Abstract
Cardiac arrhythmias can be classified into brady- and tachyarrhythmias. Bradyarrhythmias are related to sinus node dysfunction, higher degree AV block, or a combination of these. If reversible causes are ruled out (i.e., myocardial ischemia, concomitant drugs), symptomatic bradyarrhythmias often require implantation of a pacemaker. Tachyarrhythmias are divided into supraventricular (SVT) and ventricular tachycardias (VT). Regular paroxysmal SVTs are mostly related to congenital malformations of the specialized conduction system (accessory or dual pathways) and often can be causally treated by ablation therapy. The most common irregular SVT in clinical practice is atrial fibrillation (AF), which is observed in about 10 % of the elderly population. AF may be highly symptomatic (palpitation, heart failure due to reduced cardiac output) but especially in elderly patients with comorbidities also occurs unnoticed. In patients with AF, the risk for systemic thromboembolism (e.g., stroke) is increased and anticoagulation is mostly warranted. VTs carry an increased risk of hemodynamic compromise and sudden cardiac death. Immediate medical or electrical cardioversion to sinus rhythm is often the therapy of choice and implantation of a cardioverter defibrillator is indicated for high-risk patients. Pathophysiologically, tachyarrhythmias are based on (1) increased automaticity, (2) triggered activity, and/or (3) electrical reentry. Cardiac remodeling is an important predisposing factor for acquired arrhythmias. Cardiomyopathies are often characterized by increased apoptosis, necrosis, and fibrous (scar) tissue infiltration, leading to conduction abnormalities and providing a substrate for reentry as the most common mechanism of acquired arrhythmias. Myocardial heterogeneity in cardiac repolarization is typical for congenital arrhythmias related to genetic ion channel defects (e.g., long QT syndrome) but is also observed in cardiac remodeling. Ectopic (premature) beats do occur in healthy hearts but are more common in diseased hearts where they can trigger sustained arrhythmias based on the pathological myocardial substrate. Cytosolic Ca2+ and Na+ overload as it occurs in cardiomyocytes during ischemia and in heart failure can be aggravated by neurohumoral/sympathetic activation and promotes triggered premature beats (afterdepolarizations). Current antiarrhythmic therapy is mainly aimed to reduce sympathetic activation (beta-blockers), Na+ or Ca2+ influx (class I and IV antiarrhythmics), or prolonged repolarization (class III), with the most potent antiarrhythmics acting as multichannel blockers. New therapeutic approaches comprise drugs with (atrial) tissue selectivity and new targets (Ca2+ stabilizers, upstream therapy).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ion channels
- Reentry
- Afterdepolarizations
- Triggered activity
- Automaticity
- Sudden cardiac death
- Atrial fibrillation
- Ventricular tachycardia
- Substrate
- Trigger
- Antiarrhythmic
- Beta-blockers
- Long QT syndrome
- Myocardial remodeling
4.1 Cardiac Rhythm
In the heart, electrical activation of the cardiac myocytes triggers contraction in a calcium-dependent process termed excitation contraction coupling. As established by Henry Pickering Bowditch in 1871, cardiac (unlike skeletal) muscle follows the all-or-nothing principle, indicating that local electrical activation will induce contraction of the whole heart. In the healthy heart, activity of the sinus node determines the rate of electrical activation and thus contraction of the heart. Importantly, electrical activation of the heart goes beyond rhythmic impulse generation, as timely electrical activation of the atria and synchronous activation of the ventricles determine the efficacy of the heart as a pump and depend on the sequential activation of fast and slow conduction in myocardial tissue. Organized electrical activation is observed in the embryonic stage long before the heart has differentiated into its final shape emphasizing the role of differential electrical conduction system in the heart’s development and function (Van Mierop 1967). However, in cardiac remodeling, altered electrical conduction in the diseased ventricle is the most common cause for regional short circuits (reentry tachycardias, see Sect. 4.6.3) that dominate heart rate.
Cardiac arrhythmias represent a transient or persistent disturbance in cardiac rhythm. Initiation of arrhythmias is often the result of an individual predisposition and an acute triggering event (Fig. 4.1).
4.2 Regular Heart Rate
Physiologically, cardiac rhythm originates from specialized cardiac cells located in the sinus node (primary pacemaker). As opposed to the vast majority of cardiac myocytes (“working myocardium”), these pacemaker cells are able to spontaneously generate action potentials. The pacemaking mechanism involves the interplay of several sarcolemmal ion channels (including the selectively expressed pacemaking “funny” current, I f) as well as intracellular Ca2+ cycling (“Ca2+ clock,” Lakatta et al. 2010), resulting in a slow depolarization during the resting phase (phase 4) of the action potential (Fig. 4.2).
Heart rate during sinus rhythm is in the range of 60–100/min at rest and is modulated by the sympathetic and parasympathetic nervous system. In trained individuals, sinus rhythm with lower heart rates at rest (between 40 and 60/min) may be physiologic. In case of inability of a diseased sinus node to generate an electrical pulse (as in sick sinus syndrome), cells from the specialized electrical conduction system of the heart, i.e., the atrioventricular junctional cells (secondary pacemaker) or His-Purkinje system (tertiary pacemaker), and even working myocardium can trigger heartbeats, albeit at successively lower rates (escape rhythms).
Heart rate is modulated by the autonomic nervous system, with vagal influence dominating at rest. Increased heart rate at rest (>80–85/min) is associated with increased morbidity and mortality in population-based trials and represents an independent risk factor in patients with arterial hypertension, ischemic cardiac remodeling, and also pulmonary disease. Experimentally, increased resting heart rate induces maladaptive myocardial as well as vascular remodeling (Custodis et al. 2010). Lowering resting heart rate to values below 70/min, either by beta-adrenoceptor antagonists or by selective blockade of the I f current (ivabradine), reduces morbidity and mortality and has evolved to an established therapeutic strategy in patients with heart failure and ischemic cardiomyopathy.
Heart rate variability (HRV), i.e., the circadian variability in the beat-to-beat interval, reflects the autonomous control of the heart. In cardiac remodeling and heart failure, a reduction in HRV is associated with increased mortality and an increased incidence of arrhythmias, even though the predictive value of HRV in primary prevention of arrhythmogenic events in clinical practice is limited by the strong influence of confounding comorbidities.
4.3 Classification of Arrhythmias
The classification of arrhythmias in clinical practice is oriented towards the rapid assessment of the associated risk of cardiac arrest and identification of immediate treatment strategies to restore compromised cardiac output. Arrhythmias are divided by rate into bradyarrhythmias (<60/min) or tachyarrhythmias (>100/min), according to the resulting ventricular heart rate. Cardiac arrest defines a state of mechanical inactivity similarly observed during asystole (no ventricular electrical activity) or ventricular fibrillation (chaotic electrical activity).
Arrhythmias are further classified according to their origin: Supraventricular arrhythmias involve ventricular activation via the specialized conduction system of the heart, are usually better tolerated by the patient, and carry a low risk of cardiac arrest. Supraventricular arrhythmias are generally more common than ventricular arrhythmias. Ventricular arrhythmias on the other hand often occur in patients with underlying structural heart disease and imply an abnormal ventricular activation pattern further compromising cardiac function. The risk of sudden cardiac death in ventricular arrhythmias is increased. Arrhythmia duration ranges from single irregular (“premature”) atrial (PAC) or ventricular (PVC) contractions to sustained (>30 s) and incessant/persistent arrhythmias. Arrhythmias can compromise cardiac output as a result of a reduced heart rate (bradyarrhythmias), reduced stroke volume (tachyarrhythmias), and/or a less efficient contraction sequence (ectopy).
4.4 Clinical Manifestation
Patients with arrhythmias usually experience palpitations, often associated with anxiety, dizziness, dyspnea, and sometimes retrosternal discomfort even in the absence of coronary artery disease. Presyncope and syncope (transient loss of consciousness) may occur, if the arrhythmia is associated with hemodynamic compromitation. Arrhythmias with longer duration may manifest in fatigue, exercise intolerance, and overt heart failure. Sudden cardiac death (SCD) is defined as an unexpected death attributed to a cardiac cause that occurs within 1 h of the onset of symptoms. SCD has an estimated risk of 1–2/1,000 in the general population (Zipes 2005), is more common in patients with structural heart disease (see Sect. 4.7.2), and is largely (~80 %) attributed to ventricular arrhythmias. Ventricular arrhythmias associated with an increased risk of SCD (most of them are) are often termed malignant arrhythmias.
4.4.1 Premature Beats
PACs and PVCs are the most prevalent arrhythmias and do not necessarily imply an increased risk for SCD or disease progression. Forty to seventy percent of an otherwise healthy population have one or more PVCs in a 24 h Holter (Kostis et al. 1981; Bjerregaard 1982); almost 90 % have PACs. More than 200 PACs or PVCs/24 h or complex (i.e., repetitive or multiform) extra beats, however, are rarely seen in otherwise healthy individuals (≤5 % of cases, Bjerregaard 1982). Premature beats are the initiating event for reentry tachycardias in predisposed individuals. Single ectopic beats are often asymptomatic. However, the perception of palpitations varies greatly between individuals and is only weakly associated with objective measures of arrhythmia incidence. Thus, as may be expected, patients that tend to somatize more report a higher disease burden with arrhythmias (Barsky 2001). Premature beats may trigger reentry arrhythmias. However, in the CAST trials, an effective reduction of PVCs (initially >6/h) with antiarrhythmics of the Vaughan-Williams class I (encainide, flecainide, moricizine) in post-MI patients was associated with increased mortality. This indicates that the reduction of PVCs has to be weighed against potential drug-related proarrhythmic effects, in the case of these class I antiarrhythmics, a deceleration of ventricular conduction time probably predisposing for macroreentrant arrhythmias.
4.4.2 Tachyarrhythmias
Mechanistically, tachyarrhythmias are classified as focal (ectopic) tachycardias if electrical activation arises from a group of spontaneously depolarizing atrial or ventricular cardiomyocytes. The sinus node itself may also give rise to tachyarrhythmias (as observed in sick sinus syndrome, see Sect. 4.4.3.1). In contrast, reentry tachycardias are due to myocardial conduction abnormalities leading to circus movement of electrical activation along a defined path. The beat-to-beat interval is therefore very regular. Fibrillation (atrial or ventricular) is the most complex form of arrhythmia, while seemingly chaotic electrical activity during fibrillation may be sustained by focal and/or reentry mechanisms.
4.4.2.1 AV and AV Nodal Reentry Tachycardias
AV reentry tachycardia (AVRT) and AV nodal reentry tachycardia (AVNRT) belong to the group of paroxysmal supraventricular tachycardias (pSVT), characterized by a sudden onset and sudden termination. These tachyarrhythmias are based on a congenital predisposition and often observed in otherwise healthy hearts. The rhythm during tachycardia is usually fast (on average around 180/min, with up to 260/min). In AVRT, the reentry cycle driving the arrhythmia involves an accessory pathway (AP) between the atria and the ventricle, representing a congenital abnormality. During sinus rhythm, electrical activity may be conducted faster by the AP than the AV node, leading to preexcitation of ventricular tissue as reflected by a short PQ interval and a characteristic delta wave in the ECG. During tachycardia, circus movement results from antegrade (atrioventricular) conduction via one and retrograde (ventriculoatrial) conduction via the other pathway. The combination of preexcitation and paroxysmal tachycardias defines the Wolff-Parkinson-White (WPW) syndrome. AVRT tachycardias mostly (95 %) have a narrow QRS complex (antegrade condition via AV node). While generally benign, WPW syndrome carries an increased risk of SCD (~0.1 %), which is higher in familial WPW. This is attributed to an increased incidence of atrial fibrillation with fast conduction to the ventricles via the AP leading to VF. The prevalence of AP is increased in patients with congenital heart disease.
AVNRT is the most frequent pSVT (~60 %) and often manifests in the fourth decade of life. Here, the circus movement involves a fast- and a slow-conducting pathway in the atrial tissue feeding into the compact AV node, followed by rapid conduction to the ventricles via the His-Purkinje system. AVNRT and AVRT can be treated by catheter ablation with a high success rate.
4.4.2.2 Atrial Fibrillation
Atrial fibrillation (AF) is the most common sustained arrhythmia associated with increased morbidity and mortality. The overall prevalence of AF in the Western world is 0.4–2 %. As AF is more common in the elderly (see Sect. 4.6.1), this number is expected to increase (double) in the next 30 years due to the demographic trend. Lifetime risk at an age of 40 years to develop AF is ~25 %. During AF, rapid, seemingly chaotic electrical activity of the atria is sporadically conducted to the ventricles leading to a completely irregular heart rhythm. Ventricular rate is often tachyarrhythmic, but may be normocardiac or bradyarrhythmic depending on the electrical properties of the AV node and concomitant medical therapy. AF leads to the loss of atrial contraction and thus reduced left ventricular (LV) filling, which can reduce cardiac output, especially in conditions of preexisting reduced LV function, and worsen symptoms of heart failure. AF can occur sporadically, lasting seconds to days (paroxysmal AF). AF lasting longer than 7 days or requiring immediate cardioversion to SR is defined as persistent AF. AF for more than 1 year but with the therapeutic goal to convert to SR has been termed long-standing persistent AF. In many patients, episodes of AF tend to become more frequent and longer over time, as AF itself induces changes in the atrial myocardium that promote and sustain the arrhythmia (“AF begets AF,” Wijffels et al. 1995; see Sect. 4.5). If successful restoration of SR is considered unlikely and therapeutic strategy is focused on normalizing heart rate (“rate control”), AF is considered “permanent.”
In patients with AF, slow flow or stasis of blood in the atria together with altered properties of the atrial endocardial surface and cytokine-mediated activation of the coagulation cascade increases the risk of cardiac thrombi, systemic embolism, and stroke. In fact, 25 % of all otherwise unexplained (“cryptogenic”) strokes are attributed to cardiac thromboembolism related to AF. Strokes caused by AF are more often large and fatal, as compared to noncardiac strokes; silent cerebral infarcts can be detected by MRI imaging in about 15 % of all AF patients.
The risk of stroke is strongly dependent on coexisting patient characteristics and comorbidities as summarized by the CHADS-VASc score (Table 4.1). The annual risk for stroke ranges from 1.3 % with CHADS-VASc score of 1 to 15.2 % with CHADS-VASc score of 9 (European Heart Rhythm Association et al. 2010). The risk of stroke is similarly elevated in patients with paroxysmal and persistent AF. In fact, short episodes of AF (>6 min) are sufficient to raise the risk of stroke significantly (ASSERT trial, Healey et al. 2012). Additional, less established risk factors for stroke in AF patients include chronic obstructive lung disease and renal failure. In younger patients (<60) with no additional risk factors (“lone” AF), the risk of stroke is low (~1.3 % in 15 years; European Heart Rhythm Association et al. 2010). Anticoagulation therapy is recommended in patients with CHADS-VASc ≥ 1 and can significantly reduce stroke risk.
In population-based studies and clinical trials, up to 40 % of patients with AF episodes are asymptomatic (Oliner and Ballantine 1968; Disertori et al. 2011) indicating a large dark number of patients with undiagnosed AF and increased risk of stroke. Interestingly, most of the factors predisposing for stroke in the presence of AF are also risk factors for the manifestation of AF (see Table 4.1), indicating that close rhythm monitoring may be beneficial in patients with high CHADS-VASc score even in the absence of a history of AF. However, the prevalence of AF in patients with manifest cardiovascular disease is higher (~13 %) than in patients with cardiovascular risk factors only (6 %, REACH Registry; Goto et al. 2008).
4.4.2.3 Atrial Flutter
Atrial flutter is a supraventricular reentry tachycardia, where the activation path circles around an anatomical structure in the atria with a very regular rate of 250–300/min. In common-type atrial flutter (type I atrial flutter), the reentry cycle is located in the right atrium and involves the cavo-tricuspid isthmus. The electrical activation usually proceeds in a counterclockwise direction, leading to the diagnostically relevant negative P waves in the inferior ECG leads (II, III, aVF). Type I flutter with clockwise wave propagation is less common (10 % of patients with atrial flutter, Bun et al. 2012). Other types of atrial flutter are located around atrial scar tissue, the pulmonary veins, or mitral valve. Atrial flutter is most often observed in patients with concomitant heart disease (coronary artery disease, cardiomyopathy, hypertensive heart disease, following surgery or catheter ablation) but may also occur in otherwise healthy individuals. Also patients with AF receiving class I antiarrhythmics are predisposed to develop atrial flutter. Similar to AF, atrial flutter is thrombogenic and requires anticoagulation. Atrial flutter occurs in 25–35 % of AF patients. Common-type atrial flutter can be curatively treated by catheter ablation with a high (95 %) success rate.
4.4.2.4 Focal Atrial Tachycardia
Focal AT is defined as a regular AT starting at a small atrial region and spreading centrifugally across the atria (Saoudi et al. 2001). Non-sustained focal AT is a common finding in Holter ECGs and often asymptomatic. Sustained AT is generally rare in adults but accounts for 10–23 % of supraventricular tachycardias in otherwise healthy children and is more common in congenital heart disease. The most efficient therapy is catheter ablation of the focus. ATs from three or more different atrial regions (multifocal AT, MAT) lead to an irregular arrhythmia (foci with different cycle length). MAT is a rare arrhythmia (0.1–0.4 % in hospitalized patients, Scher and Arsura 1989) and is often associated with pulmonary disease, coronary artery disease, or heart failure. Treatment with current antiarrhythmic drugs or ablation is not effective and strategies aim to treat the comorbidities.
4.4.2.5 Monomorphic Ventricular Tachycardia
Monomorphic ventricular tachycardia (VT) mostly occurs in patients with structural heart disease and is then based on electrical reentry around an anatomical structure (myocardial scar or aneurysm). VTs present as regular wide/broad QRS complex tachycardia in the ECG. Dissociation of atrial (P waves) and ventricular activity (QRS) and other ECG criteria are used to confirm the diagnosis of VT. Over 90 % of monomorphic VTs are associated with coronary artery disease. Non-sustained VTs (<30 s) are often asymptomatic and then generally do not require specific therapy. However, their occurrence should trigger further diagnostics to evaluate the patient for disease progression (ischemia). Sustained or symptomatic VTs in most cases require implantation of a defibrillator (ICD) to reduce the risk of SCD, as monomorphic as well as polymorphic VT can degenerate into VF leading to SCD. In individual patients, the incidence of VT can be reduced by pharmacological therapy (mainly beta-blockers and class III antiarrhythmics; see below), but in clinical trials current antiarrhythmic therapy has been proven less effective than ICD in reducing morbidity and mortality in selected patient cohorts.
4.4.2.6 Polymorphic Ventricular Tachycardia and Ventricular Fibrillation
Polymorphic VT and VF also most commonly occur in patients with coronary artery disease. Polymorphic VT/VF is also seen in patients with hereditary ion channel dysfunction (long QT syndrome, short QT syndrome, catecholaminergic polymorphic ventricular tachycardia (CPVT), idiopathic VF), drug-induced QT prolongation, and otherwise structurally normal hearts or electrolyte imbalance (hypokalemia or hypomagnesemia). Torsades-de-pointes tachycardia, a specific form of polymorphic VT, is characteristic for conditions of prolonged QT. Polymorphic VT often degenerates into VF but may also terminate spontaneously. Symptomatic polymorphic VT/VF is an indication for ICD therapy when other reversible causes (i.e., acute ischemia due to coronary stenosis) have been ruled out.
4.4.3 Bradyarrhythmias
Bradyarrhythmias result from sinus node dysfunction or atrioventricular block (AVB). Sinus node dysfunction reflects impaired pulse formation in the sinus node or failing conduction from the sinus node cells to the atrial myocardium (sinoatrial block).
4.4.3.1 Sick Sinus Syndrome
Sick sinus syndrome (SSS) is a unifying term for different forms of sinus node dysfunction leading to sinus bradycardia, sinus arrest, or sinoatrial exit block (Bigger and Reiffel 1979). SSS mostly affects the elderly patient and is equally distributed among men and women (Lamas et al. 2000). It may in some cases be related to structural heart disease (ischemia, myocarditis, cardiomyopathies) but is often termed “idiopathic.” Generally, SSS is only treated when patients are symptomatic, mostly warranting implantation of a pacemaker. SSS is associated with other atrial arrhythmias such as sinus tachycardia, atrial fibrillation, paroxysmal supraventricular tachycardias, and atrial flutter. In 60 % of patients, SSS is associated with tachyarrhythmias (Adán and Crown 2003), commonly summarized as “tachy-brady syndrome.”
4.4.3.2 AV Block
In AV block (AVB), conduction from the atria via the AV node/His-Purkinje system to the ventricles is delayed (AVB I), blocked for single beats (AVB II), or blocked completely (AVB III). AVB I and AVB II subtype Wenckebach (progressively increasing AV conduction times before the block) are usually benign, whereas AVB II subtype Mobitz (sudden block of conduction for single beats) and AVB III (both termed high-degree AV block, hdAVB) carry an elevated risk for cardiac arrest. Electroanatomically, hdAVB is mostly located distal to His bundle (infrahisian block).
The prevalence of hdAVB is increased in patients with diabetes mellitus (odds ratio 3.1, Movahed et al. 2005) and hypertensive heart disease. hdAVB is a frequent complication of acute myocardial infarction with a reported incidence of up to 13 %, depending on the location of the infarct. A recent study suggests that the incidence has decreased (to ~3 %) with the advent of more effective revascularization therapy (Gang et al. 2012). However, also recently, hdAVB has been reported to occur during later stages (>21 days) after acute myocardial infarction in ~10 % of patients, contributing to increased morbidity (Gang et al. 2011). hdAVB historically has been the first and remains a standard indication for implantable pacemakers.
4.4.3.3 Chronotropic Incompetence
Chronotropic incompetence (CI) is not an arrhythmia in the stricter sense, but reflects the inability of the sinus node to increase heart rate with increased activity or demand. While resting heart rate remains stable with aging, the maximal heart rate with exercise decreases, largely related to a decrease in exercise tolerance. As a reference, the maximal expected heart rate in a patient is often estimated as 220 bpm – age (in years), yet more elaborated approaches have been described (Brubaker and Kitzman 2011). The lower limit cutoff for an appropriate rise in heart rate with peak exercise is not uniformly defined. Values between 70 % and more commonly 80–85 % of the predicted maximal heart rate during exercise test have been used (Adán and Crown 2003). CI is fairly common in heart failure (~30 % of patients according to one study, Witte et al. 2006) and may be aggravated by concomitant beta-adrenergic receptor blocker therapy. Other proposed pathomechanisms include downregulation of the beta-adrenergic signaling cascade and responsiveness as well as structural remodeling of the sinus node in HF (Sanders et al. 2004).
4.4.4 Sudden Cardiac Death
SCD due to coronary artery disease is the most important cause of death in the adult population of the industrialized countries, and VF is the most common first recorded underlying rhythm (in 75–80 % of cases, Hookana et al. 2011), whereas bradyarrhythmias and asystole are found in ~15–20 %. The interpretation of the causative rhythm is complicated by the fact that VT/VF at some point will convert into asystole, and bradycardia as a result of advanced AV block may trigger VF. The overall incidence of SCD is ~1/1,000/year (Priori et al. 2002). In the United States, SCD comprised up to 15 % of total mortality (Podrid and Myerburg 2005) and similar values (21 % in men and 14.5 % in women) were reported in Europe (Priori et al. 2002). As SCD often occurs in patients with CAD, the risk factors that evolved for SCD match the risk factors for atherosclerosis, i.e., age, smoking, diabetes, male gender, hypertension, and hyperlipidemia. The risk of SCD is related to the degree of structural heart disease. In patients with symptomatic heart failure, chronically severely impaired left ventricular ejection fraction (<35 %) is the strongest indicator for increased mortality due to malignant arrhythmias and indicates primary prophylaxis of SCD with an ICD (Zipes et al. 2006). However, while this group carries the highest risk, in absolute numbers, their contribution to the overall incidence of SCD is small (see Fig. 4.3 from Myerburg et al. 1997), leaving a large group of patients with preserved LV function at risk for SCD.
Sudden death: incidence overall and in subpopulations at risk. High-risk patients are the minority in the overall number of sudden death in the general population (From Myerburg et al. 1997)
4.5 Diagnosis
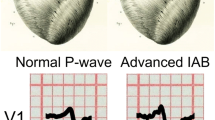
Basis for the diagnosis of rhythm abnormalities is the electrocardiogram (ECG). The highly amplified electrical signals recorded from the surface of the skin represent a summation of electrical field vectors arising from differences in the membrane potential during the cardiac cycle. ECGs allow the differentiation between atrial and ventricular arrhythmias in most cases based on the width of the QRS complex reflecting the ventricular activation sequence. Further analysis of P wave (atrial activation) and QRS morphology in the standard 12-lead surface ECG helps to narrow down further the region of ectopic activity. Twenty-four hours to 7 days Holter ECGs and surface electrode event recorders (up to 30 days) are used to document episodic arrhythmias, whereas subcutaneously implanted event monitors allow continuous rhythm monitoring for currently up to 3 years. ECG ergometry is useful to document stress-induced tachyarrhythmias or conduction deficits as well as for risk stratification (in certain cardiomyopathies and in patients with accessory pathways). Ultimately, management of patients with recurrent symptomatic arrhythmias may necessitate an electrophysiologic study with intracardial mapping and stimulation protocols to induce the arrhythmia, determine the exact mechanism and location, and potentially ablate myocardial structures involved.
4.6 Pathomechanisms of Arrhythmogeneity
Electrophysiological mapping of intracardial spread of electrical activity allows distinguishing arrhythmias driven by repetitive focal (ectopic) activity from reentry tachycardias with circus movement of electrical activation involving larger parts of the myocardium. Focal arrhythmias can be explained by enhanced impulse formation either by automaticity (spontaneous depolarization) or triggered activity (depolarization following a regular beat). Some of the arrhythmias classified as focal in origin, however, may not depend on locally enhanced impulse formation but reflect small, localized reentry cycles (“microreentry”).
4.6.1 Automaticity
Cells from the His-Purkinje system slowly depolarize during phase 4 of the AP (Fig. 4.1), albeit at a slower rate as sinus node cells. In conditions of ischemia or cell injury (e.g., myocardial infarction) as well as during increased beta-adrenergic stimulation, enhanced automaticity may occur in these cells leading to focal arrhythmias, such as accelerated idioventricular or junctional rhythm. In similar conditions, working myocardium may regain the capability of periodic depolarizations during phase 4, leading to abnormal automaticity, as is observed, e.g., in multifocal atrial tachycardias (Carmeliet 1999). While most ventricular tachycardias are reentry tachycardias, a small subset of monomorphic ventricular tachycardias triggered by enhanced activity in Purkinje cells has recently received greater attention as these arrhythmias can be cured by focal ablation of the arrhythmogenic Purkinje cells (Nogami 2011).
4.6.2 Triggered Activity
Triggered activity comprises transient membrane depolarizations that are linked to a normal action potential, which are divided into early (EAD) or delayed (DAD) afterdepolarizations. EADs occur during repolarization (phase 2 or phase 3 of the action potential) and lead to a deceleration or transient reversal of repolarization. DADs occur in phase 4 when repolarization to the resting potential has been completed (Fig. 4.4).
4.6.2.1 Delayed Afterdepolarizations
Delayed afterdepolarizations (DAD) in cardiomyocytes occur as a result of high intracellular Ca2+ load. The classical model of intracellular Ca2+ overload is digitalis toxicity (Fig. 4.5). Digitalis inhibits the sarcolemmal Na+/K+ ATPase, resulting in intracellular Na+ accumulation (1). Na+ is exchanged with Ca2+ by the sarcolemmal Na+/Ca2+ exchanger (2). Excess Ca2+ transported into the intracellular store (sarcoplasmic reticulum, SR) (3) leads to diastolic SR Ca2+ leak (4). Increased cytosolic Ca2+ triggers transsarcolemmal Na+ influx via the Na+/Ca2+ exchanger reflected by a transient inward current (I ti) (5). If the depolarization of the membrane by I ti reaches the activation threshold of the fast Na+ channels, an irregular action potential is generated.
Increased SR Ca2+ leak is also observed in experimental and human chronic heart failure, related to alterations in the properties of the SR Ca2+ release channel, the ryanodine receptor (RyR, Fig. 4.5). In heart failure, reduction in I K1, a current that repolarizes and stabilizes the resting membrane potential during diastole, can facilitate Ca2+-induced arrhythmias (Pogwizd and Bers 2004). Catecholaminergic polymorphic ventricular tachycardia (CPVT) is a rare but well-studied hereditary arrhythmia, where mutations to the ryanodine receptor (in autosomal dominant CPVT type 1) or the SR Ca2+ binding protein calsequestrin (autosomal recessive CPVT 2) lead to increased SR Ca2+ leak, DADs, bigeminus, and characteristic bidirectional polymorphic ventricular tachycardias, identical to what is observed with digitalis. In light of a common pathomechanism in hereditary and acquired arrhythmias, decreasing Ca2+ leak from the SR in cardiac remodeling is currently investigated as a potential new therapeutic target (Sacherer et al. 2012).
4.6.2.2 Early Afterdepolarizations
EADs result from a transient inward current mainly through (re)activation of sarcolemmal L-type Ca2+ channels (January and Riddle 1989) and Na+ channels (Boutjdir et al. 1994), but there may be a role for NCX-mediated inward current as well (Volders et al. 2000). EADs occur in the setting of increased AP duration (APD). APD prolongation can result from acute changes in electrolytes (hypokalemia, hypomagnesemia), from remodeling of transsarcolemmal ion channels (e.g., downregulation of rectifying potassium channels, increase in late sodium current), as well as from alterations in intracellular Ca2+ release (longer Ca2+ transient) (Volders et al. 2000). APD prolongation facilitating EADs is also induced by an increased cycle length (pause) of the preceding beat; this mechanism is called pause-dependent triggered activity; EADs (rather than DADs) are provoked in conditions of alpha- and beta-adrenergic stimulation in combination with rapid pacing rate. In the surface ECG, EADs may be apparent as T-wave alterations and U-waves.
4.6.2.3 Arrhythmias Initiated by Triggered Activity
Atrial tachycardias based on triggered activity rarely occur in clinically stable patients but are observed in the presence of acute adrenergic stimuli, either endogenous (acute illness) or exogenous (adrenergic agents, caffeine, theophylline; Josephson 2008). Triggered atrial arrhythmias are also observed during atrial ischemia (Nishida et al. 2011) and are thought to contribute to atrial fibrillation (see Sect. 4.6.5).
In ischemic cardiomyopathy, ventricular arrhythmias are mostly initiated by reentry mechanisms (see Sects. 4.6.3 and 4.7.2). In nonischemic cardiomyopathy, however, monomorphic focal arrhythmias that arise from triggered activity are more often observed (Pogwizd et al. 1998). Idiopathic arrhythmias from the ventricular outflow tract in otherwise structurally normal hearts are also based on triggered activity (O’Donnell et al. 2003). Torsades-de-pointes tachycardia, which is characteristic for hereditary and acquired long QT syndromes (prolonged APDs), is based on EADs, whereas catecholaminergic polymorphic ventricular tachycardias are initiated by DADs.
4.6.3 Reentry
Reentry tachycardias are the most common regular tachyarrhythmias. The mechanism of reentry has first been described in detail for AV reentry tachycardias (see Sect. 4.4.2.1). In these conditions, (congenitally) preformed conduction pathways run in parallel to the normal AV nodal activation sequence connecting the atria to the ventricle. These pathways possess different conduction velocities (Fig. 4.6) and refractoriness (i.e., recovery time after activation) than the physiological AV conduction. Reentry tachycardias initiate when a unidirectional block prevents activation of one pathway (Fig. 4.6, left), allowing conduction along the second pathway (2) and retrogradely along the first pathway (3), thus closing the circle. Initiation and maintenance of the reentry arrhythmia strongly depends on the relationship between the conduction velocities and recovery times of these antegradely and retrogradely conducting pathways. Often these arrhythmias occur in response to changes in autonomous tone (i.e., with exercise or before falling asleep), as this affects myocardial conduction velocities. Typically (but not always), these supraventricular reentry tachycardias can be terminated by increasing the parasympathetic tone (vagal nerve stimulation by “Valsalva” maneuvers).
Mechanisms of reentry. Left: reentry requires two differentially conducting pathways that are joined at the beginning and end. Middle and right (Adapted from Stevenson et al. (1993) and El-Sherif et al. (1982)): in diseased ventricular tissue, the substrate for reentry may be more complex, e.g., following a “figure-of-8” pattern. See text for details
Ventricular reentry tachycardias are most commonly seen in structurally diseased hearts. Circus movement of electrical activity occurs around islets of fibrotic tissue (often, infarct scar). According to a common model, rather than forming a simple circle, electrical activation is slowed down along a central common pathway (CP) of viable but dysfunctional myocardium. Upon exiting the diseased area, electrical activation returns to the CP entrance in clockwise and counterclockwise direction, thus forming two synchronous circuits in a “figure-of-8” (Fig. 4.6, right; El-Sherif et al. 1982). Often myocardial scars are interwoven with viable tissue leading to a more complex arrangement of conducting and nonconducting tissue forming the arrhythmogenic substrate (Fig. 4.6, middle; Stevenson et al. 1993). Other models agree with a more dynamic distribution of reentry circles resulting in rotating 2D vortices of electrical activation. Independent of the underlying model, typical features of reentry tachycardias are that they are usually regular, monomorphic, and easily inducible by short coupled extra stimuli during programmed electrical stimulation in an electrophysiological study.
4.6.4 Cellular Heterogeneity in the Arrhythmogenic Substrate
Even in the normal heart, epicardial, endocardial, and mid-myocardial cells have distinct electrophysiological properties. For instance, the latter, “M-cells,” are characterized by longer AP duration and higher susceptibility to class III (potassium-inhibiting) antiarrhythmics (Antzelevitch and Fish 2001). Additionally, heterogeneity in cardiomyocyte orientation, cell-to-cell coupling (connexin 43 expression), and distribution of fibrous tissue contribute to the spatial transmural dispersion of repolarization (Glukhov et al. 2010). In LV hypertrophy, epicardial APs are more prolonged than endocardial, probably related to alterations in I to, I Ca, and NCX density (Bryant et al. 1997; Shipsey et al. 1997; McIntosh et al. 1998). Also, in heart failure, APD prolongation is more heterogenously distributed. The spatial dispersion of repolarization may alter with heart rate. In the inherited long QT syndrome 3 (increased Na+ channel activity), a very pronounced dispersion of AP duration during bradycardia facilitates triggered activity.
In addition, temporal dispersion of repolarization is reflected in beat-to-beat changes in AP duration in the same cell. Electrical alternans describes a periodic change between short and long APs from beat to beat. In experimental conditions, AP alternans is often observed at higher pacing rates and has been linked to intracellular Ca2+ overload. In patients, temporal dispersion of cardiomyocyte repolarization is reflected by alterations in the amplitude of the T-wave in the surface ECG (T-wave alternans, TWA). In clinical studies, TWA has been used to predict susceptibility to ventricular arrhythmias and SCD in patients with ischemic and nonischemic cardiomyopathy or inherited arrhythmias (e.g., Brugada syndrome). However, further studies are needed to establish the role of TWA in clinical decision making (Narayan 2006).
4.6.5 From Cellular Depolarizations to Arrhythmias
Several of the arrhythmogenic mechanisms outlined before are often acting together to initiate and sustain arrhythmias. Mostly, arrhythmias are triggered by an ectopic beat as a result of triggered activity, which may then induce a monomorphic reentry tachycardia around scar tissue or a torsades-de-pointes reentry tachycardia sustained by intramyocardial heterogeneity of repolarization.
Cardiomyocytes are connected by gap junctions resulting in electrotonic coupling. In this syncytium, a depolarizing cell acts as a source of electrical charge, which will be conducted to neighboring cardiomyocytes acting as a “sink” for this charge. Based on the source-sink concept, it can be concluded that a single arrhythmogenic cell may by far not be sufficient to trigger a propagating AP throughout the myocardium (Xie et al. 2010). Recent evidence suggests that arrhythmogenic activity in neighboring cardiomyocytes can be “synchronized” by adrenergic stimuli to create a depolarizing source that can overcome the sink (Myles et al. 2012). An increase in fibrous tissue during structural remodeling can additionally passively reduce the number of surrounding cardiomyocytes acting as a sink and also forms a potential basis for electrotonic interaction between cardiomyocytes and myofibroblasts that may promote depolarizations and thus arrhythmias (Rohr et al. 1997; Myles et al. 2012).
4.7 Conditions of Increased Arrhythmogeneity
A variety of comorbidities and patient characteristics have been associated with arrhythmias. In the following, major risk factors for arrhythmias identified in large clinical studies are discussed.
4.7.1 Endogenous Triggers
As outlined above, arrhythmias may be triggered by stress or other alterations in autonomous tone. The sympathetic nervous system is a well-known trigger of arrhythmias. In cardiomyocytes, beta-adrenergic receptor stimulation increases cytosolic cAMP and downstream signaling pathways, such as protein kinase A-mediated phosphorylation of the sarcolemmal Ca2+ channel and an increase in the sarcoplasmic reticulum Ca2+ load. While these effects mediate positive inotropy, they also predispose for Ca2+-mediated triggered arrhythmias (see Sect. 4.6.2.1). In chronic heart failure but also in other systemic diseases such as sepsis, sympathetic tone is increased predisposing for arrhythmias.
The renin-angiotensin-aldosterone system (RAAS) is another important neurohumoral axis in cardiac remodeling. Angiotensin II (AT II) is a potent vasoconstrictor and has also been implicated in atrial and ventricular arrhythmias. The cellular pathomechanisms of ATII-mediated arrhythmogeneity are complex and have not been fully elucidated but likely involve Ca2+- and reactive oxygen species (ROS)-dependent signaling (Zhao et al. 2011). While RAAS antagonists (angiotensin receptor blockers, angiotensin converting enzyme inhibitors) effectively reduce ventricular arrhythmias and SCD in patients with heart failure, their use in the absence of heart failure to prevent AF (so-called upstream therapy) has so far proven unsuccessful (Savelieva et al. 2011).
4.7.2 Arrhythmias in Structurally Diseased Hearts
4.7.2.1 Acute and Chronic Myocardial Ischemia
Acute ischemia leads to cardiomyocyte depolarization, intracellular Ca2+ and Na+ overload, and K+ efflux in cardiomyocytes (Ehlert and Goldberger 1997), promoting triggered activity (EADs, DADs). Electrical dispersion of repolarization additionally contributes to an increased propensity for arrhythmias (Janse and Wit 1989), largely reentry tachycardias in the early phase (phase 1a) of ischemia. In the later phase (1b, more than 10 min ischemia), endogenous catecholamines further facilitate arrhythmias. Clinically, in the acute phase of MI, polymorphic and torsades-de-pointes tachycardia is often observed, usually not associated with QT prolongation in the surface ECG.
Ischemic heart disease (IHD) refers to chronic left ventricular dysfunction related to ischemia on the basis of coronary artery disease. The incidence of arrhythmias – atrial and ventricular – is increased in IHD. In patients with IHD, an increased prevalence of PVCs is related to an increased risk of SCD. Based on this observation, Lown has introduced a classification of PVCs based on their frequency and morphology (Lown and Wolf 1971). However, the positive predictive and discriminative value of PVCs alone to detect SCD is low (5–15 %; Crawford et al. 1999), and the Lown classification is no longer used for risk stratification in clinical practice. To date, the extent of left ventricular dysfunction (ejection fraction) remains the strongest predictor of malignant arrhythmias and SCD in clinical practice.
4.7.2.2 Heart Failure
Roughly half of the patients with chronic heart failure die of SCD. Heart failure predisposes to ventricular tachyarrhythmias (see Sect. 4.4.4). A variety of intracellular signaling cascades related to neurohumoral activation are activated in advanced heart failure independent of the origin of cardiac remodeling. Endogenous catecholamines, angiotensin II, endothelin, and other hormones and paracrine mediators promote arrhythmias in cardiac myocytes. Independent of these changes in the in vivo milieu, cardiomyocyte remodeling in heart failure alters the cellular phenotype. At the cellular level, prolonged cytosolic Ca2+ transients, Ca2+ leak from the sarcoplasmic reticulum, and AP prolongation are commonly observed, the latter also attributed to a reduction in repolarizing potassium currents (I Ks, I Kr, I K1) and increase in NCX but also to late sodium influx through the fast sodium channels (Aiba and Tomaselli 2010). Less selective cation channels (i.e., TRPC channels) and stretch-activated channels promote agonist-induced or mechanical stress-induced ectopic activity. Structural (scar, fibrosis) and functional (stretch, ischemia) conduction abnormalities contribute to the maintenance of sustained arrhythmias. In patients with heart failure, currently, the only clinically widely accepted predictor of ventricular arrhythmias and sudden cardiac death is the extent of LV contractile impairment as quantified by the LV ejection fraction (EF). Patients with chronically severely reduced LV function (EF < 35 %) should receive an implantable cardioverter defibrillator (ICD) for primary prevention of SCD, as current antiarrhythmic pharmacological therapy has proven inferior to ICD therapy in improving survival.
4.7.2.3 Nonischemic Cardiomyopathies
In dilative cardiomyopathy (DCM), ventricular tachyarrhythmias are mostly reentry tachycardias. However, as opposed to IHD, myocardial fibrosis is more diffuse. The spectrum of arrhythmogenic substrates is more heterogenous and may involve focal tachycardias, epicardial reentry circuits, and macroreentry involving the His-Purkinje system. Risk stratification for SCD is more challenging in these patients as ventricular tachyarrhythmias show a low inducibility during electrophysiological studies.
In patients with hypertrophic cardiomyopathy (HCM), the annual risk of SCD is ~1 %, with large interindividual variation related to patient characteristics (such as LV septum thickness). SCD may be the first disease manifestation (Elliott et al. 2006). HCM is the most common reason for SCD in competitive athletes. Many patients with HCM do not survive the first arrhythmogenic event, and additional risk factors have been defined to identify asymptomatic patients at increased risk (such as positive family history, unexplained syncope, pathologic exercise test, pronounced hypertrophy, and non-sustained VTs). In 50–70 % of patients, HCM can be attributed to one of the currently known mutations coding for sarcomeric genes.
4.7.3 Genetic Predisposition
Genetic predisposition to arrhythmias has been studied best in a group of rare ion channel defects with monogenetic inheritance. These channelopathies are characterized by an increased incidence for arrhythmic sudden cardiac death in otherwise apparently structurally normal hearts. Most common (~1/5,000 individuals, Kass and Moss 2003) are the long QT (LQT) syndromes, a heterogenous group of point mutations with loss-of-function defects of potassium channels (the most prevalent types LQT1 and LQT2 but also very rare LQT5-7) or gain-of-function defects of the fast sodium channel (LQTS 3) (Zipes et al. 2006). However, also cytoskeletal anchoring proteins (LQT4) can be involved. LQT syndromes are characterized by a prolonged QT interval in the resting ECG and a predisposition for torsades-de-pointes-type polymorphic VT and VF. LQT syndrome often manifests already in childhood with unexplained syncope. Recently, rare conditions of arrhythmias associated with an extraordinarily short QT interval (QTc < 350 ms) have been identified (Patel et al. 2010). As in LQT, causes for secondary alterations in the QT interval such as alterations in serum electrolytes (potassium), acid–base status, or catecholamines and other drugs (digitalis) have to be excluded. On the cellular level, a reduction in Ca2+ or Na+ inward current or an increase in K+ outward current can shorten APD. In accordance, several loss-of-function and gain-of-function mutations in these respective ion channel genes have been described in affected families. As in LQT, the disparity of repolarization is increased in short QT syndrome. Other monogenetically inherited arrhythmias include catecholaminergic polymorphic ventricular tachycardia (see Sect. 4.6.2.3), some forms of the Brugada syndrome, and arrhythmogenic cardiomyopathies such as arrhythmogenic right ventricular dysplasia (ARVD) and hypertrophic cardiomyopathy (see Sect. 4.7.2.3).
Monogenetically inherited single point mutations to ion channels, however, have only been able to explain a minority of arrhythmias with familiar clustering. Common arrhythmias, e.g., AF, or a predisposition for ventricular tachycardias during ischemia, have been linked with several predisposing genetic variations (modifier genes) and in most cases are likely polygenetic. Genome-wide association studies (GWAS) are being used to link abnormalities in heart rhythm or ECG morphology with gene polymorphisms, with variable success. A more comprehensive systems biology approach may be required to identify and manage patients with genetic predisposition for arrhythmias (Grace and Roden 2012).
4.7.4 Age
The number of ectopic PACs and PVCs increases with age in the healthy population (Kostis et al. 1981; Bjerregaard 1982) as well as in patients following myocardial infarction, where age is also associated with a higher prevalence of VTs (Josephson et al. 1995). Older patients have a higher dispersion of repolarization (Saadeh 2004) which may promote arrhythmias. Sinus node dysfunction is a typical disease of the elderly with an average age at diagnosis of 68 years. The prevalence of AF is strongly associated with age (Fig. 4.7, modified from Feinberg et al. 1995). The incidence of SCD increases with age in parallel with the increase in coronary artery disease but is relatively lower in patients above age 70 years due to competing causes of death (Zipes et al. 2006).
Increase in the prevalence of atrial fibrillation (AF) with age in population-based studies (Modified from Feinberg et al. (1995))
4.7.5 Gender
Women have a higher resting heart rate than men and this is independent of differences in autonomous tone (Jose and Collison 1970; Burke et al. 1996). Additionally, typical ECG findings associated with female gender include a slightly longer QT interval (~20 ms longer than in men) as described early by Bazett (1920) and confirmed by others (Molnar et al. 1996). This difference in QT interval may be driven by the higher testosterone levels in men (Zhang et al. 2011). For AV node reentry tachycardia, the gender ratio is about 2:1 (female to male, Rodriguez et al. 1992; Liuba et al. 2006). The reason for this difference is not completely understood but may be related to differences in the refractory periods of the fast- and slow-conducting properties of the AV nodal input (Liuba et al. 2006). Accessory pathways are more commonly seen in men than in women, with a 1:2 female to male gender ratio, and this applies to overt as well as concealed AP (Rodriguez et al. 1992). Men with WPW are more likely to develop AF and VF than women with AP, probably related to the overall increased incidence of AF in men. The incidence of focal AT is evenly distributed between men and women (Rodriguez et al. 1992). With respect to ventricular tachycardias, women are more likely to develop TdP tachycardia (Lehmann et al. 1996; Makkar et al. 1993), possibly related to the slightly longer QT interval in women which manifests especially at lower heart rates (Kligfield et al. 1996; Rautaharju et al. 1992).
4.7.6 Arterial Hypertension
An acute elevation in arterial blood pressure can trigger PVCs, PACS, as well as atrioventricular block (Sideris et al. 1987, 1988). In chronic arterial hypertension, the risk of atrial arrhythmias is increased, even more if hypertension is associated with LV hypertrophy (Loaldi et al. 1983), indicating a causative role for increased LV and consecutively left atrial pressure. Increased LV mass is associated with an increased risk for SCD (Haider et al. 1998). In patients with arterial hypertension, a higher QTc dispersion is observed (Saadeh 2004). This is consistent with experimental data, as in hypertrophied myocardium prolongation of the AP, and refractoriness is the most commonly observed electrophysiological alteration. However, this effect is not uniform to all models, and the underlying ionic mechanisms for AP prolongation vary between models and species (Pye and Cobbe 1992; Hart 1994; Boyden and Jeck 1995).
4.7.7 Diabetes Mellitus and Metabolic Syndrome
Diabetes mellitus (DM) increases the risk for SCD roughly twofold (Bergner and Goldberger 2010). DM is a strong risk factor for coronary artery disease which by itself conveys an increased risk for ventricular arrhythmias. Proarrhythmic electrophysiological changes associated with DM include a prolonged QTc interval (>440 ms in about 25 % of diabetics), which has been related to increased mortality in type 1 diabetics in one study (Veglio et al. 2000). QTc prolongation may be a result of increased endogenous catecholamines in response to transient hypoglycemia (Robinson et al. 2003). Recent evidence suggests a higher incidence in QT prolongation and dispersion in patients with metabolic syndrome even in the absence of overt diabetes mellitus (Isik et al. 2012). However, current clinical evidence linking DM to increased ventricular arrhythmogeneity remains sparse. A large meta-analysis reported a 40 % increased risk for developing AF in diabetic patients (Robinson et al. 2003).
4.7.8 Renal Dysfunction
In patients with chronic kidney disease, worsening of renal function is linked to increased QT duration, QT dispersion, and minor arrhythmias (Stewart et al. 2005). LV hypertrophy and LV diastolic dysfunction are common findings in patients with advanced renal dysfunction and may contribute to the increased arrhythmogeneity. In the presence of dilative cardiomyopathy, renal dysfunction (GFR < 60 ml/min/1.72 m2) is associated with increased incidence of ventricular arrhythmias (Takahashi et al. 2009). However, with worsening renal function, the presumed effect of arrhythmias on morbidity and mortality is outweighed by the concomitant increase in noncardiac mortality so that patients with advanced renal dysfunction generally profit less from primary prophylaxis for SCD using ICDs (Goldenberg et al. 2008). Renal dysfunction has evolved as a risk factor for AF in recent clinical studies (Piccini et al. 2013) and also in experimental conditions (Fukunaga et al. 2012); however, the underlying pathomechanisms are currently unclear. In end-stage renal failure patients, arrhythmias often occur during or shortly after hemodialysis, especially in patients with concomitant structural heart disease, and are mostly related to acute electrolyte imbalance (Zipes et al. 2006).
4.8 Summary and Perspectives
Arrhythmias are common in clinical practice and are not always symptomatic. AF and ventricular arrhythmias often occur as a manifestation of structural heart disease and are associated with increased morbidity and mortality. Genetic predisposition, acquired comorbidities, and neurohumoral activation are modulators of arrhythmogeneity. Especially in patients with structural heart disease, pharmacological therapy of arrhythmias is limited due to the proarrhythmic potential of current specific antiarrhythmic drugs (Vaughan-Williams class I and III). The degree of LV dysfunction currently determines the need for an ICD for primary prophylaxis of SCD. Risk scores derived from selective gene profiling and comprehensive evaluation of relevant clinical comorbidities could allow for identification of a number of patients at risk for SCD that currently do not fulfill the criteria for an ICD. New therapeutic approaches for the treatment of AF include the relatively atrial-selective multichannel blocker vernakalant, inhibition of the late Na+ current (ranolazine), and early catheter-based ablation of AF in selected patients. Future antiarrhythmic strategies that are currently experimentally tested include blockers of intracellular Ca2+ leak and gene therapy.
References
Adán V, Crown LA (2003) Diagnosis and treatment of sick sinus syndrome. Am Fam Physician 67(8):1725–1732
Aiba T, Tomaselli GF (2010) Electrical remodeling in the failing heart. Curr Opin Cardiol 25(1):29–36
Antzelevitch C, Fish J (2001) Electrical heterogeneity within the ventricular wall. Basic Res Cardiol 96(6):517–527
Barsky AJ (2001) Palpitations, arrhythmias, and awareness of cardiac activity. Ann Intern Med 134(9 Pt 2):832–837
Bazett H (1920) An analysis of the time-relations of electrocardiograms. Heart 7:353–370
Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA (1994) Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 271(11):840–844
Bergner DW, Goldberger JJ (2010) Diabetes mellitus and sudden cardiac death: what are the data? Cardiol J 17(2):117–129
Bigger JT Jr, Reiffel JA (1979) Sick sinus syndrome. Annu Rev Med 30:91–118
Bjerregaard P (1982) Premature beats in healthy subjects 40–79 years of age. Eur Heart J 3(6):493–503
Bloch Thomsen PE, Jons C, Raatikainen MJ, Moerch Joergensen R, Hartikainen J, Virtanen V, Boland J, Anttonen O, Gang UJ, Hoest N, Boersma LV, Platou ES, Becker D, Messier MD, Huikuri HV, Cardiac Arrhythmias and Risk Stratification After Acute Myocardial Infarction (CARISMA) Study Group (2010) Long-term recording of cardiac arrhythmias with an implantable cardiac monitor in patients with reduced ejection fraction after acute myocardial infarction: the Cardiac Arrhythmias and Risk Stratification After Acute Myocardial Infarction (CARISMA) study. Circulation 122(13):1258–1264
Boutjdir M, Restivo M, Wei Y, Stergiopoulos K, el-Sherif N N (1994) Early afterdepolarization formation in cardiac myocytes: analysis of phase plane patterns, action potential, and membrane currents. J Cardiovasc Electrophysiol 5(7):609–620
Boyden PA, Jeck CD (1995) Ion channel function in disease. Cardiovasc Res 29(3):312–318
Brubaker PH, Kitzman DW (2011) Chronotropic incompetence: causes, consequences, and management. Circulation 123(9):1010–1020
Bryant SM, Shipsey SJ, Hart G (1997) Regional differences in electrical and mechanical properties of myocytes from guinea-pig hearts with mild left ventricular hypertrophy. Cardiovasc Res 35(2):315–323
Bun SS, Latcu DG, Prevot S, Bastard E, Franceschi F, Ricard P, Saoudi N, Deharo JC (2012) Characteristics of recurrent clockwise atrial flutter after previous radiofrequency catheter ablation for counterclockwise isthmus-dependent atrial flutter. Europace 14(9):1340–1343
Burke JH, Goldberger JJ, Ehlert FA, Kruse JT, Parker MA, Kadish AH (1996) Gender differences in heart rate before and after autonomic blockade: evidence against an intrinsic gender effect. Am J Med 100(5):537–543
Carmeliet E (1999) Cardiac ionic currents and acute ischemia: from channels to arrhythmias. Physiol Rev 79(3):917–1017
Crawford MH, Bernstein SJ, Deedwania PC, DiMarco JP, Ferrick KJ, Garson A Jr, Green LA, Greene HL, Silka MJ, Stone PH, Tracy CM, Gibbons RJ, Alpert JS, Eagle KA, Gardner TJ, Gregoratos G, Russell RO, Ryan TH, Smith SC Jr (1999) ACC/AHA Guidelines for Ambulatory Electrocardiography. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the Guidelines for Ambulatory Electrocardiography). Developed in collaboration with the North American Society for Pacing and Electrophysiology. J Am Coll Cardiol 34(3):912–948
Custodis F, Schirmer SH, Baumhäkel M, Heusch G, Böhm M, Laufs U (2010) Vascular pathophysiology in response to increased heart rate. J Am Coll Cardiol 56(24):1973–1983
Disertori M, Lombardi F, Barlera S, Maggioni AP, Favero C, Franzosi MG, Lucci D, Staszewsky L, Fabbri G, Quintarelli S, Bianconi L, Latini R (2011) Clinical characteristics of patients with asymptomatic recurrences of atrial fibrillation in the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico-Atrial Fibrillation (GISSI-AF) trial. Am Heart J 162(2):382–389
Ehlert FA, Goldberger JJ (1997) Cellular and pathophysiological mechanisms of ventricular arrhythmias in acute ischemia and infarction. Pacing Clin Electrophysiol 20(4 Pt 1):966–975
Elliott PM, Gimeno JR, Thaman R, Shah J, Ward D, Dickie S, Tome Esteban MT, McKenna WJ (2006) Historical trends in reported survival rates in patients with hypertrophic cardiomyopathy. Heart 92(6):785–791
El-Sherif N, Mehra R, Gough WB, Zeiler RH (1982) Ventricular activation patterns of spontaneous and induced ventricular rhythms in canine one-day-old myocardial infarction. Evidence for focal and reentrant mechanisms. Circ Res 51(2):152–166
European Heart Rhythm Association, European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De Caterina R, De Sutter J, Goette A, Gorenek B, Heldal M, Hohloser SH, Kolh P, Le Heuzey JY, Ponikowski P, Rutten FH (2010) Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 31(19):2369–2429
Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG (1995) Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med 155(5):469–473
Fukunaga N, Takahashi N, Hagiwara S, Kume O, Fukui A, Teshima Y, Shinohara T, Nawata T, Hara M, Noguchi T, Saikawa T (2012) Establishment of a model of atrial fibrillation associated with chronic kidney disease in rats and the role of oxidative stress. Heart Rhythm 12:2023–2031
Gang UJ, Jøns C, Jørgensen RM, Abildstrøm SZ, Messier MD, Haarbo J, Huikuri HV, Thomsen PE (2011) Clinical significance of late high-degree atrioventricular block in patients with left ventricular dysfunction after an acute myocardial infarction – a Cardiac Arrhythmias and Risk Stratification After Acute Myocardial Infarction (CARISMA) substudy. Am Heart J 162(3):542–547
Gang UJ, Hvelplund A, Pedersen S, Iversen A, Jøns C, Abildstrøm SZ, Haarbo J, Jensen JS, Thomsen PE (2012) High-degree atrioventricular block complicating ST-segment elevation myocardial infarction in the era of primary percutaneous coronary intervention. Europace 14(11):1639–1645
Glukhov AV, Fedorov VV, Lou Q, Ravikumar VK, Kalish PW, Schuessler RB, Moazami N, Efimov IR (2010) Transmural dispersion of repolarization in failing and nonfailing human ventricle. Circ Res 106(5):981–991
Goldenberg I, Vyas AK, Hall WJ, Moss AJ, Wang H, He H, Zareba W, McNitt S, Andrews ML, MADIT-II Investigators (2008) Risk stratification for primary implantation of a cardioverter-defibrillator in patients with ischemic left ventricular dysfunction. J Am Coll Cardiol 51(3):288–296
Goto S, Bhatt DL, Röther J, Alberts M, Hill MD, Ikeda Y, Uchiyama S, D’Agostino R, Ohman EM, Liau CS, Hirsch AT, Mas JL, Wilson PW, Corbalán R, Aichner F, Steg PG, REACH Registry Investigators (2008) Prevalence, clinical profile, and cardiovascular outcomes of atrial fibrillation patients with atherothrombosis. Am Heart J 156(5):855–863, 863.e2
Grace AA, Roden DM (2012) Systems biology and cardiac arrhythmias. Lancet 380(9852):1498–1508
Haider AW, Larson MG, Benjamin EJ, Levy D (1998) Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. J Am Coll Cardiol 32(5):1454–1459
Hart G (1994) Cellular electrophysiology in cardiac hypertrophy and failure. Cardiovasc Res 28(7):933–946
Healey JS, Connolly SJ (2003) Atrial fibrillation: hypertension as a causative agent, risk factor for complications, and potential therapeutic target. Am J Cardiol 91(10A):9G–14G
Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, Lau CP, Fain E, Yang S, Bailleul C, Morillo CA, Carlson M, Themeles E, Kaufman ES, Hohnloser SH, ASSERT Investigators (2012) Subclinical atrial fibrillation and the risk of stroke. N Engl J Med 366(2):120–129
Hookana E, Junttila MJ, Puurunen VP, Tikkanen JT, Kaikkonen KS, Kortelainen ML, Myerburg RJ, Huikuri HV (2011) Causes of nonischemic sudden cardiac death in the current era. Heart Rhythm 8(10):1570–1575
Huxley RR, Filion KB, Konety S, Alonso A (2011) Meta-analysis of cohort and case–control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol 108(1):56–62
Isik T, Tanboga IH, Kurt M, Kaya A, Ekinci M, Ayhan E, Uluganyan M, Ergelen M, Guvenc TS, Altay S, Uyarel H (2012) Relation of the metabolic syndrome with proarrhythmogenic electrocardiographic parameters in patients without overt diabetes. Acta Cardiol 67(2):195–201
Janse MJ, Wit AL (1989) Electrophysiological mechanisms of ventricular arrhythmias resulting from myocardial ischemia and infarction. Physiol Rev 69(4):1049–1169
January CT, Riddle JM (1989) Early afterdepolarizations: mechanism of induction and block. A role for L-type Ca2+ current. Circ Res 64(5):977–990
Jose AD, Collison D (1970) The normal range and determinants of the intrinsic heart rate in man. Cardiovasc Res 4(2):160–167
Josephson ME (2008) Clinical cardiac electrophysiology – techniques and interpretations, 4th edn. Wolters Kluwer
Josephson RA, Papa LA, Brooks MM, Morris M, Akiyama T, Greene HL (1995) Effect of age on postmyocardial infarction ventricular arrhythmias (Holter Registry data from CAST I and CAST II). Cardiovascular Arrhythmia Suppression Trials. Am J Cardiol 76(10):710–713
Kass RS, Moss AJ (2003) Long QT syndrome: novel insights into the mechanisms of cardiac arrhythmias. J Clin Invest 112(6):810–815
Kligfield P, Lax KG, Okin PM (1996) QT interval-heart rate relation during exercise in normal men and women: definition by linear regression analysis. J Am Coll Cardiol 28(6):1547–1555
Kostis JB, McCrone K, Moreyra AE, Gotzoyannis S, Aglitz NM, Natarajan N, Kuo PT (1981) Premature ventricular complexes in the absence of identifiable heart disease. Circulation 63(6):1351–1356
Lakatta EG, Maltsev VA, Vinogradova TM (2010) A coupled SYSTEM of intracellular Ca2+ clocks and surface membrane voltage clocks controls the timekeeping mechanism of the heart’s pacemaker. Circ Res 106(4):659–673
Lamas GA, Lee K, Sweeney M, Leon A, Yee R, Ellenbogen K, Greer S, Wilber D, Silverman R, Marinchak R, Bernstein R, Mittleman RS, Lieberman EH, Sullivan C, Zorn L, Flaker G, Schron E, Orav EJ, Goldman L (2000) The mode selection trial (MOST) in sinus node dysfunction: design, rationale, and baseline characteristics of the first 1000 patients. Am Heart J 140(4):541–551
Lehmann MH, Hardy S, Archibald D, quart B, MacNeil DJ (1996) Sex difference in risk of torsade de pointes with d, l-sotalol. Circulation 94(10):2535–2541
Liuba I, Jönsson A, Säfström K, Walfridsson H (2006) Gender-related differences in patients with atrioventricular nodal reentry tachycardia. Am J Cardiol 97(3):384–388
Loaldi A, Pepi M, Agostoni PG, Fiorentini C, Grazi S, Della Bella P, Guazzi MD (1983) Cardiac rhythm in hypertension assessed through 24 hour ambulatory electrocardiographic monitoring. Effects of load manipulation with atenolol, verapamil, and nifedipine. Br Heart J 50(2):118–126
Lown B, Wolf M (1971) Approaches to sudden death from coronary heart disease. Circulation 44(1):130–142
Makkar RR, Fromm BS, Steinman RT, Meissner MD, Lehmann MH (1993) Female gender as a risk factor for torsades de pointes associated with cardiovascular drugs. JAMA 270(21):2590–2597
Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, Carolei A (2005) Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke 36(6):1115–1119
McIntosh MA, Cobbe SM, Kane KA, Rankin AC (1998) Action potential prolongation and potassium currents in left-ventricular myocytes isolated from hypertrophied rabbit hearts. J Mol Cell Cardiol 30(1):43–53
Michelena HI, Powell BD, Brady PA, Friedman PA, Ezekowitz MD (2010) Gender in atrial fibrillation: ten years later. Gend Med 7(3):206–217
Molnar J, Zhang F, Weiss J, Ehlert FA, Rosenthal JE (1996) Diurnal pattern of QTc interval: how long is prolonged? Possible relation to circadian triggers of cardiovascular events. J Am Coll Cardiol 27(1):76–83
Movahed MR, Hashemzadeh M, Jamal MM (2005) Increased prevalence of third-degree atrioventricular block in patients with type II diabetes mellitus. Chest 128(4):2611–2614
Myerburg RJ, Interian A Jr, Mitrani RM, Kessler KM, Castellanos A (1997) Frequency of sudden cardiac death and profiles of risk. Am J Cardiol 80(5B):10F–19F
Myles RC, Wang L, Kang C, Bers DM, Ripplinger CM (2012) Local β-adrenergic stimulation overcomes source-sink mismatch to generate focal arrhythmia. Circ Res 110(11):1454–1464
Nabauer M, Gerth A, Limbourg T, Schneider S, Oeff M, Kirchhof P, Goette A, Lewalter T, Ravens U, Meinertz T, Breithardt G, Steinbeck G (2009) The Registry of the German Competence NETwork on Atrial Fibrillation: patient characteristics and initial management. Europace 11(4):423–434
Narayan SM (2006) T-wave alternans and the susceptibility to ventricular arrhythmias. J Am Coll Cardiol 47(2):269–281
Nishida K, Qi XY, Wakili R, Comtois P, Chartier D, Harada M, Iwasaki YK, Romeo P, Maguy A, Dobrev D, Michael G, Talajic M, Nattel S (2011) Mechanisms of atrial tachyarrhythmias associated with coronary artery occlusion in a chronic canine model. Circulation 123(2):137–146
Nogami A (2011) Purkinje-related arrhythmias part I: monomorphic ventricular tachycardias. Pacing Clin Electrophysiol 34(5):624–650
O’Donnell D, Cox D, Bourke J, Mitchell L, Furniss S (2003) Clinical and electrophysiological differences between patients with arrhythmogenic right ventricular dysplasia and right ventricular outflow tract tachycardia. Eur Heart J 24(9):801–810
Oliner L, Ballantine JJ (1968) Effect of human growth hormone on thyroidal secretion, radiothyroxine turnover and transport in man. J Clin Endocrinol Metab 28(5):603–607
Patel C, Yan GX, Antzelevitch C (2010) Short QT syndrome: from bench to bedside. Circ Arrhythm Electrophysiol 3(4):401–408
Piccini JP, Stevens SR, Chang Y, Singer DE, Lokhnygina Y, Go AS, Patel MR, Mahaffey KW, Halperin JL, Breithardt G, Hankey GJ, Hacke W, Becker RC, Nessel CC, Fox KA, Califf RM (2013) Renal dysfunction as a predictor of stroke and systemic embolism in patients with nonvalvular atrial fibrillation: validation of the R(2)CHADS(2) index in the ROCKET AF (Rivaroxaban Once-daily, oral, direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation) and ATRIA (AnTicoagulation and Risk factors In Atrial fibrillation) study cohorts. Circulation 127(2):224–232
Podrid PJ, Myerburg RJ (2005) Epidemiology and stratification of risk for sudden cardiac death. Clin Cardiol 28(11 Suppl 1):I3–I11
Pogwizd SM, Bers DM (2004) Cellular basis of triggered arrhythmias in heart failure. Trends Cardiovasc Med 14(2):61–66
Pogwizd SM, McKenzie JP, Cain ME (1998) Mechanisms underlying spontaneous and induced ventricular arrhythmias in patients with idiopathic dilated cardiomyopathy. Circulation 98(22):2404–2414
Priori SG, Aliot E, Blømstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P, Camm JA, Cappato R, Cobbe SM, Di MC, Maron BJ, McKenna WJ, Pedersen AK, Ravens U, Schwartz PJ, Trusz-Gluza M, Vardas P, Wellens HJ, Zipes DP (2002) Task Force on Sudden Cardiac Death, European Society of Cardiology. Europace 4(1):3–18
Psaty BM, Manolio TA, Kuller LH, Kronmal RA, Cushman M, Fried LP, White R, Furberg CD, Rautaharju PM (1997) Incidence of and risk factors for atrial fibrillation in older adults. Circulation 96(7):2455–2461
Pye MP, Cobbe SM (1992) Mechanisms of ventricular arrhythmias in cardiac failure and hypertrophy. Cardiovasc Res 26(8):740–750
Rautaharju PM, Zhou SH, Wong S, Calhoun HP, Berenson GS, Prineas R, Davignon A (1992) Sex differences in the evolution of the electrocardiographic QT interval with age. Can J Cardiol 8(7):690–695
Robinson RT, Harris ND, Ireland RH, Lee S, Newman C, Heller SR (2003) Mechanisms of abnormal cardiac repolarization during insulin-induced hypoglycemia. Diabetes 52(6):1469–1474
Rodriguez LM, de Chillou C, Schläpfer J, Metzger J, Baiyan X, van den Dool A, Smeets JL, Wellens HJ (1992) Age at onset and gender of patients with different types of supraventricular tachycardias. Am J Cardiol 70(13):1213–1215
Rohr S, Kucera JP, Fast VG, Kléber AG (1997) Paradoxical improvement of impulse conduction in cardiac tissue by partial cellular uncoupling. Science 275(5301):841–844
Saadeh AM (2004) Relation between age, ventricular arrhythmia, left ventricular hypertrophy and QT dispersion in patients with essential hypertension. Acta Cardiol 59(3):249–253
Sacherer M, Sedej S, Wakula P, Wallner M, Vos M, Kockskamper J, Stiegler P, Sereinigg M, von Lewinski D, Antoons G, Pieske B, Heinzel F (2012) JTV519 (K201) reduces sarcoplasmic reticulum Ca(2+) leak and improves diastolic function in vitro in murine and human non-failing myocardium. Br J Pharmacol 167(3):493–504
Sanders P, Kistler PM, Morton JB, Spence SJ, Kalman JM (2004) Remodeling of sinus node function in patients with congestive heart failure: reduction in sinus node reserve. Circulation 110(8):897–903
Saoudi N, Cosío F, Waldo A, Chen SA, Iesaka Y, Lesh M, Saksena S, Salerno J, Schoels W, Working Group of Arrhythmias of the European of Cardiology and the North American Society of Pacing and Electrophysiology (2001) A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical bases; a Statement from a Joint Expert Group from The Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J 22(14):1162–1182
Savelieva I, Kakouros N, Kourliouros A, Camm AJ (2011) Upstream therapies for management of atrial fibrillation: review of clinical evidence and implications for European Society of Cardiology guidelines. Part II: secondary prevention. Europace 13(5):610–625
Scher DL, Arsura EL (1989) Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment. Am Heart J 118(3):574–580
Shipsey SJ, Bryant SM, Hart G (1997) Effects of hypertrophy on regional action potential characteristics in the rat left ventricle: a cellular basis for T-wave inversion? Circulation 96(6):2061–2068
Sideris DA, Kontoyannis DA, Michalis L, Adractas A, Moulopoulos SD (1987) Acute changes in blood pressure as a cause of cardiac arrhythmias. Eur Heart J 8(1):45–52
Sideris DA, Chrysos DN, Maliaras GK, Michalis LK, Moulopoulos SD (1988) Effect of acute hypertension on the cardiac rhythm. Experimental observations. J Electrocardiol 21(2):183–191
Stevenson WG, Khan H, Sager P, Saxon LA, Middlekauff HR, Natterson PD, Wiener I (1993) Identification of reentry circuit sites during catheter mapping and radiofrequency ablation of ventricular tachycardia late after myocardial infarction. Circulation 88(4 Pt 1):1647–1670
Stewart GA, Gansevoort RT, Mark PB, Rooney E, McDonagh TA, Dargie HJ, Stuart R, Rodger C, Jardine AG (2005) Electrocardiographic abnormalities and uremic cardiomyopathy. Kidney Int 67(1):217–226
Takahashi A, Shiga T, Shoda M, Manaka T, Ejima K, Hagiwara N (2009) Impact of renal dysfunction on appropriate therapy in implantable cardioverter defibrillator patients with non-ischaemic dilated cardiomyopathy. Europace 11(11):1476–1482
Van Mierop LH (1967) Location of pacemaker in chick embryo heart at the time of initiation of heartbeat. Am J Physiol 212(2):407–415
Veglio M, Sivieri R, Chinaglia A, Scaglione L, Cavallo-Perin P (2000) QT interval prolongation and mortality in type 1 diabetic patients: a 5-year cohort prospective study. Neuropathy Study Group of the Italian Society of the Study of Diabetes, Piemonte Affiliate. Diabetes Care 23(9):1381–1383
Volders PG, Vos MA, Szabo B, Sipido KR, de Groot SH, Gorgels AP, Wellens HJ, Lazzara R (2000) Progress in the understanding of cardiac early afterdepolarizations and torsades de pointes: time to revise current concepts. Cardiovasc Res 46(3):376–392
Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA (1995) Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation 92(7):1954–1968
Witte KK, Cleland JG, Clark AL (2006) Chronic heart failure, chronotropic incompetence, and the effects of beta blockade. Heart 92(4):481–486
Xie Y, Sato D, Garfinkel A, Qu Z, Weiss JN (2010) So little source, so much sink: requirements for afterdepolarizations to propagate in tissue. Biophys J 99(5):1408–1415
Zhang Y, Ouyang P, Post WS, Dalal D, Vaidya D, Blasco-Colmenares E, Soliman EZ, Tomaselli GF, Guallar E (2011) Sex-steroid hormones and electrocardiographic QT-interval duration: findings from the third National Health and Nutrition Examination Survey and the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol 174(4):403–411
Zhao Z, Fefelova N, Shanmugam M, Bishara P, Babu GJ, Xie LH (2011) Angiotensin II induces afterdepolarizations via reactive oxygen species and calmodulin kinase II signaling. J Mol Cell Cardiol 50(1):128–136
Zipes DP (2005) Epidemiology and mechanisms of sudden cardiac death. Can J Cardiol 21(Suppl A):37A–40A
Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ, Priori SG, Quinones MA, Roden DM, Silka MJ, Tracy C, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL, Smith SC Jr, Jacobs AK, Adams CD, Antman EM, Anderson JL, Hunt SA, Halperin JL, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology, American Heart Association Task Force, European Society of Cardiology Committee for Practice Guidelines, European Heart Rhythm Association, Heart Rhythm Society (2006) ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Europace 8(9):746–837
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Heinzel, F.R., Pieske, B.M. (2014). Cardiac Arrhythmias. In: Wakabayashi, I., Groschner, K. (eds) Interdisciplinary Concepts in Cardiovascular Health. Springer, Cham. https://doi.org/10.1007/978-3-319-01074-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-01074-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01073-1
Online ISBN: 978-3-319-01074-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)