Abstract
A 56-year-old female was evaluated for dysphagia, revealing an adenocarcinoma of the distal esophagus. The patient received neoadjuvant chemoradiotherapy and after a period of 6 weeks he underwent a three stage open transthoracic esophagectomy with a cervical anastomosis. Progressively, the patient developed an important pleura effusion of the left hemithorax on the chest radiography.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Postoperative hiatal herniation
- Esophageal resection
- Esophageal cancer
- Cervical anastomosis
- Esophagectomy
Diagnosis and Indication for Surgery
A 56-year-old female was evaluated for dysphagia, revealing an adenocarcinoma of the distal esophagus. The tumor could not be assessed with endosonography because of luminal stenosis. A CT scan and PET-CT scan stage the tumor as cTxN1M0. The patient received neoadjuvant chemoradiotherapy.
Operation
Subsequently, a three stage open transthoracic esophagectomy with a cervical anastomosis was performed.
Pathology
Radically resected T3N1 adenocarcinoma. Two out of 17 lymph nodes showed metastasis. The circumferential resection margin was 3 mm.
Postoperative Course: Identification and Treatment of the Complication
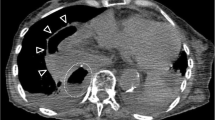
Progressively, during the first two postoperative days, the patient developed an increasing pleural effusion of the left hemithorax on the chest radiograph (Fig. 4.1). A CT scan on the 3rd day revealed a hiatal herniation of the small bowel, renouncing the image on the chest radiograph (Fig. 4.2). A relaparotomy was performed. The bowel was reduced, being vital and a hiatal plasty was performed (Fig. 4.3). The patient could be discharged on the 30th postoperative day.
Discussion
Hiatal herniation is a rare complication after transthoracic esophageal resection for cancer. A report of 355 patients demonstrated an incidence of hiatal herniation of 3.5 % [1]. The median time to diagnosis was 8 months. Another series of 218 patients showed an incidence of hiatal herniation of 4 % of which only 2 % occurred during the first week after surgery [2]. In the case presented above, the hiatal herniation occurred at the third day postoperatively and was associated with intestinal obstruction and strangulation. Radiological assessment such as a chest radiograph and a CT scan are essential in the diagnosis of hiatal herniation, although in this case the chest radiograph was misleading. Management should include reduction of the hernia by laparotomy and approximation of the hiatal defect with—if necessary—a mesh, which is rarely necessary (Illustration 4.1a, b) [2]. An important factor is the enlargement of the hiatus performed during the operation, although this is not a standard procedure in transthoracic esophagectomy compared to transhiatal esophagectomy [3]. Prevention of this complication by narrowing of the diaphragmatic opening and some form of fixation of the gastric conduit to the hiatus may be indicated to avoid this complication. Awareness of its possible occurrence may help prevent the development of intestinal obstruction and strangulation.
References
Vallböhmer D, Hölscher AH, Herbold T, et al. Diaphragmatic hernia after conventional or laparoscopic-assisted transthoracic esophagectomy. Ann Thorac Surg. 2007;84:1847–52.
Schieman C, Grondin SC. Paraesophageal hernia: clinical presentation, evaluation, and management controversies. Thorac Surg Clin. 2009;19:473–84.
van Sandick JW, Knegjens JL, van Lanschot JJ, Obertop H. Diaphragmatic herniation following oesophagectomy. Br J Surg. 1999;86:109–12.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Biere, S.S.A.Y. (2014). Case on Postoperative Hiatal Herniation After Esophageal Resection. In: Cuesta, M., Bonjer, H. (eds) Case Studies of Postoperative Complications after Digestive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-01613-9_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-01613-9_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01612-2
Online ISBN: 978-3-319-01613-9
eBook Packages: MedicineMedicine (R0)