Abstract
Medical and diagnostic evaluation of musculoskeletal trauma is a complex issue for several aspects.
Every year, a quarter of the child population goes to the emergency department for an orthopedic trauma.
Around 40 % of the musculoskeletal traumas in the young population are sports-related, involving mostly male patients (2:1).
It is known that an erroneous diagnosis and further mishandling of orthopedic pediatric injuries may cause future disabilities in the patient.
This is why diagnostic imaging plays a very important role in this given scenario, thanks to the use of different types of techniques, confirming clinical data and evaluating the follow-up of the lesion.
Several imaging modalities are used in sports medicine.
X-ray imaging is the first technique of choice for the study of the bone component. Ultrasound (US) and magnetic resonance imaging (MRI) are the main imaging modalities in studying and approaching issues concerning tendons, ligaments, muscles, and osteochondral cartilage.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
6.1 Introduction
Medical and diagnostic evaluation of musculoskeletal trauma, together with epidemiologic data, is a complex issue for several aspects.
Firstly, it is because of the anatomy and physiological changes of the musculoskeletal system during physical and psycho-attitudinal growth.
Around 10–15 % of the overall pediatric traumas are represented by musculoskeletal injuries.
Around 40 % of the musculoskeletal traumas in the young population are sports-related, involving mostly male patients (2:1).
During the child’s growth, the characteristics of the musculoskeletal apparatus are unique, so it is necessary and important to know the anatomy and physiological changes during the growth in order to better understand and evaluate injuries and to perform the most adequate and correct management.
It is known that an erroneous diagnosis and further mishandling of orthopedic pediatric injuries may cause future disabilities in the patient.
X-ray imaging represents the first technique of choice for the study of the bone component, even though it is not fully satisfying with respect to soft tissue injuries.
Ultrasound (US) and magnetic resonance imaging (MRI) are the main imaging modalities in studying and approaching issues concerning tendons, ligaments, muscles, and osteochondral cartilage.
Every year, a quarter of the child population goes to the emergency department for an orthopedic trauma.
During early childhood, most traumas are caused by falls (1/3) and car accidents (1/5), especially for young children involved in pedestrian and bike-riding accidents, and later on, teenagers are involved in trauma during sports activities (1/10), at an amateur or competitive level.
The increasing incidence of sports trauma is due to the increase of the number of young people doing sports activity and of the number of sport/fitness centers.
Furthermore, sports activity is often suggested by pediatrics in helping the child’s physical and psycho-attitudinal growth, in strengthening self-confidence, and for possibilities of creating new relationships and friends. This is often supported by the family that considers the success in sports as an improvement in their child’s future social life.
The basic principle is that a child is not “a small adult” and traumatic injury and radiological appearance can be different in childhood from that in other ages.
In all young athletes, but mainly in those that play sports at a competitive level, an early diagnosis of the injury allows to determine the recovery period and allows the patient to start playing sports again in the best possible safety conditions.
This is why diagnostic imaging plays a very important role in this given scenario, thanks to the use of different types of techniques, allowing to confirm clinical data and evaluate the follow-up of the lesion.
Another important topic is that the musculoskeletal system can be affected, in both acute and chronic injury, by different and simultaneous lesions, such as muscle trauma contusions (of different degrees), tendon and/or ligament injuries, fracture or joint dislocation, frequently in combination between them.
Several imaging modalities are used in sports medicine.
Ultrasound has many positive aspects: basically easy to use, inexpensive, widely used, and totally safe.
The radiologist who carries out the musculoskeletal ultrasound is highly supported by an “interactive” method with the patient, which allows to depict and locate the involved area in real time and carry out comparative views and dynamic maneuvers eventually by using power Doppler, useful for the muscular injury follow-up.
This method has a high-level sensibility in muscular injuries (distraction, contusion), both tendinous and ligamentous (75 % sensibility and 90 % specificity), and in evaluating superficial hematoma.
The main limit of ultrasound is to be strongly dependent by the physician so it is necessary for radiologists, handling musculoskeletal injuries, to have confidence with it, and be supported by an important background experience and knowledge skill in clinical cases concerning pediatric pathologies.
Thanks to its high spatial and contrast resolution, MR imaging is a method that allows to carry out a detailed and complete study on tendinous, cartilaginous, and osteochondral components, all issues in which an injury is suspected and where first-level exams are inconclusive.
Furthermore, MRI being without radiation exposure, it is particularly recommended in the “management” of pediatric patients especially in young athletes that must undergo follow-ups after traumatic injury in the monitoring of complete “restitutio ad integrum.”
6.2 Upper Limb
6.2.1 Clavicle Fractures
Clavicle fracture is the most common fracture of the child owing to its superficial anatomical position.
It may occur during natural childbirth in high-weight children or during a difficult delivery, generally at the level of the middle-distal third, due to the pressure of the shoulder against the symphysis pubis in the ejection phase.
An anteroposterior radiograph can easily be achieved for the diagnosis, but also ultrasonography can be useful to highlight the discontinuity of the bone heads in those cases of incomplete lesions and in the follow-ups.
Ultrasound may be usefull.
In older children, they are due to trauma from a fall with the arm in extension or to a side impact.
The most common site is the middle third, the less flexible point (75–80 %), then the lateral third (15–20 %), and the medial bone (5 %) [1].
Clinically, pain with any shoulder movement and upon holding the arm across the chest and tenderness over the fracture can be observed.
In the third side fractures, the latter one is displaced downward owing to the weight of the arm and to the action of the pectoralis major and latissimus dorsi muscles, while in third-medium fractures, the bone fragment is displaced upward by the action of the sternocleidomastoid muscle.
Complications are rare but they must be recognized as the damage of the neurovascular bundle or pleuropulmonary lesions may occur.
In case of more complex injuries or when it is associated with a sternoclavicular joint dislocation, CT is indicated, especially CT angiography, to rule out potential vascular injury.
Sternoclavicular joint dislocation is anterosuperior in 90 % and posterior in the remaining 10 %; it is difficult to diagnose on plain radiographs and it can be associated with other complications.
Nonunion is common in clavicle fractures that occur distal to the attachment of the coracoclavicular ligament.
Stress or “academic” clavicular fractures may be seen in students who carry heavy loads of books on their shoulders.
Acromioclavicular joint dislocation represents 12 % of all shoulder injuries, and it is more common than clavicular ones (98 %) and has been subdivided into six types of growing instability.
US is very useful and more sensitive than x-ray, especially in low-grade lesions.
6.2.2 Shoulder: Acute Injuries
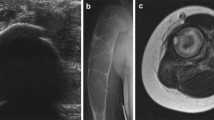
Children acute shoulder fractures commonly involve the proximal humeral and scapular aspect. Most of them are clearly diagnosed by x-ray. However, avulsion fractures in the coracoid and glenoid growth center are more difficult to detect by radiographs, and in these cases, US or MRI might be necessary for the diagnosis [2] (Fig. 6.1).
The addition of several imaging modalities can be useful also for the diagnosis of preexisting pathologies (Fig. 6.2).
A young female patient with a history of a known juvenile bone cyst presenting with acute pain after a fall. (a) US shows irregularity of the cortical zone. (b) Anteroposterior view of the right shoulder confirmed the cyst rupture with cortical interruption. (c) Axial T2-weighted image highlights the presence of a double-density fluid-level lesion within the bone, associated with an inhomogeneous intensity of adjacent soft tissue, appearing edematous and inflamed
Traumatic glenohumeral dislocations usually occur in collision sports, such as football and hockey. It is a disorder of the growing-up age, and about 40 % of these occur in patients under the age of 22, although it is uncommon in younger children, with only 1.6 % seen in patients under the age of 10 years [3, 4].
Recurrent dislocation and glenohumeral instability are common after a first-time dislocation and have the highest incidence in patients with open physis.
Most glenohumeral dislocations are anterior with the humerus abducted and externally rotated at the time of the impact with anteroinferior aspect of the humeral head.
The labro-ligamentous complex can be avulsed from the glenoid (classic Bankart lesion) with or without disruption (distacco) of the adjacent scapular periosteum or with bony glenoid fracture (bony Bankart).
The impact of the posterolateral aspect of the humeral head may create a visible depression in the humeral head (Hill-Sachs defect), seen in 38–90 % of patients [5].
Hill-Sachs defect is associated with a higher incidence of recurrence (82 % vs 50 %) [3, 6, 7].
In patients with recurrent instability, a more detailed imaging is mandatory.
A great deal of soft tissue capsulolabral injuries associated with acute or chronic recurrent dislocations or instability and diagnosis is best provided by MRI.
Many authors agree that MR arthrography is the most accurate technique, with the greatest efficacy in the younger, athletic population [8, 9] and an overall sensitivity of 91 % for the detection of labral pathology.
HAGL lesion (humeral avulsion of the glenohumeral ligament) is very important to recognize on MRI; the anterior band of the inferior glenohumeral ligament is torn from its humeral neck attachment and can be seen on MRI as a “J” sign.
About two-thirds of HAGL lesions are associated with other shoulder pathologies, such as labral tears, rotator cuff tears, and Hill-Sachs alterations [10, 11].
Failure to recognize these types of lesions leads to recurrent instability; MR diagnosis is important in surgical planning [11].
Ultrasound has a poor indication in cases of instability; therefore, in these cases, it can be useful in the assessment of fluid collection or indirect signs of instability at the level of the long head of the biceps, the glenohumeral ligament, or the acromioclavicular joint.
Posterior dislocation is less common, and it usually occurs with an axial loading of an adducted internally rotated arm, violent muscle contraction, or posterior glenoid deficiency, as occurs in brachial plexus palsy [12].
MRI is usually performed in order to evaluate the presence of a posterior labral tear, a capsular rent, a “reverse” Hill-Sachs, or an abnormal glenoid version [13, 14].
Superior labral anterior to posterior (SLAP) tears occurring in children are due to microtrauma associated with overhead throwing or are traumatic. In throwers, they are caused by the increased external rotation during the cocking phase, producing enormous torsional stresses at the biceps anchor and the superior labrum causing the detachment of the labrum medially, over the corner of the glenoid.
Another cause of SLAP tears in throwers is the internal impingement; it occurs when the arm is abducted and externally rotated, as we have in the cocking phase, leading to repetitive contact between the humeral and the posterosuperior aspect of the glenoid.
In addition may be those traumas producing traction or compression on the biceps anchor, such as a fall onto an outstretched arm [15, 16].
MRI is mandatory in SLAP tears when surgery is planned; typical MR findings consist of rotator cuff tears, anterior and posterior labral tears, paralabral cysts, and chondral injuries.
MRI can recognize the normal variants of the anterior labrum: the superior sublabral recess, the sublabral foramen, and the Buford complex [17].
MRI can recognize the presence of a paralabral or spinoglenoid notch cyst, associated with persistent symptoms and failure of nonoperative treatment in children with SLAP tears, or compression of the suprascapular nerve and denervation of the infraspinatus [18].
6.2.3 Shoulder: Chronic Repetitive Trauma
Repetitive stress is the leading cause of shoulder injuries in younger athletes. Most of them are observed during the mid to the late teen years, due to the increase of stress forces applied to muscular structures in this age group. These particular conditions have been often observed in baseball players but also in football, swimming, tennis, and all those sports requiring an overhead activity [19].
Little leaguer’s shoulder is a descriptive term used to refer to a stress-related injury of the proximal humeral physis, characterized by the epiphysiolysis of the proximal humeral growth plate.
It usually occurs in 11- to 16-year-olds, presenting with dominant arm shoulder pain aggravated by throwing and tenderness to palpation.
This condition affects those athletes who frequently repeat the action of overhead throwing, such as baseball players, track-and-field athletes, only later volleyball players, tennis players, and swimmers. It is a benign and self-limited condition responding well to conservative treatment [20].
It is characterized by the widening and irregularity of the proximal humeral physis, easily detectable both on x-ray and MRI, which can also highlight the logistic aspect as an area of high signal intensity on T2-weighted images [21].
Rotator cuff injuries are rare in children because the rotator cuff in young patients is more elastic and stronger, without the degenerative changes observed in the elderly population.
They usually occur as tendonitis or strain in response to repetitive microtrauma caused by overhead arm motion.
In younger athletes, rotator cuff injuries are often associated with joint instability [5, 22].
Primary impingement can occur as a result of a tight coracoacromial arch or simple overuse.
With repetitive stress, the muscle becomes weaker and rotator cuff impingement can result from a multidirectional instability.
These injuries are the major indicators for an ultrasound examination.
They can be classified as complete, incomplete, or partial (sensitivity: 91 %) [9].
Complete lesions extend over the whole thickness from the articular side to the bursal one, presenting hypo-anechoic focal areas with evidence of joint effusion within the coracoid and axillary recesses or in the anatomical locations of tendons. In complete rupture, the tendon is no longer recognizable and tucked beneath the coracoacromial arch.
Other described signs are the double cortex sign, the sagging peribursal fat sign, compressibility, and muscle atrophy.
A partial lesion is characterized by a hypo-anechoic area with poorly defined margins affecting only the articular or bursal portion of the tendon.
However, there is a spectrum of non-rotator cuff abnormalities that are amenable to US examination, including the instability of the biceps tendon, glenohumeral joint, and acromioclavicular joint; arthropathies and bursitis (inflammatory diseases, degenerative and infiltrative disorders, infections); nerve entrapment syndromes; and space-occupying lesions.
MRI is the modality of choice for the evaluation of rotator cuff tears.
When a tendinopathy occurs, it is easy to see an intermediate signal intensity on T2-weighted images within the tendon.
A full-thickness tear appears as a hyperintensity on T2-weighted images extending completely through the tendon. A complete tear disrupts the tendon completely, with musculotendinous retraction and a possible upward subluxation of the humeral head.
A partial-thickness tear may present both on the articular and bursal surface and appears as a hyperintensity on T2-weighted images extending through the tendon thickness, superiorly or inferiorly [23, 24].
A rim-rent tear is a partial articular tear of the insertional fibers of the rotator cuff at the greater tuberosity; it is considered as a form of partial rotator cuff tear, and it may involve both the supraspinatus and infraspinatus insertion. If left untreated, it may progress to a full-thickness tear [25].
Subscapularis tendon tears are less common and are frequently associated with biceps tendon abnormalities.
Internal impingement is characterized by the entrapment of the undersurface of the posterior supraspinatus tendon or anterior infraspinatus tendon between the humeral head and posterior glenoid. Undersurface tears of one or both tendons with cystic changes in the posterior humeral head and posterosuperior labral pathology are diagnostic for internal impingement [26].
In conclusion, once adequate radiographs have been obtained to exclude apparent bone disorders, high-resolution US should be the first-line imaging modality in the assessment of non-rotator cuff disorders, assuming the study is performed with high-end equipment by an experienced examiner. More costly and invasive modalities such as MR imaging and MR arthrography should be reserved for bone marrow evaluation and preoperative assessment.
6.2.4 Elbow: Acute Injuries
Pediatric elbow joint trauma is challenging and particularly complex mainly because of the complex anatomy and the presence of several growth plates appearing in different phases of the growing process.
In children, elbow trauma may lead to bony, cartilaginous, or soft tissue injury.
In most of cases, basic radiographs compared with the injured elbow can allow a complete evaluation of injuries, such as joint effusions or fractures, identifying injuries that require surgical intervention, obviating the need for multiplanar imaging.
A careful assessment of soft tissues can provide information about the presence of a possible fracture, because it is frequently associated with the presence of joint effusion.
In the L-L radiogram, when effusion is present, the “fat-pad sign,” reported in 1954, will appear both anteriorly and posteriorly to the third distal aspect of the humerus.
When an anterior conspicuous dislocation of the fat pad is observed, it will result in the classic “sign of the sail,” which is very important because about 90 % of young patients with these radiographic features have a fracture of the elbow. The posterior humeral fat pad is not visible on a normal elbow and becomes visible in the presence of joint effusion.
However, x-ray does not show bone bruising or cartilaginous or soft tissue injury and may underestimate physeal injury, as demonstrated by Beltran and Rosenberg [27] who reported, in a study comprising of eight patients with elbow fractures, that two children had unsuspected transphyseal fracture extension through the unossified epiphyseal cartilage shown by MR imaging.
Carey et al. [28] reported that in 14 suspected physeal injuries, MRI changed the radiographic diagnosis in 50 % of the cases by showing either radiographically occult fractures or unsuspected transphyseal extension. MR findings resulted in a change of treatment in 36 % of the cases.
MRI can improve the understanding of complex trauma; confirm the presence of an occult fracture suggested just by a joint effusion on x-ray; show the condition of the surrounding musculotendinous structures, such as the insertion of biceps muscle upon the radial tuberosity; and evaluate the ulnar nerve, because of its path posteriorly around the medial epicondyle.
In fact, as demonstrated by Major and Crawford, MRI highlighted marrow edema and missed fractures in 13 patients whose initial posttraumatic elbow showed just a joint effusion without fracture [29].
In children of less than 2 years, before the mineralization of secondary growth plates, bony landmarks are not present, limiting the accuracy of x-rays. On the contrary, MRI may easily visualize the unossified growth plate and the cartilage, providing a good contrast between joint fluid, cartilage, and ossified bone [30].
The joint is well assessed by ultrasound which allows the evaluation of tendons, ligaments, muscles, and neurovascular components.
It also allows the assessment of any intra-articular body and the search for any incomplete fracturative lesion where painful swelling is visible.
Pediatric elbow injuries are commonly classified as lateral compression, medial tension overload, and extension overload depending on the mechanism of injury.
They typically occur during the acceleration phase of the throwing cycle when enormous forces are applied on the elbow joint.
In fact, during this phase, compressive forces are applied laterally, across the radiocapitellar joint; tensile forces are exerted medially across the ulnar collateral ligament and flexor/pronator muscle group; posterior tensile forces are applied as the triceps muscle contracts; and impaction forces are exerted as the olecranon extends into the olecranon fossa [31].
Some authors described that about 17–20 % of baseball pitchers between 9 and 15 years of age experience elbow pain during their careers. The incidence of elbow injuries is directly correlated with pitching frequency and is higher for pitchers who throw with poor technique [32–34].
Acute elbow injuries in the pediatric age are not only a characteristic of sports activities; they often occur because of a fall onto an outstretched hand, seen within or outside the sports field.
Medial epicondylar avulsion fracture: It is common (12 % overall) and sometimes associated with the alteration of normal articular relations; they are classified into two types by Woods.
It often occurs among baseball pitchers (7–15 years old) as the medial epicondyle begins to fuse. It is the result of a violent valgus force exerted on the elbow during overhead throwing with a contemporary contraction of the flexor/pronator muscle group.
Radiography is often diagnostic, although US and MRI might be useful when we have an avulsed fracture fragment difficult to see on x-rays [35].
Ulnar collateral ligament (UCL) lesion: In an older adolescent with a fused epicondyle, the UCL may be torn, partially (involving the deep intracapsular layer of the anterior bundle) or completely (more common, involving the midsubstance of the anterior bundle) [36].
It is an uncommon injury and US and MRI can easily depict this kind of lesion.
On T2-weighted MRI sequences, a disruption of the ligament and wave aspect of the fibers and increased intensity can be noticed.
However, the radiologist must be careful about the interpretation of the high signal intensity at the origin of the ligament, because a mild increase of T2 signal intensity at the origin is normal also in the immature skeleton.
Partial tears occur at the ulnar insertion, and in this case, MRI shows the “T” sign, which is the high signal intensity at the distal site of the ligament.
Tendon lesions: They most commonly occur at the distal side of the biceps and at the insertion site of the triceps.
Biceps lesions typically occur during the teenage phase, and they are commonly due to a lift effort; they are well depicted by both US and MRI.
US evaluation can be challenging because of its complex anatomy.
It is important to evaluate also the contralateral elbow and to perform the dynamic tests.
The distal biceps tendon has no tendon sheath that lies in the anterior compartment of the elbow, superficial to the brachialis muscle. Its tendon passes through the antecubital fossa to insert on the radial tuberosity.
Ultrasound examination shows thickening of the tendon fibers, muscle retraction, and the presence of blood infarction.
Searching for the triceps tendon injuries, the comparative radiological evaluation of the elbow in L-L projection is critical; in addition, US is very useful for the diagnosis of complete and partial tears, providing an alternative to MR imaging [37, 38].
6.2.5 Elbow: Chronic Repetitive Trauma
During school age, the shoulder, elbow, and wrist can be susceptible to many sports-related overuse injuries.
Little leaguer’s elbow: It is a term used to describe those injuries which affect the medial, lateral, and posterior compartments of the elbow of throwers and gymnasts, in which the “primum movens” is the repetitive valgus overload [39].
Classic little leaguer’s elbow: During childhood and adolescence, the weakest site is the medial epicondyle physis, where chronic and repeated stress, aged by the common tendon of the flexor/pronator muscles and the ulnar collateral ligament, results in the irritation of the physeal cartilage. When it becomes chronic, it is easily detectable by the widening of the medial epicondyle physis, irregularity of the margins, and, eventually, sclerosis and fragmentation [40].
The most common radiographic manifestations are displacement and fragmentation of the medial epicondyle apophysis, although plain film can be normal in up to 85 % of cases.
US and MRI are very useful, especially in those cases in which there is a high clinical suspicion but radiographs are normal.
Sonography has a great ability to medial epicondylar fragmentation.
The epicondyle shows a large area of marrow edema, the physis being widened and hyperintense on T2-weighted images; a thickening of common flexor tendon could also be shown.
Panner disease: It is an osteochondral lesion responsible for lateral elbow pain in children.
It is attributed to avascular necrosis of the capitellum and typically affects the dominant elbow of boys aged 5–12 years.
The onset age is younger than that of patients with osteochondritis dissecans (OCD), occurring during the period of active ossification of the capitellar epiphysis [41].
X-ray shows lucency adjacent to the capitellar articular surface with mild surrounding sclerosis. Days later, larger areas of capitellar radiolucency mixed with diffuse sclerotic changes are clearly visible.
MRI is much more sensitive than x-ray in the early detection of Panner disease; in fact, it can demonstrate diffuse capitellar marrow edema. Normalization of capitellar appearance usually occurs within 1–2 years.
Almost all patients affected by Panner disease recover well, with no treatment, and fully reconstitute the normal architecture of the capitellum.
Osteochondritis dissecans (OCD) of the capitellum: It typically occurs in older adolescents aged 11–15 years, when the capitellar epiphysis is almost completely ossified. It consists of a fragment of the capitellum separated or isolated from the surrounding bone. The cause is still unclear, but many authors suggest that it could be a combination of repetitive microtrauma across the radiocapitellar joint and the mild blood supply of the capitellum [41].
Baseball players and gymnasts are often affected by this condition, perhaps because of distraction forces across the medial elbow producing tension forces across the lateral joint.
OCD begins on the anterolateral aspect of the capitellum as a mild subchondral lucency, while Panner disease involves the entire ossification center.
Later on, there is an increasing process of lytic and sclerotic changes with the flattening and fragmentation of the capitellum. Advanced aspects of OCD are characterized by loose body formation, expansion of the radial head, and osteophyte formation.
Sonography is very sensitive to detect OCD capitellar fragmentation.
MRI spectrum of OCD is more severe than that of Panner disease, including abnormal marrow signal, cystic changes, cartilaginous defects, fragmentation, and intra-articular loose bodies.
Two patterns of OCD presentation have been described: one pattern shows a low-signal-intensity ring surrounded by an intermediate area on T1-weighted sequences; the inner portion of the ring is hyperintense on T2-weighted images. The second pattern is characterized by a segmental area of hypointensity on T1-weighted images, which is hyperintensity on T2-weighted ones.
The use of MRI arthrography with gadolinium improves the staging of osteochondral lesions; in fact, in unstable lesions, we observe some fluid or contrast agent encircling the fragment or a cystic lesion under the fragment on T2-weighted images.
MRI not only makes diagnosis and evaluates its extension and the possible presence of displaced fragments, but it can also assist with the evaluation of the stability of the lesion.
Stable lesions have a focus of low signal intensity on T1-weighted images and high signal intensity on T2-weighted images in a portion of the anterior capitellum.
MR instability criteria are a rim of high T2 signal intensity around the lesion, disruption of the subchondral bone plate, cartilage cracks around the lesion and cysts inside it, or displaced fragments [41].
The presence of intra-articular contrast material around the lesion suggests disruption of the articular surface, indicating the instability of the lesion.
Post-contrast MRI can also be used in order to evaluate patients affected by OCD. The use of i.v. gadolinium contrast may help assess the stability and viability of the lesion. In fact, enhancement of the lesion suggests that it is viable and with good blood supply. On the other hand, the presence of a ring of diffuse enhancement between the OCD lesion and adjacent subchondral bone might represent granulation tissue, indicating that the lesion is unstable.
The last component is the posterior elbow involvement. In fact, during throwing or tumbling, the triceps may impute strong traction on the olecranon, known as “extension overload,” in which the first site affected is the olecranon physis. This condition is characterized by apophyseal widening, irregularity, and delayed closure.
6.2.6 Wrist and Hand: Acute Injuries
Plain film radiographs can provide a detailed evaluation of bone injuries, the degree of radial foreshortening, abnormalities or angulation of the distal radius, possible ulnar fracture or dislocation, and so on.
However, MRI allows additional evaluation of soft tissue supporting structures, especially the intercarpal ligaments and the triangular fibrocartilage (TFC).
TFC tears may occur not only as a long-term result of gymnast wrist or positive ulnar variance but also acutely. In younger athletes, traumatic injuries with respect to the degenerative ones are most common [42, 43].
TFC tears can be a partial-thickness defect or complete perforation through the entire thickness of the disk and can affect both the central (radial) side and the peripheral (ulnar) side. This distinction is important because it affects the treatment; in fact, tears of the ulnar side are repaired because of the rich vascular supply, while central tears are debrided [44].
Clinically, they manifest with ulnar-side wrist pain and a palpable click, associated also with swelling and loss of grip strength.
At MRI, a partial tear is characterized by an irregular or linear surface defect, whereas a complete tear or perforation shows a hyperintense linear abnormality on T2-weighted images. MR arthrography increases MR sensitivity in detecting TFC tears [45].
There is not a great deal of formal studies about the scapholunate tears in the pediatric population, and for this reason, we cannot use the adult upper limit of 2 mm for the normal width of the space between the two bones until the age of 12 [46].
Distal forearm and scaphoid fractures in children often occur from falls onto an outstretched hand.
Diagnosis is usually achieved by x-ray, but in some cases, it may be difficult to visualize on plain films, although the fracture is present. In fact, occult scaphoid fractures represent 10–15 % of the whole scaphoid lesions. In these cases, MRI may help to identify an occult scaphoid fracture, showing areas of high signal intensity on T2-weighted images, especially in those obtained with short-tau inversion recovery (STIR) (Fig. 6.3) [47].
Scaphoid fracture in a 16-year-old-basketball player occurred after a direct blow to the palm. (a) T1-weighted image on the coronal plane shows an inhomogeneous aspect of the distal scaphoid pole, characterized by a diffuse area of low signal intensity, with a subtle fracture within it. (b) VRT reconstruction on the coronal plane shows the irregular presentation of the distal pole, finding suggestive of fracture. (c) Fracture of the body scaphoid, misdiagnosed on plain film in a 10-year-old girl, occurred after a fall onto an outstretched hand. T1-weighted image on coronal plane shows a subtle linear image of low signal intensity at the middle aspect of the bone, suggestive of fracture
US can highlight an irregular aspect of cortical zone which can be misdiagnosed on plain film; it can also show effusion or compartmental hematoma.
Pediatric patients are more likely to suffer from scaphoid tuberosity fracture, which are innocuous unlike scaphoid waist fracture, which may lead to osteonecrosis or nonunion of the proximal pole. Non-displaced waist fracture may appear silent on an initial x-ray; in patients with persistent snuffbox tenderness, MRI can be performed in order to exclude an occult fracture. In this sense, MRI has a 100 % sensitivity for scaphoid fractures, showing a high signal intensity on T2 and a low signal infraction on T1-weighted sequences.
Besides, MRI may also demonstrate marrow edema, and it can also show causes other than fracture, responsible for the patient’s pain, such as osseous and soft tissue contusions and capsular-ligament injuries, clinically known as “dorsal wrist pain.”
US can be defined as the technique of choice in order to search for ligamentous or tendon lesions.
Gamekeeper’s thumb is a common injury in football and basketball players and skiers that occurs following abnormal radially directed force on an abducted thumb. Rupture of the UCL may be total or partial at the distal point of insertion. An avulsion fracture fragment at the ulnar base of the thumb proximal phalanx is typical at the site of UCL attachment. US can show a ligament thickening with an alteration of its normal architecture.
With respect to the contralateral site, it is possible to observe an asymmetrical widening of the first metacarpophalangeal joint on the affected site [48].
MRI is occasionally used to evaluate the soft tissue injury of trigger finger distal avulsion fractures and UCL in patients with a suspected gamekeeper’s thumb prior to surgical intervention.
In some UCL tears, we may have the interposition of the adductor aponeurosis between the torn UCL and the bone, a condition known as “Stener lesion,” which requires surgical intervention.
Mallet finger occurs when there is an abrupt axial load on a partially flexed finger, and it is characterized by the avulsion of the extensor digitorum tendon from the dorsal aspect of the distal phalanx. This avulsion may be tendinous or, more commonly, go with a small bone fragment of the phalanx. It is easily detectable radiographically [49].
If an avulsion fracture occurs on the volar aspect of the distal phalanx, it is termed “jersey finger,” and it develops at the insertion site of the flexor digitorum profundus tendon.
6.2.7 Wrist and Hand: Chronic Injuries
Only a small percentage of young athletes are affected by an overuse condition of the wrist related to wielding rackets, bats, and clubs.
The primary and better known overuse condition of the wrist is the so-called gymnast wrist, more common in female gymnasts, which consists of several conditions affecting the triangular fibrocartilage (TFG) complex tears, interosseous ligament tears, scaphoid stress fractures, ulnar impaction, and ganglion cyst formation.
The repetitive weight bearing on the wrist leads to physeal stress changes of the distal portion of the radius and, sometimes, the ulna. If the injury is stopped, the growth plate may recover itself and the radius may return to normal length; on the contrary, a positive ulnar variance could develop, since the ulna does not undergo the same forces and suffer the same injuries.
The radial physis appears widened, irregular with metaphyseal sclerosis and mild breaking. Later on, the radius appears short due to a delayed growth
MR imaging is more sensitive than x-ray in the detection of physeal changes.
6.3 Lower Limb
6.3.1 Pelvis
Avulsion fractures are common in young athletes aged between 11 and 16 years with a predominance in males.
They usually occur in a “locus minoris resistentiae,” represented by the insertion of the tendons at the level of the apophysis that are secondary ossification centers before the fusion. They are mostly composed by cartilage.
Some biomechanical conditions may determine its detachment, such as excessive lengthening or eccentric contraction, especially in subjects with an imbalance of muscle groups.
The biomechanics of these lesions are the same as those in adults, and they are due to a high degree of muscle injuries generally at the myotendinous junction.
X-ray of the pelvis is usually sufficient for the diagnosis and to assess the extent of the lesion.
Ultrasonography is useful when it is difficult to diagnose the radiological extent of the damage in the growth plate.
The sonographic appearance is characterized by an irregular profile, with a modification of the normal echogenicity and a possible hematoma.
MRI examination (and in some cases CT) may be indicated in more complex cases, with the advantage of being able to explore deep parts poorly evaluated by ultrasound.
MRI is a very helpful technique because it can further characterize the injury by showing the bone edema on T2-weighted and STIR images and the focal extension into the unmineralized cartilage [49].
In the bone pelvis, avulsion can occur in different sites [50].
The anterior superior iliac spine is the proximal insertion site of the sartorius and the tensor fascia lata muscle (Fig. 6.4).
Sartorius lesion is common in runners, where athletic effort consists of a forced extension of the hip during knee flexion.
The diagnosis is clinical, but x-ray examination, essential to assess the avulsion extent, can be integrated with a comparative ultrasound examination and with MRI (Fig. 6.5).
The growth plate of the anterior inferior iliac spine appears between 9 and 13 years, welding around 17 years (Fig. 6.6).
At this level, the direct tendon of the anterior rectus muscle of the thigh inserts and its action consists of extending the leg on the thigh and flexing the thigh on the pelvis. The lesion may occur in some sports such as football or rugby, due to a strong contraction against a resistance.
Also in this case, the clinical diagnosis can be integrated with a multidisciplinary study [51–53].
On the other hand, avulsion fractures at the level of the pubic symphysis, where we find the insertion of the adductor muscles, gracilis, and abdominal recti, are rare because they are more often caused by repetitive microtrauma and supported by some anatomical conditions such as asymmetry of the lower limbs [54] (Fig. 6.7).
Ultrasound allows to detect the presence of morphological alterations at the site of tendon insertion.
In these cases, MRI is necessary to study the functional myotendinous unit and bone and cartilaginous components and in particular to search for the “stress response” typically associated with these conditions.
The most common anatomical location of pelvis avulsion fractures is the growth plate of the ischial tuberosity (Fig. 6.8), site of insertion of semimembranosus tendons and hamstrings (composed by semitendinosus and long head of the biceps femoris), characterized by its typical lunate morphology [55] (Fig. 6.9).
The treatment of these injuries is generally conservative, but we have to remember that in some significant (>2 cm) dislocations, the outcome may be disabling.
MRI is a very useful to assess the degree of soft tissue involvement, to define whether the injury is complete or incomplete, and to assess the relationship with the sciatic nerve.
Avulsions at the iliopsoas insertion on the lesser tuberosity of the femur (Fig. 6.10) or of gluteus or tensor fascia lata muscles at the level of the greater trochanter (Fig. 6.11) are very rare [56].
Legg-Calvè-Perthes disease is a form of idiopathic osteochondrosis of the femoral head physis, rarely connected to overuse injuries, difficult to diagnose both clinically and radiographically.
It occurs early during childhood, generally between 2 and 14 years of age, with a peak around 5–6 years of age, and it is a common cause of pain in children.
It is usually unilateral, although in 15 % of cases it is bilateral, and it usually affects children between 5 and 8 years old, without a significative history of mechanical abuse.
It is a diagnosis of exclusion, and other causes of avascular necrosis (such as sickle cell disease, leukemia, corticosteroid administration, and Gaucher’s disease) as well as epiphyseal dysplasia must be ruled out.
X-ray plays an important role in its diagnosis.
US may be useful just to assess the presence of intra-articular fluid collection [57] (Fig. 6.12).
MRI may give some essential information to recognize the disease early and to start the therapy as soon as possible; in fact, it has been demonstrated that those children diagnosed at a younger age typically experience a more benign disease course, while those diagnosed at an older age typically require increased rates of intervention and generally experience poorer outcomes.
In addition, MRI can accurately stage the disease, evaluate some associated complications, and, above all, differentiate LCP disease from other epiphyseal lesions [58].
Slipped capital femoral epiphysis can result from a chronic overload of compressive and tangential strains acting on the physeal plate, leading to an incomplete or complete lesion, such as type I Salter-Harris lesion. When a complete lesion of the physis occurs, the epiphysis displaces posteriorly and slips.
It can be a real overuse injury when the physis is normal or a relative overuse injury when a normal overload might be excessive for the physeal plate weakened by adverse hormonal conditions (such as hypogonadism).
The diagnosis is easily made by radiography, although MRI can show the “preslippage” in controversial cases. It can also highlight edematous changes in the epiphysis and the adjacent metaphysis, and it can also recognize its complications, such as AVN or chondrolysis [59] (Fig. 6.13).
6.3.2 Knee
The knee joint is anatomically made up of the tibiofemoral and the patellofemoral joint.
Capsular-ligament lesions can vary depending on the biomechanics of the trauma, and they occur more frequently in adolescents during sports activity.
It is essential for the radiologist to recognize and interpret the type of lesion also through knowledge of the biomechanical mechanism.
A proper diagnosis is essential to direct the clinician toward the most suitable treatment.
The Osgood-Schlatter syndrome, known for more than a century (1903), is the most known osteochondritis, which occurs in some athletes who practice running and jumping, conditions that cause repeated microtrauma to the tibial tubercle, where the patellar tendon inserts.
This condition, more common in males, is usually bilateral, often asymptomatic.
The tibial tubercle is an anterior extension of the tibial physis and is prone to injury because of its unique composition, which varies from the other physes.
Since the very beginning, it was described as a pathology affecting firstly the tibial tubercle, but recently, several studies have been demonstrated that the main cause is the action of repetitive microtrauma at the level of tibial insertion of the patellar tendon.
Repetitive stress on the tubercle causes inflammation at the patellar tendon insertion site, reactive bone formation, bone marrow edema, thickening of the proximal portion of patellar tendon, and soft tissue swelling [60, 61].
In addition to the classic findings of bone fragmentation, easily detectable on plain radiographs, ultrasound allows to appreciate the irregularity and fragmentation of the growth plate profile, thickening and abnormal echogenicity of the tendon, and edema of the soft tissue anterior to the tuberosity (Fig. 6.14).
MRI is useful in detecting these signs, especially in the early stage of the disease when only bone marrow edema near the tubercle is visible [62].
This syndrome may predispose to the avulsion fractures of the tibial tubercle, in most cases due to a strong knee hyperextension and classified in three types by Watson-Jones, depending on the physis involvement and on the degree of bone fragment dislocation [63].
Sinding-Larsen-Johansson syndrome is a bone avulsion at the proximal patellar insertion.
Ultrasound examination, performed at the patellar inferior pole, highlights the lack of fusion of growth plate of the lower pole of the patella and thickening of the patellar tendon, which appears hypoechoic peripherally, with some rare calcifications.
MRI can determine the extent of the disease, such as fragmentation of the inferior patellar pole, infiltration of Hoffa fat pad, and thickening of the proximal patellar tendon. It is also possible to detect calcification or ossification of the tendon [61, 62].
Isolated rupture of the patellar tendon, generally uncommon in young patients, is usually caused by direct trauma.
Ultrasound examination allows an accurate assessment of the lesion, with a retracted and hypoechoic appearance of the tendon in the context of a hematoma which can be quantifiable in dimension.
Lateral radiographs can reveal patella alta deformity and one or multiple tiny osseous fragments adjacent to the inferior pole of the patella; in these cases, MRI is indicated for its panoramic views in order to define the exact extent of damage for a possible surgical treatment [64] (Fig. 6.15).
Patellar sleeve avulsion is a cartilaginous injury to the lower pole of the patella.
Conventional radiography is useful in order to define patellar position with respect to the femur and to detect a small bone fragment.
Ultrasonography is useful to search for the cartilage fragment avulsed together with the tendon, but even in these cases, MRI is indicated because it can accurately define the extent of the cartilage damage.
Jumper’s knee is a pain syndrome involving the proximal or distal insertion of the patellar tendon, resulting from chronic stress and inflammation, commonly seen in young athletes.
At US examination, the patellar tendon appears hypoechoic in its deep portion with focal loss of the normal fibrillar structure, without signs of hyperemia on power Doppler examination [61].
Other less common conditions are the avulsion of the quadriceps tendon, iliotibial tract, arcuate complex, semimembranosus, or biceps of the femur.
Ultrasound examination is a key contributor in the study of the extensor mechanism, even for anatomical location, and MRI can provide valuable additional information for adequately defining the extent of damage.
Patellofemoral dislocations are acute conditions of loss of normal articular links with sudden lateralization of the sesamoid and distractive injury of the retinacula with a characteristic pattern of injury contusion at the level of the medial articular aspect of the patella and the external condyle of the femur.
These findings are well documented with MRI, which is the test of choice for its diagnosis and also for the evaluation of any dysplastic predisposing conditions and to assess the severity of the ligament damage at the level of the retinacula [63] (Fig. 6.16).
A 15-year-old female patient affected by patella luxation spontaneously reduced. (a) T2-weighted image on axial plane shows lipohemarthrosis with three layers visible (from above: fat, fluid, and red blood cells). (b, c) STIR sequences obtained on the sagittal and axial plane show bone marrow edema on the lateral aspect of the external femoral condyle and on the patella medial aspect, as a consequence of sesamoid luxation
Acute meniscus lesions are more common in adolescents and in those patients with congenital anomaly predisposing morphological variants such as the discoid meniscus.
MRI is definitely crucial to search for meniscus tears (Fig. 6.17).
(a) A bucket-handle lesion. In the axial plane. (b) STIR image on sagittal plane shows the “double posterior cruciate ligament” sign, indicating a bucket-handle lesion. (c) Axial plane: lateral meniscus lesion. (d) Sagittal plane demonstrates a transverse-oblique lesion of the anterior horn of meniscus
The medial and lateral collateral ligaments are peripheral structures which merge deeply together with the joint capsule and the corresponding corner points, with stabilizing functions complementary to those of the central pivot.
Collateral ligament injuries are well evaluated with ultrasonography, which is a useful tool in determining the degree of injury and the subsequent monitoring.
In partial injury, the ligament appears thickened, hypoechoic and inhomogeneous, but continuous, with rare signs of hyperemia on power Doppler.
In complete injuries, however, the ligament is strongly thickened and hypoechoic, sometimes hardly recognizable and surrounded by fluid collection.
MRI allows to accurately define the degree of injury and the presence of bone bruise and to look for other associated injuries [65] (Fig. 6.18).
Clip pattern lesion is a contact injury that occurs after a pure valgus stress is applied to the knee while the knee is in a state of mild flexion.
It is common among American football players. In this type of lesions, bone marrow edema is usually most prominent in the lateral femoral condyle secondary to direct blow, whereas a second smaller area of edema may be present in the medial femoral condyle secondary to avulsive stress to the MCL.
The main constituents of the central pivot are the cruciate ligaments, intra-articular structures surrounded by the synovial membrane, which are essential to the stability and to the correct functioning of the joint. They are distinct anteriorly and posteriorly according to their anatomical arrangement and insertion on the tibial plate. The lesions are rare in preadolescents and more frequent in sportive adolescents.
The most frequent injuries are those involving the anterior cruciate, easily detected by MRI through assessment of direct and indirect signs.
These lesions are classified according to the site and degree: focal, partial, and complete.
It is also possible to distinguish the phase of injury as acute, subacute, or chronic.
Among the direct signs to look for, the so-called bone contusions (bone bruises) should be taken into consideration.
These findings were considered infrequent in children, but the increasing number of injuries and the number of MRI examinations in young adolescent have modified these concepts.
The distribution and morphology of the contusion areas is a real track of the natural biomechanics of the trauma that helps us to identify the various capsular ligamentous injuries associated with it.
At MRI examination, the contusion lesions appear as areas of low signal intensity on T1-weighted sequences and strongly hyperintense on T2-weighted and STIR sequences.
Pivot shift injury is a noncontact injury commonly seen in skiers or American football players. It occurs when a valgus load is applied to the knee in various states of flexion combined with external rotation of the tibia or internal rotation of the femur. The resulting bone contusion pattern involves the posterior aspect of the lateral tibial plateau and the midportion of the lateral femoral condyle near the condyle-patellar sulcus [66, 67].
Hyperextension of the knee can result when direct force is applied to the anterior tibia while the foot is planted or from an indirect force, such as a forceful kicking motion.
It is characterized by edema of the anterior aspect of the condyle and the tibial plate.
Segond avulsion fracture, originally described by the French surgeon Paul Segond in 1879 after a series of cadaveric experiments, involves cortical avulsion of the tibial insertion of the middle third of the lateral capsular ligament.
The mechanism of this injury is often the result of internal rotation of the knee and varus stress, producing abnormal tension on the central portion of the lateral capsular ligament [68, 69].
The lesion consists of an elliptic fragment of bone parallel to the tibia, just distal to the lateral tibial plateau, well detectable on plain radiograph.
Radiographic appearance of Segond fracture is a strong indication for an MRI examination.
MR imaging should be performed in all cases of Segond fracture due to the extensively documented association of this injury with the disruption of the anterior cruciate ligament and meniscal tear.
The Meyers and McKeever classification system describes four degrees of of tibial eminence fractures, and gravity. Tibial eminence fractures are most commonly seen in children and adolescents aged 8 to 14 years depends on the degree of bone fragment dislocation. It usually occurs in children aged between 8 and 14 years.
The first degree is treated conservatively.
The “kissing” bone contusion is a common finding.
The diagnosis must be accurate since the choice of treatment is affected by the degree of injury, the presence of any associated meniscal tears, and especially the degree of skeletal maturity.
Posterior cruciate ligament injury is uncommon in adolescents, and it is typically caused by a direct trauma on the anterior aspect of the tibia when the knee is in a flexed position, as occurs in the dashboard injury when the knee strikes against the dashboard during an automobile accident, with a posterior dislocation of the tibia with respect to the femur.
MRI examination will show edema at the anterior aspect of the tibia and, occasionally, at the posterior surface of the patella.
Reverse Segond lesion, recently described, consists of the presence of a bone fragment arising from the medial aspect of the proximal tibia, and it is associated with both midsubstance tears of the posterior cruciate ligament and avulsions of the PCL from the posterior tibial plateau, as well as tears of the medial meniscus.
Osteochondrosis is generally due to a repeated compressive trauma which causes an abnormal blood supply in the stressed area, leading to bone necrosis.
This alteration generally affects the physeal growth plates, and in younger patients, where the growth plate is in training, the normal process of ossification is compromised until a final deformation.
In young patients, the vascular changes may result in a circumscribed area of osteonecrosis with possible subsequent detachment of a necrotic fragment.
It is important to recognize this condition promptly to establish the most appropriate therapy for the reduction of the overload.
X-ray examination accurately depicts this alteration, especially in an advanced stage. Nevertheless, MRI is the technique of choice which allows to highlight, since the beginning, the deformation of the cortex profile and the evidence of the osteochondral fragment (Fig. 6.19).
MRI on sagittal plane before and after conservative treatment. (a) A diffuse cartilage thickening with a lunate subchondral suffering area on the lateral aspect of the femoral condyle, without cartilage lesion, is evident. (b) MRI examination performed after 5 years shows a complete restoration of bone integrity
Koenig disease is an osteochondral defect of the knee accounting for 80–85 % of all osteochondral lesions. It commonly affects male patients (especially those with florid physis) on the medial femoral condylar epiphysis, as a consequence of repeated microtrauma during athletic activities (Fig. 6.20).
An 8-year-old male patient affected by Koenig disease. (a) STIR sequence on the coronal plane shows a subchondral area of marrow edema involving both the articular cartilage and the lateral aspect of the internal femoral condyle, typical signs of osteochondritis. (b–d) Coronal, sagittal, and VRT CT reconstructions demonstrate irregularity and fragmentation of the articular cartilage of the internal femoral condyle
6.3.3 Ankle
Among the most frequent ligament injuries affecting children and adolescents, lesions of ankle inversion trauma with involvement of the external collateral ligament, such as the peroneal-talar component, should be cited. X-ray, allowing to highlight the presence of a fracture or bone detachment, can be integrated with ultrasound examination that can show the degree of ligament injury, capsular distension, and the presence of effusion.
MRI provides more information about the evaluation of cartilage components, and it is indicated in high-degree lesions associated with instability [70, 71] (Fig. 6.21).
Osteochondritis dissecans of the talus is a very common disease in running and jumping sports, because of repeated compressive microtrauma. The most common site of lesion is the posterior and internal aspect of the talus. In this case, MRI is a very useful tool in detecting the classical signs of this pathology [71] (Fig. 6.22).
Sever disease is an alteration of the physis plate of the heel, typical of growth age. The most accepted cause is the overloaded performed by the Achilles tendon on heel apophysis. The imaging features are quite similar to those described before, although the radiographic pattern might be confused with a normal densification of apophyseal plate; so, in such difficult cases, MRI can be a reliable tool to make the correct diagnosis [72].
It must be stressed that ultrasound examination is very helpful in the differential diagnosis with acute Achilles tendonitis, for the evaluation of peroneal tendons and their anatomical position, and also to evaluate the posterior tibial tendon and the common flexor and extensor compartment.
Iselin disease is an osteochondrosis of the fifth metatarsal base, caused by a traction mechanism of the peroneal tendons.
Freiberg disease affects the physeal plate of the second metatarsal head and, rarely, the third, and it commonly occurs in runner athletes. MRI can be useful in the evaluation of spongeous bone which appears hyperintense on T2-weighted images, indicating bone marrow edema [73] (Fig. 6.23).
6.4 Acute Stress Injuries in Children
Stress fractures are acute injuries caused by repetitive microtrauma during sports activity. These conditions are common in practicing athletics.
Typical locations of stress fractures are the tibia, fibula, femur, tarsal, and metatarsal bones.
They clinically present with swelling and pain related to physical activity, without a history of acute injury.
They are not easily detected with conventional radiography, especially in the acute setting when the examination is driven by painful symptoms, and cortical thickening and spongeous reaction are not visible.
In acute phase, MRI is the best diagnostic modality, owing to its high sensitivity in detecting marrow edema, which results in low signal intensity on T1-weighted images and high signal intensity on STIR and T2-weighted images. The fracture line, on the other hand, is well depicted as a low signal intensity on both T1- and T2-weighted sequences (Fig. 6.24).
Subperiosteal fluid is a helpful ancillary finding in a subtle fracture.
Immature skeleton is particularly prone to stress injuries; this is due to some factors, such as increased physical activities, narrower bones with thinner cortices, hormonal changes, and less muscle mass.
Stress injuries can occur in a healthy bone which undergo a functional overuse cyclically repeated, which causes microscopic injuries that, when frequently applied, do not allow a complete structural restoration, leading to anatomical alterations and particular clinical features.
In fact, when a bone is subject to stress, initially it responds with an accelerated cortical resorption and remodeling of the haversian system, inducing a cortex weakening; a prolonged stress results in osteoclastic resorption outpacing osteoblastic repair, causing even further weakening and fracture if the stressor is not reduced.
These lesions, less common in adult patients, are the leading cause of sports injuries in young athletes, maybe because during growth, sudden changes in body size could complicate the coordination of athletic movements, thus modifying the strain type and, therefore, increasing the chance of stress injuries.
In the physis, long-standing overuse affects the endochondral ossification, resulting in abnormal physeal widening and, occasionally, bone bridging [74].
Toddler’s stress fractures of the lower extremities are associated with the onset of ambulation. They typically occur between 9 months and 3 years of age, and they manifest with a refusal to bear weight and are not preceded by a recognized acute traumatic event.
The typical toddler’s fracture is a non-displaced oblique fracture of the distal portion of the tibia. Other locations are the fibula, the posterior aspect of the calcaneus, the talus, and the base of the cuboid.
Stress fractures of the pelvic bones are difficult to detect radiographically owing to its anatomical complexity and bowel gas interposition.
The most common bones involved are the pubis and the sacrum; they usually affect young runners and sometimes volleyball players and gymnasts.
Stress fractures of the upper extremities are less common, where the ulna and radius are the most frequently involved bones, especially in tennis players, and the olecranon apophysis in gymnasts. Stress fractures of the carpal bones are uncommon in young patients, and they often are underdiagnosed. The capitate is the most frequently affected bone, followed by lunate and scaphoid.
The lumbar spine and sacral spine are common sites of stress fractures observed during the teenage growth spurt, and they involve the pars interarticularis, causing spondylolysis, with or without spondylolisthesis.
It usually occurs before 16 years as a gradual vertebral slip, but the patient is typically asymptomatic.
This condition has been encountered in as many as 47 % of adolescent athletes with low back pain, with respect to only 5 % of adult athletes with the same symptom.
Stress injuries of the pars interarticularis range from changes in signal intensity, such as stress response, to bony defects. The prognosis is worse when there is nonunion.
6.5 Muscle Lesions
Muscle derangements in athletes have a wide variety of causes, treatments, and prognoses.
They represent 10–30 % of all sports injuries in young adolescents, and they require an accurate diagnosis because the therapeutic treatment is based on a correct clinical reading of the lesions.
They usually occur at the onset of athletic activity, involving more frequently the lower limb muscles crossing two joints, such as the rectus femoris, hamstrings, and gastrocnemius muscles. They commonly affect the myotendinous junction but sometimes also the muscular belly.
There are some predisposing factors such as fatigue, outside temperature, electrolyte imbalances, poor training, recovery after long injury, “recovery of athletic preparation,” and one of the considerable impacts, the “imbalance” between agonistic and antagonistic muscle groups.
Their incidence gradually increases in the last phase of adolescence, owing to a gradual strengthening of tendinous junctions, shifting the site of minor resistance toward the muscle.
The clinical impact of diagnostic imaging is very significant owing to the fact that its classification, necessary to assess the degree of injury, to direct the treatment, and to define the recovery time, is based on clinical and radiological criteria.
Given that the cause and severity of athletic injuries may be difficult to determine clinically, US and MR imaging are utilized increasingly to evaluate muscle injuries, especially in young athletes.
Ultrasonography is the first-choice technique in the acute setting, since it has a high cost-benefit ratio, is easily repeatable and therefore useful in the monitoring of the lesions, and is well tolerated by the patient.
It is also possible to evaluate the dynamics of muscle in comparison with the contralateral side.
MRI is highly sensitive in the diagnosis of low-grade lesions owing to its high contrast resolution, its multiplanarity, and its ability to explore the deep layers [75].
In some traumatic conditions, when clinical findings are subtle or absent, MR imaging becomes essential to reach the correct diagnosis (Fig. 6.25).
Muscle lesions can be divided, depending on the cause of the trauma, into direct (such as contusions) and indirect injuries.
Muscle contusions are the most common type of muscle injuries occurring during the pediatric age, particularly in the first adolescence, and they usually involve lower limb muscles (quadriceps and tibialis anterior) exhibiting pain, swelling, ecchymosis, spasm, and functional limitation.
MR imaging is quite similar to that of indirect injuries, although the site usually is deep, adjacent to the bone surface, owing to the different traumatic cause.
Muscle girth is usually increased, without fiber discontinuity or laxity.
On T2-weighted sequences, a large area of high signal intensity, with a diffuse or geographic appearance, may be displayed, often with feathery margins. In such hard cases, the edema is associated to a muscular hematoma.
Indirect injuries are muscle strains due to the application of longitudinal forces overcoming the elastic strength of muscular fibers.
They are classified using a three-grade continuous spectrum of injury, from mild (first degree) to severe (third degree), and low-grade injuries are more common than high-grade ones.
A mild lesion is characterized by microscopic injury to the muscle or tendon.
The treatment is conservative, consisting in rest from aggravating activities.
A moderate lesion (partial-thickness tear) consists of a tissue damage involving 2/3 of the muscle belly, and it exhibits a sudden, acute and localized pain associated with function limitation.
A severe lesion (complete disruption), typically at the site of junction, involves the whole muscular section, with or without retraction; it exhibits with strong pain and a complete loss of muscular function. Sometimes, it requires surgical intervention.
Grading the tears by US:
-
Mild lesion (first degree – elongation): US can be negative or can show the presence of a small hypoechoic area within the muscular fibers. Healing is quick, usually in 15 days.
-
Moderate lesion (second degree): in the acute setting (<24 h), we can find the presence of a hyperechoic hematoma which often underestimates the underlying muscle injury. It appears as a discontinuity of the muscular fibrolipidic septa, with some hypo-anechoic areas with irregular edges.
-
Severe lesion (third degree): complete breakdown of muscle fibers resulting in mass effect associated with distal muscle fiber retraction and adjacent effusion.
Grading the tears by MRI [76]:
-
Grade I tear: focal high signal intensity on T2-weighted and STIR sequences with muscle edema and hemorrhage at the myotendinous junction; edema and hemorrhage may track along muscle fascicles, creating a feathery margin to the lesion. We can also find a rim of hyperintense perifascial fluid around a muscle belly or a group of muscles.
-
Grade II tear: this is a partial-thickness strain of the myotendinous junction with interstitial feathery high signal intensity on T2-weighted sequences or hematoma in the acute setting. Perifascial fluid also is common in this situation. Low signal can represent either fibrosis or hemosiderin and can be seen in chronic or old injuries.
-
Grade III tear: it represents a complete myotendinous disruption, and if muscle retraction is associated, it can be seen as an enlargement of the retracted belly with a focal fluid collection filling the gap. It is also associated with a significant hematoma formation.
Some complications of muscle injuries include myositis ossificans and rarely compartment syndrome or pyomyositis.
At US examination, the posttraumatic scarring alterations may appear as hyperechoic linear streaks after an indirect distractive trauma or as nodular areas with streaks of increased echogenicity after a blunt trauma.
Muscle laceration is caused by a penetrating injury and is uncommon in athletic patients. MR imaging is not usually performed in the acute setting, although it may show a focal and sharp discontinuity of fibers and a high signal intensity on T2-weighted sequences, caused by hemorrhage and edema.
Muscle herniation refers to the protrusion of muscle belly through a focal fascia defect (such as those traversed by vessels and nerves) caused, in traumatic setting, by a tear, a penetrating lesion, or fractures; more commonly, it usually occurs because of muscle hypertrophy and increased intracompartmental pressure.
The most involved sites are the middle to the lower portions of the leg, with the tibialis anterior most commonly involved.
MR imaging shows an outward muscle bulging with a discontinuity in the overlying fascia.
References
Kumar R, Lindell MM, Madewell JE et al (1989) The clavicle: normal and abnormal. Radiographics 9(4):677–706
Curtis RJJ (1994) Skeletal injuries: shoulder injuries. In: Stanitski CL, DeLee JC, Drez D (eds) Pediatric and adolescent sports medicine. W.B. Saunders, Philadelphia, pp 175–215
Cleeman E, Flatow EL (2000) Shoulder dislocations in the young patient. Orthop Clin North Am 31(2):217–229
Rowe CR (1956) Prognosis in dislocations of the shoulder. J Bone Joint Surg Am 38-A(5):957–977
Emery KH (2006) Imaging of sports injuries of the upper extremity in children. Clin Sports Med 25:513–568
Deitch J, Menhlman CT, Food SL et al (2003) Traumatic anterior shoulder dislocation in adolescents. Am J Sports Med 31(5):758–763
Marans HJ, Angel KR, Schemitsch EH et al (1992) The fate of traumatic anterior dislocation of the shoulder in children. J Bone Joint Surg Am 74(8):1242–1244
Magee T, Williams D, Mani N (2004) Shoulder MR arthrography: which patient group benefits most? AJR Am J Roentgenol 183(4):969–974
Meister K, Thesing J, Montgomery WJ et al (2004) MR arthrography of partial thickness tears of the undersurface of the rotator cuff: an arthroscopic correlation. Skeletal Radiol 33(3):136–141
Lee SY, Lee JK (2002) Horizontal component of partial thickness tears of rotator cuff: imaging characteristics and comparison of ABER view with oblique coronal view at MR arthrography initial results. Radiology 224(2):470–476
Bui Mansfield LT, Banks KP, Taylor DC (2007) Humeral avulsion of the glenohumeral ligaments: the HAGL lesion. Am J Sports Med 35:1960–1966
Dahlin LB, Erichs K, Andersson C et al (2007) Incidence of early posterior shoulder dislocation in brachial plexus birth palsy. J Brachial Plex Peripher Nerve Inj 2:24
Tung GA, Hou DD (2003) MR arthrography of the posterior labrocapsular complex: relationship with glenohumeral joint alignment and clinical posterior instability. AJR Am J Roentgenol 180:369–375
Bradley JP, Baker CL 3rd, Kline AJ et al (2006) Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulder. Am J Sports Med 34:1061–1071
May MM, Bishop K (2013) Shoulder injuries in young athletes. Pediatr Radiol 43:135–140
Heyworth BE, Williams RJ 3rd (2009) Internal impingement of the shoulder. Am J Sports Med 37:1024–1037
Kanati U, Ozturk BY, Bolukbasi S (2010) Anatomical variations of the anterosuperior labrum: prevalence and association with type II superior labrum anterior-posterior (SLAP) lesions. J Shoulder Elbow Surg 19:1199–1203
Piatt BE, Hawkins RJ, Fritz RC et al (2002) Clinical evaluation and treatment of spinoglenoid notch ganglion cysts. J Shoulder Elbow Surg 11:600–604
Chen FS, Diaz VA, Loebenberg M et al (2005) Shoulder and elbow injuries in the skeletally immature athlete. J Am Acad Orthop Surg 13(3):172–185
Carson WG Jr, Grasser SI (1998) Little Leaguer’s shoulder. A report of 23 cases. Am J Sports Med 26(4):575–580
Song JC, Lazarus ML, Song AP (2006) MRI findings in Little Leaguer’s shoulder. Skeletal Radiol 35(2):107–109
Wasserlauf BL, Paletta GA Jr (2003) Shoulder disorders in the skeletally immature throwing athlete. Orthop Clin North Am 34(3):427–437
Paley KJ, Jobe FW, Pink MM et al (2000) Arthroscopic findings in the overhead throwing athlete: evidence for posterior internal impingement of the rotator cuff. Arthroscopy 16(1):35–40
Sanders TG, Miller MD (2005) A systematic approach to magnetic resonance imaging interpretation of sports medicine injuries of the shoulder. Am J Sports Med 33(7):1088–1105
Vinson EN, Helms CA, Higgins LD (2007) Rim-rent tear of the rotator cuff: a common and easily overlooked partial tear. AJR Am J Roentgenol 189(4):943–946
Giaroli EL, Major NM, Higgins LD (2005) MRI of internal impingement of the shoulder. AJR Am J Roentgenol 185(4):925–929
Beltran J, Rosenberg ZS (1997) MR imaging of pediatric elbow fractures. Magn Reson Imaging Clin N Am 5(3):567–578
Carey J, Spence L, Blickman H et al (1998) MRI of pediatric growth plate injury: correlation with plain film radiographs and clinical outcome. Skeletal Radiol 27(5):250–255
Major NM, Crawford ST (2002) Elbow effusion in trauma in adults and children: is there an occult fracture? AJR Am J Roentgenol 178:413–418
White PG, Mah JY, Friedman L (1994) Magnetic resonance imaging in acute physeal injuries. Skeletal Radiol 23:527
Lyman S, Fleisig GS, Andrews JR, Osinski ED (2002) Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med 30(4):463–468
Kijowsku R, Tuite MJ (2010) Pediatric throwing injuries of the elbow. Semin Musculoskelet Radiol 14(4):419–429
Greiwe RM, Saifi C, Ahmad CS (2010) Pediatric sports elbow injuries. Clin Sports Med 29(4):677–703
Rudzki JR, Paletta GA Jr (2004) Juvenile and adolescent elbow injuries in sports. Clin Sports Med 23(4):581–608
Timmermann LA, Andrews JR (1994) Undersurface tear of the ulnar collateral ligament in baseball players. A newly recognized lesion. Am J Sports Med 22(1):33–36
Sugimoto H, Ohsawa T (1994) Ulnar collateral ligament in the growing elbow: MR imaging of normal development and throwing injuries. Radiology 192(2):417–422
Hayter CL, Adler RS (2012) Injuries of the elbow and the current treatment of tendon disease. AJR Am J Roentgenol 199:546–557
Iyer RS, Thapa MM, Khanna PC et al (2012) Pediatric bone imaging: imaging elbow trauma in children – a review of acute and chronic injuries. AJR Am J Roentgenol 198:1053–1068
Benjamin HJ, Briner WW Jr (2005) Little league elbow. Clin J Sport Med 15(1):37–40
KijowskuR DSAA (2005) Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol 34(5):266–271
Kramer J, Stiglbauer R, Engel A, Prayer L, Imhof H (1992) MR contrast arthrography (MRA) in ostechondrosis dissecans. J Comput Assist Tomogr 16(2):254–260
Zetaruk MN (2000) The young gymnast. Clin Sports Med 19(4):757–780
Kocher MS, Waters PM, Micheli LJ (2000) Upper extremity injuries in the paediatric athlete. Sports Med 30(2):117–135
Zlatkin MB, Rosner J (2004) MR imaging of ligaments and triangular fibrocartilage complex of the wrist. Magn Reson Imaging Clin N Am 12:301–331
Schweitzer ME, Natale P, Winalski CS, Culp R (2000) Indirect wrist MR arthrography: the effects of passive motion versus active exercise. Skeletal Radiol 29:10–14
Kaawach W, Ecklund K, Di Canzio J, Zurakowski D, Waters PM (2001) Normal ranges of scapholunate distance in children 6 to 14 years old. J Pediatr Orthop 21(4):464–467
Eustace S, Denison W (1997) Pictorial review: magnetic resonance imaging of acute orthopaedic trauma to the upper extremity. Clin Radiol 52:338–344
Gaca AM (2009) Basketball injuries in children. Pediatr Radiol 39(12):1275–1285
Pan J, Bredella MA (2013) Imaging of soft tissue abnormalities about the hip. Radiol Clin North Am 51:353–369
Stevens MA, El- Khoury GY, Kathol MH et al (1999) Imaging features of avulsion Injuries. Radiographics 19:655–672
Bancroft LW, Blankenbaker DG (2010) Imaging of the tendons about the pelvis. AJR Am J Roentgenol 195:605–617
Gyftopoulos S, Rosenberg ZS, Schweitzer ME et al (2008) Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. AJR Am J Roentgenol 190:182–186
Galloway HR (2013) Overuse injuries of the lower extremity. Radiol Clin North Am 51:511–528
Omar IM, Zoga AC, Kavanagh EC et al (2008) Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics 28:1415–1438
Koulouris G, Connell D (2003) Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol 32:582–589
Patel K, Wallace R, Busconi BD (2011) Radiology. Clin Sports Med 30:239–283
Stuecker MH, Habermann C, Bubenheim M et al (2008) Sonography for evaluation of containment in perthes disease: a comparison with magnetic resonance imaging. Ultraschall Med 29(Suppl 5):245–249
Stücker MH, Buthmann J, Meiss AL (2005) Evaluation of hip containment in legg-calvé-perthes disease: a comparison of ultrasound and magnetic resonance imaging. Ultraschall Med 26(5):406–410
Harland U, Krappel FA (2002) Value of ultrasound, CT, and MRI in the diagnosis of slipped capital femoral epiphysis (SCFE). Orthopade 31(9):851–856, German
Draghi F, Danesino GM, Coscia D et al (2008) Overload syndromes of the knee in adolescents: sonographic findings. J Ultrasound 11(4):151–157
Carr JC, Hanly S, Griffin J et al (2001) Sonography of the patellar tendon and adjacent structures in pediatric and adult patients. AJR Am J Roentgenol 176:1535–1539
Dupuis CS, Westra SJ, Makris J et al (2009) Injuries and conditions of the extensor mechanism of the pediatric knee. Radiographics 29:877–886
Gottsegen CJ, Eyer BA, White EA et al (2008) Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics 28(6):1755–1770
Ostlere S (2013) The extensor mechanism of the knee. Radiol Clin North Am 51:393–411
Lopomo N, Zaffagnini S, Amis AA (2013) Quantifying the pivot shift test: a systematic review. Knee Surg Sports Traumatol Arthrosc 21(4):767–783
Ahldén M, Samuelsson K, Fu FH et al (2013) Rotatory knee laxity. Clin Sports Med 32:37–46
Dodds AL, Halewood C, Gupte CM et al (2014) The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J 96-B(3):325–331
Geiger D, Chang E, Pathria M et al (2013) Posterolateral and posteromedial corner injuries of the knee. Radiol Clin North Am 51:413–432
Vanhoenacker FM, Snoeckx A (2007) Bone marrow edema in sports: general concepts. Eur J Radiol 62:6–15
Hunt KJ, Githens M, Riley GM et al (2013) Foot and ankle injuries in sport imaging correlation with arthroscopic and surgical findings. Clin Sports Med 32:525–557
Nazarenko A, Beltran LS, Bencardino JT (2013) Imaging evaluation of traumatic ligamentous injuries of the ankle and foot. Radiol Clin North Am 51:455–478
Bailey CW, Cannon ML (2014) Sever disease (calcaneal apophysitis). J Am Osteopath Assoc 114(5):411
Talusan PG, Diaz-Collado PJ, Reach JS Jr (2014) Freiberg’s infraction: diagnosis and treatment. Foot Ankle Spec 7(1):52–56
Berger FH, de Jonge MC, Maas M (2007) Stress fractures in the lower extremity. The importance of increasing awareness amongst radiologists. Eur J Radiol 62:16–26
May DA, Disler DG, Jones EA et al (2000) Abnormal signal intensity in skeletal muscle at MR imaging: patterns, pearls, and pitfalls. Radiographics 20:S295–S315
Elsayes KM, Lammle M, Shariff A et al (2006) Value of magnetic resonance imaging in muscle trauma. Curr Probl Diagn Radiol 35:206–212
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Galluzzo, M., Piccolo, C., Buquicchio, G.L., Palliola, R., Trinci, M. (2015). Ultrasound and Magnetic Resonance Imaging of Pediatric Musculoskeletal Injuries. In: Miele, V., Trinci, M. (eds) Imaging Trauma and Polytrauma in Pediatric Patients. Springer, Cham. https://doi.org/10.1007/978-3-319-08524-1_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-08524-1_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-08523-4
Online ISBN: 978-3-319-08524-1
eBook Packages: MedicineMedicine (R0)