Abstract
A 48-year-old male patient was admitted to the hospital after a scooter-to-car accident. Patient had abdominal pain, the physical and radiological examinations revealed his two lowest ribs broken, the CT scan showed the spleen ruptured. A decision was taken to perform angiographic examination and coiling. On CT-angiography, a blush was seen in the splenic artery, it being coiled successfully on angiography. Patient recovered and went home 3 days later, being stable and having adequate pain treatment. Two months later he was readmitted because of a large mass in the left upper abdomen and abdominal pain. A new angiography revealed a large branch of the short vessels with a blush in the splenic old rupture.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Diagnosis and Indication for Angiography
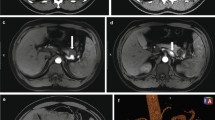
A 48-year-old male patient was admitted to the hospital after a scooter-to-car accident. Patient had abdominal pain, the physical and radiological examinations revealed his two lowest ribs broken, the CT scan showed the spleen ruptured (Fig. 52.1), hemoglobin was low 6.5, and the patient became hemodynamically stable after fluid reposition. A decision was taken to perform angiographic examination and coiling. On CT-angiography, a blush was seen in the splenic artery, it being coiled successfully on angiography (Fig. 52.2a, b). Patient recovered and went home 3 days later, being stable and having adequate pain treatment.
Follow-Up: Identification and Treatment of Complication
Two months later, he was acutely readmitted on to the ward, because of a large mass in the left upper abdomen and abdominal pain. On the CT scan, some sort of splenic fluid collection or cyst of 15 cm was observed that was attached to the inferior aspect of the spleen (Fig. 52.3). Patient was hemodynamically stable, but his hemoglobin was 7.3. A new angiography was performed, and it revealed a large branch of the short vessels going to the splenic old ruptured surface. This was considered the cause for the bleeding and it was subsequently coiled (Fig. 52.4a, b). In retrospect, at the first angiography this short vessel had been seen producing a blush. The next day, the cyst was drained by means of a percutaneous drain, evacuating 1.5 l old blood (Fig. 52.5). After 2 days, the drain was retired and patient could go home.
Discussion
Angiographic coiling is becoming the standard approach for this blunt abdominal trauma. Only those hemodynamic unstable patients who are not reacting to fluid reposition or having associated traumatic lesions should be considered for explorative laparotomy. During angiography, all blush should be coiled. In the present case, only the splenic artery bleeding had been initially coiled, whereas in retrospection also a blush was present at one short vessel. Patient developed a slow bleeding with a hemorrhagic cyst. During the second admission a new angiography showed the bleeding. This was coiled and the cyst percutaneously drained (Illustration 52.1) [1].
Spleen trauma is frequently conservatively treated. CT-angiography scan showing a blush should be treated by angiography and coiling. In the case that patient is hemodynamically unstable and does not react to fluids, surgical approach is indicated. Moreover if multi-trauma patient, surgical treatment of the splenic trauma should be done
Reference
Bhullar IS, Frykberg ER, Siraqusa D, et al. Selective angiographic embolization of blunt splenic traumatic injuries in adults decreases failure rate of nonoperative management. J Trauma Acute Care Surg. 2012;72:1127–34.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lely, R.J., Cuesta, M.A. (2014). Case on Rebleeding After Initial Coiling of Spleen Trauma. In: Cuesta, M., Bonjer, H. (eds) Case Studies of Postoperative Complications after Digestive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-01613-9_52
Download citation
DOI: https://doi.org/10.1007/978-3-319-01613-9_52
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01612-2
Online ISBN: 978-3-319-01613-9
eBook Packages: MedicineMedicine (R0)