Abstract
Autonomic hyperactivities are severe life-threatening conditions, which require intensive management. Treatment is mainly symptomatic, eventually supported with a variable degree of sedation and stimulus deprivation. Stabilization of blood pressure, heart rate, and temperature is a challenge in these patients.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
7.1 Case Introduction
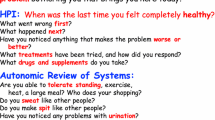
In March, a 63-year-old accountant wanted to ride his motorbike from a shed, where he kept it in winter times, to his house to prepare it for the new season. Since this was only some 150 meters, he did not care to wear a helmet. After riding about half of the distance, he pulled the gas not noticing that the concrete at this very spot was covered with some gravel from winter times. His family heard a short revving of his engine, followed by crash noise, and immediately came to help. When paramedics arrived, he had Glasgow Coma Scale of 9, continuously worsening. Paramedics requested an air-bound emergency doctor transport to the hospital. Due to his diminishing consciousness, he was intubated before the helicopter left the site.
Emergency trauma room CT revealed a basal skull fracture, temporal right contrecoup hemorrhage, right subdural hematoma, and subarachnoidal hematoma (Fig. 7.1a). An intracranial transducer was placed; opening intracranial pressure was 22 mmHg. Through intensive care management, the intracranial pressure could be controlled, but autonomic monitoring revealed severe fluctuations of heart rate and blood pressure, occurring at the very moment of intracranial pressure fluctuations (Fig. 7.1b). The frequency of fluctuations increased (Fig. 7.1c). On day 3, MRI revealed an additional left frontal coup hemorrhage. On day 5 the patient suffered cardiac arrest. Despite prolonged cardiopulmonary resuscitation at the intensive care ward, a sufficient circulation could not be restored, and the patient died.
(a) Admission CT scan showing temporal right contrecoup hemorrhage, right subdural hematoma, subarachnoidal hematoma, and basal skull fracture. (b) Autonomic monitoring day 1: fluctuations of heart rate, blood pressure according to intracranial pressure fluctuations. Upper trace (white) heart rate, lower trace (red) systolic and diastolic blood pressure. (c) Autonomic monitoring day 3: increased frequency of fluctuations. Upper trace (white) heart rate, lower trace (red) systolic and diastolic blood pressure
7.1.1 Introduction
One of the most dangerous expressions of autonomic disease is autonomic hyperactivity, usually caused by a profound sympathetic increase.
Causes of autonomic hyperactivity include acute intracranial lesions (e.g., severe head trauma, hemorrhage, brain stem lesions) [1], spinal cord lesions causing autonomic dysreflexia, peripheral neuropathies (e.g., Guillain-Barré), drugs (intoxications), and alcohol withdrawal [2].
Features of autonomic hyperactivity
-
Fluctuations in
-
Blood pressure
-
Heart rate
-
Respiratory function
-
Body temperature
-
-
May include
-
Agitation
-
Sweating
-
Flushing
-
Piloerection
-
Pupillary dilatation
-
Muscle tone increase
-
Autonomic hyperactivity may mount in severe complications.
Parasympathetic increase, especially acute loss of modulation, might also cause severe or even life-threatening complications (hypotonia or bradycardia, paralytic ileus, or bladder dysfunction). They are much less common but occur in, e.g., patients suffering autonomic dysreflexia or generalized seizures.
Consequences of autonomic hyperactivities are baroreceptor reflex failure, heart rate fluctuations, ECG changes (see Fig. 7.1b, c), cardiac arrhythmias, blood pressure disturbances, chemoreceptor reflex failure, and respiratory complications in variable degrees. The most severe of these complications is the collapse of the cardiovascular function. Apart from measuring blood pressure, heart rate, and oxygenation, blood flow might be already evaluated at bedside (skin color, skin temperature). During intensive care monitoring, invasive circulation measurements are needed. Provocation factors should be avoided.
Provocative factors/triggers
-
Pain including intestinal pain during bowel movement and body manipulation during nursing
-
Tracheal suctioning
-
Catheterization
-
Bladder distention
-
Pressure on the carotid sinus
-
Eyeball pressure
-
Loud and sudden noise
Autonomic hyperactivity needs urgent attention in identifying the lesion site and monitoring the patient.
7.2 Diagnosing Autonomic Involvement
In contrast to autonomic tests presented in Chaps. 2, 3, and 4, autonomic standard investigations are rarely accessible at an intensive care or critical care units. However, these patients are monitored, and several biosignals are of great help in hinting to autonomic disorders.
7.2.1 ECG [3]
The heart frequency is an important biomarker of autonomic dysfunction in intensive care patients. Tachycardia, bradycardia, or arrhythmia indicates sympathetic or parasympathetic overactivity (see Table 7.1). In addition, autonomic innervation of the heart leads to altered ECG morphologies. These include prolonged PQ and QT interval, T wave, and ST and U interval morphologies.
7.2.1.1 Blood Pressure
As discussed in Chaps. 1 and 3, the sympathetic nervous system regulates the arterial vessel constriction. Blood pressure is therefore a strong marker for sympathetic innervation in intensive care patients. This biomarker is best monitored “beat to beat” employing an arterial catheter. In patients with autonomic dysfunction, blood pressure trends might be valuable to monitor autonomic dysfunction.
7.2.1.2 General Management Considerations
Patients with autonomic hyperactivity should be managed at critical care wards including basic monitoring of ECG, temperature, respiratory frequency, continuous blood pressure, fluid balance (eventually invasive), and blood oxygenation.
As soon as the patient is initially stabilized, elaborate evaluation of the condition causing autonomic hyperactivity is necessary to initiate optimal treatment. Pursuing an approach as presented in Table 7.1 might prove valuable to derive an etiologic differential diagnosis.
Even if the condition is already well established at the onset of autonomic hyperactivity (e.g., head trauma, intracranial hemorrhage), reevaluation is mandatory, to exclude secondary complications such as hydrocephalus, drug effects, seizures, increasing brain edema, systemic inflammatory response syndrome (SIRS), or multiple organ dysfunction syndrome.
General management considerations include concise fluid management to maintain euvolemic conditions, exclusion or early treatment of infection, sufficient analgesia or analgosedation if necessary, and focused attention to triggering factors.
7.3 Syndromes
7.3.1 Sympathetic Hyperactivity
-
Autonomic storm is considered in patients suffering extensive activation of the sympathetic nervous system. This activation might have three different pathophysiological mechanisms: sympathoadrenal discharge, Cushing’s response, and end diencephalic “seizures.”
-
Typical signs of sympathoadrenal discharge are hypertension, tachycardia, increased cardiac output, and decreased vascular resistance. Autonomic hyperactivity is caused by increased sympathetic nerve activity due to severe CNS lesions, either with sympathetic neural discharge or excessive adrenal activity.
-
Cushing’s response on the contrary shows hypertension but bradycardia as well as slow irregular breathing. Causes are acute distortion of the lower brain stem or cerebral hematomas.
-
Diencephalic “seizures” are characterized by acute hypertension, tachycardia, pupillary dilatation, and often extensive sweating. The pathophysiology is unclear; there is no convincing evidence for epileptic discharge. Causes might be closed head injuries resulting in a decorticate state or widespread axonal injury.
7.3.2 Specific Syndromes
7.3.2.1 Head Trauma
Paroxysmal sympathetic hyperactivity is a regular complication of head trauma patients. Disconnections involving the posterior corpus callosum and posterior limb of the internal capsule may play a role in the pathogenesis [4]. Paroxysms often start 5–7 days after injury, eventually starting earlier, and follow a regular pattern for several times a day. Diagnosis might be achievable quite early [5]. Each episode may last from less than 1 h to 10 h. It might be present from 1 week to several months. The diagnosis of paroxysmal sympathetic hyperactivity was proposed if four of six criteria are present in the absence of other potential causes [6]:
-
1.
Fever (higher than 38.3 °C)
-
2.
Tachycardia (heart rate more than 120 beats per minute or more than 100 beats per minute if the patient is treated with beta-blocker)
-
3.
Hypertension (systolic blood pressure higher than 160 mmHg or pulse pressure higher than 80 mmHg)
-
4.
Tachypnea (respiratory rate over 30 breaths per minute)
-
5.
Excessive diaphoresis
-
6.
Extensor posturing of extremitiesor severe dystonia
Infection needs to be excluded as well as epileptiform activity in EEG.
In addition to the management as presented later, morphine sulfate is effective to abort ongoing paroxysms.
7.3.2.2 Subarachnoid Hemorrhage
Profound sympathoexcitation is a common finding in subarachnoid hemorrhage [7]. ECG changes may occur, including elevation or depression of the ST segment, inverted or biphasic T waves, QTc prolongation, and even Q waves (see Fig. 7.2a–e). Troponin and creatine kinase might be increased. Abnormalities resolve within 1–4 days, whereas echocardiographic akinesia or hypokinesia might be present for weeks. Tachyarrhythmias are common.
(a–c) CT scan of a patient suffering severe traumatic subarachnoid hemorrhage and subdural frontal hematoma (dominated on the right side): (a) admission, (b) 6 h after admission, (c) 4d after admission. (d–e) ECG: admission (d) and day 5 (e). (f) Coronary angiography 63 minutes after detection of ECG changes, (e) no impeded coronary artery blood flow, no coronary artery disease
Massive release of norepinephrine leads to myocardial damage, leading to subendocardial contraction band necrosis. Coronary artery disease is typically not present (see Fig. 7.2f). Neurogenic pulmonary edema might occur but might also be caused by vascular congestion.
7.3.3 Ischemic Insular Stroke
Strokes within the insular region can trigger excessive sympathetic activity, mounting in myocytolysis and arrhythmogenicity [8]. The lateralization was discussed, but similar complications are caused by strokes regardless of the side. Even more parietal lobe infarctions were identified as an increased risk for cardiac death and myocardial infarction [9, 10].
7.4 Management
Hypertension may be controlled by agents blocking sympathetic action. Alpha-blocker urapidil is valuable to sufficiently control blood pressure, eventually added by beta-blocking agents (e.g., metoprolol, labetalol, esmolol) or agents reducing central sympathetic outflow (clonidine). All those agents are given intravenously but clonidine, which is administered enterally to avoid the initial hypertensive response. Any medication that can increase intracranial pressure (calcium channel blockers, many vasodilators) is contraindicated. Avoid initially any long-acting oral medication as severe blood pressure fluctuations might occur. Reduce external and internal stimuli (pain, loud noises, endotracheal suctioning, or constipation).
Cardiac complications might be prevented by frequent electrolyte screening and early potassium and magnesium replacement if necessary. Sinus tachycardia sometimes might need treatment by beta-blockers as listed above. Cardiac arrhythmias should be treated as recommended in cardiologic guidelines. Atrial fibrillation or flutter may be treated with diltiazem or verapamil or digoxin loading, the latter being given especially in older patients. Amiodarone might achieve pharmacological cardioversion to sinus rhythm in atrial fibrillation but is demanded in sustained ventricular tachycardia. Reflex bradycardia should be avoided. Persisting bradycardia might be treated with atropine. Atrioventricular block second or third grade or recurring asystoles demand placement of a cardiac pacemaker.
7.4.1 Neurogenic Pulmonary Edema
Sudden development makes neurogenic pulmonary edema dangerous. Pulmonary venoconstriction and elevation of left-sided cardiovascular pressures might be contributing factors, as well as myocardial dysfunction. It might lead to profound hypoxemia.
Management
In contrast to cardiogenic pulmonary edema, neurogenic pulmonary edema does not respond well to diuretics, if there is no cardiogenic component in addition. It is best treated by positive end-expiratory pressure and adequate oxygenation. It improves usually within 48 h, with resolution within 4–5 days.
7.4.2 Takotsubo Cardiomyopathy
Takotsubo syndrome is a cardiomyopathy mainly affecting the left ventricle [11]. Characteristic cardiac motion abnormalities are revealed in echocardiogram (transient hypokinesis, akinesis, or dyskinesis of the left ventricular midsegments with or without apical involvement; regional wall motion abnormalities beyond a single epicardial vascular distribution). There are no signs of coronary artery disease or angiographic evidence of acute plaque rupture. ST segment elevation and/or T-wave inversion in the electrocardiogram might mimic myocardial infarction; modest elevation in cardiac troponin might occur [12]. In acute phase, left ventricular ejection fraction might be severely reduced, and congested heart failure might be the consequence. Complete resolution within 2–4 weeks is often observed.
Management
Main management strategies are supportive. There is so far no consensus on pharmacological treatment. Supportive treatment often leads to resolution of the condition. In the initial phase, aspirin or other antiplatelet agents are usually prescribed, although the benefit of this management is not clear. Cardiologic assistance systems are sometimes needed.
7.4.3 Noninfectious Fever
Noninfectious fever should only be suspected in those patients, who have no other causes of infection (including CNS). It occurs in direct lesions of the ventral hypothalamic thermoregulation (e.g., SAH, traumatic brain injury, encephalitis) or autonomic dysfunction in efferent projection to the sweat glands (GBS) or anticholinergic medication.
This is usually only seen in ICU patients, especially with SAH [13].
Management
Antipyretic medication, physical cooling, invasive temperature regulation, eventually blockade of muscle activity.
7.4.4 Complications of Drugs Acting on Dopamine Receptors: Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome is caused by D2 dopaminergic receptor blockade by psychiatric medication or sudden withdrawal of dopaminergic agonists in Parkinson’s disease patients. Patients therefore have a psychiatric or movement disorder history. The risk to develop neuroleptic malignant syndrome is higher in treatment with high-potency antipsychotics (e.g., haloperidol), or antiemetics (metoclopramide), also in atypical antipsychotic drugs (e.g., clozapine, olanzapine, risperidone, quetiapine, etc.) [2, 14]. Around 80% of the patients are under the age of 40, and males are twice as often affected as females. Patients with Lewy body disease might develop neuroleptic malignant syndrome at low antipsychotic doses already. Signs include tachycardia, labile blood pressure, hypersalivation, excessive sweating, fluctuations in the level of consciousness, pyrexia, and severe muscle rigidity. Laboratory evaluations show leukocytosis and elevated creatine kinase levels due to rhabdomyolysis.
Management
Discontinue all antipsychotic medications, and possibly antidepressants, and lithium. Control body temperature by extra- or intracorporeal cooling, and monitor creatine phosphate kinase daily. Hypertension might respond to clonidine, and dantrolene or amantadine might be considered to control muscle tonus. Eventually muscle relaxants are needed such as dantrolene, although conflicting reports exist on the benefit of dantrolene. Benzodiazepine use had been reported, mainly to facilitate muscle relaxation.
7.4.5 Complications of Drugs Acting on Serotonin Receptors: Serotonin Syndrome
Symptoms are dose related and occur after administration of single or a combination of drugs acting on the serotonin receptors, particularly 5-HT2a (serotonin reuptake inhibitors like fluoxetine, paroxetine, sertraline, citalopram, etc.); 5-Ht1 agonists (e.g., triptans); monoamine oxidase inhibitors; opioids, valproate, lithium, antiemetic agents (metoclopramide, ondansetron), and cyclobenzaprine; and a number of drugs such as LSD and ecstasy [2]. Patients usually present in altered mental state (agitation, excitement, confusion) and show excessive profuse sweating, pyrexia, mydriasis, tachycardia, and tachypnea. Neuromuscular hyperactivity including tremor, clonus, myoclonus, and hyperreflexia might be present. Symptoms develop rapidly in 60% within 6 h of medication initiation, change in dosage, or overdosage [14]. In contrast to neuroleptic malignant syndrome in addition to clonus, diarrhea or hyperactive bowel sounds are typical symptoms.
Management
Discontinue all serotoninergic medication. Control body temperature by extra- or intracorporeal cooling. Benzodiazepines might be beneficial for neuropsychiatric signs; eventually consider cyproheptadine, which acts as 5-HT2 antagonist.
7.4.6 Alcohol Withdrawal
Alcohol withdrawal may cause delirium tremens. Symptoms include confusion, anxiety, insomnia, tremor, hallucinations, and fluctuating psychomotor activity and usually appear 2 or 3 days after cessation of drinking. Sympathetic hyperactivity with hypertension, tachycardia, fever, diaphoresis, and flushing occurs [15].
Management
Main treatment options are benzodiazepines, such as lorazepam. Dose should be individualized based on the symptoms. In severe cases, sedation at an intensive care unit is required.
7.4.7 Spinal Lesion: Acute Phase
In acute phase of spinal lesions, patients might suffer spinal shock with autonomic consequences.
Neurogenic shock is observed rather in higher lesions (20% of cervical, 3% of lumbar lesions); signs are reduced blood pressure and reduced heart rate.
Management
Prevent vagal stimulation; prevent hypotonia (might lead to additional ischemia of the myelon); support therapy of bladder, gastric, or bowel atonia.
7.4.8 Spinal Lesion: Autonomic Dysreflexia
Autonomic dysreflexia in chronic stage of a spinal lesion is caused by reorganization of the spinal cord. It develops a month or more after the spinal lesion occurred. Determinants are the severity of the spinal lesion (incomplete or complete) and the level of the lesion, especially in relation to the major sympathetic outflow in lesions above T6. Potential stimuli, e.g., bladder and colonic distention, might induce autonomic activation: sympathetic activation below the level of spinal lesion with vasoconstriction (evident as dry, pale skin) and increased blood pressure. Secondary baroreceptor-mediated parasympathetic response above the lesion results in profuse sweating, piloerection, flushing, and bradycardia. These activations are mild to life threatening.
Management
Prevent stimuli (especially the bladder); in acute hypertension, introduce blood pressure control: e.g., glyceryl trinitrate and nifedipine. In some patients, local anesthetics to the bladder might be considered.
7.4.9 Immune-Mediated Neuropathies: AIDP
In AIDP a number of autonomic complications are encountered. A sensitive early marker for autonomic complications is autonomic sinus tachycardia (> 100 /min). Persistent hypertension is common, likely based on reduced baroreflex function due to afferent neuropathy. Labile blood pressure (> 85 mmHg blood pressure fluctuation within a day systolic) is a prognostic marker for severe bradycardia [16]. Bradycardia occurs spontaneously or on vagal stimulation. Sudomotor changes are common with increased but also decreased sweating, often regional.
Management
Patient with autonomic signs of AIDP have to be monitored. Hypertension should be treated only if sustained or secondary complications are present, due to the danger of labile blood pressure and severe hypotension. Tachyarrhythmias or vagally induced bradycardia might complicate the course. Eventually a pacemaker is needed.
Bladder dysfunction and adynamic ileus are frequent complications.
Take home messages
Autonomic hyperactivities are severe life-threatening conditions, which require intensive management. Treatment is mainly symptomatic, eventually supported with a variable degree of sedation and stimulus deprivation. Stabilization of blood pressure, heart rate, and temperature is a challenge in these patients.
References
Marthol H, Intravooth T, Bardutzky J, De Fina P, Schwab S, Hilz MJ (2010) Sympathetic cardiovascular hyperactivity precedes brain death. Clin Auton Res 20(6):363–369
Low PA, Benarroch EE, editors. Clinical autonomic disorders (2008) 3rd edn. philadelphia: Wolters Kluwer health/lippincott Williams & Wilkins
Sander D, Hilz MJ, Ziemssen T (2008) Autonome störungen. In: Schwab S, Schellinger P, Werner C, Unterberg A, Hacke W (eds) NeuroIntensiv. Springer, Heidelberg, pp 642–660
Hinson HE, Puybasset L, Weiss N, Perlbarg V, Benali H, Galanaud D et al (2015) Neuroanatomical basis of paroxysmal sympathetic hyperactivity: a diffusion tensor imaging analysis. Brain Inj 29:1–7
Hughes JD, Rabinstein AA (2014) Early diagnosis of paroxysmal sympathetic hyperactivity in the ICU. Neurocrit Care 20(3):454–459
Rabinstein AA, Benarroch EE (2008) Treatment of paroxysmal sympathetic hyperactivity. Curr Treat Options Neurol 10(2):151–157
Di Pasquale G, Andreoli A, Lusa AM, Urbinati S, Biancoli S, Cere E et al (1998) Cardiologic complications of subarachnoid hemorrhage. J Neurosurg Sci 42(1 Suppl 1):33–36
Goldstein DS (1979) The electrocardiogram in stroke: relationship to pathophysiological type and comparison with prior tracings. Stroke 10(3):253–259
Hilz MJ, Schwab S (2008) Stroke-induced sudden-autonomic death: areas of fatality beyond the insula. Stroke 39(9):2421–2422
Rincon F, Dhamoon M, Moon Y, Paik MC, Boden-Albala B, Homma S et al (2008) Stroke location and association with fatal cardiac outcomes: Northern Manhattan Study (NOMAS). Stroke 39(9):2425–2431
Yoshikawa T (2014) Takotsubo cardiomyopathy, a new concept of cardiomyopathy: Clinical features and pathophysiology. Int J Cardiol 182C:297–303
Roshanzamir S, Showkathali R (2013) Takotsubo cardiomyopathy a short review. Curr Cardiol Rev 9(3):191–196
Rabinstein AA, Sandhu K (2007) Non-infectious fever in the neurological intensive care unit: incidence, causes and predictors. J Neurol Neurosurg Psychiatry 78(11):1278–1280
Haddad PM, Dursun SM (2008) Neurological complications of psychiatric drugs: clinical features and management. Hum Psychopharmacol 23(Suppl 1):15–26
Mirijello A, D'Angelo C, Ferrulli A, Vassallo G, Antonelli M, Caputo F et al (2015) Identification and management of alcohol withdrawal syndrome. Drugs 75(4):353–365
Pfeiffer G, Schiller B, Kruse J, Netzer J (1999) Indicators of dysautonomia in severe Guillain-Barre syndrome. J Neurol 246(11):1015–1022
Recommended Further Reading
Clinical Autonomic Disorders – Evaluation and Management, ed. Phillip A. Low, Lippincot Ravens; Chapter 47
Acknowledgment
We want to thank Prof. F. Fellner (chair, Insitute for Radiology, Kepler University Hospital Linz) for providing imaging data, Prof. G. Ransmayr (chair) and Dr. F. Gruber (Clinic for Neurology 2) for providing case data, and for providing coronary angiography slides for this book chapter we want to especially acknowledge PD C. Steinwender (chair, Department of Cardiology).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Struhal, W., Lahrmann, H. (2017). Autonomic Hyperactivity Syndromes. In: Struhal, W., Lahrmann, H., Fanciulli, A., Wenning, G. (eds) Bedside Approach to Autonomic Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-05143-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-05143-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-05142-0
Online ISBN: 978-3-319-05143-7
eBook Packages: MedicineMedicine (R0)