Abstract
Bacteria represent the earliest form of independent life on this planet. Bacterial development has included cooperative symbiosis with plants (e.g., Leguminosae family and nitrogen fixing bacteria in soil) and animals (e.g., the gut microbiome). It is generally agreed upon that the fusion of two prokaryotes evolutionarily gave rise to the eukaryotic cell in which mitochondria may be envisaged as a genetically functional mosaic, a relic from one of the prokaryotes. This is expressed by the appearance of mitochondria in eukaryotic cells (an alpha-proteobacteria input), a significant endosymbiotic evolutionary event. As such, the evolution of human life has been complexly connected to bacterial activities. Hence, microbial colonization of mammals has been a progressively driven process. The interactions between the human host and the microbiome inhabiting the gastrointestinal tract (GIT) for example, afford the human host the necessary cues for the development of regulated signals that in part are induced by reactive oxygen species (ROS) . This regulated activity then promotes immunological tolerance and metabolic regulation and stability, which then helps establish control of local and extraintestinal end-organ (e.g., kidneys) physiology. Pharmacobiotics , the targeted administration of live probiotic cultures, is an advancing area of potential therapeutics, either directly or as adjuvants. Hence the continued scientific understanding of the human microbiome in health and disease may further lead to fine tuning the targeted delivery of probiotics for a therapeutic gain.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Probiotics
- Gastrointestinal tract
- Inflammatory diseases
- Arthritis
- Dysbiosis
- Pharmacobiotics
- Mitochondria
- Endosymbiotic
- Microbiome
1 Introduction
The evolution of a primordial prokaryote that led to the development of the eukaryotic cell (i.e., acquisition of mitochondria) has been hypothesized as arising from an oxygen consuming bacterial ancestor (Dolan and Margulis 2007; Shih and Matzkeb 2013) by endosymbiosis. This has been reported as an event that highlights a significant evolutionary step that is obligatory for the continued symbiotic existence between bacteria, plants and animals, which is vital for life and survival on this planet.
During the twentieth century, there was an increasing dependency on antimicrobial compounds as mainstream therapy for bacterial infections. It is only somewhat recent that the focus of basic scientific and clinical research has moved beyond the premise that all bacteria are harmful to now clarifying the critical interrelationships that exist between the human host and its microbiome in regards to health/wellness and disease. This new understanding has redefined the interactions between gut microbes and vertebrates, now recognizing that the microbial active cohort and its mammalian host have shared coevolutionary metabolic interactions that span millennia.
At the time of birth, humans experience an induced proinflammatory beneficial event. The mediators of this encouraged activity is a fleet of bacteria that assault all mucosal and extramucosal tissue sites that include the mouth, hair, nose, ears, eyes, urogenital tract, lungs, GIT, and skin which express their own unique microbiomes (Dominguez-Bello et al. 2010) thus initiating effects that eventually provide the infant with immune tissue maturation . These effects occur beneath an emergent immune system surveillance and antigenic tolerance capability radar. Over time, continuous and regulated interactions with environmental, as well as commensal microbial, viral, and other antigens lead to an adapted and maintained symbiotic state of tolerance, especially in the GIT, the organ site of the largest microbial biomass.
The GIT is reported to harbor thousands of bacterial species while being the site of the most dense and diverse microbiome cohort known on the planet with an average of 1012−14 bacterial cells (predominantly in the large bowel) per wet weight of luminal content. Notwithstanding, recent reports suggest that the skin microbiome may be just as dense and complex (Grice and Segre 2011). The number of bacterial cells residing within and on the human body of the average healthy adult is estimated to outnumber human cells by a factor of 10 to 1.
Bacteria that colonize the GIT metabolically outperform somatic cells with enzymatic/metabolic activity, that include (1) triggering and regulating the normal development and function of the mucosal barrier (Xu and Gordon 2003); (2) assisting with the maturation of immunological tissues, which in turn promote immunological tolerance to antigens from the external environment/foods or potentially pathogenic organisms that are ingested or reside within the GIT (Berg and Savage 1975); (3) the control of nutrient metabolism and assimilation (Mazmanian et al. 2005; Rakoff–Nahoum et al. 2004), and (4) the prevention of the proliferation of pathogenic bacteria (Tappenden and Deutsch 2007). Early reports have hypothesized that changes in the profile of the resident GIT microbiota may reduce beneficial functions and affect the regulation of GIT immune and inflammatory responses (Pickering 1950). Hence, in addition to its inherited constitution of genes, the GIT microbiota together with environmental influence may comprise critical factors in disease causation (Pickering 1950).
2 Immunological Tolerance and the Control of Inflammation Originating from the GIT
Prebirth mammalian young were previously thought to be sterile in utero. However, a recent review has documented that neonatal colonization actually begins in utero (Rautava et al. 2012). Hence establishing clearly that mammals on this planet engage with bacterial species throughout a lifetime (Cert–Bensussan and Gaboriau–Routhiau 2010). In vivo studies with germ-free animals have confirmed the posit that antigenic tolerance has a bacterial triggered requisite. Comparative studies between mice that were raised in conventional versus germ-free environments highlight the importance of the intestinal microbiota for the development of the peripheral immune system in immunocompetent hosts (Hooper and MacPherson 2010). Most notably, the spleens of germ-free mice contain fewer and smaller germinal centers (Bauer et al. 1963) and decreased numbers of memory CD4+ T cells whose cytokine production demonstrates a Th2-type profile (Mazmanian et al. 2005). Moreover, a balanced microbiome prevents the growth of disease-causing bacteria within the intestine via a number of mechanisms. The GIT microbiota produce vitamins (e.g., vitamin K and B12) and are also important for maintaining the muscular activity of the small intestine. Specifically, studies reveal that the functions of the human GIT immune system are only partially encoded in the host’s genes and that cues are required from the symbiotic microbial cohort for its full development (Hooper 2004). The bacteria that colonize the adult human GIT hence function collectively as a metabolic organ (Backhead et al. 2007) and within this evolutionary paradigm, the development of an immune-metabolic-competent host may be a necessary response for survival. The microbiota that then colonize the human GIT exhibit a high phylogenetic diversity reflecting their immense metabolic potential. The mechanism by which bacteria colonize the GIT alludes to the cues required by the GIT to develop a regulated immuno-metabolic-competent profile. This basic scientific understanding reinforces the idea that bacteria can drive the epigenetic control of the host genome and hence host survival.
Upregulated immune responses in an individual are necessary to clear the GIT of pathogenic cells. The immune system achieves this by initiating a proinflammatory response . The microbiota act partly in an immune-surveillance role by detecting an overgrowth of pathogenic bacteria, stimulating the immune system and subsequently initiating an appropriate eradicative inflammatory response (Eckmann 2006). Once the pathogenic cells are reduced/cleared, anti-inflammatory signals are switched on to restore the pro-inflammatory response back to a normal level. Accordingly, the healthy gut is in a constant state of regulated inflammation . The role that the GIT microbiota play in triggering the anti-inflammatory response is still unclear. Accumulating evidence indicates that the balance of commensal bacteria within the GIT may be associated with the development of some GIT disorders (Swidsinski et al. 2002). Patients diagnosed with inflammatory bowel disease (IBD) or irritable bowel syndrome (IBS) have been reported to present with increased proinflammatory or potentially pathogenic bacterial species such as Escherichia coli (Mylonaki et al. 2005; Martin et al. 2004), members of the genus Bacteroides (Swidsinski et al. 2002) and Enterococci; and decreased Bifidobacteria and Lactobacilli species (Giaffer et al. 1991; Van de Merwe et al. 1988). For example, the etiology of IBD is not fully understood, but is considered to be a T-cell-driven inflammatory response resulting from a persistent preponderance of pro-over anti-inflammatory cytokine production (Hvas et al. 2007), whereas, Crohn’s disease (CD) is reported to be driven by an T-helper 1 (Th1) immune response (Matsuoka et al. 2004; Fuss et al. 1996) that can affect any part of the GIT, i.e., from the mouth to the anus. By contrast, ulcerative colitis (UC) is a T-helper 2 (Th2) driven response, and is restricted to the mucosa of the colon and rectum (Heller et al. 2005; Fuss et al. 1996). Figure 1 illustrates a diagrammatic view of the control of proinflammatory activity that is attenuated by probiotic live cultures.
Diagrammatic representation of GIT epithelial and mucosal homeostasis. Probiotic bacterial actions include those on epithelial cells, mucus producing cells, gap junctions between epithelial cells and integrity maintenance and the control of pathogenic bacteria. Multiple microbial pattern recognition receptors (e.g., TLR4 and TLR2) are known and are involved in supporting homeostasis by recognition and protection from opportunistic pathogenic infections and commensal bacterial tolerance. * G−Gram-negative G+ Gram positive
3 The Hygiene Hypothesis
The past 60 years has seen a significant increase in the prevalence of autoimmune diseases (Mackay et al. 2001; Sironi and Clerici 2010). This trend has triggered the formulation of the hygiene hypothesis that has been defined as a lack of early childhood exposure to infectious agents, symbiotic microorganisms (e.g., gut microbes or probiotic bacteria) and parasites that increases an individual’s susceptibility to allergic diseases by suppressing the natural development of tolerance by the immune system.
Over the past two to three decades, the hygiene theory has been tested and tweaked, expanded and extended (Sironi and Clerici 2010). This hypothesis provides a biologically plausible explanation for the trend that implicates diminished exposure in early childhood to those commensal infections that boost immune defenses while promoting tolerance. This deficit subsequently enhancing the risk for later life GIT proinflammatory shifts that disrupt normal regulated GIT inflammatory responses increasing the susceptibility to developing autoimmune diseases (Bach 2002).
This proposed postulation of reduced early childhood exposure to infections is possibly linked to diminished family size and better personal hygiene, which may contribute to decreased antigenic tolerance and a concomitant increase in the risk of developing allergic disease (Bach 2002). The interface of the microbial environment with the Innate immune system can be significantly modulated so that its ability to impart instructions to adaptive/regulatory immune/inflammatory responses are adversely affected, particularly when such interactions occur in utero and or are presaged in early life. Bach (2002) documented this trend highlighting that an epidemic of both GIT autoimmune diseases in which the immune response was dominated by Th1 cells (such as type 1 diabetes mellitus, CD, multiple sclerosis) or allergic diseases in which the immune response was dominated by Th2 cells (such as asthma, allergic rhinitis, and atopic dermatitis) were becoming increasingly prevalent in Western communities.
Evolution has naturally endowed the human species with immune/inflammatory regulatory mechanisms activated by the interactions with both the external and internal microbial environments. These then serve to fine-tune both Th1 and Th2 antigen-driven effector responses (Wills–Karp et al. 2001). The innate immune system samples the environment and accordingly modulates the T regulatory arm, the ultimate keeper of the balance between antigen tolerance and responsiveness. The efficiency of the regulatory interface in its current state would paradoxically be jeopardized by a decrease in the microbial burden that the immune system has coevolved with (Wills–Karp et al. 2001).
Studies exploring the molecular mechanisms that might underpin the hygiene hypothesis have focused mostly on the interactions between bacterial products and Toll-like receptors (TLRs) —the main transducers of microbial signals to the innate immune system and critical regulators of CD4+ T-cell activation and regulation (O’Neill 2006; Pasare and Medzhitov 2004) (Fig. 1). Therapeutically, a recent review has highlighted how individuals with chronic helminth infections often have a reduced prevalence of inflammatory disorders, including allergic diseases (Hussaarts et al. 2011). Mechanistically, it is purported that inducing or expanding regulatory B cells with helminth infection , novel avenues for the treatment of inflammatory diseases such as allergic asthma are revealed (Hussaarts et al. 2011).
4 The Influence of Probiotic Therapies
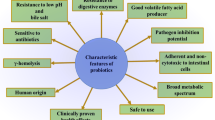
The World Health Organization and others have defined probiotics as live bacterial cultures that when consumed in foods (e.g., yogurts ) and dietary supplements can improve the health of the host beyond their inherent basic nutritional content (Fuller 1989; Morelli and Capurso 2012).
Perhaps the most studied site for investigating probiotic efficacy is the GIT and inflammatory conditions such as CD, UC, and IBS. It has been reported that probiotic bacteria may operate on three levels of host functionality that enhances GIT and extraintestinal activity (Fig. 1) namely by (a) interfering with the growth of pathogenic bacteria in the lumen of the GIT; (b) strengthening gut epithelial barrier function and mucosal immunity as well as mucus production ; and (c) beyond the gut influencing both the systemic immune and organ systems such as the liver, brain, and heart. A series of clinical trials (reviewed elsewhere c.f. Vitetta et al. 2014a, b) that implemented various combinations of probiotic species frequently demonstrated efficacy in treating GIT conditions/diseases and various other end-organ tissues (Vitetta et al. 2014a, b). The core notion emanating from the reviews was the administration of multistrain probiotic formulations could, in addition to improving GIT function, influence numerous end-organ tissues beneficially. Furthermore, clinical studies indicate that administration of probiotic bacterial species provides efficacious results in restoring the GIT microbiome to a more balanced metabolic state. This possibly achieved in part by reducing pathogenic bacterial overgrowth and the resulting adverse localized effects that in turn affect end-organ physiology.
It is postulated that a dysbiotic GIT , induced by a microbiome drift toward an overgrowth of pathogenic bacteria , may play a significant role in the induction of pro-inflammatory mediators that begin in the GIT and then may affect different end-organs as shown in Fig. 2. For example, disruption of the GIT epithelial barrier that accompanies chronic anti-inflammatory/analgesic (e.g., NSAIDs) medication use or over prescription of others (e.g., antibiotics) exacerbates local proinflammatory responses induced by the pathogenic commensal cohort . This activity can further disturb GIT physiological and epithelial barrier function leading to disruption of controlled pro-inflammatory actions.
The rescue of an adversely affected GIT microbiome may depend on the introduction of a multistrain probiotic rather than that of single strains. Given the extensive array of microorganisms that inhabit the GIT, probiotic combinations may be a more biologically plausible therapeutic option in rescuing GIT microbiome aberrant functionality. Recently, it was reported that multistrain probiotics may appear to be more effective against a wide range of end points (Chapman et al. 2011). Chapman et al. (2011) also reported that based on a limited number of studies, multistrain probiotics may show greater efficacy than single strains, including strains that are components of the mixtures themselves demonstrating an additive effect.
A problem with probiotic therapy is ascertaining and correctly administering the optimal therapeutic dose for the condition being treated. As each probiotic species/strain has been clinically trialed using variable dose concentrations for varying disease etiologies, defining the ideal dose is complex. To assess the efficacy of probiotics, improvements in disease outcome measures have been assessed. Whorwell and colleagues (2006) investigated the effects of three different doses of Bifidobacterium infantis 35624 (1 × 106, 1 × 108 and 1 × 1010, CFU/mL) in treating primary-care IBS patients. The dose of 1 × 108 CFU/mL proved superior in relieving abdominal pain compared with the placebo and other doses. Further investigation of the highest dosage demonstrated that the probiotics coagulated into a firm glue-like mass making them resistant to acid and agitation. The lowest dose of probiotics may not have been effective because of the duration of the study, or insufficient biological activity. These findings highlight the potential importance of how probiotics are dosed and administered in order to maximize bioavailability within the GIT.
Probiotics have been shown to reduce abdominal pain , discomfort , and symptom scores in patients with IBS when administered Lactobacillus acidophilus (Sinn et al. 2008), Lactobacillus plantarum 299 V (Niedzielin et al. 2001), or ProSymbioflor (a combination of E. coli DSM 17252 and Enterococcus faecalis DSM 16640 ) (Enck et al. 2008) compared with a placebo. In contrast, Drouault-Holowacz and colleagues (2008) found that Bifidobacterium longum LA 101, L. acidophilus LA 102, Lactobacillus lactis LA 103 and Streptococcus thermophilus LA 104 were not superior to the placebo treatment for relieving disease symptoms except that of abdominal pain, due to a strong placeboFootnote 1 effect. Further analysis of the IBS subgroups revealed that patients with changing bowel habits (alternating between constipation and diarrhea and those with short durations of symptom exacerbation and remission) reported significantly less abdominal pain with constipation-predominant IBS patients reporting improved bowel motions. These results indicate that different disease etiologies may exist between IBS subgroups and that some probiotics may be more efficient than others for treating symptoms within these subgroups. These findings also point to the need to further classify patients into relevant sub groups whenever possible for assessing the efficacy of a probiotic.
A number of studies investigating the effects of probiotics within specific subgroups of IBS have shown the beneficial effects of probiotic supplements . Therefore, Zeng and colleagues (2008) first separated patients with IBS into sub groups (those with increased small bowel permeability and those with increased colonic permeability), treating diarrhea-predominant IBS patients with S. thermophilus and Lactobacillus bulgaricus , Lactobacillus bulgaricus and B. longum . The proportion of patients with increased small bowel permeability (lactulose/mannitol ratio >0.025) decreased significantly (p < 0.023) after treatment. These patients also demonstrated improved IBS scores with diminished abdominal pain and flatulence. Similarly, symptoms improved after treatment with the probiotic VSL#3 in subjects with either diarrhea-predominant IBS (Kim et al. 2003) or IBS with bloating (Kim et al. 2005). In subjects complaining of IBS with bloating, the VSL#3 reduced flatulence scores and retarded colonic transit time , without altering bowel function. In patients with diarrhea-predominant IBS , VSL#3 only relieved abdominal bloating, having no effect on mean transit measures, bowel function scores or satisfactory relief of symptoms. VSL#3 has also been shown to be superior to a placebo in children with IBS. VSL#3 supplementation improved overall IBS symptoms as assessed by abdominal pain/discomfort, abdominal bloating/gassiness, and on family life disruption.
To date, monitoring disease symptoms is usually employed to assess the efficacy of probiotics in conditions such as IBS and IBD. These subjective measures, usually self-assessed by the patients, have provided slight indications of the underlying mechanisms of probiotics or the disease etiology. In an attempt to understand the physiological mechanisms of probiotics, Kajander and colleagues (2005, 2008) administered patients with IBS a mixture of probiotic species/strains containing Lactobacillus rhamnosus GG, L. rhamnosus LC705, B. breve Bb99 and Propionibacterium freudenreichii ssp. shermanii JS (Kajander et al. 2005) or L. rhamnosus GG, L. rhamnosus Lc705 (DSM 7061), P. freudenreichii ssp. Shermanii JS (DSM 7067), and Bifidobacterium animalis ssp. lactis Bb12 (Kajander et al. 2008). Serum C-reactive protein and pro- and anti-inflammatory cytokines (IFN-γ, TNF-α, IL-2, IL-4, IL-6 and IL-10) concentrations were generally below the limit of detection, and therefore did not indicate any differences between the treatment groups (Kajander et al. 2008). Both studies did, however, report an improvement in the IBS scores from baseline, particularly for distention and abdominal pain. The IBS score had at 5 months decreased by 14 points (−19 to −9) with the multispecies probiotic versus 3 points (−8 to 1) with placebo (P = 0.0083). Moreover, the study also reported that there was a stabilization of the GIT microbiota as the microbiota similarity index increased with the probiotic supplementation (1.9 ± 3.1), while it decreased with placebo (−2.9 ± 1.7).
In contrast to the benefits of probiotics in relieving IBS symptoms, other studies report few or no beneficial effects of probiotics. O’Mahony and colleagues (2005) found disparate effects when providing L. salivarius UCC4331, B. infantis 35624, or a placebo to subjects with IBS and to healthy volunteers. Following supplementation, the composite score (weeks 1–8), pain/discomfort (at weeks 1, 2, 4, 5, and 7), bloating/distention (at weeks 2, 5, and 6), and difficulty with bowel movements (at weeks 2, 3, 5, and 6) were generally lower in the B. infantis group than in the placebo (malted milk drink) group. Composite score was only lower in the L. salivarius group than the control group in the second week of supplementation, indicating that the effects of L. salivarius were short-lived and intermittent. In vitro production of IL-10 and IL-12 by isolated mononuclear cells (peripheral blood mononuclear cells [PBMC]) from whole blood was a proinflammatory profile at baseline in patients with IBS. Patients with IBS had low levels of IL-10 and high levels of IL-12 synthesis compared with healthy volunteers. Notably, however, supplementation with B. infantis restored IL-10 and IL-12 syntheses to levels similar to those observed in healthy volunteers.
To understand the apparent lack of effect of probiotics in some clinical studies, it is essential that the placebo effect or natural healing cycle needs to be critically considered. Niv and colleagues (2005) provided Lactobacillus reuteri ATCC 55730 or a placebo to subjects with IBS. Following supplementation, an improvement in IBS symptoms was reported. However, a similar response occurred in the placebo group (treatment versus placebo P = 0.0714 and P = 0.0971, respectively). This may demonstrate a strong placebo effect or stimulation of the natural healing cycle of the disease allowing some IBD and IBS patients to more frequently enter periods of remission. Notwithstanding, the overall therapeutic effect of probiotics in humans supports beneficial findings. While some results were inconsistent, probiotic treatment generally reduced symptoms of IBS, particularly abdominal pain, and restored the balance of pro- and anti-inflammatory cytokines.
5 The GIT, Probiotics and End-Organ Physiology
Table 1 presents an overview of clinical studies that have administered a probiotic strains (formulations) and have reported improvements on numerous conditions and symptoms in various organ systems (c.f. Vitetta et al. 2014b).
5.1 Probiotics and the Liver
It has recently been reported that there exists a gut–liver axis that suggests the GIT microbiota may significantly affect liver physiology and act as a cofactor in the etiology of chronic liver disease (Loguercio et al. 2002). This hypothesis has stemmed largely from the long-standing practice of using lactulose in the treatment of hepatic encephalopathy (Polson and Lee 2005). This suggests that the gut microbiota is intimately involved in the management of chronic liver disease . A GIT microbiota that sustains a persistent low-level proinflammatory pathogenic profile could modulate liver damage caused by ethanol and other toxic compounds such as acetaldehyde, phenols and endotoxins. We have reviewed the clinical evidence of studies that have employed probiotics in the treatment of chronic liver diseases reporting significant improvements (c.f. Vitetta et al. 2014b). Clinical studies that demonstrated efficacy were related to improving endotoxaemia that in turn improved liver functionality. It would seem that the probiotic actions most relevant to chronic liver diseases were modification of intestinal barrier function and the prevention of bacterial/toxin translocations . Increased GIT overloads with Gram-negative bacteria, increased permeability and impaired immunity may all contribute to increased bacterial/toxin translocations. Furthermore, a strong correlation between the rate of bacterial/toxin overload and the severity of cirrhosis has been demonstrated. Hence, the combined clinical studies seem to suggest that multistrain probiotics may alter gut microbiota and rescue the GIT microbiome toward a protective commensal profile with a concomitant increase in GIT epithelial barrier function.
5.2 Probiotics and Obesity
In vitro screening experiments with bacteria from the genus Lactobacillus and Bifidobacteria isolated from the human GIT have demonstrated significant cholesterol-lowering actions (Pereira and Gibson 2002). Recent research findings suggest that a high-fat diet and the GIT bacterial cohort interact to promote early inflammatory changes in the gut that contribute to the development of obesity and insulin resistance (Ding and Lund 2011).
Clinical studies investigating probiotic preparations in obesity (c.f. Vitetta et al. 2014b) have reported an overall trend that demonstrates probiotic preparations could positively influence weight reduction. Particularly, in a study with healthy infants (Chorell et al. 2013) it was demonstrated that probiotic administration significantly lowered levels of palmitoleic acid and significantly increased levels of putrescine . The data suggested that palmitoleic acid a major monounsaturated fatty acid that has strongly been linked to visceral obesity was reduced with probiotic supplementation whereas putrescine an important polyamine with importance for gut integrity was beneficially increased. Probiotic supplementation in adulthood (Kadooka et al. 2010) and during childhood (from birth to 10 years) (Luoto et al. 2010) demonstrated that probiotics in part assisted with the metabolic control of abdominal visceral and subcutaneous fat. In an additional study, administration of a multispecies probiotic supplement provided a synergistic effect on overweight and obese individuals when provided with a weight loss diet (Zarrati et al. 2013). In a further study with overweight children , a multispecies probiotic and prebiotic (synbiotic) formulation demonstrated a significant decrease in blood lipid profiles (Safavi et al. 2013).
Mechanistically, Tien et al. (2006) have reported that the anti-inflammatory effects of Lactobacillus casei were aLactobacillus caseisociation with NF-κB activation. Therefore, suggesting that the health properties of probiotics could be related to peroxisome proliferator-activated receptor gamma (PPAR-g) activation , which then blocks the activity of NF-κB (Amaral et al. 2008; Nakamura and Omaye 2012). Interestingly the overconsumption of food triggers GIT proinflammatory bacterial activity; this then may induce GIT metabolic dysfunction increasing the risk of metabolic diseases . Whereas, a balanced diet with an optimally balanced GIT microbiota that promotes regulated/controlled PPAR-g activation could alleviate or suppress the risk of developing metabolic diseases such as T2DM.
5.3 Probiotics and the Brain
There is an increasing body of preclinical evidence supporting the important role that the gut microbiota plays in influencing emotional behavior as well as monitoring underlying brain mechanisms (c.f. Vitetta et al. 2014b). Studies with germ-free mice have demonstrated the important role of the gut microbiota in brain development and resultant adult pain responses and emotional behaviors, as well as on adult hypothalamic–pituitary axis responsiveness. Of the scant clinical trials that have investigated probiotics and brain function, the results have shown significant improvement in behavior with probiotic administration (c.f. Vitetta et al. 2014b). In one study, assessing patients with traumatic brain injury , probiotic supplementation improved the anti-inflammatory clinical picture (Tan et al. 2011).
5.4 Probiotics and Joint Disease
Patients diagnosed with joint diseases have been reported as being predisposed to GIT disturbances (Lee et al. 2010). There are a small number of human clinical trials that have assessed the therapeutic efficacy of administering probiotics to patients with autoimmune arthritic diseases (c.f. Vitetta et al. 2014b). However, there are no clinical studies that have investigated the role of probiotics in reducing the symptoms of osteoarthritis . A recent animal study however has provided plausible data that the probiotic species L. casei could act as a potent nutraceutical modulator for the treatment of osteoarthritis. Pain was reduced, as were inflammatory responses and articular cartilage degradation (So et al. 2011).
5.5 Probiotics and Respiratory Diseases
Respiratory allergies include allergic rhinitis , sinusitis and asthma . As previously presented herein, the advent of the hygiene hypothesis has proposed that the increase in allergic diseases reflects a decrease in infections during childhood. Clinical trials have also suggested that the exposure to microbes through the GIT robustly shapes immune function (Dominguez-Bello et al. 2010). Probiotics have been reported to exert a beneficial effect in the prevention as well as the treatment of allergic diseases through modification of the immune system of the host via the GIT ecosystem. This has prompted studies of feeding probiotics in the prevention as well as the treatment of respiratory allergies (c.f. Vitetta et al. 2014b). The clinical data presents a contentious profile of probiotic efficacy. In a recent controlled study, it was reported that long-term consumption of fermented milk containing L. casei may improve the health status of children with allergic rhinitis, however no effect was found in asthmatic children (Giovannini et al. 2007).
5.6 Probiotics and Skin Conditions
Lactobacillus rhamnosus GG has been reported to reduce clinical symptoms, intestinal inflammation and mucosal barrier permeability in infants with allergic dermatitis (MacDonald and Sabatino 2006).
Allergic conditions are caused by abnormal or exaggerated immune reactions of the skin . A range of symptoms can be expressed however the most common chronic allergic conditions of the skin are atopic dermatitis/eczema . Probiotics are reported to exert some benefit in such conditions, which is thought to be due to the immune modulating effects of the bacteria. Studies demonstrate that probiotics contribute to relief of symptoms and also prevention of atopic conditions in infants (c.f. Vitetta et al. 2014b). In one study, a probiotic preparation induced the repair of ultra violet damaged skin (Bouilly-Gardner et al. 2010).
5.7 Probiotics and Chronic Kidney Disease (CKD) [See Further Sect. 6]
Dysfunction of the kidneys leads to disturbed renal metabolism impaired glomerular filtration and tubular secretion/reabsorption problems. This results in the retention of toxic solutes, which affect all organs of the body. It has been posited that toxins generated by gastrointestinal dysbiosis, and introduced into the body via the small and large bowel, may all contribute to CKD. They comprise advanced glycation end products, phenols, and indoles (Vitetta and Gobe 2013). Moreover, recent reports suggest that the bacterial load and the adverse products of the intestinal microbiota might influence chronic disease pathogenesis (Wu et al. 2005; Arumugam et al. 2011). This is particularly relevant to the development of CKD, a disease of increasing prevalence in many Western societies. It has also been recently reported that the pharmacobiotic potential of the GIT micro-biometabolome may provide a plausible therapeutic role with the administration of live multistrain probiotic cultures (Vitetta and Alford 2013).
Although current evidence of probiotic efficacy in reducing uremic toxins is limited, clinical evidence does demonstrate that specific strains in a multiple species matrix configuration, in combination with prebiotics , may be most beneficial in reducing gut-derived uremic toxins (c.f. Vitetta et al. 2014b). In addition, selecting and administering probiotic species with known metabolic functions, such as Streptococcus thermophilus , for metabolizing urea as a nitrogen growth source, could contribute to reducing uremia.
5.8 Prebiotics
The introduction of prebiotics in Japan and Europe as food additives point to the need for further controlled clinical studies before prebiotics can be unequivocally recommended as a food additive for infant formulas and yogurts or as dietary supplements that should be consumed on a daily basis. No human studies have been conducted to confirm the suggested in vitro and animal study effects of prebiotics on carcinogenesis. Long-term trials with prebiotics, perhaps among patients with chronic digestive diseases such as colon cancer-prone patients, would certainly be useful (de Vrese and Schrezenmeir 2008).
The symbiotic effect of combining prebiotics with probiotics needs to be further evaluated and quantified. Such studies could include investigations as to whether there is altered bacterial colonization in the gut following the ingestion of both prebiotics and probiotics. For example, by determining the natural adaptation of the gut to recolonization with commensal bacteria and their growth-promoting nutrients (after pre/probiotic treatment) may establish how dietetic influences could influence the pathogenesis of inflammatory diseases of the digestive system.
The FAO/WHO Expert Consultation and Working Group on probiotics presented their recommendations to Codex (Pineiro et al. 2007) with the hope that these will be used for a science-based risk assessment process for managerial decisions concerning probiotics.
The resolution of some human diseases does not reside solely within the host but rather could involve the host’s interface with the microbial environment. Manipulating the gut microbial cohort is a realistic therapeutic and prophylactic strategy for many infectious, inflammatory and neoplastic diseases within the gut. But the promise of pharmacobiotics (therapeutic exploitation of the commensal cohort) is only likely to be fulfilled following greater attention to the endogenous enteric microbiome. The GIT microbiome is certainly an affluent repository of metabolites that can be exploited for therapeutic benefit. Elucidating the molecular details of host–gut microbiome interactions is therefore, a prerequisite for a bacterially derived metabolite program of discovery and control of GIT inflammation. Reports that have demonstrated dietary neosugar, a fructooligosaccharides non-nutritive sweetener can significantly influence the feacal microbiome and activities of reductive enzymes (Buddington et al. 1996) certainly warrant further study.
5.9 Synbiotics
Synbiotics are products that contain both a probiotic and prebiotic component (Bengmark and Martindale 2005; Scholz–Ahrens et al. 2007). The rationale for such combined formulations is to enhance the survival of probiotic bacteria in transit through the proximal GIT; improve colonization of the probiotics in the large bowel and to induce a stimulating effect on the growth of the endogenous microbiome as well (Bengmark and Martindale 2005). This effect may rescue the GIT from a dysregulated inflammatory response that may increase risk of disease.
6 Commensal GIT Bacteria/Probiotics Cellular Signaling and Macromolecular Redox Changes—Chronic Kidney Disease as an Exemplar
Over the last decade, oxidative stress has been proposed to play a major role in the development of co-morbid conditions such as cardiovascular disease (CVD) among, for example, renal failure patients (Himmelfarb et al. 2002; Terawaki et al. 2004), advocating that antioxidant strategies should become part of the treatment for pre-dialysis renal failure (Rutkowski et al. 2007). Additionally, it has been proposed uremic toxins and oxidative stress play significant roles in the development of uremia and its complications (Vanholder et al. 2003). Thus, the concept of oxidative stress being a major deleterious player in all manner of situations has been massively supported by expansive literature (Rutkowski et al. 2007; Chiang et al. 2012; Dounousi et al. 2006). We assert this is incorrect. Reactive oxygen species (ROS) are known to play a major role in maintaining normal physiological function (Linnane et al. 2007). The investigations on protein albumin thiol oxidations and serum protein carbonyl formations indicate that these biochemical events progressively increase with advancing stages of CKD (Dounousi et al. 2006), leading to the conclusion that there exists a close association between oxidative stress and carbonyl formation and that there is a correlation with carbonyl formation and renal dysfunction among pre-dialysis CKD patients (Dounousi et al. 2006). This inference further nurtures support for the administration of antioxidant therapies. However, there are no reported clinical trials that support this conclusion, indeed studies on the protective antioxidant role of administered alpha lipoic acid for the prevention of contrast-induced nephropathy in diabetic patients demonstrated no benefit (Cicek et al. 2013). A recent systematic review and commentary reported that antioxidant therapy with vitamin C does not reduce the risk of death or cardiovascular events overall in CKD, but that possibly may benefit people with more advanced kidney failure (Jun 2013). It has been (LV, AWL c.f. extensive review) (Linnane et al. 2007) previously considered and challenged that the commonly held view that proteins are randomly oxidized in an uncontrolled process by superoxide anion, hydrogen peroxide, nitric oxide, and peroxynitrite, thereby contributing directly to the development of chronic diseases and the aging process is a simplistic view of complex physiological processes. It was concluded that this concept is not tenable and it is in error, misrepresenting stringently regulated cellular redox metabolism.
The oxidation of protein amino acid residues , since their discovery some decades ago, has been almost universally reported as leading to protein inactivation and requiring mandatory proteolysis to prevent their deleterious cellular accumulation. It is clear that oxidatively modified proteins do not simply arise as the result of random oxidative damage (hydroxylations of various amino acid residues, sulphoxidation of methionines, nitrosylations of sulphydryl groups, and so on). There is an increasing number of situations where free radical protein modifications can be shown to be part of normal cellular regulatory signaling activity. To support these conclusions, some examples follow.
6.1 Specific Protein Oxidations
-
i.
One of the most sensitive amino acids to oxidation is methionine , being converted to methionine sulfoxide . This phenomenon is commonly cited as an example of random oxidative damage to proteins. The following example would bring such an overriding conclusion into serious question. Calmodulin function and its regulation by superoxide anion/hydrogen peroxide oxidation of specific methionine residues is well-documented (Yin et al. 1999). The oxidation of only two of the seven specific methionine residues (144 and 145) of calmodulin is involved in the process of down-regulating plasma membrane-Ca++ATPase . Using genetically engineered calmodulin in which the two methionines (144, 145) were replaced by glutamines, it was shown that oxidation of the remaining methionines did not significantly downregulate calmodulin-plasma membrane-Ca++ATPase activation (Yin et al. 2000). It has also been reported from the same laboratory (Sun et al. 1999) that methionine sulfoxide reductase can act reductively to restore the ability of oxidized calmodulin to regulate plasma membrane-Ca++ATPase. These results showed that superoxide anion and/or hydrogen peroxide are functioning as part of the controlled regulation of the calmodulin-plasma membrane-Ca++ATPase complex. Further that proteasomal degradation of oxidized calmodulin, when and where it occurs, is part of the normal process of regulated protein turnover. Protein turnover is rigidly controlled, some proteins turnover in minutes, others in hours and longer, but all these proteins are part of a system tightly regulated by the ubiquitin/proteasome system.
-
ii.
The turnover of the hypoxia-inducible factor-alpha (HIFα) and its proteasome degradation is clearly regulated by hydroxylation of its prolyl residues (Stolze et al. 2006). This is an ordered process involving signaling by the free radical system comprised of superoxide anion, nitric oxide and peroxynitrite .
-
iii.
Bota et al. (Bota et al. 2002, 2005) have reported that mitochondrial aconitase is preferentially oxidatively modified and inactivated, and that the ATP activation of the mitochondrial Lon protease specifically acts to degrade the oxidized inactivated enzyme. The authors interpret their results as demonstrating the toxicity of ROS. We believe that this conclusion is in error; rather their results demonstrate how tightly regulated is the formation of ROS and its directed activity in regulating the metabolome. The controlled specific degradation of aconitase (among the hundreds of mitochondrial proteins ) to regulate citric acid cycle activity is an excellent example of the regulatory role that ROS play in the modulation or control of the metabolome, and that ROS do not randomly contribute to the damage or degradation of cellular metabolic processes.
-
iv.
Consider the nitrosylation of sulphydryl groups, proposed as a damaging phenomenon. We have previously referred to and sited the hemoglobin system as a remarkably regulated machine, finely tuned allosterically for the carriage of the daily massive amounts of inhaled oxygen from lungs to cells (Linnane et al. 2007). It is now recognized that hemoglobin undergoes subtle but critical changes as result of sequential reactions with dioxygen, protons and CO2 to regulate the delivery of oxygen to the tissues. As part of this process, it is relatively recently recognized that NO• participates in the regulation (Singel et al. 2005). In the cyclic oxygen carriage by hemoglobin, NO• reacts with the b subunit ferrous ions. Subsequently on the b subunit binding of dioxygen , the NO• is displaced to nitrosylate the cys 93 thiol group of the hemoglobin b subunit. These changes are accompanied by an allosteric change from the T (tense) to the R (relaxed) form. The various allosteric changes which hemoglobin undergoes are now recognized as of the utmost importance to hemoglobin function. They are the outcome of over 80-years study (that includes the Bohr effect/Perutz X ray structural studies/the detailed effector allosteric inducers, namely H+, CO2, O2, NO•, 2;3-bisphosphoglycerate /and the allosteric positive and negative cooperative changes that occur) (Linnane et al. 2007). Suffice for here, is that the recently recognized NO• nitrosylation of hemoglobin is part of the normal physiological transport of oxygen delivery to tissues; nitrosylation of proteins is not conditionally deleterious. Parenthetically, it may be added that superoxide anion continually formed in small amounts during the process oxidizes hemoglobin to meet hemoglobin in the order of a steady-state amount of 1–3 %. The met hemoglobin formed is itself continually reduced back to hemoglobin by erythrocyte met hemoglobin reductase to maintain regulated oxygen homeostasis.
-
v.
Farout and Friguet (Farout and Friguet 2006) have considered that there is an age-related deleterious accumulation of oxidized proteins resulting from impaired redox homeostasis and proteolysis. Further, they consider that changes in proteasome structure with increasing age and dysfunction of the proteasome leads to an exacerbated accumulation of oxidatively modified proteins due to their impaired proteolysis . Somewhat contrary to this interpretation, it has been reported when cellular proteasome activity is inhibited, the resultant decrease in its activity leads to a concerted increase in cellular synthesis of the proteasome (the phenomenon of hormesis) (Meiners et al. 2003). Husom et al. (2004) have reported an increase in the 20S proteasome in aged rat skeletal muscle, albeit with some change in function.
It is suggested that the proteasome activity and changes in structure with increasing age and organ dysfunction (for example, in the kidneys and the gut epithelium) be viewed from a different perspective. The proteasome system makes a major demand on the available cellular ATP and will become increasingly dysfunctional in the absence of sufficient ATP substrate. Central to any consideration of aging and its outworking is the universally recognized decline in bioenergy capacity with age from increasingly dysfunctional mitochondria (DNA mutations and deletions). Arising from this consideration, declining ATP availability leads to declining proteasome function which contributes to the multisystem aging process, that includes single organ dysfunction, albeit not as a primary effector and not as a direct result of oxygen radical damage to proteins. Furthermore, with the increasing understanding of the upstream regulation of the superoxide anion/hydrogen peroxide second messenger system, it is becoming increasingly apparent that they play a major role in the ordered regulation of proteolysis and protein homeostasis; and that the damage process is far from random.
6.2 The Antioxidant Effect
Vitamin C has long been promoted as an outstanding antioxidant and of benefit in the prevention or amelioration of age-associated diseases proposed arising from oxygen radical damage. There is no doubt that vitamin C is an essential nutritional supplement required for normal mammalian function but it has yet to be demonstrated by clinical trial that it has any role as a meaningful therapeutic antioxidant.
Ascorbic acid plays an essential co-enzyme oxidoreductase role in the hydroxylations of pro-collagen (pro-collagen trimer formation and release from the endoplasmic reticulum), dopamine (to give rise to norepinephrine), and HIF (regulation). Ascorbate occurs in high concentration in the adrenal and pituitary glands but it is not evenly distributed throughout mammalian tissues. Its occurrence is low in tissues such as skeletal muscle, testes, thyroid and lung (Hornig et al. 1975), so that it would not constitute a general endogenous tissue antioxidant, if that were its proposed antioxidant role. Recently, it was reported that administered ascorbate acts as a pro-oxidant during surgical ischemia-reperfusion (Bailey et al. 2006). On the contrary in large doses it may act as a pro-drug for the production and delivery of H2O2 to tissues, especially as has been reported for the treatment of some cancers (Chen et al. 2005). There is no convincing clinical evidence for ascorbic acid acting beneficially in mammals as an antioxidant. Furthermore and importantly, vitamin C has been demonstrated to directly inhibit bacterial spreading factor (Li et al. 2001). In that study vitamin C was reported to competitively inhibit hyaluronan degradation by Streptococcus pneumoniae hyaluronate lyase , highlighting a compound capable of inhibiting a pathogenic bacterial enzyme in order to maintain homeostasis.
6.3 Commensal/Probiotic Bacteria and Mechanism of Action
CKD has been recently linked to severe disruption of the gut epithelial tight junction barrier (Vaziri et al. 2012; Vinik et al. 2011) with oxidative stress the reported primary factor that drives metabolic abnormalities that contribute to CKD development (Vinik et al. 2011).
It is extensively reported that probiotics can temper a range of GIT physiological functions, including control over immune responses, epithelial barrier function , and cellular proliferation (Vitetta et al. 2012). A recent study has demonstrated that some genera of human GIT bacteria can induce a rapid increase of ROS, eliciting a physiological response through the activation of epithelial NADPH oxidase-1 (Nox1) (Bermudez-Brito et al. 2012; Neish 2013). In addition, reports cite in vitro experiments with epithelial cells that, when co-cultured with specific probiotic bacteria, show an increased and rapid oxidation reaction of soluble redox sinks, namely glutathione and thioredoxin (Bermudez-Brito et al. 2012; Neish 2013) that indicate the presence of a regulated process. This effect was demonstrated as an increase in the oxidoreductase reaction of transcriptional factor activations such as NFκB, NrF2 and the antioxidant response element, reflecting a cellular response to increased ROS production that is regulated (Bermudez-Brito et al. 2012; Neish 2013). This effect must be decisive in order to elicit a restrained anti-infective response with a minimal chance of proinflammatory damage to the tissue. These reactions define potent regulatory effects on host physiological functions that include immune function and intracellular signaling.
The reported mechanisms of action of probiotics are similarly aligned acting to enhance the epithelial barrier, increased bacterial adhesion to the intestinal mucosa , with an attendant inhibition of pathogen adhesion to the competitive exclusion of pathogenic microorganisms ((Bermudez-Brito et al. 2012; Neish 2013; Lin et al. 2009a; Lee 2008; Yan et al. 2007; Patel et al. 2012; Collier-Hyams et al. 2005). Furthermore, probiotic species have also been reported to generate a range of antimicrobial substances and to positively affect and modulate immune system function. Lee (2008) has reported that the enteric commensal bacteria , by rapidly generating ROS, negotiate an acceptance by the GIT epithelia. Different species of commensal bacteria can elicit markedly different levels of ROS from contacted cells. Lactobacilli are especially potent inducers of ROS generation in cultured cells and in vivo, though all bacteria tested have some ability to alter the intracellular oxidoreductase environment (Lin et al. 2009b). Yan et al. (2007) has reported that there are soluble factors that are produced by species of Lactobacilli that are capable of mediating beneficial effects in in vivo inflammatory models. This result expands our understanding that there are ROS-stimulating bacteria that possess effective specific membrane components and or secreted factors that activate cellular ROS production to maintain homeostasis.
It has been reported that redox signaling by microbial ROS formation is in response to microbial signals via formyl peptide receptors and the gut epithelial NADPH oxidase 1 (Nox1) (Neish 2013). As previously documented (Linnane et al. 2007) ROS generated by Nox enzymes have been shown to function as essential second messengers in multiple signal transduction metabolic pathways through the rapid and transient oxidative inactivation of a distinct class of sensor proteins bearing oxidant-sensitive thiol groups. These redox-sensitive proteins include tyrosine phosphatases that attend as regulators of the MAP kinase pathways , focal adhesion kinase (Linnane et al. 2007; Neish 2013). These reports focus our understanding on the importance of second messenger functionality for the maintenance of homeostasis and brings into serious question of the annulment of ROS by antioxidant supplements for the amelioration of chronic diseases such as CKD. The established importance of recent investigations regarding probiotic/microbial-elicited ROS teaches that stimulated cellular proliferation and motility is strictly controlled and is a regulated signaling process for proper innate immunity and gut barrier functionality (Lin et al. 2009a, b; Patel et al. 2012; Collier-Hyams et al. 2005) The observations that the vertebrate epithelia of the intestinal tract supports a tolerable low-level inflammatory response toward the GIT microbiome, can be viewed as an adaptive activity that maintains homeostasis (Neish et al. 2000).
7 Fecal Microbiota Transplants
The accepted definition for fecal microbiota transplants (FMT) is a term that describes the infusion of a fecal suspension from a healthy individual into the gastrointestinal tract of an individual with colonic disease (Borody and Campbell 2012).
Recently, there has been strong interest in the use of FMT for the treatment of gastrointestinal and non-gastrointestinal diseases (Sha et al. 2014). A systematic review that reported on 844 patients who had undergone FMT was identified from 67 published clinical studies (Sha et al. 2014). The most common indications in this review were for refractory/relapsing Clostridium difficile infection (CDI) (76.3 %) and inflammatory bowel disease (IBD) (13.2 %). Seven publications reported FMT use in pediatric patients with a total of 11 treated, 3 with chronic constipation and the remainder with recurrent CDI or ulcerative colitis (UC). Patients diagnosed with refractory/relapsing CDI had a 90.7 % cure rate and 78.4 % of patients with IBD were in remission after FMT. It was further reported that FMT therapy could also be effective in the treatment of some non-gastrointestinal disorders such as chronic fatigue syndrome. The only reported serious adverse event attributed to the therapy was a case of suspected peritonitis. Furthermore, the review reported that at the time of the review there had been only one placebo-controlled trial, reporting a successful treatment of 43 patients diagnosed with recurrent CDI (Van Nood et al. 2013).
We have previously reviewed and reported (Bella et al. 2014) that multistrain probiotic formulations may also be efficacious for the treatment and also prevention of proton pump inhibitor induced Clostridium difficile associated diarrhea (CDAD). In that review we reported that there are numerous probiotic species hat have been investigated as useful and these include L. rhamnosus GG , various Lactobacillus and Bifidobacterium species, and the yeast Saccharomyces boulardii (Hickson 2011). The groups of probiotics that have been investigated varied from single species (Saccharomyces boulardii, L. rhamnosus GG, Bacillus clausii , B. longum , Clostridium butyricum miyairir , L. acidophilus , Enterococcus faecium SF68 ), to mixtures of two types of probiotics and to a synbiotic (a probiotic combined with a prebiotic substance) (Hickson 2011). A meta-analysis reporting on probiotics for the prevention of CDAD efficacy was reported for L. rhamnosus GG [dose: 109–1010 CFU/day]; L. acidophilus [dose: 109–1010 CFU/day]; S. boulardii lyophilized [dose: 109 CFU/day]; L. plantarum [dose:109 CFU/day]; L. acidophilus and L. casei [dose:109 CFU/day], and VSL3# [dose:109 CFU/day]. The duration of follow-up varied from 2 weeks to 12 weeks and the risk of developing CDAD was 0–24 %. Hence the systematic review reported that 20 randomized trials testing the effect of probiotics in patients receiving antibiotics showed a large relative risk reduction in the incidence of CDAD of 0.34 (CI, 0.24–0.49).
8 Discussion
Inflammation is an essential physiological response by body tissues to injury, chemical irritation, or an assault by generally pathogenic bacteria (Mazmanian et al. 2008). Once the insult is neutralized, normal physiological function needs to be restored. In the GIT, an inflammatory response can be elicited to clear pathogenic bacteria with adaptive responses by commensal and probiotic bacteria that can then subsequently reduce the inflammatory event, thereby promoting a regulated pro-or anti-inflammatory state and assisting in reducing the symptoms of conditions such as IBS or IBD. Figure 1 illustrates diagrammatically the complexity exhibited by the GIT in the continuous regulation of inflammation that is required throughout a lifetime. Furthermore, research (Parassol et al. 2005; Zyrek et al. 2007) supports the notion that increased intestinal permeability resulting from the disruption of the epithelial tight junction may initiate or promote dysregulated inflammation . Maintaining and protecting the tight junctions , preserves barrier function (Nunbhakdi–Craig et al. 2002; Schneeberger and Lynch 2004). It has been demonstrated in vitro that treatment of T84 and Caco-2 cells with probiotics restored or maintained tight junction complexes, thereby restoring the epithelial barrier function in enteropathogenic E. coli stimulated cells. Regardless of the timing, incubation with E. coli Nissle 1917 or L. casei following or during enteropathogenic E. coli infection restored the integrity of the epithelial cell barrier (Parassol et al. 2005; Zyrek et al. 2007).
The clinical evidence for the benefits of probiotics is sometimes contentious, however, the data presented herein indicates that probiotics provide both a prophylactic and therapeutic benefit in improving inflammatory conditions (e.g., in the GIT, skin) by regulating cytokine and cell signaling pathways (Mencarelli et al. 2011).
Commensal bacteria and vertebrate immune systems form a symbiotic relationship and have a coevolutionary profile. Such that proper immune development and function relies on colonization of the GIT by commensal bacteria and the maturation cues elicited by the bacterial cohort.
Modification of the gut bacterial cohort has strong therapeutic implications. The demonstration that commensal bacteria are not sequestered by the gut epithelium but are instead recognized by TLRs under normal steady-state conditions attests to this complexity. Indeed, the interaction of commensal bacterial products with host microbial pattern recognition receptors plays a crucial role in resistance to epithelial injury and promoting intestinal homeostasis (Rossi et al. 2013). Because mammalian TLRs recognize products of both pathogenic and commensal bacteria, they might have at least two distinct functions, namely: (i) protection from infection and (ii) control of mucosal homeostasis, both of which are dependent on the recognition of microorganisms (pathogens and commensals, respectively) (Fig. 1). This dual function might explain why some of the TLR-induced gene products, such as inflammatory cytokines and chemokines, are intricately involved in both host defense and tissue repair.
Previously reviewed published human studies of probiotics and of prebiotics (a nutritional supplement favoring the growth and increasing the lifespan of probiotic bacteria) demonstrate their effects on several clinical scenarios (Vitetta and Sali 2008; Vitetta et al. 2012, 2014a). Their beneficial effects can occur when the internal human environment is influenced by the commensal/probiotic environment throughout the digestive tract. Understanding both the bacteria—bacteria interactions and the bacteria—host interactions, especially in the distal GIT, will provide further opportunities for modulating the bacterial cohort of bacteria for therapeutic gain. Although many clinical studies indicate promising trends, the present consensus is that a number of larger controlled trials will be necessary before warranting the use of probiotic supplements as a routine medical treatment for numerous conditions.
There is considerable public and scientific interest in various natural products that include probiotics and prebiotics in modulating intestinal as well as end-organ physiology. Probiotic bacteria demonstrate promise as a biotherapeutic modality as scientific evidence continues to accumulate on the properties, functionality and benefits reported for promoting human health. Manipulating the GIT, a most complex ecosystem, is particularly challenging for therapeutic interventions that aim to regulate the GIT microbiome for the effective treatment of diseases such as irritability and inflammation of the GIT and possibly also cancer of the large bowel. However, the promise is often admixed with the hype. It is untenable to think that one probiotic will cure all diseases, but rather that probiotics are certainly an integral part of the integrative approach to health.
9 Future Research
Future directions for research may involve exploring the optimal doses of probiotics, duration of treatment, their effects in different models (in vitro and animal) of inflammatory disease, and suitability as a prophylactic and or therapeutic treatment. Probiotics and prebiotics can be delivered to the GIT but the percentage of ingested viable bacteria that reach the intestinal tract is not well characterized. Studies aimed at calculating the quantity of viable probiotic bacteria that reaches the upper and lower GIT may be useful. There is still a clear lack of evidence about the effect probiotics have on patients with for example IBD in terms of restoring the GIT microbiome profile. While alleviating the symptoms of IBD and IBS is clinically relevant, future research may also benefit from collecting colon tissue from CD and UC subjects for analysis of gastrointestinal inflammation, bacterial adhesion to the mucus barrier and epithelial cells and colonic crypts histology. This would certainly provide a better understanding of the underlying mechanisms of each condition and possibly lead to better strategies for treatments. Ultimately, probiotic research may also need to examine the synergistic benefits associated with individual bacterial strains that are currently used to formulate commercially available probiotic mixtures.
Within the beneficial efficacy of FMT could probiotics have an adjuvant role? This is a plausible accessory that may further improve FMT efficacy. Patients who elect to undergo FMT could gain a further benefit with the prior administration of probiotics (i.e., days–weeks in advance). The effect may be translated to a further reduction in the risk of gastrointestinal disease relapse.
Mechanistically, the causal relationship between reactive oxygen species and the unbridled damage proposed to macromolecules has led to an over simplification of complex biological processes. It has previously been reported that the formation of superoxide anion/hydrogen peroxide and nitric oxide do not conditionally lead to random macromolecular damage as under normal physiological conditions their production is actually regulated consistent with their second messenger roles (Linnane et al. 2007). As for the GIT it would expected that it too would behave in a manner that sustains a redox regulated state. Intestinal cells that maintain a redox balance preserve the cellular and microbial environment that supports physiological processes and orchestrates networks of enzymatic/metabolic reactions whereby inflammation remains regulated. Furthermore, the innate immune system presents a wide array of different receptors that can recognize specific bacterial molecular patterns. Hence, an enhanced understanding of the role played by individual probiotic molecular patterns becomes crucial in order to evolve the current complex area of live probiotic bacteria toward improved efficacious pharmacobiotic strategies (Caselli et al. 2011). This research area is complex and intellectually challenging.
Notes
- 1.
A placebo is a substance containing no medication benefit and prescribed to reinforce a patient’s expectation of possibly attaining a beneficial effect.
References
Amaral FA, Sachs D, Costa VV et al (2008) Commensal microbiota is fundamental for the development of inflammatory pain. PNAS USA 105:2193–2197
Arumugam M, Raes J, Pelletier E et al (2011) Enterotypes of the human gut microbiome. Nature 473(7346):174–80.
Bach JF (2002) The effect of infections on susceptibility to autoimmune and allergic diseases. NEJM 347(12):911–920
Backhead F, Manchester JK, Semenkovich CF, Gordon JI (2007) Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. PNAS USA 104:979–984
Bailey DM, Raman S, McEnery J et al (2006) Vitamin C prophylaxis promotes oxidative lipid damage during surgical ischemia-reperfusion. Free Radic Biol Med 40:591–600
Bauer H, Horowitz RE, Levenson SM et al (1963) The response of the lymphatic tissue to the microbial flora. Studies on germfree mice. Am J Pathol 42:471–483
Bella CJ, Coulson S, Vitetta L (2014) Is co–prescribing a multi–strain probiotic the simple solution for treating and preventing Proton Pump Inhibitor (PPIs) induced Clostridium difficile Associated Diarrhoea (CDAD) while maintaining evidence based pharmacotherapy? Submitted Adv Integr Med 1:52–54
Bengmark S, Martindale R (2005) Prebiotics and synbiotics in clinical medicine. Nutr Clin Pract 20(2):244–261
Berg RD, Savage DC (1975) Immune responses of specific pathogen-free and gnotobiotic mice to antigens of indigenous and nonindigenous microorganisms. Infect Immun 11(2):320–329
Bermudez-Brito M, Plaza-Diaz J, Munoz-Quezada S et al (2012) Probiotic mechanisms of action. Ann Nutr Metab 61(2):160–174
Borody TJ, Campbell J (2012) Fecal microbiota transplantation: techniques, applications, and issues. Gastroenterol Clin North Am 41(4):781–803
Bota DA, Van Remmen H, Davies KJ (2002) Modulation of Lon protease activity and aconitase turnover during aging and oxidative stress. FEBS Lett 532(1–2):103–106
Bota DA, Ngo JK, Davies KJ (2005) Down regulation of the human Lon protease impairs mitochondrial structure and function and causes cell death. Free Radic Biol Med 38(5):665–677
Bouilly-Gauthier D, Jeannes C, Maubert Y et al (2010) Clinical evidence of benefits of a dietary supplement containing probiotic and carotenoids on ultraviolet-induced skin damage. Br J Dermatol 163:536–543
Buddington RK, Williams CH, Chen SC et al (1996) Dietary supplement of neosugar alters the fecal flora and decreases activities of some reductive enzymes in human subjects. Am J Clin Nutr 63(5):709–716
Caselli M, Vaira G, Calo G et al (2011) Structural bacterial molecules as potential candidates for an evolution of the classical concept of probiotics. Adv Nutr 2:372–376
Chapman CM, Gibson GR, Rowland I (2011) Health benefits of probiotics: are mixtures more effective than single strains? Eur J Nutr 50(1):1–17
Chiang CK, Tanaka T, Nangaku M (2012) Dysregulated oxygen metabolism of the kidney by uremic toxins: review. J Ren Nutr 22(1):77–80
Cert-Bensussan N, Gaboriau-Routhiau V (2010) The immune system and the gut microbiota: friends or foes? Nat Rev Immunol 10(10):735–744
Chen Q, Krishna Espey MG et al (2005) Pharmacologic ascorbic acid concentrations selectively kill cancer cells: action as a pro-drug to deliver hydrogen peroxide to tissues. Proc Natl Acad Sci USA 102:13604–13609
Chorell E, Karlsson Videhult F, Hernell O et al (2013) Impact of probiotic feeding during weaning on the serum lipid profile and plasma metabolome in infants. Br J Nutr 110:116–126
Cicek M, Yıldırır A, Okyay K et al (2013) Use of alpha-lipoic acid in prevention of contrast-induced nephropathy in diabetic patients. Ren Fail 35(5):748–753
Cimperman L, Bayless G, Best K et al (2011) A randomized, double-blind, placebo-controlled pilot study of Lactobacillus reuteri ATCC 55730 for the prevention of antibiotic-associated diarrhea in hospitalized adults. J Clin Gastroenterol 45(9):785–789
Collier-Hyams LS, Sloane V, Batten BC, Neish AS (2005) Cutting edge: bacterial modulation of epithelial signaling via changes in neddylation of cullin-1. J Immunol 175(7):4194–4198
de Vrese M, Schrezenmeir J (2008) Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol 111:1–66
Ding S, Lund PK (2011) Role of intestinal inflammation as an early event in obesity and insulin resistance. Curr Opin Clin Nutr Metab Care 14:328–333
Dolan MF, Margulis L (2007) Advances in biology reveal truth about prokaryotes. Nature 445(7123):21
Dominguez-Bello MG, Costello EK, Contreras M et al (2010) Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. PNAS 107:11971–11975
Dounousi E, Papavasiliou E, Makedou A et al (2006) Oxidative stress is progressively enhanced with advancing stages of CKD. Am J Kidney Dis 48:752–760
Drouault-Holowacz S, Bieuvelet S, Burckel A et al (2008) A double blind randomized controlled trial of a probiotic combination in 100 patients with irritable bowel syndrome. Gastroenterol Clin Biol 32(2):147–152
Eckmann L (2006) Sensor molecules in intestinal innate immunity against bacterial infections. Curr Opin Gastroenterol 22(2):95–101
Enck P, Zimmermann K, Menke G et al (2008) A mixture of Escherichia coli (DSM 17252) and Enterococcus faecalis (DSM 16440) for treatment of the irritable bowel syndrome–a randomized controlled trial with primary care physicians. Neurogastroenterol Motil 20(10):1103–1109
Farout L, Friguet B (2006) Proteasome function in aging and oxidative stress: implications in protein maintenance failure. Antioxid Redox Signal 8:205–216
Fuller R (1989) Probiotics in man and animals. J Appl Bacteriol 66(5):365–378
Fuss IJ, Neurath M, Boirivant M et al (1996) Disparate CD4+ lamina propria (LP) lymphokine secretion profiles in inflammatory bowel disease. Crohn’s disease LP cells manifest increased secretion of IFN-gamma, whereas ulcerative colitis LP cells manifest increased secretion of IL-5. J Immunol 157(3):1261–1270
Giaffer MH, Holdsworth CD, Duerden BI (1991) The assessment of faecal flora in patients with inflammatory bowel disease by a simplified bacteriological technique. J Med Microbiol 35(4):238–243
Giovannini M, Agostoni C, Riva E et al (2007) Felicita study group. A randomized prospective double blind controlled trial on effects of long-term consumption of fermented milk containing Lactobacillus casei in pre-school children with allergic asthma and/or rhinitis. Pediatr Res 62(2):215–220
Grice EA, Segre JA (2011) The skin microbiome. Nat Rev Microbiol 9(4):244–253
Heller F, Florian P, Bojarski C et al (2005) Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterol 129(2):550–564
Hickson M (2011) Probiotics in the prevention of antibiotic-associated diarrhoea and Clostridium difficile infection. Therap Adv Gastroenterol 4(3):185–197
Himmelfarb J, Stenvinkel P, Ikizler TA et al (2002) The elephant in uremia: oxidant stress as a unifying concept of cardiovascular disease in uremia. Kidney Int 62:1524–1538
Hooper LV (2004) Bacterial contributions to mammalian gut development. Trends Microbiol 12:129–134
Hooper LV, Macpherson AJ (2010) Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol 10(3):159–169
Hornig D (1975) Distribution of ascorbic acid, metabolites and analogues in man and animals. Ann NY Acad Sci 258:103–118
Husom AD, Peters EA, Kolling EA et al (2004) Altered proteasome function and subunit composition in aged muscle. Arch Biochem Biophys 421(1):67–76
Hussaarts L, van der Vlugt LE, Yazdanbakhsh M, Smits HH (2011) Regulatory B-cell induction by helminths: implications for allergic disease. J Allergy Clin Immunol 128(4):733–739
Hvas CL, Kelsen J, Agnholt J et al (2007) Crohn’s disease intestinal CD4+ T cells have impaired interleukin-10 production which is not restored by probiotic bacteria. Scand J Gastroenterol 42(5):592–601
Jun M (2013) Antioxidants for chronic kidney disease. Nephrology Carlton 18:576–578
Kadooka Y, Sato M, Imaizumi K et al (2010) Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr 64:636–643
Kajander K, Hatakka K, Poussa T et al (2005) A probiotic mixture alleviates symptoms in irritable bowel syndrome patients: a controlled 6-month intervention. Aliment Pharmacol Ther 22(5):387–394
Kajander K, Myllyluoma E, Rajilic-Stojanovic M et al (2008) Clinical trial: multispecies probiotic supplementation alleviates the symptoms of irritable bowel syndrome and stabilizes intestinal microbiota. Aliment Pharmacol Ther 27(1):48–57
Kim HJ, Camilleri M, McKinzie S et al (2003) A randomized controlled trial of a probiotic, VSL#3, on gut transit and symptoms in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 17(7):895–904
Kim HJ, Vazquez Roque MI, Camilleri M et al (2005) A randomized controlled trial of a probiotic combination VSL# 3 and placebo in irritable bowel syndrome with bloating. Neurogastroenterol Motil 17(5):687–696
Lee WJ (2008) Bacterial-modulated signaling pathways in gut homeostasis. Sci Signal 1(21):pe24
Lee HJ, Waller RD, Stebbings S et al (2010) The effects of an orally administered probiotic on sulfasalazine metabolism in individuals with rheumatoid arthritis: a preliminary study. Int J Rheum Dis 13:48–54
Ley RE, Hamady M, Lozupone C et al (2008) Evolution of mammals and their gut microbes. Science 320:1647–1651
Li S, Taylor KB, Kelly SJ, Jedrzejas MJ (2001) Vitamin C inhibits the enzymatic activity of Streptococcus pneumoniae hyaluronate lyase. J Biol Chem 276(18):15125–15130
Lin PW, Myers LE, Ray L et al (2009a) Lactobacillus rhamnosus blocks inflammatory signaling in vivo via reactive oxygen species generation. Free Radic Biol Med 47(8):1205–1211
Lin JS, Chiu YH, Lin NT et al (2009b) Different effects of probiotic species/strains on infections in preschool children: a double-blind, randomized, controlled study. Vaccine 27(7):1073–1079
Linnane AW, Kios M, Vitetta L (2007) Healthy aging: regulation of the metabolome by cellular redox modulation and prooxidant signaling systems: the essential roles of superoxide anion and hydrogen peroxide. Biogerontology 8(5):445–467
Loguercio C, de Simone T, Federico A et al (2002) Gut-liver axis: A new point of attack to treat chronic liver damage? Am J Gastroenterol 97:2144–2146
Luoto R, Kalliomaki M, Laitinen K, Isolauri E (2010) The impact of perinatal probiotic intervention on the development of overweight and obesity: follow-up study from birth to 10 years. Int J Obes (Lond) 34:1531–1537
MacDonald TT, di Sabatino A (2006) The exposure of infants to Lactobacillus rhamnosus GG in Finland. J Pediatr Gastroenterol Nutr 42:476–478
Mackay IR, Rosen FS, Zinkernagel RM (2001) Maternal antibodies, childhood infections, and autoimmune diseases. NEJM 345(18):1331–1335
Martin HM, Campbell BJ, Hart CA et al (2004) Enhanced Escherichia coli adherence and invasion in Crohn’s disease and colon cancer. Gastroenterology 127:80–93
Matsuoka K, Inoue N, Sato T et al (2004) T-bet upregulation and subsequent interleukin 12 stimulation are essential for induction of Th1 mediated immunopathology in Crohn’s disease. Gut 53(9):1303–1308
Mazmanian SK, Liu CH, Tzianabos AO, Kasper DL (2005) An immunomodulatory molecule of symbiotic bacteria directs maturation of the host immune system. Cell 122(1):107–118
Mazmanian SK, Round JL, Kasper DL (2008) A microbial symbiosis factor prevents intestinal inflammatory disease. Nature 453:620–625
Meiners S, Heyken D, Weller A et al (2003) Inhibition of proteasome induces concerted expression of proteasome genes and de novo formation of mammalian proteasomes. J Biol Chem 278:21517–21525
Mencarelli A, Distrutti E, Renga B et al (2011) Probiotics modulate intestinal expression of nuclear receptor and provide counter-regulatory signals to inflammation-driven adipose tissue activation. PLoS ONE 6(7):e22978
Morelli L, Capurso L (2012) FAO/WHO guidelines on probiotics: 10 years later. J Clin Gastroenterol 46 Suppl:S1-2
Mylonaki M, Rayment NB, Rampton DS et al (2005) Molecular characterization of rectal mucosa-associated bacterial flora in inflammatory bowel disease. Inflamm Bowel Dis 11(5):481–487
Nakamura YK, Omaye ST (2012) Metabolic diseases and pro- and prebiotics: mechanistic insights. Nutr Metab (Lond) 9:60
Neish AS (2013) Redox signaling mediated by the gut microbiota. Free Radic Res (Epub ahead of print)
Neish AS, Gewirtz AT, Zeng H et al (2000) Prokaryotic regulation of epithelial responses by inhibition of Ikappa B-alpha ubiquitination. Science 289:1560–1563
Niedzielin K, Kordecki H, Birkenfeld B (2001) A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299 V in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol 13(10):1143–1147
Niv E, Naftali T, Hallak R, Vaisman N (2005) The efficacy of Lactobacillus reuteri ATCC 55730 in the treatment of patients with irritable bowel syndrome–a double blind, placebo-controlled, randomized study. Clin Nutr 24(6):925–931
Nunbhakdi-Craig V, Machleidt T, Ogris E et al (2002) Protein phosphatase 2A associates with and regulates atypical PKC and the epithelial tight junction complex. J Cell Biol 158(5):967–978
O’Mahony L, McCarthy J, Kelly P et al (2005) Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology 128(3):541–551
O’Neill LA (2006) How Toll-like receptors signal: what we know and what we don’t know. Curr Opin Immunol 18:3–9
Parassol N, Freitas M, Thoreux K et al (2005) Lactobacillus casei DN-114 001 inhibits the increase in paracellular permeability of enteropathogenic Escherichia coli-infected T84 cells. Res Microbiol 156(2):256–262
Pasare C, Medzhitov R (2004) Toll-dependent control mechanisms of CD4 T cell activation. Immunity 21:733–741
Patel RM, Myers LS, Kurundkar AR et al (2012) Probiotic bacteria induce maturation of intestinal claudin 3 expression and barrier function. Am J Pathol 180(2):626–635
Pereira DI, Gibson GR (2002) Cholesterol assimilation by lactic acid bacteria and bifidobacteria isolated from the human gut. Appl Environ Microbiol 68:4689–4693
Pickering GW (1950) Significance of the discovery of the effects of cortisone on rheumatoid arthritis. Lancet 6620–6621
Pineiro M, Stanton C (2007) Probiotic bacteria: legislative framework—requirements to evidence basis. J Nutr 137(3 Suppl 2):850S–853S
Polson J, Lee WM (2005) AASLD position paper: The management of acute liver failure. Hepatology 41:1179–1197
Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R (2004) Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell 118(2):229–241
Rautava S, Luoto R, Salminen S, Isolauri E (2012) Microbial contact during pregnancy, intestinal colonization and human disease. Nat Rev Gastroenterol Hepatol 9(10):565–576
Rossi O, van Baarlen P, Wells JM (2013) Host-recognition of pathogens and commensals in the mammalian intestine. Curr Top Microbiol Immunol 358:291-321
Rutkowski P, Słominska EM, Szołkiewicz M et al (2007) Relationship between uremic toxins and oxidative stress in patients with chronic renal failure. Scand J Urol Nephrol 41(3):243–248
Safavi M, Farajian S, Kelishadi R et al (2013) The effects of synbiotic supplementation on some cardio-metabolic risk factors in overweight and obese children: a randomized triple-masked controlled trial. Int J Food Sci Nutr 64:687–693
Schneeberger EE, Lynch RD (2004) The tight junction: a multifunctional complex. Am J Physiol Cell Physiol 286(6):C1213–C1228
Scholz-Ahrens KE, Ade P, Marten B et al (2007) Prebiotics, probiotics, and synbiotics affect mineral absorption, bone mineral content, and bone structure. J Nutr 137(3 Suppl 2):838S–846S
Sha S, Liang J, Chen M, Xu B, Liang C, Wei N, Wu K (2014) Systematic review: faecal microbiota transplantation therapy for digestive and nondigestive disorders in adults and children. Aliment Pharmacol Ther 39(10):1003–1032
Shih PM, Matzke NJ (2013) Primary endosymbiosis events date to the later Proterozoic with cross-calibrated phylogenetic dating of duplicated ATPase proteins. Proc Natl Acad Sci USA 110(30):12355–12360
Sinn DH, Song JH, Kim HJ et al (2008) Therapeutic effect of Lactobacillus acidophilus-SDC 2012, 2013 in patients with irritable bowel syndrome. Dig Dis Sci 53(10):2714–2718
Singel DJ, Stamler JS (2005) Chemical physiology of blood flow regulation by red blood cells: the role of nitric oxide and S-nitrohemoglobin. Ann Rev Physiol 67:99–145
Sironi M, Clerici M (2010) The hygiene hypothesis: an evolutionary perspective. Microbes Infect 12(6):421–427
So JS, Song MK, Kwon HK et al (2011) Lactobacillus casei enhances type II collagen/glucosamine-mediated suppression of inflammatory responses in experimental osteoarthritis. Life Sci 88:358–366
Stolze IP, Mole DR, Ratcliffe PJ (2006) Regulation of HIF: prolyl hydroxylases. Novartis Found Symp 272:15–25
Sun H, Gao J, Ferrington DA et al (1999) Repair of oxidized calmodulin by methionine sulfoxide reductase restores ability to activate the plasma membrane Ca-ATPase. Biochemistry 38:105–112
Swidsinski A, Ladhoff A, Pernthaler A et al (2002) Mucosal flora in inflammatory bowel disease. Gastroenterol 122(1):44–54
Tan M, Zhu JC, Du J et al (2011) Effects of probiotics on serum levels of Th1/Th2 cytokine and clinical outcomes in severe traumatic brain-injured patients: a prospective randomized pilot study. Crit Care 15:R290
Tappenden KA, Deutsch AS (2007) The physiological relevance of the intestinal microbiota-contributions to human health. JACN 26(6):679S–683S
Terawaki H, Yoshimura K, Hasegawa T et al (2004) Oxidative stress is enhanced in correlation with renal dysfunction: examination with the redox state of albumin. Kidney Int 66(5):1988–1993
Tien MT, Girardin SE, Regnault B et al (2006) Anti-inflammatory effect of Lactobacillus casei on Shigella-infected human intestinal epithelial cells. J Immunol 176:1228–1237
Van de Merwe JP, Schroder AM, Wensinck F et al (1988) The obligate anaerobic faecal flora of patients with Crohn’s disease and their first-degree relatives. Scand J Gastroenterol 23(9):1125–1131
Vanholder R, De Smet R, Glorieux G et al (2003) Review on uremic toxins: Classification, concentration, and interindividual variability. Kidney Int 63:1934–1943
Van Nood E, Vrieze A, Nieuwdorp M et al (2013) Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 368:407–415
Vaziri ND, Yuan J, Rahimi A, Subramanian VS et al (2012) Disintegration of colonic epithelial tight junction in uremia: a likely cause of CKD-associated inflammation. Nephrol Dial Transp 27:2686–2693
Vinik A (2011) The question is, my dear watson, why did the dog not bark? the joslin 50-year medalist study. Diabetes Care 34(4):1060–1063
Vitetta L, Alford H (2013) The pharmacobiotic potential of the gastrointestinal tract micro-biometabolome–probiotic connect: a brief commentary. Drug Dev Res 74(6):353–359
Vitetta L, Gobe G (2013) Uremia and chronic kidney disease: the role of the gut microflora and therapies with pro- and prebiotics. Mol Nutr Food Res 57:824–832
Vitetta L, Sali A (2008) Probiotics, prebiotics and gastrointestinal health. Med Today 9:65–70
Vitetta L, Briskey D, Hayes E, Shing C, Peake J (2012) A review of the pharmacobiotic regulation of gastrointestinal inflammation by probiotics, commensal bacteria and prebiotics. Inflammopharmacol 20(5):251–66
Vitetta L, Briskey D, Alford H, Hall S, Coulson S (2014a) Probiotics, prebiotics and the gastrointestinal tract in health and disease. Inflammopharmacology 22(3):135–154
Vitetta L, Manuel R, Zhou JY, Linnane AW, Hall S, Coulson S (2014b) The overarching influence of the gut microbiome on end-organ function: the role of live probiotic cultures. Pharmaceuticals (Basel) 7(9):954–989
Wills-Karp M, Santeliz J, Karp CL (2001) The germless theory of allergic disease: revisiting the hygiene hypothesis. Nat Rev Immunol 1:69–75
Whorwell PJ, Altringer L, Morel J et al (2006) Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. Am J Gastroenterol 101(7):1581–1590
Wu JT, Lin HC, Hu YC, Chien CT (2005) Neddylation and deneddylation regulate Cul1 and Cul3 protein accumulation. Nat Cell Biol 7(10):1014–1020
Xu J, Gordon JI (2003) Honor thy symbionts. PNAS 100:10452–10459
Yan F, Cao H, Cover TL et al (2007) Soluble proteins produced by probiotic bacteria regulate intestinal epithelial cell survival and growth. Gastroenterology 132(2):562–575
Yin D, Sun H, Weaver RF, Squier TC (1999) Nonessential role for methionines in the productive association between calmodulin and the plasma membrane Ca-ATPase. Biochemistry 38:13654–13660
Yin D, Kuczera K, Squier TC (2000) The sensitivity of carboxyl-terminal methionines in calmodulin isoforms to oxidation by H2O2 modulates the ability to activate the plasma membrane Ca-ATPase. Chem Res Toxicol 13:103–110
Zarrati M, Shidfar F, Nourijelyani K et al (2013) Lactobacillus acidophilus La5, Bifidobacterium BB12, and Lactobacillus casei DN001 modulate gene expression of subset specific transcription factors and cytokines in peripheral blood mononuclear cells of obese and overweight people. BioFactors 39:633–643
Zeng J, Li YQ, Zuo XL et al (2008) Clinical trial: effect of active lactic acid bacteria on mucosal barrier function in patients with diarrhoea-predominant irritable Bowel syndrome. Aliment Pharmacol Ther 28(8):994–1002
Zyrek AA, Cichon C, Helms S et al (2007) Molecular mechanisms underlying the probiotic effects of Escherichia coli Nissle 1917 involve ZO-2 and PKCzeta redistribution resulting in tight junction and epithelial barrier repair. Cell Microbiol 9:804–816
Acknowledgments/Conflict of Interest
Luis Vitetta has received National Institute of Complementary Medicine and National Health and Medical Research Council of Australia competitive funding and industry support for research into probiotics. The authors have no further conflicts of interest relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Basel
About this chapter
Cite this chapter
Vitetta, L., Palacios, T., Hall, S., Coulson, S. (2015). Gastrointestinal Tract Commensal Bacteria and Probiotics: Influence on End-Organ Physiology. In: Rainsford, K., Powanda, M., Whitehouse, M. (eds) Novel Natural Products: Therapeutic Effects in Pain, Arthritis and Gastro-intestinal Diseases. Progress in Drug Research, vol 70. Springer, Basel. https://doi.org/10.1007/978-3-0348-0927-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-0348-0927-6_1
Published:
Publisher Name: Springer, Basel
Print ISBN: 978-3-0348-0926-9
Online ISBN: 978-3-0348-0927-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)