Abstract
The recognition of secondary etiologies is critically important to all those treating patients with headaches.
Secondary headaches occur in close temporal relation to another disorder, or there is evidence of a causal relationship. Secondary headache, by definition, should improve or go away within 3 months spontaneously or after successful treatment of the cause.
While the International Classification of Headache Disorders, third edition (ICHD-3) lists nine different classifications of secondary headaches, this clinically focused chapter delves into recognizing red flags, when to order neuroimaging and appropriate laboratory testing, as well as other workup.
Post-traumatic headaches must start within 7 days of precipitating trauma and are most often associated with milder headache and neck trauma. They can bring about a syndrome of symptoms frequently best treated with a multidisciplinary plan.
Vascular headaches are those associated with ischemia, vasculitis, hemorrhage, or alteration in brain circulation. While stroke, aneurysm, and transient ischemic attack (TIA) are considered first, other genetic and mitochondrial abnormalities can result in serious and progressive secondary headache disorders.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Secondary headaches
- Post-traumatic headaches
- Vascular headaches
- Stroke headaches
- Diagnosis headaches
- Diagnostic headache workup
Introduction
Headaches attributable to another disorder are classified as secondary headaches .
If during the investigation, no underlying disorder or disease process can be identified, the headache is then considered a primary headache.
The most common primary headache disorders include migraine, tension-type headache, and cluster headache. Although primary headaches are what are most often encountered in clinical practice, concern for secondary causes often requires that the clinician initiate an appropriate investigation with laboratory and neuroimaging studies.
There are numerous causes of secondary headaches , classified into eight groups by the International Classification of Headache Disorders, 3rd edition, beta version (ICHD-3); see Table 6.1). In order to cover the investigation and treatment of secondary headaches, two chapters have been set aside. Chapter 6 covers the basics of when to work up the possibility of secondary headaches, and also examines headaches stemming from head and neck trauma and vascular disorders. Chapter 7 covers secondary headaches caused by nonvascular disorders. Chapter 7 will also review those headaches not considered to be a primary headache disorder which are classified under painful cranial neuropathies, other facial pains, and other headaches.
Diagnostic Criteria for Secondary Headaches
By definition, either a secondary headache must be in close temporal relation to another disorder or there is evidence of a causal relationship (Table 6.2). Patients may present to the emergency department when a new headache is acute in onset or seek outpatient evaluation when the headache is subacute or chronic .
It is easier to establish causation in acute onset headaches, but less so in those that are in a chronic pattern. Secondary headaches often lack defining features or may have characteristics that overlap with primary headaches. Causative disorders may also change the frequency or pattern of headache in an individual known to have a primary headache disorder. This can make the diagnosis of secondary headache challenging. Previously, the ICHD-2 criteria specified that the diagnosis of a secondary headache could be made only if the headache improved or remitted within 3 months of treatment of the causative factor. This stipulation is no longer required for diagnosis with the ICHD-3 .
Clinical History of Secondary Headaches
Some patients with secondary headache have a preexisting history of primary headaches . Therefore, clinicians must be vigilant for any change in pattern, character, or overall worsening of the patient’s headaches, as this may suggest a new secondary etiology.
Obtaining a detailed headache history is essential in the evaluation of secondary headaches. It is important to know whether the onset was preceded by an unusual event or provocation, whether there is a trend in pain intensity since onset, duration, associated symptoms, and particularly any reported focal neurological deficits . A workup is warranted in patients whose clinical history raises red flags or is atypical. As previously mentioned in Chap. 1, a useful mnemonic created by Dr. David Dodick for identifying red flags is “SNOOP” (Table 6.3) .
Diagnostic Testing
Many patients, particularly those presenting with an episodic occurrence of a typical primary headache, do not warrant further investigation if their physical and neurological examinations are normal and no red flags are elicited in the history. Fortunately, less than 5 % of the patients presenting to the emergency department or physician’s office with headache will be found to have significant underlying causative pathology. The majority of those pathological diagnoses are found in older individuals. In the pediatric population, it is even more unlikely to find an intracranial tumor as a cause of headache in the absence of any focal neurological signs or symptoms. Only a small percent of chronic headache suffers, ~ 1 %, will have significant findings on neuroimaging. Despite the relatively low odds of finding such pathology, clinicians still have to determine which patients, presenting with de novo or persistent headache, warrant investigation to uncover potentially treatable headache etiologies.
Some patients are so disabled by fear that a serious cause underlies their headache that investigation is appropriate to relieve their concerns. There are various medicolegal and managed care constraints that also influence ordering of diagnostic tests. Patients reporting typical common headache characteristics along with demonstration of a normal neurological examination may simply be reassured that the likelihood of finding an intracranial abnormality of significance, with imaging testing, is similar to the general population. The American Academy of Neurology (AAN) has published practice parameter guidelines for nonacute headache neuroimaging (Table 6.4) and the American College of Emergency Physicians (ACEP) has published recommendations for acute headache imaging (Table 6.5). These guidelines along with the clinician’s clinical judgment can be helpful in deciding which patients warrant further testing.
Diagnostic tests generally include imaging such as computed tomography (CT) or magnetic resonance imaging (MRI), and/or lumbar puncture (LP), and laboratory studies. Although routine blood tests are generally not useful in headache diagnosis , many clinicians order a baseline complete blood count (CBC) and chemistry profile (CMP) to include renal and liver function tests, along with a thyroid-stimulating hormone (TSH). Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are useful to exclude the diagnosis of giant cell arteritis (GCA) in patients aged 50 years and above. Other laboratory tests which may be helpful depending on the clinical situation are listed in Table 6.6.
MRI is the imaging study of choice in most instances because of its increased sensitivity in detecting pathology, as well as its higher resolution for normal structures. MRI with gadolinium is advised when there is concern for an inflammatory or infectious process, brain tumor, demyelinating disease, or low cerebral spinal fluid headache. However, in the acute/emergency setting, or if contraindications to MRI exist, CT is still useful and will detect most abnormalities that cause headache. Conventional cerebral angiography remains the best diagnostic tool for central nervous system vasculitis or for patients with subarachnoid hemorrhage (SAH). MR angiography/venography (MRA/MRV) and CT angiography/venography (CTA/CTV) are useful for detecting vascular lesions such as arterial stenosis, dissection, thrombosis, reversible cerebral vasoconstriction syndrome (RCVS), and aneurysm. CTA has a higher sensitivity than MRA in detecting cerebral aneurysms. When lesions are identified that require serial monitoring with repeat imaging, MRI is the preferred method due to risk of repeated radiation exposure with CT.
Electroencephalography (EEG) is only recommended in patients with headache who also report symptoms that may be suggestive of a seizure. EEG is no longer indicated in the routine evaluation of headache as a means to exclude a structural lesion.
In patients presenting to the ER with sudden-onset, severe headache and a negative noncontrast head CT scan result, LP should be performed to rule out SAH. The timing of the LP is important when interpreting results, as results may be falsely negative when performed within 12 h of onset of bleeding. Patients with signs of meningeal irritation should undergo an LP to exclude meningitis/encephalitis. As a general rule, cerebrospinal fluid (CSF) white blood cells (WBCs) should be less than 5, with 1 additional WBC allowed for each 700 red blood cells (RBCs) in the case of a traumatic tap. CSF protein is also elevated in the presence of RBCs, with an increase of 1 mg/dL for every 750 RBCs. CSF glucose should be two-thirds of serum glucose level.
Headache Attributed to Trauma or Injury to the Head and/or Neck
Following trauma to the head or neck, it is not uncommon for patients to report the onset of new headache. Headache attributed to trauma or injury to the head and/or neck may be associated with mild, moderate, or severe head injury, whiplash-type injuries, as well as following craniotomy. Traumas may worsen preexisting headache conditions. Post-traumatic headache (PTHA) is frequently associated with other somatic, psychological, and cognitive symptoms which are referred to as post-concussion syndrome or post-traumatic syndrome in those who did not suffer a concussion (Table 6.7). PTHA and concussion are covered more extensively in Chap. 24, but will be discussed briefly here.
The risk for developing PTHA and post-concussion syndrome seems to be inversely related to the severity of head injury. Other risk factors include female gender, prior known headache disorder, as well as history of psychiatric disease. The mechanism and pathophysiology behind PTHA and this post-concussion syndrome is not well understood. It is likely that axonal injury along with changes in brain metabolism and blood flow can contribute to PTHA, particularly in individuals with a genetic predisposition or premorbid conditions. Recent scientific evidence with more sophisticated imaging has demonstrated structural abnormalities to the brain even with minor head injuries.
Acute headache attributed to trauma or injury to the head and/or neck by ICHD-3 beta definition occurs within 7 days of the head or neck trauma (or within 7 days of when the patient regains consciousness or is able to feel pain and report it), and resolves within 3 months. Persistent headache attributed to trauma or injury to the head and/or neck is diagnosed when the headache following injury fails to resolve after 3 months’ time. This was previously referred to as chronic PTHA . The post-traumatic headaches are also classified according to the severity of injury, mild, moderate, or severe. Cases in which headache onset is delayed greater than 7 days following injury should be noted as such by the clinician.
Clinical features of PTHA are not specified by the ICHD-3 beta, and are similar to the primary headache disorders, most frequently tension-type headache. Patterns similar to migraine, cluster headache, cervicogenic headache, and a variety of other headache types have been noted as well. These patients are at risk of medication-overuse headache (MOH), and development of this secondary etiology should be considered in persistent cases. The role that litigation or malingering plays in persistence of symptoms is still undetermined.
Headaches Associated with Vascular Disease
Headache is a relatively common symptom in a variety of underlying cerebrovascular diseases (Table 6.8) . Intracranial hemorrhages are most often associated with an abrupt onset of severe headache, termed “thunderclap” headache. Thunderclap headache is defined as a severe headache reaching maximal intensity within seconds to a minute. Headaches may be a consequence of stroke, particularly hemorrhagic infarction. Migraine is also a known risk factor for stroke or vascular dissection.
Headache-Attributed Stroke and Transient Ischemic Attacks
Headache may be reported in 10–30 % of patients presenting with an acute ischemic stroke and less commonly in transient ischemic attacks (TIAs) . Distinguishing the focal neurologic deficit of a TIA from a migraine aura can be challenging. Deficits associated with a TIA are sudden in onset versus those related to a migraine aura, which tend to develop over 15–20 min. Headaches can also occur in association with strokes related to large-vessel atherothrombotic disease, cardioembolism, and to a lesser extent small-vessel atherothrombotic disease resulting in lacunar infarcts (Table 6.9).
The symptoms of TIA-related headache may develop just prior to or concurrent with the development of focal neurologic deficits. There are no defining characteristics of the headache associated with ischemia, but they tend to be of moderate intensity.
Ischemia in the distribution of the posterior circulation is more likely to produce headaches than ischemia involving the anterior circulation. The headache pain is often unilateral, occurring on the same side of the stroke. A stroke patient who develops progression of neurologic deficits along with new-onset headache must be reevaluated for hemorrhagic transformation of the area of ischemia (Table 6.10) .
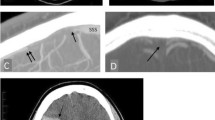
Headache Attributed to Intracranial Hemorrhage
For patients presenting with acute focal neurologic deficits consistent with a stroke pattern, the concurrent report of sudden headache raises great concern for the presence of an intracranial hemorrhage (ICH). Indeed, headache is reported in up to 70 % of patients diagnosed with ICH. The headache is most severe on the day of onset, localized to the side of hemorrhage, and tends to resolve with clinical improvement. Hemiparesis and decreased consciousness are associated clinical findings. Hypertension and advanced age are the two most significant risk factors for ICH. Headaches associated with ICH are more severe in nature than those associated with ischemic stroke.
Headache Attributed to Subarachnoid Hemorrhage (SAH)
Patients with subarachnoid hemorrhage (SAH) usually present with the sudden onset of “the worst headache of my life” or thunderclap headache. Thunderclap headache was covered in Chap. 3, but because of its importance and the frequency with which it is a secondary and not a primary headache, it is reviewed again here. The headache may be associated with alteration of consciousness, vomiting, photophobia, drowsiness, agitation, or neck stiffness. In 50 % of patients, an unruptured aneurysm may produce a warning headache referred to as a sentinel headache. Sentinel headaches occur in the days to weeks prior to aneurysm rupture.
Although thunderclap headache is the classic presentation of rupture of a saccular aneurysm resulting in SAH, many other diagnoses can have an abrupt presentation as well (Table 6.11). Diagnosis is confirmed by an emergent CT and/or lumbar puncture. Cerebral angiography is usually needed to identify the source of the hemorrhage (Table 6.12).
Spontaneous SAH occurs when aneurysms reach 7–10 mm in size. Aneurysmal rupture increases in risk with age, with a mean incidence of 50 years, and rarely occurs before 20 years of age. SAH is considered a neurosurgical emergency with a high morbidity and mortality rate. A high index of suspicion is required to avoid misdiagnosis, which has been reported to occur in as much as 25–50 % of patients.
Giant Cell Arteritis (GCA)
Giant cell arteritis (GCA), formerly known as temporal arteritis, is a vasculitis of large- and medium-sized arteries that affects the elderly. The inflammation predominantly involves extracranial branches of the carotid artery, especially the temporal artery.
GCA exclusively occurs in individuals over the age of 50 years, and the incidence increases with age. Women are more likely to be affected than men. It is rare in African-Americans.
Classical symptoms of GCA include headache, scalp tenderness, jaw claudication, and visual loss if untreated. An elevated ESR (> 50 mm/h) is suggestive of the diagnosis, and the ESR is rarely normal, most often early in the disease (Table 6.13). Transcranial Doppler ultrasonography may be useful in confirming the diagnosis, but temporal artery biopsy remains the gold standard for diagnosis.
Some patients with GCA have myalgias consistent with the related inflammatory disorder, polymyalgia rheumatica. Prompt treatment with corticosteroids for GCA can prevent permanent visual loss which is the result of anterior ischemic optic neuropathy. The headache associated with GCA will dramatically improve or resolve within 3 days of high-dose steroid treatment.
Primary Angiitis of the Central Nervous System (PACNS) and Reversible Cerebral Vasoconstriction Syndrome (RCVS)
Primary angiitis of the central nervous system (PACNS) is a rare form of central nervous system (CNS) vasculitis. Common presenting symptoms include headache along with altered mental status. It is not uncommon for patients to go undiagnosed for 6 months or more due to the fact that other focal neurologic signs are less common at onset. Situations that should trigger consideration and possible investigation for possible PACNS would include multiple infarcts in different vascular territories, headache associated with cognitive changes, and chronic aseptic meningitis (Table 6.14).
This condition typically affects males over the age of 50 years. In contrast to other primary systemic vasculitides, serologic markers of inflammation are typically normal. MRI of the brain may demonstrate nonspecific white matter changes. CSF studies may also be nonspecific, revealing a modest elevation in total protein as well as a modest lymphocytic pleocytosis. Conventional angiography may be useful in diagnosing by demonstrating “beading” as evidence of segmental arterial narrowing, but confirmatory diagnosis with leptomeningeal and brain biopsy is often necessary. Once diagnosis is confirmed, immunosuppressive treatment is initiated with either corticosteroids and/or cyclophosphamide.
Reversible cerebral vasoconstriction syndrome (RCVS) is a syndrome that can be difficult to distinguish from primary CNS angiitis, because presenting signs and symptoms are similar. Angiography in both disorders demonstrates segmental narrowing but in RCVS this is related to vasospasm. Imaging of brain parenchyma can be normal in RCVS, but when infarcts occur, they are typically larger than those as a result of PACNS. Intracranial hemorrhage can be associated with RCVS but is not typical of PACNS. The correct diagnosis is critical, because RCVS patients are treated with calcium channel blockers, and CNS angiitis is often treated with cytotoxic therapy. The outcome is more favorable for RCVS (Table 6.15).
Cerebral Venous Thrombosis
Thrombosis within the cerebral venous system most often is associated with a headache that is acute to subacute in onset. The headache pain is generally described as severe, diffuse, and constant in nature, but has occasionally been described as thunderclap in onset. The headache is worsened by recumbency or Valsalva-type maneuvers such as coughing or sneezing.
This disorder typically affects children or young adults, and women much more frequently than men (Table 6.16). Obstruction of the venous sinuses results in intracranial hypertension and thrombosis. This may eventually lead to venous infarctions which tend to undergo hemorrhagic transformation. Focal neurologic signs, encephalopathy, or seizures commonly accompany the onset of headache.
Patients with cortical vein thrombosis may present very similarly to idiopathic intracranial hypertension (pseudotumor cerebri, IIH) with signs and symptoms of dizziness, tinnitus, diplopia, and visual obscurations. Papilledema may be found on examination.
Risk factors for cortical vein thrombosis include hypercoagulable states, pregnancy, use of oral contraceptives and dehydration. Venous thrombosis may be diagnosed through MRV or CTV. The recommended duration of treatment with anticoagulation for cerebral venous thrombosis is 6 months. However, the headache generally resolves within 1 month of the initiation of treatment.
Headache Attributed to Carotid or Vertebral Artery Pain
Spontaneous dissection of the vertebral or carotid artery may produce head pain. The diagnosis should be considered in individuals reporting new onset of head pain along with neck pain. Clinical suspicion should be raised if the patient endorses a recent history of known provocative factors such as chiropractic adjustment, severe vomiting, and neck trauma including whiplash-type injuries. Patients with collagen vascular disease or fibromuscular dysplasia are at particular risk. The headache tends to be ipsilateral to the side of dissection (Table 6.17).
Location of pain is frontal for carotid dissections and more occipital for vertebral dissections. Carotid artery dissection may manifest clinically with a Hornerʼs syndrome or amaurosis fugax. Vertebral artery dissection may produce vertebrobasilar symptoms, especially a Wallenberg syndrome (difficulty with swallowing, hoarseness, dizziness, nausea, nystagmus, gait and balance abnormalities, and sensory and motor deficits, sometimes on opposite sides). Patients should undergo diagnostic evaluation with an MRI/MRA with a fat-saturation protocol, CT angiogram, or conventional angiography, which will also help identify secondary complications such as stroke or pseudoaneurysm formation.
Headache has been reported following carotid endarterectomy, carotid clipping, and other endovascular procedures including angioplasty, coiling, embolization, and stenting. The headache begins in the first few days after surgery but often resolves within the month of onset.
Post-carotid endarterectomy headache follows three pain patterns unilateral and ipsilateral to the side of surgery:
-
1.
Diffuse mild pain
-
2.
Cluster headache-like pain
-
3.
Severe and pulsating pain
Preexisting headache conditions may be a risk factor for these post-procedural headaches. The mechanism can be related to a hyperperfusion syndrome following improved blood flow or manipulation of intracranial vessel resulting in activation of the trigeminovascular system.
Pituitary Apoplexy
Pituitary apoplexy is an important syndrome to recognize, as it can be a life-threatening emergency. It is the result of hemorrhage or infarction of the pituitary gland, most often in patients with a pituitary adenoma. Patients report the abrupt onset of a severe headache along with symptoms of vision loss, ophthalmoplegia, and mental status change. Serious complications include adrenal crisis, coma, and even death. MRI is the most sensitive imaging study for detection of pituitary apoplexy (Table 6.18).
Conclusions on Diagnosis of Secondary Headaches
-
Use the SNOOP mnemonic (Table 6.3) to decide when to workup patients with headache for secondary causes
-
MRI is generally superior to CT in working up secondary headaches
-
Post-traumatic headaches begin within 1 week of the injury, according to the ICHD-3 beta, and have no required clinical features
-
Headaches associated with TIA, stroke, and dissection are usually ipsilateral to the event
-
TIAs can usually be distinguished from migrainous aura by sudden onset, negative features, and briefer duration
-
Always work up headache in the elderly with a sedimentation rate and CRP for GCA
Suggested Reading
Abrams BM. Factors that cause concern. Med Clin North Am 2013;97:225–242.
Baron EP, Moskowitz SI, Tepper SJ, Gupta R, Novak E, Hussain MS, Stillman MJ. Headache Following Intracranial Neuroendovascular Procedures. Headache 2012;52:739–748.
Bigal ME, Lipton RB. The differential diagnosis of chronic daily headaches: an algorithm-based approach. J Headache Pain 2007;8:263–272.
De Luca GC, Bartleson JD. When and how to investigate the patient with headache. Seminars in Neurology. 2010;30:131–44.
Donohoe CD. The role of laboratory testing in the evaluation of headache. Med Clin North Am 2013;97:217–224.
Edlow JA and the American College of Emergency Physicians Clinical Policies Subcommittee. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2008;52:407–36.
Eller M, Goadsby PJ. MRI in headache. Expert Rev Neurother 2013;12:263–273.
Frishberg BM, Rosenberg JH, Matchar DB, et al. Evidence-Based Guidelines in the Primary Care Setting: Neuroimaging in Patients with Nonacute Headache. Available at http://www.aan.com/professionals/practice/pdfs/gl0088.pdf.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorder, 3rd Edition, Beta Version. Cephalalgia 2013;33:629–808.
Ju YE. Abrupt onset of severe headache. Seminars in Neurology 2010;30:192–200.
Lester MS, Liu BP. Imaging in the evaluation of headache. Med Clin North Am 2013;97:243–265.
Mayer CL, Huber R, Peskind E. Traumatic brain injury, neuroinflammation, and post-traumatic headaches. Headache 2013; doi:10.1111/head.12173.
Hajj-Ali, RA, Calabrese LH. Primary angiitis of the central nervous system. Autoimmunity Reviews 2013;12:463–466.
Salvarani C, Pipitone N, Versari A, Hunder GG. Clinical features of polymyalgia rheumatica and giant cell arteritis. Nature Reviews Rheumatology 2012:8:509–21.
Schwedt TJ, Matharu MS, Dodick DW. Thunderclap headache. Lancet Neurol 2006;5:621–631.
Sheftell FD, Tepper SJ, Lay CL, Bigal M. Post-traumatic headache: emphasis on chronic types following mild closed head injury. Neurol Sci 2007;28:S203–S207.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mays, M. (2014). Diagnosis of Major Secondary Headaches 1, the Basics, Head and Neck Trauma, and Vascular Disorders. In: Tepper, S., Tepper, D. (eds) The Cleveland Clinic Manual of Headache Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-04072-1_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-04072-1_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-04071-4
Online ISBN: 978-3-319-04072-1
eBook Packages: MedicineMedicine (R0)