Abstract
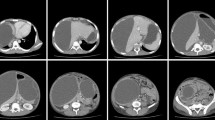
A female patient of 32 years of age (previously presented above in case 45), and who now had been diagnosed with SLE-like autoimmune necrotizing acute pancreatitis that was complicated by several pseudocysts, finally went home after a stay of 6 months at the hospital, largely in the Intensive Care department. During her revalidation period, the patient had developed a mechanical bowel obstruction with important abdominal distension. CT scan demonstrated an increase in diameter of the known pseudocyst in the left abdominal cavity. Three months before, she experienced a short period of blood loss in the feces with significant diarrhea. At that time, we did not dare to perform a colonoscopy because the descending colon was located at the wall of the pseudocyst and the bleeding had no hemodynamic consequences. The patient was then transfused with two erythrocyte concentrated units. At readmission, an MRI showed the pseudocyst with a maximum diameter of 20 by 15 cm in the left abdominal cavity. Because of the mechanical problems caused by the pseudocyst, a decision was taken to drain the cyst by laparotomy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Diagnosis and Indication for Surgery
A female patient of 32 years of age (previously presented above in case 47), and who now had been diagnosed with SLE-like autoimmune necrotizing acute pancreatitis that was complicated by several pseudocysts, finally went home after a stay of 6 months at the hospital, largely in the Intensive Care department. During her revalidation period, the patient had developed a mechanical bowel obstruction with important abdominal distension. CT scan demonstrated an increase in diameter of the known pseudocyst in the left abdominal cavity. Three months before, she experienced a short period of blood loss in the feces with significant diarrhea. At that time, we did not dare to perform a colonoscopy because the descending colon was located at the wall of the pseudocyst and the bleeding had no hemodynamic consequences. The patient was then transfused with two erythrocyte concentrated units. At readmission, an MRI showed the pseudocyst with a maximum diameter of 20 by 15 cm in the left abdominal cavity. Because of the mechanical problems caused by the pseudocyst, a decision was taken to drain the cyst by laparotomy.
Operation
The problem was considered how to drain the pseudocyst far from the stomach. Percutaneous drainage was not considered an option, because of the high chance of recurrence. Through an infraumbilical laparotomy, the pseudocyst was drained (2,300 ml debris was evacuated and cultured), followed by a Roux-en-Y reconstruction at the lowest aspect of the cyst with proximal jejunal loop, and leaving a drain along the anastomosis. An Enterococcus faecalis was cultured and the antibiotic therapy was iv administered.
Postoperative Course: Identification and Treatment of Complication
On the first postoperative day, she had an acute onset of abdominal pain with tenderness, local peritonitis, fever, and drain of cyst content through the drain. Relaparotomy showed a normal anastomosis but leakage of the cystic wall as caused by perforation of the drain. After repair, she recovered and was discharged 1 month after surgery without symptoms. After 6 months, follow-up control showed no recurrence of symptoms.
Discussion
Approximately 75–80 % of the cystic lesions of the pancreas are pancreatic pseudocysts. There is a difference in pathogenesis of the several pseudocysts [1, 2]. The most common etiologies for pancreatic pseudocysts include chronic pancreatitis (40 %), acute pancreatitis, pancreatic trauma, pancreatic duct obstruction, and pancreatic malignancies. Complications of pancreatic pseudocyst include infection, hemorrhage (caused by a leaking pseudoaneurysm of the splenic artery), rupture, gastric outlet obstruction, and biliary obstruction.
A pseudocyst is a localized fluid collection that contains pancreatic enzymes and necrotic tissue. Pseudocysts have a non-epithelialized wall consisting of fibrous and granulation tissue and therefore are distinguished from true cysts with epithelial lining.
Pseudocysts are usually in continuity with the pancreas. Most frequently, the pseudocysts are located in the lesser peritoneal sac behind the stomach. Large pseudocysts may extend beyond the lesser sac and become remote from the pancreas in the area of the paracolic gutters, the pelvis, and the mediastinum. The traditional guidelines for management of larger pseudocysts call for drainage after a 6-week observation period. As a vast majority of the pseudocysts resolve spontaneously, asymptomatic pseudocysts should therefore not be drained. In case of complications or persistent symptoms, pseudocysts should be treated. Pseudocysts can be managed by several types of interventions. Three different types of interventions are available: endoscopic drainage, imaging guided percutaneous drainage, and laparoscopic or open cystogastrostomy or cystojejunostomy (Figs. 48.1, 48.2, and 48.3). When possible, an endoscopic drainage through the stomach is preferred as it provides high success and low complication rates. Feasibility of endoscopic drainage is highly dependent on the anatomy and topography of the pseudocyst, considering the relation with the posterior wall of the stomach and local vessels (see cases 47). In this current case, involving a pseudocyst far from the stomach in the left abdominal cavity, applying an endoscopic procedure, was not an option. Imaging-guided percutaneous drainage may give rise to a significant number of complications such as a high risk of infection, persistent leakage from the drain, and repositioning of the drain. However, percutaneous drainage is useful if the pseudocyst has become infected. The type of surgical procedure to follow depends on the location of the cyst. When a retrogastric cyst is not attached to the stomach, high suspicion for malignant process should be in order. And finally, if the pseudocyst is not in contact with the stomach, a Roux-Y-reconstruction needs to be performed. Generally speaking, an operation of pseudocysts might be complicated by anastomosis leakage, postoperative bleeding, and in some cases a mistaken diagnosis as in cystadenocarcinoma.
So far, no prospective controlled studies have been reported contrasting the different drainage approaches. Several retrospective studies compared these approaches and showed slightly higher morbidity and mortality in the surgical group as compared with endoscopic intervention. Because of the heterogeneity in the groups, these results are not comparable. In addition, there is also an enormous difference in morbidity between emergency operations versus elective procedures. Most important is that the preferred intervention varies particularly on the localization and the surrounding anatomy of the pseudocyst and may also depend on personal expertise. In this case, based on the location and the large size of the pseudocyst, an open cystojejunostomy was the preferred option. Aljarabah et al. published a review study about successful laparoscopic approaches [3]. Again, as there have been no prospective randomized trials, it is very difficult to compare the short- and long-term outcome of laparoscopic versus open procedures.
References
Behrns K. Surgical therapy of pancreatic pseudocysts. J Gastrointest Surg. 2008;12:2231–9.
Aghdassi A, Mayerle J, Kraft M, et al. Diagnosis and treatment of pancreatic pseudocysts in chronic pancreatitis. Pancreas. 2008;36:105–12.
Aljarabah M, Ammori BJ. Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series. Surg Endosc. 2007;21:1936–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Vehmeijer-Heeman, M.L.A.W. (2014). Case on Pancreatic Pseudocyst Far from the Stomach. In: Cuesta, M., Bonjer, H. (eds) Case Studies of Postoperative Complications after Digestive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-01613-9_48
Download citation
DOI: https://doi.org/10.1007/978-3-319-01613-9_48
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01612-2
Online ISBN: 978-3-319-01613-9
eBook Packages: MedicineMedicine (R0)