transfused was 2.0 in the liberal-strategy group and 0 in the restrictive-strategy group. The liberal-strategy group had a 1.3 g/dL higher hemoglobin level prior to transfusion as compared to that of the restrictive-strategy group. Almost 60 % of the patients in the restrictive-strategy group did not receive a blood transfusion.
The results showed an odds ratio of 1.01 (95 % confidence interval, 0.84–1.22) comparing the primary outcome (death or inability to walk 10 ft without human assistance at 60 days) in the liberal-strategy group (35.2 %) versus the restrictive-strategy group (34.7 %). Interactions according to age were not significant. Furthermore, the difference in mortality at 30 days was not statistically significant (5.2 % in the liberal-strategy group and 4.3 % in the restrictive-strategy group) nor were the rates of in-hospital myocardial infarction or unstable angina.
Overall, no evidence was found to support maintaining a postoperative hemoglobin level above 10 g/dL as compared to 8 g/dL. The authors note that a “high-risk group of patients with a mean age of more than 81 years” was enrolled, a population “for whom untreated anemia would probably be more harmful than in a healthier or younger population undergoing most surgical procedures.” In other words, despite the old age and high prevalence of cardiovascular disease and other comorbidities, no change in functional ability, mortality, or morbidity was found in a population who may be expected to benefit most from increased hemoglobin- and oxygen-carrying capacity.
The TRICC study performed by Hébert et al. [28] also adds to our knowledge of blood transfusion in the elderly. This randomized, controlled, clinical trial examined a restrictive versus liberal transfusion strategy in 838 critically ill patients across 25 hospitals in Canada in the mid-1990s. Patients were included if they were expected to stay in the intensive care unit for more than 24 h, had a hemoglobin level of 9 g/dL or less within 3 days of admission to the intensive care unit, and were considered euvolemic by their treating physicians. Key exclusion criteria included major active blood loss (a decrease in hemoglobin of 3.0 g/dL or more in the preceding 12 h) and chronic anemia with a hemoglobin level less than 9.0 g/dL.
Patients were then randomized to the liberal- or restrictive-strategy group after being stratified by their APACHE II score. In the liberal-strategy group, patients were transfused to maintain a hemoglobin of at least 10 g/dL with a goal hemoglobin of 10–12 g/dL. Conversely, the goal hemoglobin in the restrictive-strategy group was 7–9 g/dL, such that transfusion was indicated for a hemoglobin less than 7.0 g/dL. Suggestions for the use of intravenous fluids and vasoactive medications were provided but all management decisions were left to the discretion of the treating physicians.
The primary outcome was death from all causes in the first 30 days after randomization, and secondary outcomes included 60-day rates of death from all causes, death during the intensive care unit stay and during hospitalization, and survival times in the first 30 days. The two groups were similar in terms of baseline characteristics. The average age was 57–58 years old. Adherence to the study protocol was excellent. The average daily hemoglobin concentration was 8.5 g/dL in the restrictive-strategy group as compared to 10.7 g/dL in the liberal-strategy group (P < 0.01). Accordingly, patients in the restrictive-strategy group received an average of 3 fewer red cell units.
At the end of the study, the primary outcome (rate of death from all causes after 30 days) was 18.7 % in the restrictive-strategy group and 23.3 % in the liberal-strategy group (P = 0.11; Fig. 7.2). The authors also analyzed a prespecified subgroup of patients 55 years or older as these patients were thought to potentially suffer worse outcomes due to a decreased ability to compensate for anemia. The subgroup of patients >55 years old did not differ significantly in their baseline characteristics from those of younger patients. All outcomes between the two transfusion strategies in older patients were similar. Of note, in patients under the age of 55, the 30-day mortality rate was significantly higher in the liberal-strategy group (13.0 % vs. 5.7 %, P = 0.02).
All in all, while TRICC used a cutoff age of 55 years old, the study failed to show that older adults benefit from a higher hemoglobin level derived from a liberal transfusion strategy.
7.6 Clinical Guidelines on Blood Transfusion in the Elderly
The majority of professional society guidelines on blood transfusions do not incorporate age into their recommendations. For example, the AABB (formerly the American Association of Blood Banks) guidelines, perhaps the most widely used set of recommendations, do not explicitly mention the elderly in their recommendations [29]. However, the authors note that “clinical trials are needed in other patient populations that include…elderly medical patients recovering from illnesses that result in hospitalization….” The “Clinical practice guideline: Red blood cell transfusion in adult trauma and critical care,” published in Critical Care Medicine in 2009, also does not explicitly mention age as a consideration [30]. Other examples of guidelines that fail to specifically comment on the elderly include the 2013 clinical practice guideline of treatment of anemia in patients with heart disease by the American College of Physicians [31] and “Guidelines for transfusion in the trauma patient” by West et al. published in the Journal of Trauma [32].
When mentioned, age is generally considered a small piece of the puzzle in the decision-making process of transfusing blood. Guidelines published in 2001 in the British Journal of Haematology briefly allude to anemia in the elderly in the following statement: “In patients who may tolerate anaemia poorly, e.g. patients over the age of 65 years,…consider adopting a higher concentration at which transfusions are indicated, e.g. when the haemoglobin concentration becomes <8 g/dL” [33].
Similarly, the International Society of Nephrology guidelines on anemia in patients with chronic kidney disease (CKD) reference anemia in the elderly very briefly [34]. In the section entitled “Use of erythropoiesis-stimulating agents and other agents to treat anemia in CKD,” the authors generally recommend a hemoglobin goal of 10 g/dL in the adult patient with CKD. However, the authors go on to caution readers that in certain subsets of patients with CKD stages III–V, it “may not be wise” to allow the hemoglobin level to drift below 10 g/dL, especially in “elderly patients who are more prone to developing symptoms and signs of anemia.”
The Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists Clinical Practice Guidelines, published in the Annals of Thoracic Surgeons in 2012, discuss anemia in the elderly [35]. Ferraris et al. note that several factors contribute to an increased risk of bleeding and the subsequent need for blood transfusion (such as advanced age, preoperative anemia, small body size, multiple comorbidities, etc.). The authors reason that such patients should be identified prior to surgery and “all available preoperative and perioperative measures of blood conservation should be undertaken in this group.” They go on to assert that while these high-risk patient factors are listed as single factors that are either present or absent, many of them represent a spectrum of severity. Age is used as an example of this assertion in that “the risk [of bleeding and the need for blood transfusion] associated with age greater than 75 years is significantly greater than the risk for a patient aged 55 years or younger, and it is quite likely that the risk of transfusion associated with age is not a continuous function.”
7.7 Conclusion
Given the rapid pace of aging in the population and the increased prevalence of anemia with age, anemia in the elderly is an important topic of consideration. The etiology of anemia in this population remains puzzling as high rates of unexplained anemia have been found. Furthermore, it is theorized that the elderly are less able to tolerate anemia due to their inability to mount an adequate physiologic response as compared to that of younger persons. Observational data has shown that anemia is associated with worse outcomes in the elderly, including an increase in mortality. However, given the increased prevalence of diseases such as coronary artery disease, congestive heart failure, chronic kidney disease, and cancer in the elderly, such studies are unable to determine if anemia is the true cause of adverse outcomes or merely a marker of underlying comorbidity. Randomized controlled trials such as the TRICC and FOCUS studies, which included a large proportion of elderly patients with cardiovascular disease and risk factors, did not show evidence that a liberal versus restrictive blood transfusion strategy improves outcomes. Major society guidelines have not set forth specific recommendations on the topic of adopting a restrictive versus liberal blood transfusion strategy in the elderly, a result of the lack of randomized clinical trials that specifically address the subject.
All in all, anemia is a common disease affecting the elderly and has been shown in observational data to portend worse outcomes, but there is no evidence to incorporate age itself in developing a blood transfusion strategy.
References
Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC. Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004;104:2263–8.
Inelmen EM, D’Alessio M, Gatto MR, et al. Descriptive analysis of the prevalence of anemia in a randomly selected sample of elderly people living at home: some results of an Italian multicentric study. Aging (Milan, Italy). 1994;6:81–9.
Salive ME, Cornoni-Huntley J, Guralnik JM, et al. Anemia and hemoglobin levels in older persons: relationship with age, gender, and health status. J Am Geriatr Soc. 1992;40:489–96.
Zakai NA, Katz R, Hirsch C, et al. A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort: the cardiovascular health study. Arch Intern Med. 2005;165:2214–20.
Robinson B, Artz AS, Culleton B, Critchlow C, Sciarra A, Audhya P. Prevalence of anemia in the nursing home: contribution of chronic kidney disease. J Am Geriatr Soc. 2007;55:1566–70.
Artz AS, Fergusson D, Drinka PJ, et al. Prevalence of anemia in skilled-nursing home residents. Arch Gerontol Geriatr. 2004;39:201–6.
Price EA, Mehra R, Holmes TH, Schrier SL. Anemia in older persons: etiology and evaluation. Blood Cells Mol Dis. 2011;46:159–65.
Hebert PC, Van der Linden P, Biro G, Hu LQ. Physiologic aspects of anemia. Crit Care Clin. 2004;20:187–212.
Curtis LH, Whellan DJ, Hammill BG, et al. Incidence and prevalence of heart failure in elderly persons, 1994-2003. Arch Intern Med. 2008;168:418–24.
Members WG, Roger VL, Go AS, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–220.
Makipour S, Kanapuru B, Ershler WB. Unexplained anemia in the elderly. Semin Hematol. 2008;45:250–4.
Ferrucci L, Maggio M, Bandinelli S, et al. Low testosterone levels and the risk of anemia in older men and women. Arch Intern Med. 2006;166:1380–8.
Rossi DJ, Jamieson CHM, Weissman IL. Stems cells and the pathways to aging and cancer. Cell. 2008;132:681–96.
Dumble M, Moore L, Chambers SM, et al. The impact of altered p53 dosage on hematopoietic stem cell dynamics during aging. Blood. 2007;109:1736–42.
Chaves PH, Semba RD, Leng SX, et al. Impact of anemia and cardiovascular disease on frailty status of community-dwelling older women: the Women’s Health and Aging Studies I and II. J Gerontol A Biol Sci Med Sci. 2005;60:729–35.
Chaves PH, Ashar B, Guralnik JM, Fried LP. Looking at the relationship between hemoglobin concentration and prevalent mobility difficulty in older women. Should the criteria currently used to define anemia in older people be reevaluated? J Am Geriatr Soc. 2002;50:1257–64.
Penninx BW, Guralnik JM, Onder G, Ferrucci L, Wallace RB, Pahor M. Anemia and decline in physical performance among older persons. Am J Med. 2003;115:104–10.
Penninx BW, Pahor M, Cesari M, et al. Anemia is associated with disability and decreased physical performance and muscle strength in the elderly. J Am Geriatr Soc. 2004;52:719–24.
Penninx BW, Pluijm SM, Lips P, et al. Late-life anemia is associated with increased risk of recurrent falls. J Am Geriatr Soc. 2005;53:2106–11.
Chaves PH, Carlson MC, Ferrucci L, Guralnik JM, Semba R, Fried LP. Association between mild anemia and executive function impairment in community-dwelling older women: The Women’s Health and Aging Study II. J Am Geriatr Soc. 2006;54:1429–35.
Lucca U, Tettamanti M, Mosconi P, et al. Association of mild anemia with cognitive, functional mood and quality of life outcomes in the elderly: the “Health and Anemia” study. PLoS One. 2008;3:e1920.
Hong CH, Falvey C, Harris TB, et al. Anemia and risk of dementia in older adults: findings from the Health ABC study. Neurology. 2013;81:528–33.
Atti AR, Palmer K, Volpato S, Zuliani G, Winblad B, Fratiglioni L. Anaemia increases the risk of dementia in cognitively intact elderly. Neurobiol Aging. 2006;27:278–84.
Shah RC, Buchman AS, Wilson RS, Leurgans SE, Bennett DA. Hemoglobin level in older persons and incident Alzheimer disease: prospective cohort analysis. Neurology. 2011;77:219–26.
Izaks GJ, Westendorp RG, Knook DL. The definition of anemia in older persons. JAMA. 1999;281:1714–7.
Penninx BW, Pahor M, Woodman RC, Guralnik JM. Anemia in old age is associated with increased mortality and hospitalization. J Gerontol A Biol Sci Med Sci. 2006;61:474–9.
Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–62.
Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340:409–17.
Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med. 2012;157:49–58.
Napolitano LM, Kurek S, Luchette FA, et al. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. J Trauma. 2009;67:1439–42.
Qaseem A, Humphrey LL, Fitterman N, Starkey M, Shekelle P. Treatment of anemia in patients with heart disease: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159:770–9.
West MA, Shapiro MB, Nathens AB, et al. Inflammation and the host response to injury, a large-scale collaborative project: patient-oriented research core–standard operating procedures for clinical care: IV. Guidelines for transfusion in the trauma patient. J Trauma Acute Care Surg. 2006;61:436–9. doi:10.1097/01.ta.0000232517.83039.c4.
Murphy MF, Wallington TB, Kelsey P, Boulton F, Bruce M, Cohen H, Duguid J, Knowles SM, Poole G, Williamson LM, British Committee for Standards in Haematology, Blood Transfusion Task Force. Guidelines for the clinical use of red cell transfusions. Br J Haematol. 2001;113:24–31.
Kidney Disease: Improving Global Outcomes (KDIGO) Anemia Work Group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl. 2012;2:279–335.
Ferraris VA, Ferraris SP, Saha SP, et al. Perioperative blood transfusion and blood conservation in cardiac surgery: the Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists clinical practice guideline. Ann Thorac Surg. 2007;83:S27–86.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Czaja, M.T., Carson, J.L. (2015). Red Blood Cell Transfusion in the Elderly. In: Juffermans, N., Walsh, T. (eds) Transfusion in the Intensive Care Unit. Springer, Cham. https://doi.org/10.1007/978-3-319-08735-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-08735-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-08734-4
Online ISBN: 978-3-319-08735-1
eBook Packages: MedicineMedicine (R0)