Abstract
Endovascular treatment of wide-necked intracranial aneurysms frequently requires stent- or balloon-assisted coiling to prevent coil herniation into the parent artery. Provided that coils can be securely deployed within the aneurysm sac, these adjunctive devices and their associated risk can be avoided. The Penumbra 400 Coil (PC-400) has a larger diameter than conventional coils and is constructed completely of metal, a feature that increases the coil stability and may improve its ability to respect the aneurysm neck. The purpose of this study was to examine the frequency of adjunctive stent usage when coiling wide-necked intracranial aneurysms with the PC-400 in comparison with conventional coils. We examined consecutive patients with unruptured wide-necked aneurysms treated at our institution with endovascular coils. Aneurysm characteristics and procedural outcomes were compared between patients treated with PC-400 compared with a control group treated with conventional coils. Thirty-eight patients met criteria for this study. Stent-assisted coiling was required in 34 % fewer cases using PC-400 compared with conventional coils (P = .049). Fewer coils and less length were required with the PC-400 to obtain the same packing densities, occlusion types, and short-term stability. This may reduce treatment cost and prove to be valuable in patients with contraindications to dual antiplatelet therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Coil embolization has become the leading treatment modality for intracranial aneurysms. However, this technique can be particularly challenging for wide-necked aneurysms, often requiring neck remodeling to provide a mechanical scaffold that prevents coil herniation into the parent artery [5]. Adjunctive balloon assistance or stent placement can accomplish this feat, but not without increased risk of procedural complications and long-term morbidity [1, 3, 10, 12].
Balloon-assisted coiling is one adjunctive technique used to maintain arterial lumen patency during coil placement in wide-necked aneurysms and provides the benefits of avoiding a stent and the need for long-term antiplatelet agents. Disadvantages of balloon assistance include the possibility of aneurysm or parent artery rupture and repeated episodes of cerebral ischemia during balloon inflation, thromboembolic events, and coil migration into the parent artery after deflation. There are mixed reports regarding the safety of balloon remodeling for wide-necked aneurysms; some reveal no increased adverse events whereas others demonstrate a high complication rate and advise against its use when possible [7, 8, 12, 13].
Stent-assisted coil embolization of wide-necked aneurysms increases the risk of procedural complications as well, specifically, of thromboembolic occlusions, stent migration, vessel wall injury, delayed thromboembolic events, and in-stent stenosis [1, 3]. Dual antiplatelet therapy is recommended for at least 6 weeks to minimize the delayed complications, but their use introduces the higher risk of a new set of potential bleeding problems [14, 15].
Provided that a coil can be securely deployed into the sac while respecting the aneurysm neck–parent artery interface, the additional risk from adjunctive remodeling can be eliminated from the treatment of wide-necked aneurysms. Presumably, a coil construct that is more stable, such as that seen with the Penumbra Coil 400 System (PC-400) (Penumbra, Inc., Alameda CA, USA), may be better able to respect the aneurysm neck than conventional coils.
PC-400 coils are designed with a larger outer diameter (0.020″) than most conventional coils (e.g., 0.010″ for GDC 10) (Fig. 1). Conventional coils are constructed with a nonmetallic polymer, whereas the PC-400 is designed with three layers of metal providing a more robust and sturdier construct (Fig. 2). The innermost layers of the PC-400 coils are composed of Nitinol wire, a memory-shape material designed to resist the stress of hemodynamic forces encountered within the aneurysm sac. This added resistance to mechanical stressors purportedly prevents coil compaction after placement and promotes coil loop stability within the aneurysm sac. This latter coil characteristic may provide the additional advantage of stabilizing the coils securely on the shoulders of the aneurysm neck to prevent herniation into the parent artery, thus avoiding the need for adjunctive remodeling and stent placement. Despite the physical properties of these completely metallic coils, we hypothesized that there would be no difference in adjunctive stent usage for wide-neck aneurysms between those treated with the PC-400 system and those occluded with conventional coils.
Methods
Approval was obtained from the Institutional Review Board of our university for this study. We retrospectively collected data from consecutive patients with unruptured intracranial aneurysms with a wide-neck (≥4-mm neck or dome:neck ratio <2:1) treated by the senior author (EMD) between October 2008 and December 2012. Patients were divided into two groups based on the choice of endovascular coils: (1) PC-400 and (2) conventional coils (Cashmere, Micrusphere, DeltaWind, and Ultipaq: Codman & Shurtleff, Inc., Raynham MA, USA; Hydrogel, Cosmos, Complex, and HyperSoft: MicroVention, Inc., Tustin CA, USA). All patients had planned adjunctive stenting with either an Enterprise (Codman & Shurtleff, Inc., Raynham MA, USA) or Neuroform (Stryker Corporation, Kalamazoo MI, USA) intracranial stent. Only unruptured aneurysms were considered in the present analysis because adjunctive stent placement is a rarity after aneurysm subarachnoid hemorrhage where antiplatelet therapy is a relative contraindication.
In our series, the first framing coil was placed into the aneurysm sac and its ability to respect the ostium of the neck was tested to confirm that it would not herniate into the parent vessel before detachment. In the PC-400 group, the stiffer standard coils were typically inserted first to frame the aneurysm so that they would maintain their position within the sac better and minimize the chance of coil loop herniation into the parent vessel. Subsequently, the coils were rapidly downsized and soft or extra-soft PC-400 coils were used to finish the packing to avoid pushing the previous coils out of the aneurysm sac. The initial PC-400 framing coil typically was chosen based on the maximum aneurysm sac diameter, downsizing to the closest loop size that matched the dome because of their more robust nature. Similar techniques were used with the conventional coils, except that the first framing coil was upsized to the closest loop length to secure them against the sac wall; our initial experience demonstrated that when the PC-400 system was chosen in the same manner, the coils were too large and would push out of the aneurysm. In both cases, if the first framing coil herniated into the parent vessel, it was removed and the process was repeated with a larger-sized framing coil and when stent assistance was required, a Neuroform or Enterprise stent was placed across the neck to act as a scaffold for the coil mass according to our standard treatment preferences.
The goal of every coiling was total occlusion of the aneurysm, aneurysm embolization grade (AEG) = A, with stent assistance only when framing coils would not respect the aneurysm neck. The AEG system was used because of its unique angiographic filling characteristics, which have been demonstrated to have predictive value for determining aneurysm sac thrombosis [2, 11]. The filling characteristics include persistent contrast in the aneurysm neck (AEG = B) or dome (AEG = C) in the capillary or venous phase of the angiogram, and emptying of contrast from the aneurysm neck (AEG = D) or dome (AEG = E) during the arterial phase in sync with the parent artery.
Coil insertion was stopped when total occlusion of the aneurysm was achieved or the microcatheter dislodged from the aneurysm neck and could not be accessed again, thus preventing additional coils from being inserted into the sac. An AEG was assigned by the interventionalist based on the flow of contrast material into the aneurysm neck and dome immediately after embolization. The packing density was calculated using AngioCalc (www.angiocalc.com) for all treated aneurysms. The length of coils and aneurysm volume were also used to calculate the total coil length per unit aneurysm volume (cm/mm3). Short-term radiographic occlusion was noted at follow-up imaging typically scheduled 6 months postprocedure. The long-term occlusion durability of the PC-400 is being examined on a larger scale in the Aneurysm Coiling Efficiency Clinical Trial (NCT01465841).
Data were analyzed using SPSS Version 17 (IBM Corporation, Armonk NY, USA). Nominal variables were compared between the PC-400 and conventional coil groups using Fisher’s Exact test. Continuous variables were compared between groups using independent samples t-tests. Two-sided probability values less than .05 were considered statistically significant for all analyses.
Results
Thirty-eight patients (59 ± 14 years) were identified who underwent coil embolization for wide-necked intracranial aneurysms. Fifteen patients were treated with the PC-400 system and the remaining 23 with conventional coils (Table 1). There were no significant differences in neck size or the maximum aneurysm dimension between groups (P = .760 and P = .425, respectively).
Adjunctive Stent
In patients treated with conventional coils, adjunctive stent placement was required in 74 % of the cases (17 of 23). The PC-400 resulted in a significantly reduced need for stent assistance, with only 40 % of the cases (6 of 15) requiring adjunctive stent placement (P = .049).
Initial Occlusion
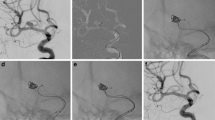
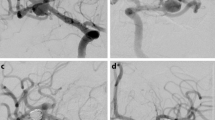
Total occlusion of the aneurysm neck and dome (AEG = A) was noted in 40 % of the PC-400 cases (Fig. 3) and 39 % of the conventional coil cases. Minimal residual dome filling with contrast stasis (AEG = C), suggesting a high likelihood of autothrombosis, was observed in 27 % of PC-400 cases and 22 % of the conventional coil cases. The packing density was not significantly different between PC-400 and conventional coils (P = .379). The number of coils necessary to occlude the aneurysm, total coil length, and length per unit sac volume were all significantly lower for cases treated with PC-400 compared with conventional coils (Table 1). No procedural complications occurred in either group.
Short-Term Follow-Up Occlusion
The mean time at follow-up was 5.3 ± 2.4 months. Stable or improved aneurysm occlusion was noted in 11 (85 %) of 13 patients treated with PC-400 (2 patients were excluded because of lack of imaging). One aneurysm exhibited a significant recurrence with recommended retreatment. Another aneurysm worsened from complete obliteration to a small residual neck with recommended observation rather than treatment. Neither worsened aneurysm was treated with adjunctive stent.
Patients treated with conventional coils exhibited stable or improved aneurysm occlusion in 20 (87 %) of 23 cases. Three aneurysms exhibited significant recurrence with recommended retreatment, two of which were initially treated with adjunctive stent placement. There was no significant difference in occlusion stability between PC-400 versus conventional coils (P = 1.000). Additionally, 2 of 23 patients treated with stent assistance in the conventional coil group demonstrated asymptomatic in-stent stenosis at follow-up.
Discussion
Stenosis and thromboembolic complications associated with the use of neck-remodeling devices increase the risk of treating wide-necked intracranial aneurysms [9]. A retrospective review of 161 patients treated with stent–coil embolization of an intracranial aneurysm documented a procedural morbidity rate of 14.9 %, along with stenosis and thromboembolic complications in 6.8 % of patients [6]. Delayed in-stent stenosis is not a rare occurrence. A review of 156 cerebral aneurysms treated with a Neuroform stent demonstrated stenosis in 5.8 % of patients at follow-up [4]. The stenosis can be symptomatic and may require endovascular treatment or surgical bypass. In addition to delayed complications, Piotin et al. recently reported a large series of 216 patients in which the periprocedural mortality rate in patients treated with adjunctive stent placement was 6.0 %, considerably higher than the 1.2 % in their procedures without stents [10].
For these reasons, avoidance of adjunctive stent usage and balloon assistance is a goal during endovascular treatment of aneurysms at our university. A coil that can respect the geometry of a wide-necked aneurysm without the need for a mechanical scaffold is highly desirable. In this study, the PC-400 was noted to rely less on adjunctive stent placement to secure the coil mass within the aneurysm sac than conventional coils. This may be because of its larger 0.020″ loops and inner Nitinol design, providing more stability of the coil mass within the aneurysm sac.
Techniques that minimize device dependence should be fully explored to minimize the risk and cost of these procedures to patients and health care insurers. Balloon-assisted coil embolization is one such technique that avoids the long-term complications associated with endovascular placement of a permanent metallic device. However, the potential for repeated episodes of cerebral ischemia and arterial wall injury may be increased with this technique and its use is not without controversy [12, 13]. Balloon assistance was not compared in this study because it is not the preferred adjunctive coiling technique at our university and is rarely used for aneurysm treatment.
The Penumbra-Slim microcatheter (0.025″ ID; 2.95Fr Proximal OD; 2.6Fr Distal OD) is recommended for placement of the PC-400 coils and requires a 6F (0.070″ ID) guide catheter. One of the main disadvantages of using the Penumbra-Slim microcatheter through a 6F guide is that the simultaneous use of a balloon catheter or a second microcatheter for stent deployment using the jailing technique is essentially prohibitive with the 0.070″ ID. A larger guide catheter is needed for dual microcatheter use in conjunction with the Penumbra-Slim. Additionally, the larger microcatheter size needed for this coil system may be prohibitive in patients with tortuous cervicocranial vasculature and very narrow-necked aneurysms, increasing the difficulty in accessing the aneurysm. The microcatheter size can also be an impediment when trying to access individual lobes of a multilobulated aneurysm or when trying to cross a stent wall for aneurysm access.
An additional finding in this study was that there was no significant difference between immediate postembolization packing densities and filling characteristics between the PC-400 and conventional coil systems. Despite the packing densities being similar, the total coil length and number of coils was significantly lower with the larger diameter PC-400 coil system. Short-term follow-up was included in the present study and demonstrated no significant difference in occlusion stability between PC-400 versus conventional coils. Long-term occlusion durability is being examined in the Aneurysm Coiling Efficiency Clinical Trial (NCT01465841) and will ultimately be important when evaluating the performance of the PC-400 system.
The limitations of this study include the small sample size, single interventionalist, and retrospective examination. However, limiting the results to a single interventionalist reduces technique variation and results in consistent procedural decisions across all cases.
Conclusion
Embolization of wide-necked aneurysms with the PC-400 system required significantly less stent assistance, fewer coils, and shorter coil length than conventional coils, resulting in similar short-term angiographic outcomes. This may reduce treatment cost and prove to be valuable in patients with contraindications to dual antiplatelet therapy.
References
Akpek S, Arat A, Morsi H, Klucznick RP, Strother CM, Mawad ME (2005) Self-expandable stent-assisted coiling of wide-necked intracranial aneurysms: a single-center experience. AJNR Am J Neuroradiol 26(5):1223–1231
Deshaies EM, Adamo MA, Boulos AS (2007) A prospective single-center analysis of the safety and efficacy of the hydrocoil embolization system for the treatment of intracranial aneurysms. J Neurosurg 106(2):226–233
Fiorella D, Albuquerque FC, Han P, McDougall CG (2004) Preliminary experience using the Neuroform stent for the treatment of cerebral aneurysms. Neurosurgery 54(1):6–16; discussion 16–17
Fiorella D, Albuquerque FC, Woo H, Rasmussen PA, Masaryk TJ, McDougall CG (2006) Neuroform in-stent stenosis: incidence, natural history, and treatment strategies. Neurosurgery 59(1):34–42; discussion 34–42
Jabbour P, Koebbe C, Veznedaroglu E, Benitez RP, Rosenwasser R (2004) Stent-assisted coil placement for unruptured cerebral aneurysms. Neurosurg Focus 17(5):E10
Kanaan H, Jankowitz B, Aleu A et al (2010) In-stent thrombosis and stenosis after neck-remodeling device-assisted coil embolization of intracranial aneurysms. Neurosurgery 67(6):1523–1532; discussion 1532–1533
Layton KF, Cloft HJ, Gray LA, Lewis DA, Kallmes DF (2007) Balloon-assisted coiling of intracranial aneurysms: evaluation of local thrombus formation and symptomatic thromboembolic complications. AJNR Am J Neuroradiol 28(6):1172–1175
Lefkowitz MA, Gobin YP, Akiba Y, Duckwiler GR, Murayama Y, Guglielmi G, Martin NA, Viñuela F (1999) Balloon-assisted Guglielmi detachable coiling of wide-necked aneurysms: Part II – Clinical results. Neurosurgery 45(3):531–537; discussion 537–538
McDonald JS, Norgan AP, McDonald RJ, Lanzino G, Kallmes DF, Cloft HJ (2012) In-hospital outcomes associated with stent-assisted endovascular treatment of unruptured cerebral aneurysms in the USA. J Neurointerv Surg. doi:10.1136/neurintsurg-2012-010349
Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, Moret J (2010) Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke 41(1):110–115
Singla A, Villwock MR, Jacobsen W, Deshaies EM (2012) Aneurysm embolization grade: a predictive tool for aneurysm recurrence after coil embolization. Acta Neurochir (Wien). doi:10.1007/s00701-012-1554-3
Sluzewski M, van Rooij WJ, Beute GN, Nijssen PC (2006) Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg 105(3):396–399
Soeda A, Sakai N, Sakai H, Iihara K, Yamada N, Imakita S, Nagata I (2003) Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol 24(1):127–132
Toyoda K, Yasaka M, Iwade K et al (2008) Dual antithrombotic therapy increases severe bleeding events in patients with stroke and cardiovascular disease: a prospective, multicenter, observational study. Stroke 39(6):1740–1745
Tumialán LM, Zhang YJ, Cawley CM, Dion JE, Tong FC, Barrow DL (2008) Intracranial hemorrhage associated with stent-assisted coil embolization of cerebral aneurysms: a cautionary report. J Neurosurg 108(6):1122–1129
Conflict of Interest Statement
Dr. Eric Deshaies consults for MicroVention Inc., Covidien Neurovascular, Integra LifeSciences Corporation, and McKesson Health Solutions.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Villwock, M.R., Singla, A., Padalino, D.J., Deshaies, E.M. (2015). The Penumbra Coil 400 System for Treatment of Wide-Necked Intracranial Aneurysms: Initial Single-Center Experience. In: Fandino, J., Marbacher, S., Fathi, AR., Muroi, C., Keller, E. (eds) Neurovascular Events After Subarachnoid Hemorrhage. Acta Neurochirurgica Supplement, vol 120. Springer, Cham. https://doi.org/10.1007/978-3-319-04981-6_33
Download citation
DOI: https://doi.org/10.1007/978-3-319-04981-6_33
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-04980-9
Online ISBN: 978-3-319-04981-6
eBook Packages: MedicineMedicine (R0)