Abstract
Major depressive disorder (MDD) is common. Despite numerous available treatments, many individuals fail to improve clinically. MDD continues to be diagnosed exclusively via behavioral rather than biological methods. Biomarkers—which include measurements of genes, proteins, and patterns of brain activity—may provide an important objective tool for the diagnosis of MDD or in the rational selection of treatments. Proteomic analysis and validation of its results as biomarkers is less explored than other areas of biomarker research in MDD. Mass spectrometry (MS) is a comprehensive, unbiased means of proteomic analysis, which can be complemented by directed protein measurements, such as Western Blotting. Prior studies have focused on MS analysis of several human biomaterials in MDD, including human post-mortem brain, cerebrospinal fluid (CSF), blood components, and urine. Further studies utilizing MS and proteomic analysis in MDD may help solidify and establish biomarkers for use in diagnosis, identification of new treatment targets, and understanding of the disorder. The ultimate goal is the validation of a biomarker or a biomarker signature that facilitates a convenient and inexpensive predictive test for depression treatment response and helps clinicians in the rational selection of next-step treatments.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autism Spectrum Disorder
- Major Depressive Disorder
- Diffusion Tensor Imaging
- Major Depressive Disorder
- Salivary Cortisol
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
27.1 Introduction
Major depressive disorder (MDD) occurs frequently, affecting 7.1 % people each year and 14.4 % of people over the course of a lifetime [1]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the diagnosis of MDD requires at least five symptoms, present for at least 2 weeks; among the five symptoms at least one should be depressed mood and/or loss of interest or pleasure [2]. Other symptoms include change in sleep, appetite, fatigue/energy loss, feelings of worthlessness or guilt, diminished concentration, and suicidal thoughts [2, 3]. In addition to suffering from impairment in normal functioning, patients with MDD experience increased rates of other comorbid medical illnesses, including diabetes, arthritis, cardiovascular disease as well as comorbid psychiatric disorders [4–10].
Effective treatments for MDD are greatly needed, since MDD is very common and associated with high costs of health care as well as high morbidity and mortality [8, 9, 11–13]. Unfortunately, partial or suboptimal response to treatment occurs commonly in MDD, and only 30–40 % of patients receiving treatment will fully remit (achieving near-complete resolution of symptoms) [14–17]. The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study is one of the largest and more comprehensive studies of MDD treatments ever conducted. Responses to up to four successive treatment steps were studied in individuals with MDD. Remission was achieved in less than one third of patients receiving first- and second-line treatments; rates of remission were significantly lower in patients with treatment-resistant depression (TRD, i.e., those who have had failed two or more consecutive treatments) [14, 15]. The cumulative rate of remission was 67 % after all four levels. These sobering results indicate that the current treatment options are not very effective; even when effective treatment effects are very slow. Each level of treatment requires 12 weeks; a full year of treatments may be required in order to achieve significant positive outcomes (remission) in two thirds of the patients. This problem of treatment-resistant depression has led to the continued search for novel, more effective antidepressant treatments [18–25].
Given the current only partially effective antidepressant treatments and the imperfect, trial-and-error methods for treatment selection in MDD, predictive biomarkers could be particularly useful. Ideally, biomarkers predictive of treatment response to specific therapies could eliminate multiple and lengthy treatment steps by selecting the right treatment from the start.
The use of biomarkers to predict or identify a disease or disorder is an essential strategy in many areas of medicine, and is increasingly studied in psychiatric research. The United States Food and Drug Administration (FDA) defines a biomarker as an objective measurement of a normal biological process, a pathological, biological process or an objective measurement that indicates response to a therapeutic [26]. Biomarkers are commonly used for diseases such as cancer [27–29], however, no biomarker is routinely used clinically in psychiatry, despite the assumption that biological changes underlie or contribute to many psychiatric problems [30, 31]. Biomarkers could have several functions in psychiatry, including clarification of the etiology of psychiatric problems, and could be used as predictors of therapeutic response [32].
Many different biological parameters may potentially serve as biomarkers, such as specific genetic or epigenetic abnormalities, metabolites, proteins, or brain activity patterns. For example, specific changes in theta power on prefrontal leads in electroencephalograms (EEG) from baseline to week 1 of treatment have been used to predict antidepressant treatment outcomes at week 8 [33]. Moreover, EEG data has been shown to be specific enough to guide clinical treatment in patients with MDD [34]. Both resting-state EEGs as well as evoked potentials have been explored as biomarkers predictive of antidepressant treatment response [35]. EEGs may provide a useful tool for aiding in antidepressant therapy however access to the technology and imperfect predictive ability have limited its development so far. It is likely that, similar to other areas of medicine, biomarkers useful in psychiatry will involve a composite of clinical and biological factors [35]; proteins found in human biomaterials could play a significant role.
Brain neuroanatomical changes, as measured by MR morphometry, diffusion tensor imaging (DTI), or even functional MRI may also provide depression biomarkers. For example, DTI studies have suggested that white matter abnormalities may be present in treatment-resistant depression [36]. DTI has also been used to indicate that MDD may be associated with abnormal microstructure in brain reward/aversion regions, specifically the ventral tegmental area and dorsolateral prefrontal white matter [37]. While neuroimaging provides the potential to understand the impairment in neurocircuitry underlying TRD, it is unclear whether such results are specific enough to become useful biomarkers for diagnosis or treatment selection. Brain imaging techniques are also not easily accessible to all clinicians and expensive. Such instruments tend to be limited to major medical centers. Therefore, additional biomarkers, more easily deployed in the general population and based on blood or saliva samples that can be easily analyzed in remote labs, warrant exploration.
Genomics has witnessed a major search for biomarkers in psychiatry and candidate genomic biomarkers have been found for several psychiatric conditions, most notably, serotonin transport protein polymorphisms as predictors of depression and anxiety [38–41]. Specific gene mutations may interact with environmental factors to ultimately increase the risk of psychiatric problems [42–45]. However, despite the initial promise of genetic information, a recent mega-analysis of genome-association studies in MDD failed to find consistent genetic associations [46]. The search for gene mutations as psychiatric biomarkers may be flawed, since genomic information does not necessarily reflect active protein levels [47] or tell the researcher about possible important posttranslational modifications (PTMs) such as glycosylation, phosphorylation, or formation/destruction of disulfide bridges to keep/disturb the protein’s three-dimensional structure [48]. Epigenetics, studying the transcription status of genes, is probably a better reflection of temporal changes in gene expression; but the study of epigenetics with respect to biomarkers in MDD is still in its infancy. Additional proteomic information may expand possibilities for a disorder’s identification in clinical tests. Proteins represent the functional molecules in a biological system; therefore, study of proteins may take a researcher closer to identifying the cause of a disorder and could also suggest targets for therapeutics. Protein profiling of candidate biomarkers in psychiatry is therefore an area of/with great potential [49, 50]. Mass spectrometry (MS) is currently the technique of choice for proteomic studies [32, 49–73].
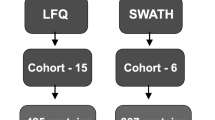
A recent PubMed search of depression and biomarkers reveals the extent to which different biomarker approaches are emphasized in the field of depression research. Using the search terms “depression biomarker” and adding a variable third term, yielded the following results: genomic = 306 articles, EEG = 112 articles, neuroimaging = 103 articles, proteomic = 34 articles, mass spectrometry = 40 articles (Fig. 27.1). This search underscores the need for expansion into the proteomic realm in the field of depression research.
MS-based proteomics is very useful for protein biomarker identification for several reasons. Using a variety of proteomics approaches, a researcher can detect and determine multiple properties of a specific sample [55, 56, 61, 63, 65–67]. Virtually all information about a protein/peptide such as mass, sequence information, and the charge state can be measured and identified using MS-based proteomic methods [66, 69, 70, 72, 74, 75]. Knowledge-based methods for protein biomarker discovery can also be employed, such as enzyme-linked immunoabsorbant assay (ELISA) [76], Western Blotting [72, 77], or immunohistochemistry [72, 78, 79]. These techniques can be used independently, with the downside being that the “discovery” aspect is negated by the need to identify a target protein. They may also be used to validate and expand upon the more comprehensive screening provided by MS. A general proteomics approach is presented in Fig. 27.2. Here the protein samples from various sources are either fractionated, digested, and then analyzed by MS (liquid chromatography-tandem mass spectrometry), followed by data analysis, validation, and follow up, or analyzed without a priori digestion (i.e., by matrix-assisted laser desorption ionization MS or MALDI-MS) followed by data analysis, verification, and follow up. Many times, when the expertise and instrumentation are available, both methods are used simultaneously and their outcome complements each other.
Schematic of a full proteomics experiment. The protein sample is separated/fractionated under non-denaturing (1) and denaturing (2) conditions, digested (3) and analyzed by LC-MS/MS (4) (bottom-up proteomics). Database search and data analysis (5) led to identification of proteins, post-translational modifications (PTMs) in proteins and protein–protein interactions (PPIs), that were verified and then validated by Western blotting (6), and then monitored by single reaction monitoring (SRM), multiple reaction monitoring (MRM), and/or cross-validation. The original protein samples can also be analyzed by MALDI-MS (8) that leads to identification of specific protein/peptide patterns whose data analysis (10) leads to identification of proteins, PTMs, and PPIs. The fractionated samples in (2) can also be investigated without using electrophoretic denaturing conditions (2A) in a process called in solution digestion, or analyzed without any digestion (2B) in a process called top-down proteomics. In a third alternative, the fractionated samples from (2) are analyzed without digestion directly by MALDI-MS (2C). © 2013 Wormwood KL, et al. Reproduced from Wormwood et al., J. Proteomics Bioinform 2013, S5, http://dx.doi.org/10.4172/jpb.S5-001
27.1.1 Protein Biomarkers in MDD
Depression has indeed been associated with several protein biomarkers, which have been identified using both directed methods as well as mass spectrometry [49, 80]. For example, serum brain-derived neurotrophic factor (BDNF) appears to be decreased relative to healthy controls, based on immunological measurement techniques [81–85]. A recent study using ELISA confirmed that ketamine treatment indeed results in rapid upregulation of BDNF in those patients who are responders, measured in blood sera. Ketamine has been recently identified as producing rapid antidepressant response [86], which is in contrast to many antidepressants currently used, which take several weeks to produce a response [87]. Greater understanding of the factors producing BDNF upregulation may help in predicting responders to ketamine or possibly other antidepressants. MS and comprehensive proteomics may further expand upon directed approaches to yield more biomarker candidates.
27.1.2 Use of Animal Models and MS
MS and proteomic approaches have been utilized to identify putative biomarkers in depression animal models. An animal study examined the effects of chronic stress on proteins found in the hippocampus of rats. MALDI-TOF-MS was utilized to identify found 27 potential protein markers that were dysregulated relative to non-stressed control animals. These proteins were known to have roles in neurogenesis, oxidative metabolism, transcription, and signal transduction [88]. This is particularly relevant to depression based on the observation that the hippocampus may decrease in volume in individuals who are depressed [89]. A separate study Using iTRAQ labeling, a label-based method used to identify and quantify proteins, coupled with MS, quantified 2,000 proteins from rat hippocampus in a stress model of depression. Seventy-three proteins were found to be differentially expressed. Deficits in vesicular release proteins (SNCA, SYN-1, and AP-3) were found with a relationship to stress susceptibility. Increased expression of a sodium channel protein (SCN9A) also predicted susceptibility to stress [90]. Such susceptibility could provide a model for biomarkers predictive of depression, although naturally these results would need to be replicated in humans.
27.1.3 Protein Biomarkers in MDD: Human Studies
In addition to animal models, MS has indeed also yielded biomarker insights in humans. Alawam et al., used MALDI-MS with a C18 magnetic beads protocol to analyze serum samples from 39 individuals with depression and 30 controls. C18 magnetic silica beads are used for protein and peptide sample concentration, desalting, and fractionation. C18 beads are coated with C18 alkyl groups, which allow them to provide a reversed phase surface chemistry and, through fractionation of proteins and peptides, reduce sample complexity. No protein signals distinguished participants with depression from controls, however, analysis of individual peptide signals identified three signals that were distinct in the depression group. The specific identities of these peptides were however, not reported [91]. Protein identification is the next step to establish biomarkers, although comprehensive protein fingerprints via spectral differences could also serve as a potential diagnostic.
Proteomic analysis of brain tissue is an approach that can be used to identify MDD biomarkers, although naturally the approach is limited to post-mortem tissue. A proteomic study using difference gel electrophoresis (DIGE) identified 59 potential biomarkers in cerebral cortex and 11 in amygdala in post-mortem brain tissue from suicide victims. Proteins identified were those that control biological functions and structures such as metabolism, the redox system, the cytoskeleton, synaptic function, and proteolysis [92]. Another group used shotgun proteomics to analyze post-mortem dorsolateral prefrontal cortex brain tissue from 24 MDD patients and 12 matched controls [93]. Shotgun proteomics refers to the use of bottom-up proteomics techniques in identifying proteins in complex mixtures. This method usually takes advantage of combining HPLC with MS. Distinct protein fingerprints resulted from significantly, differentially expressed proteins between subgroups of MDD patients (with and without psychosis) as well as between MDD subjects and healthy controls. Differentially expressed proteins between MDD patients and healthy controls were those involved in metabolism, transport, cell communication and signalling, cell growth and maintenance, protein metabolism, and regulation of nucleic acid metabolism [93].
In addition to the analysis of brain tissue, MS and proteomic approaches have been used to analyze bodily fluids. The advantage of this approach is naturally the possibility of identifying biomarkers in live subjects, with the hope that the proteins identified reflect brain processes or have the potential for diagnosis and/or prediction of response. Cerebrospinal fluid (CSF) is naturally the closest fluid to brain tissue, and therefore may be most suitable for reflecting brain content. The downside of CSF use is the invasive nature of collection and need for a spinal tap. CNS has been analyzed using MALDI-TOF-MS to compare individuals with MDD versus controls. This study reported 11 proteins and 144 peptide features that were significantly different in the CSF from depressed patients versus controls. The investigators also found differences in the phosphorylation pattern of several CSF proteins, underscoring the additional utility of MS for identifying PTMs as well as protein levels. Identified dysregulated proteins in this study were those involved with neuroprotection, neuronal development, sleep regulation, and amyloid plaque deposition in aging brain [94], reflecting possible disruptions of these systems by depression, involvement of these systems in the etiology of depression, or both.
Blood plasma or serum is more accessible than CSF, and may also be used for proteomic identification in MDD. Depression has been associated with disturbances in cholesterol transport and metabolism, which is mediated by apolipoproteins [32]. Indeed, a study utilizing multidimensional liquid chromatography-tandem mass spectrometry with validation by immunoblotting or ELISA to analyze blood plasma, several protein biomarkers that are altered in depressed individuals. The primary function of the identified proteins was in lipid metabolism and immunoregulation [95]. This is consistent with prior observations of increased disease incidence with depression [4–10] as well as lipid perturbations that have been observed in depression [32].
Urine analysis could be most convenient and amenable to an MDD diagnostic or predictive test. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) was used to corroborate levels of urinary serotonin in individuals with depression taking antidepressants. A strong correlation was measured between urinary serotonin levels measured by ELISA. Using ELISA, serotonin levels detected in depressed patients were significantly lower than in control subjects and 5-hydroxy-tryptophane and/or selective serotonin re-uptake inhibitors significantly increased urinary serotonin levels [96]. Biological monitoring of depression and response to antidepressants may therefore be possible via urinary analysis.
Saliva is an accessible biofluid that has not been fully exploited in depression research. Saliva collection is noninvasive and convenient. In all, 2,290 proteins have been found in saliva compared with 2,698 proteins found in plasma. Nearly 40 % of proteins believed to be candidate markers for diseases such as cancer, cardiovascular disease, and stroke can be found in whole saliva, Therefore, saliva presents a convenient, noninvasive, accessible bodily fluid for analysis [97]. Potential salivary biomarkers have been identified for other disorders, specifically Alzheimer’s disease [98] and autism spectrum disorder [99]. Although we have not been able to identify analyses of MDD salivary proteome, salivary cortisol in MDD has been analyzed using directed methods (competitive radioimmunoassay for cortisol) rather than the comprehensive screening provided by MS. High salivary cortisol was not found to be a risk factor for MDD, however, low mean salivary cortisol concentration and a small difference between morning and evening cortisol concentrations were identified as possible risk factors [100]. Saliva may be an unexploited biofluid for MS analysis in MDD that warrants further exploration.
27.1.4 Metabolomics for MS-Based Biomarker Discovery in MDD
Based on prevalent hypotheses that small molecules, such as monoamine neurotransmitters, are dysregulated in MDD [2], metabolomics is an approach that may yield biomarkers in MDD. Metabolomics is the investigation of the metabolites, or small molecules that exist on a cell or a bodily fluid at a particular timepoint, and can be performed using specialized MS approaches. In a study comprising 26 subjects with MDD versus controls, blood sera content was measured using a 3200 QTRAP MS system. The investigators found depletions in tryptophan, lysine, and gamma amino butyric acid (GABA) in the subjects with MDD [101]. Proton nuclear magnetic resonance ((1)H NMR) spectrometry has also been used to distinguish metabolomic differences in MDD plasma relative to control plasma. Investigators have reported use of this method to accurately diagnose MDD in 26 subjects with sensitivity and specificity of 92.8 % and 83.3 %, respectively [102]. The prevalent monoamine theory of depression as well as the known mechanism of action of many antidepressant medications on neurotransmitters (small molecules) suggests that metabolomics may be particularly useful for MS-based exploration of biomarkers in MDD. The ability to measure metabolites in blood, urine, or saliva could provide a useful diagnostic and predictive test for MDD.
27.1.5 Protein Preparation Methods
Preparing samples for MS analysis can be a crucial component of biomarker discovery. In fact, it may be considered the most important component of the MS analysis. Depending on how the sample is prepared, one can get either useless results or significant results with high clinical relevance. This is well reflected in the NCI Clinical Proteomic Tumor Analysis Consortium (CPTAC) study, in which different proteomics labs from the United States, with different instrumentation and instrument settings obtained different results [103]. For example, the methods by which samples are collected are crucial, including how they are processed, frozen (and how many times they are thawed). Instrument settings need to be identical, for high reproducibility. Furthermore, It also matters whether the samples to be analyzed (i.e., sera) are depleted or not and if so, whether the depletion is performed under identical conditions in different labs. At its best, due to the secretome and/or functional degradome (truncated proteins with physiological significance), as well as posttranslational proteomics (labile or transient/reversible phosphorylations, acetylations, methylations, glycosylations, etc.), the samples have to be kept as intact as possible and then processed. For example, one study identified transferrin and fibrinogen as potential biomarkers, based on 6 M HCL hydrolyzation of serum proteins followed by MALDI-TOF MS [104]. However, HCl incubation caused rapid protein decomposition. To distinguish between samples from individuals with MDD versus control samples, the same investigators reported that protein hydrolysis using 20 % TFA and sinapinic acid were the optimal reagents for protein hydrolysis and found that the same markers, fibrinogen and transferrin, could be distinguished as potential biomarkers for MDD, with higher peaks identified for fibrinogen relative to controls and lower peaks for transferrin (relative intensity) [105]. However, analysis of the forced, uncontrolled fragmentation of the proteins from the samples may be dangerous, as it may be difficult to reproduce and translate into clinical settings. Therefore, sample preparation is and will always be the most crucial part of the proteomics that will allow one to obtain significant results with clinical relevance.
27.1.6 Effects of Antidepressant Treatment on Protein Biomarkers
In addition to understanding depression, naturally MS-based proteomics may ultimately elucidate markers that correspond with outcomes of antidepressant treatment. Initial proteomic analysis in animal models indicates possible protein changes associated with the use of antidepressant medications. A proteomic study analyzed monoamine reuptake inhibitors (MAOIs) and protein changes that occurred in rat hippocampal cytosolic extract. Either venlafaxine (primarily noradrenergic) or fluoxetine (primarily serotonergic) was systemically administered to adult rats for 2 weeks, after which 2D gel electrophoresis identified 31 proteins that were upregulated and two that were down-regulated. MALDI TOF MS was used to identify these proteins. Treatment with both antidepressants led to the upregulation of several factors associated with central nervous system function. These include those associated with neurogenesis (IGF-1, glia maturation factor) neuronal process outgrowth, and maintenance (hippocampal cholinergic neurostimulating peptide [HCNP]-precursor; PCTAIRE-3; serine protease inhibitor 2.1), and anti-apoptotic activity (dimethylargininase-1 l-N,N-dimethylarginine dimethylaminohydrolase-1 [DDAH1], antioxidant protein-2 [AOP-2], and pyruvate dehydrogenase-E1 [PDH-E1]) [106]. Whether similar markers can be measured in human bodily fluids remains to be seen.
Using directed protein measurements (immunoblot and electrophoretic mobility shift assays) of total cyclic AMP response element binding protein (tCREB) in T-lymphocytes, it has been found that subjects with MDD and low baseline tCREB were significantly more likely to respond (78 %) to selective serotonin reuptake inhibitor (SSRI) treatment than individuals with high baseline tCREB (36 %) [107]. This study illustrates that biomarkers that are predictive of antidepressant response could be very useful to directing and selecting treatments. The question remains as to whether tCREB is a specific marker for SSRI response, or anti-depressant response in general. MS and proteomic have the potential to reveal further protein biomarkers and expand upon this therapeutic area, which will become increasingly important as more treatment options with different mechanisms of action become available.
27.2 Concluding Remarks
Although various biomarkers for MDD have been identified using an assortment of methods, the true test of a biomarker will be its validity, reproducibility, and prediction of therapeutic response. In addition, biomarkers for use in clinical tests will need to be identified in an inexpensive, quick, and convenient manner. For this reason, protein tests may be particularly useful. Proteins can be derived from easily obtainable bodily fluids, such as blood and even saliva. MS has the potential to identify new protein or even metabolite targets that may ultimately be used in tests. Such tests may be conducted via MS, or using directed protein-identification methods that are quick, cheap, and easy. The hope is to develop a form of personalized medicine for MDD that can direct the choice of treatment, particularly in light of the high rate of depression relapse and the high rate of treatment-resistance.
References
Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU (2012) Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res 21:169–184
To SE, Zepf RA, Woods AG (2005) The symptoms, neurobiology, and current pharmacological treatment of depression. J Neurosci Nurs 37:102–107
APA (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Arlington, VA
Woods AG (2004) Understanding depression and diabetes. Diabetes Self Manag 21:6, 8, 11–12
Strine TW, Mokdad AH, Balluz LS, Gonzalez O, Crider R, Berry JT et al (2008) Depression and anxiety in the United States: findings from the 2006 Behavioral Risk Factor Surveillance System. Psychiatr Serv 59:1383–1390
Niranjan A, Corujo A, Ziegelstein RC, Nwulia E (2012) Depression and heart disease in US adults. Gen Hosp Psychiatry 34:254–261
Mathew CS, Dominic M, Isaac R, Jacob JJ (2012) Prevalence of depression in consecutive patients with type 2 diabetes mellitus of 5-year duration and its impact on glycemic control. Indian J Endocrinol Metab 16:764–768
Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:617–627
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR et al (2003) The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289:3095–3105
Chapman D, Perry G, Strine T (2005) The vital link between chronic disease and depressive disorders. Prev Chronic Dis 2:A14
Shim RS, Baltrus P, Ye J, Rust G (2011) Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. J Am Board Fam Med 24:33–38
Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D (2003) Cost of lost productive work time among US workers with depression. JAMA 289:3135–3144
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC (2005) Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:629–640
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D et al (2006) Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 163:1905–1917
Trivedi MH, Rush AJ, Wisniewski SR, Warden D, McKinney W, Downing M et al (2006) Factors associated with health-related quality of life among outpatients with major depressive disorder: a STAR*D report. J Clin Psychiatry 67:185–195
Trivedi MH, Fava M, Wisniewski SR, Thase ME, Quitkin F, Warden D et al (2006) Medication augmentation after the failure of SSRIs for depression. N Engl J Med 354:1243–1252
Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME et al (2006) Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med 354:1231–1242
Woods AG (2008) Give a man a fish. Essential fatty acids in health and disease. Diabetes Self Manag 25:8, 11–12, 14
Roth R (2012) Lisdexamfetamine dimesylate augmentation for executive dysfunction in adults with fully or partially remitted major depressive disorder. In: The 165th annual meeting of the American Psychiatric Association, Philadelphia, PA
Piet J, Hougaard E (2011) The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev 31:1032–1040
Pehrson AL, Sanchez C (2013) Serotonergic modulation of glutamate neurotransmission as a strategy for treating depression and cognitive dysfunction. CNS Spectr 19(2):121–133
Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Green CM, Perez AM et al (2013) Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry 170:1134–1142
Mantione E, Micheloni S, Alcaino C, New K, Mazzaferro S, Bermudez I (2012) Allosteric modulators of alpha4beta2 nicotinic acetylcholine receptors: a new direction for antidepressant drug discovery. Future Med Chem 4:2217–2230
Keefe R (2012) Lisdexamfetamine dimesylate in the treatment of cognitive dysfunction in patients with partially or fully remitted major depressive disorder. In: 165th annual meeting of the American Psychiatric Association, Philadelphia, PA
Celada P, Bortolozzi A, Artigas F (2013) Serotonin 5-HT1A receptors as targets for agents to treat psychiatric disorders: rationale and current status of research. CNS Drugs 27:703–716
Martins-De-Souza D, Wobrock T, Zerr I, Schmitt A, Gawinecka J, Schneider-Axmann T et al (2010) Different apolipoprotein E, apolipoprotein A1 and prostaglandin-H2 D-isomerase levels in cerebrospinal fluid of schizophrenia patients and healthy controls. World J Biol Psychiatry 11:719–728
Pallis AG, Fennell DA, Szutowicz E, Leighl NB, Greillier L, Dziadziuszko R (2011) Biomarkers of clinical benefit for anti-epidermal growth factor receptor agents in patients with non-small-cell lung cancer. Br J Cancer 105:1–8
Phillips KA, Marshall DA, Haas JS, Elkin EB, Liang SY, Hassett MJ et al (2009) Clinical practice patterns and cost effectiveness of human epidermal growth receptor 2 testing strategies in breast cancer patients. Cancer 115:5166–5174
Ross JS (2011) Biomarker-based selection of therapy for colorectal cancer. Biomark Med 5:319–332
Lakhan SE, Vieira K, Hamlat E (2010) Biomarkers in psychiatry: drawbacks and potential for misuse. Int Arch Med 3:1
Singh I, Rose N (2009) Biomarkers in psychiatry. Nature 460:202–207
Woods AG, Sokolowska I, Taurines R, Gerlach M, Dudley E, Thome J et al (2012) Potential biomarkers in psychiatry: focus on the cholesterol system. J Cell Mol Med 16:1184–1195
Cook IA, Hunter AM, Gilmer WS, Iosifescu DV, Zisook S, Burgoyne KS et al (2013) Quantitative electroencephalogram biomarkers for predicting likelihood and speed of achieving sustained remission in major depression: a report from the biomarkers for rapid identification of treatment effectiveness in major depression (BRITE-MD) trial. J Clin Psychiatry 74:51–56
Greenblatt JM, Sussman C, Jameson M, Yuan L, Hoffman DA, Iosifescu DV (2011) Retrospective chart review of a referenced EEG database in assisting medication selection for treatment of depression in patients with eating disorders. Neuropsychiatr Dis Treat 7:529–541
Iosifescu DV (2011) Electroencephalography-derived biomarkers of antidepressant response. Harv Rev Psychiatry 19:144–154
Hoogenboom WS, Perlis RH, Smoller JW, Zeng-Treitler Q, Gainer VS, Murphy SN et al (2014) Limbic system white matter microstructure and long-term treatment outcome in major depressive disorder: a diffusion tensor imaging study using legacy data. World J Biol Psychiatry 15:122–134
Blood AJ, Iosifescu DV, Makris N, Perlis RH, Kennedy DN, Dougherty DD et al (2010) Microstructural abnormalities in subcortical reward circuitry of subjects with major depressive disorder. PLoS One 5:e13945
Barnett JH, Smoller JW (2009) The genetics of bipolar disorder. Neuroscience 164: 331–343
Kvajo M, McKellar H, Gogos JA (2010) Molecules, signaling, and schizophrenia. Curr Top Behav Neurosci 4:629–656
Poelmans G, Pauls DL, Buitelaar JK, Franke B (2011) Integrated genome-wide association study findings: identification of a neurodevelopmental network for attention deficit hyperactivity disorder. Am J Psychiatry 168:365–377
Weber H, Kittel-Schneider S, Gessner A, Domschke K, Neuner M, Jacob CP et al (2011) Cross-disorder analysis of bipolar risk genes: further evidence of DGKH as a risk gene for bipolar disorder, but also unipolar depression and adult ADHD. Neuropsychopharmacology 36:2076–2085
Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE (2010) Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry 167:509–527
Kolassa IT, Kolassa S, Ertl V, Papassotiropoulos A, De Quervain DJ (2010) The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-o-methyltransferase Val(158)Met polymorphism. Biol Psychiatry 67:304–308
Lahey BB, Rathouz PJ, Lee SS, Chronis-Tuscano A, Pelham WE, Waldman ID et al (2011) Interactions between early parenting and a polymorphism of the child’s dopamine transporter gene in predicting future child conduct disorder symptoms. J Abnorm Psychol 120:33–45
Roy A, Sarchiopone M, Carli V (2009) Gene-environment interaction and suicidal behavior. J Psychiatr Pract 15:282–288
Major Depressive Disorder Working Group of the Psychiatric GWAS Consortium, Ripke S, Wray NR, Lewis CM, Hamilton SP, Weissman MM et al (2013) A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 18:497–511
Anderson L, Seilhamer J (1997) A comparison of selected mRNA and protein abundances in human liver. Electrophoresis 18:533–537
Junaid MA, Pullarkat RK (2001) Proteomic approach for the elucidation of biological defects in autism. J Autism Dev Disord 31:557–560
Ngounou Wetie AG, Sokolowska I, Wormwood K, Michel TM, Thome J, Darie CC et al (2013) Mass spectrometry for the detection of potential psychiatric biomarkers. J Mol Psychiatry 1:8
Woods AG, Ngounou Wetie AG, Sokolowska I, Russell S, Ryan JP, Michel TM et al (2013) Mass spectrometry as a tool for studying autism spectrum disorder. J Mol Psychiatry 1:6
Darie C (2013) Investigation of protein-protein interactions by blue native-PAGE & mass spectrometry. Mod Chem Appl 1:e111
Darie CC, Biniossek ML, Gawinowicz MA, Milgrom Y, Thumfart JO, Jovine L et al (2005) Mass spectrometric evidence that proteolytic processing of rainbow trout egg vitelline envelope proteins takes place on the egg. J Biol Chem 280:37585–37598
Darie CC, Biniossek ML, Jovine L, Litscher ES, Wassarman PM (2004) Structural characterization of fish egg vitelline envelope proteins by mass spectrometry. Biochemistry 43:7459–7478
Darie CC, Biniossek ML, Winter V, Mutschler B, Haehnel W (2005) Isolation and structural characterization of the Ndh complex from mesophyll and bundle sheath chloroplasts of Zea mays. FEBS J 272:2705–2716
Darie CC, Deinhardt K, Zhang G, Cardasis HS, Chao MV, Neubert TA (2011) Identifying transient protein-protein interactions in EphB2 signaling by blue native PAGE and mass spectrometry. Proteomics 11:4514–4528
Darie CC, Janssen WG, Litscher ES, Wassarman PM (2008) Purified trout egg vitelline envelope proteins VEbeta and VEgamma polymerize into homomeric fibrils from dimers in vitro. Biochim Biophys Acta 1784:385–392
Darie CC, Litscher ES, Wassarman PM (2008) Structure, processing, and polymerization of rainbow trout egg vitelline envelope proteins. Nato Scie Peace Secu 23–36
Darie CC, Shetty V, Spellman DS, Zhang GJ, Xu CF, Cardasis HL et al (2008) Blue native page and mass spectrometry analysis of ephrin stimulation-dependent protein-protein interactions in Ng108-Ephb2 cells. Nato Scie Peace Secu 3–22
Ngounou Wetie AG, Sokolowska I, Woods AG, Darie CC (2013) Identification of post-translational modifications by mass spectrometry. Aust J Chem 66:734–748
Ngounou Wetie AG, Sokolowska I, Woods AG, Roy U, Deinhardt K, Darie CC (2014) Protein-protein interactions: switch from classical methods to proteomics and bioinformatics-based approaches. Cell Mol Life Sci 71:205–228
Ngounou Wetie AG, Sokolowska I, Woods AG, Roy U, Loo JA, Darie CC (2013) Investigation of stable and transient protein-protein interactions: past, present, and future. Proteomics 13:538–557
Ngounou Wetie AG, Sokolowska I, Woods AG, Wormwood KL, Dao S, Patel S et al (2013) Automated mass spectrometry-based functional assay for the routine analysis of the secretome. J Lab Autom 18:19–29
Sokolowska I, Dorobantu C, Woods AG, Macovei A, Branza-Nichita N, Darie CC (2012) Proteomic analysis of plasma membranes isolated from undifferentiated and differentiated HepaRG cells. Proteome Sci 10:47
Sokolowska I, Gawinowicz MA, Ngounou Wetie AG, Darie CC (2012) Disulfide proteomics for identification of extracellular or secreted proteins. Electrophoresis 33:2527–2536
Sokolowska I, Ngounou Wetie AG, Roy U, Woods AG, Darie CC (1834) Mass spectrometry investigation of glycosylation on the NXS/T sites in recombinant glycoproteins. Biochim Biophys Acta 2013:1474–1483
Sokolowska I, Ngounou Wetie AG, Woods AG, Darie CC (2012) Automatic determination of disulfide bridges in proteins. J Lab Autom 17:408–416
Sokolowska I, Ngounou Wetie AG, Woods AG, Darie CC (2013) Applications of mass spectrometry in proteomics. Aust J Chem 66:721–733
Sokolowska I, Ngounou Wetie AG, Wormwood K, Michel TM, Thome J, Darie CC et al (2013) The potential of biomarkers in psychiatry: focus on proteomics. J Neural Transm. [Epub ahead of print]
Sokolowska I, Woods AG, Gawinowicz MA, Roy U, Darie CC (2012) Identification of potential tumor differentiation factor (TDF) receptor from steroid-responsive and steroid-resistant breast cancer cells. J Biol Chem 287:1719–1733
Sokolowska I, Woods AG, Gawinowicz MA, Roy U, Darie CC (2013) Characterization of tumor differentiation factor (TDF) and its receptor (TDF-R). Cell Mol Life Sci 70:2835–2848
Sokolowska I, Woods AG, Wagner J, Dorler J, Wormwood K, Thome J et al (2011) Mass spectrometry for proteomics-based investigation of oxidative stress and heat shock proteins. In: Andreescu S, Hepel M (eds) Oxidative stress: diagnostics, prevention, and therapy. American Chemical Society, Washington, DC
Woods AG, Sokolowska I, Deinhardt K, Sandu C, Darie CC (2013) Identification of tumor differentiation factor (TDF) in select CNS neurons. Brain Struct Funct. [Epub ahead of print]
Woods AG, Sokolowska I, Yakubu R, Butkiewicz M, LaFleur M, Talbot C et al (2011) Blue native page and mass spectrometry as an approach for the investigation of stable and transient protein-protein interactions. In: Andreescu S, Hepel M (eds) Oxidative stress: diagnostics, prevention, and therapy. American Chemical Society, Washington, DC
Roy U, Sokolowska I, Woods AG, Darie CC (2012) Structural investigation of tumor differentiation factor. Biotechnol Appl Biochem 59:445–450
Taurines R, Dudley E, Grassl J, Warnke A, Gerlach M, Coogan AN et al (2011) Proteomic research in psychiatry. J Psychopharmacol 25:151–196
Haile CN, Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Foulkes A et al (2014) Plasma brain derived neurotrophic factor (BDNF) and response to ketamine in treatment-resistant depression. Int J Neuropsychopharmacol 17(2):331–336
Kazuno AA, Ohtawa K, Otsuki K, Usui M, Sugawara H, Okazaki Y et al (2013) Proteomic analysis of lymphoblastoid cells derived from monozygotic twins discordant for bipolar disorder: a preliminary study. PLoS One 8:e53855
Woods AG, Poulsen FR, Gall CM (1999) Dexamethasone selectively suppresses microglial trophic responses to hippocampal deafferentation. Neuroscience 91:1277–1289
Woods AG, Guthrie KM, Kurlawalla MA, Gall CM (1998) Deafferentation-induced increases in hippocampal insulin-like growth factor-1 messenger RNA expression are severely attenuated in middle aged and aged rats. Neuroscience 83:663–668
Schneider B, Prvulovic D (2013) Novel biomarkers in major depression. Curr Opin Psychiatry 26:47–53
Yoshida T, Ishikawa M, Niitsu T, Nakazato M, Watanabe H, Shiraishi T et al (2012) Decreased serum levels of mature brain-derived neurotrophic factor (BDNF), but not its precursor proBDNF, in patients with major depressive disorder. PLoS One 7:e42676
Kotan Z, Sarandol E, Kirhan E, Ozkaya G, Kirli S (2012) Serum brain-derived neurotrophic factor, vascular endothelial growth factor and leptin levels in patients with a diagnosis of severe major depressive disorder with melancholic features. Ther Adv Psychopharmacol 2:65–74
Molendijk ML, Bus BA, Spinhoven P, Penninx BW, Kenis G, Prickaerts J et al (2011) Serum levels of brain-derived neurotrophic factor in major depressive disorder: state-trait issues, clinical features and pharmacological treatment. Mol Psychiatry 16:1088–1095
Huang TL, Lee CT, Liu YL (2008) Serum brain-derived neurotrophic factor levels in patients with major depression: effects of antidepressants. J Psychiatr Res 42:521–525
Karege F, Perret G, Bondolfi G, Schwald M, Bertschy G, Aubry JM (2002) Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res 109:143–148
Carlson PJ, Diazgranados N, Nugent AC, Ibrahim L, Luckenbaugh DA, Brutsche N et al (2013) Neural correlates of rapid antidepressant response to ketamine in treatment-resistant unipolar depression: a preliminary positron emission tomography study. Biol Psychiatry 73:1213–1221
Harmer CJ, Cowen PJ (2013) ‘It’s the way that you look at it’—a cognitive neuropsychological account of SSRI action in depression. Philos Trans R Soc Lond B Biol Sci 368:20120407
Mu J, Xie P, Yang ZS, Yang DL, Lv FJ, Luo TY et al (2007) Neurogenesis and major depression: implications from proteomic analyses of hippocampal proteins in a rat depression model. Neurosci Lett 416:252–256
Posener JA, Wang L, Price JL, Gado MH, Province MA, Miller MI et al (2003) High-dimensional mapping of the hippocampus in depression. Am J Psychiatry 160:83–89
Henningsen K, Palmfeldt J, Christiansen S, Baiges I, Bak S, Jensen ON et al (2012) Candidate hippocampal biomarkers of susceptibility and resilience to stress in a rat model of depression. Mol Cell Proteomics 11:M111.016428
Alawam K, Dudley E, Donev R, Thome J (2012) Protein and peptide profiling as a tool for biomarker discovery in depression. Electrophoresis 33:3830–3834
Kekesi KA, Juhasz G, Simor A, Gulyassy P, Szego EM, Hunyadi-Gulyas E et al (2012) Altered functional protein networks in the prefrontal cortex and amygdala of victims of suicide. PLoS One 7:e50532
Martins-de-Souza D, Guest PC, Harris LW, Vanattou-Saifoudine N, Webster MJ, Rahmoune H et al (2012) Identification of proteomic signatures associated with depression and psychotic depression in post-mortem brains from major depression patients. Transl Psychiatry 2:e87
Ditzen C, Tang N, Jastorff AM, Teplytska L, Yassouridis A, Maccarrone G et al (2012) Cerebrospinal fluid biomarkers for major depression confirm relevance of associated pathophysiology. Neuropsychopharmacology 37:1013–1025
Xu HB, Zhang RF, Luo D, Zhou Y, Wang Y, Fang L et al (2012) Comparative proteomic analysis of plasma from major depressive patients: identification of proteins associated with lipid metabolism and immunoregulation. Int J Neuropsychopharmacol 15:1413–1425
Nichkova MI, Huisman H, Wynveen PM, Marc DT, Olson KL, Kellermann GH (2012) Evaluation of a novel ELISA for serotonin: urinary serotonin as a potential biomarker for depression. Anal Bioanal Chem 402:1593–1600
Hu S, Li Y, Wang J, Xie Y, Tjon K, Wolinsky L et al (2006) Human saliva proteome and transcriptome. J Dent Res 85:1129–1133
Shi M, Sui YT, Peskind ER, Li G, Hwang H, Devic I et al (2011) Salivary tau species are potential biomarkers of Alzheimer’s disease. J Alzheimers Dis 27:299–305
Castagnola M, Messana I, Inzitari R, Fanali C, Cabras T, Morelli A et al (2008) Hypo-phosphorylation of salivary peptidome as a clue to the molecular pathogenesis of autism spectrum disorders. J Proteome Res 7:5327–5332
Grynderup MB, Kolstad HA, Mikkelsen S, Andersen JH, Bonde JP, Buttenschon HN et al (2013) A two-year follow-up study of salivary cortisol concentration and the risk of depression. Psychoneuroendocrinology 38:2042–2050
Xu HB, Fang L, Hu ZC, Chen YC, Chen JJ, Li FF et al (2012) Potential clinical utility of plasma amino acid profiling in the detection of major depressive disorder. Psychiatry Res 200:1054–1057
Zheng P, Gao HC, Li Q, Shao WH, Zhang ML, Cheng K et al (2012) Plasma metabonomics as a novel diagnostic approach for major depressive disorder. J Proteome Res 11:1741–1748
Ellis MJ, Gillette M, Carr SA, Paulovich AG, Smith RD, Rodland KK et al (2013) Connecting genomic alterations to cancer biology with proteomics: the NCI Clinical Proteomic Tumor Analysis Consortium. Cancer Discov 3:1108–1112
Lo LH, Huang TL, Shiea J (2009) Acid hydrolysis followed by matrix-assisted laser desorption/ionization mass spectrometry for the rapid diagnosis of serum protein biomarkers in patients with major depression. Rapid Commun Mass Spectrom 23:589–598
Huang TL, Cho YT, Su H, Shiea J (2013) Principle component analysis combined with matrix-assisted laser desorption ionization mass spectrometry for rapid diagnosing the sera of patients with major depression. Clin Chim Acta 424:175–181
Khawaja X, Xu J, Liang JJ, Barrett JE (2004) Proteomic analysis of protein changes developing in rat hippocampus after chronic antidepressant treatment: implications for depressive disorders and future therapies. J Neurosci Res 75:451–460
Lim SW, Kim S, Carroll BJ, Kim DK (2013) T-lymphocyte CREB as a potential biomarker of response to antidepressant drugs. Int J Neuropsychopharmacol 16:967–974
Acknowledgments
This work was supported in part by the U.S. Army research office through the Defense University Research Instrumentation Program (DURIP grant #W911NF-11-1-0304). We thank supporters of the Biochemistry & Proteomics Group, specifically Bob and Karen Brown, Bonhomie Imports, Wolverine, and the SciFund challenge contributors.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Woods, A.G., Iosifescu, D.V., Darie, C.C. (2014). Biomarkers in Major Depressive Disorder: The Role of Mass Spectrometry. In: Woods, A., Darie, C. (eds) Advancements of Mass Spectrometry in Biomedical Research. Advances in Experimental Medicine and Biology, vol 806. Springer, Cham. https://doi.org/10.1007/978-3-319-06068-2_27
Download citation
DOI: https://doi.org/10.1007/978-3-319-06068-2_27
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06067-5
Online ISBN: 978-3-319-06068-2
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)