Abstract
Endogenous antimicrobial peptides (AMPs) are gene encoded and can be considered as our own antibiotics. These peptides represent an ancient system since they are widespread in nature and have been identified in invertebrates, vertebrates, mammals and also in plants. Defensins and cathelicidins are the main families of AMPs in mammals including humans. From an evolutionary point of view, AMPs have coevolved with microbes in specific niches and constitute an important parameter in host–microbe interactions. The development of bacterial resistance against classical antibiotics is a growing problem, and novel antimicrobial strategies are urgently needed. Here, we present a concept based on the idea of inducing endogenous AMP expression by small compounds, such as vitamin D and butyrate. The induction of multiple AMPs with different mechanisms of action would minimize the risk of bacterial resistance. Thus, such inducing compounds may open new avenues for pharmaceutical intervention in the treatment or prevention of infections. Additional novel targets for medical treatment may be identified by dissecting signaling pathways and regulatory circuits for induced expression of AMPs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
1.1 Antimicrobial Peptides Are Included in a Conserved Defense Concept
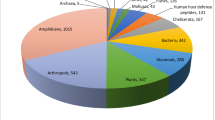
Gene-encoded antimicrobial peptides (AMP) are found among diverse life forms of eukaryotes from simple metazoan such as Hydra to complex mammals including humans (Bosch et al. 2009). There are even fungal species that are able to synthesize gene-encoded peptides, although fungi are better known for making antibiotics that are chemically distinct from peptides in order to defend themselves against bacteria. The first fungal peptide identified was plectasin, isolated from the saprophytic ascomycete Pseudoplectania nigrella (Mygind et al. 2005). More recently additional related fungal peptides were identified and found to be related to the animal defensins, indicating an ancient evolutionary origin for the mammalian defensins (Zhu 2008b). Furthermore, AMPs have also been identified in several plants (Sels et al. 2008). Characterized AMPs exhibit diverse structures but participate in a conserved defense concept. The expression at epithelial surfaces and phagocytes is the consensus among the diverse group of metazoans that are best studied. Epithelial cells are the first cells confronted by microbes, while phagocytes are the first cells recruited to the site of microbial challenge. Phagocytes contribute to various antimicrobial components including AMPs and amplify the first line of defense in metazoans. Thus, AMPs are included at the front of the host defense barrier. The fact that these peptides are widespread in nature emphasizes their importance and success in eukaryotic evolution. AMPs are grouped in families based on their primary structures, where defensins and cathelicidins constitute the main families of mammalian AMPs (Zasloff 2002). Defensins exhibit an extended evolutionary history and are present from fungi to humans, while cathelicidins appeared later in evolution and have only been found in vertebrates. The different peptide families show independent lineage-specific patterns, being expanded in some species but deleted in other. The comparison of different AMPs shows rapid divergence with alterations of primary structures, resulting in multiple forms that might reflect the evolutionary race with fast evolving microbes. In vertebrates AMPs are an important part of innate immunity that have influenced the coevolution with microbes and are still determinants of the niche for the natural microbial community. Thus, AMPs can be viewed as parameters of the intertwined evolution of host–microbe interactions. Importantly, this interaction is at many levels and influences not only defenses but also access to dietary energy for the host. The evolutionary time of AMPs assumes their inclusion in the platform that the advanced adaptive immunity was based on. The importance of AMP function in vertebrate defenses and immunity is established, and consequences of deficiency are known to result in susceptibility to infections (Nizet et al. 2001). Furthermore, an altered expression profile of AMPs, exemplified in transgenic mice, affects the composition of the microbial flora (Salzman et al. 2010). Importantly, this ancient system has maintained the antimicrobial function, fending off microbes through millions of years of evolution. Thus, they are an example of a surviving defense system including different effectors that have been selected for in evolution. In contrast, the human use of classical antibiotics has resulted in widespread resistance that has evolved among bacteria only in decades, as a result of strong selection against a single antimicrobial target. Most likely the key to the antimicrobial success of AMPs is the sequence divergence and coexpression of multiple peptide forms together with defense proteins such as lysozyme and lactoferrin, lipocalin, and RegIII-gamma working together in synergy. This network builds a complex defense system, utilizing various signaling pathways (Cederlund et al. 2010; Gudmundsson et al. 2010). All these different defense effectors are directed toward vital functions or structure of the microbes, i.e., the cell wall, the cell membrane, or depletion of essential nutrients such as iron (Fe). Thus, there is no single simple solution for the microbe to escape the frontier of innate defenses. AMPs have affinity toward the bacterial cell membrane leading to membrane destabilization and loss of vital functions such as elimination of membrane potential with subsequent lysis of the microbe. A more specific target than the whole cell membrane was recently added for several defensins, which bind to lipid II and thereby disturb the synthesis of the microbial cell wall (Schneider et al. 2010). If this activity applies to other amphipathic antimicrobial peptides remains to be elucidated. The majority of AMPs are cationic with an amphipathic character, a quality that allows flexibility with respect to their primary structures but still maintaining the activity. This is one criterion allowing a rapid evolutionary divergence among AMPs. The outcome is that every species has its own repertoire of AMPs exemplified by the mammalian cathelicidins with one cathelicidin gene in humans, mice, and rats; three in horses; seven in sheep (Zanetti 2004); and 11 genes in pigs (Zhu 2008).
1.2 AMPs and the Normal Flora
The rapid divergence of AMPs has been an important host parameter, influencing initial defenses and making up defined barriers for the coevolving microbes. The composition of AMPs also determines the complexity of the microbial community (Salzman et al. 2010). The microbe interaction with the host is multifarious, including the span from beneficial symbionts to harmful pathogens. These different host–microbe interactions follow different routes in selection, where the mammalian gut can serve as a prime example. Using genomic and metabolomic approaches, considerable research effort has resulted in characterization of up to 1,000 different microbial species in the human gut with an estimation of up to 100 trillion (1014) microbial cells on individual basis. This research also highlights the importance of the relationship between the microbial community and human diseases such as obesity, diabetes, and inflammatory bowel diseases (Hooper and Macpherson 2010).
A substantial part of the microbes in the gut are symbionts, contributing to vital processes for the whole organism. For the host, the symbionts are an important metabolic adduct by degrading dietary carbohydrates, and hence, the host gains access to energy as well as the microbe. In addition, symbionts synthesize essential components for the host such as vitamin K. Symbiotic microbes exhibit metabolic adaptation and thrive in the luminal space of the gut. They are dependent on a number of hydrolyzing enzymes encoded in the bacterial genome that degrade complex carbohydrates (Hooper 2009). Thus, the symbionts do not need host tissues for energy and are kept outside the internal milieu of the body by the epithelia.
Recently, an interesting opinion has been presented with respect to metabolic adaptation of characterized symbionts in comparison to virulent pathogens. Pathogens do not show the advanced metabolic adaptation; instead, they need access to host tissues for their survival (Hooper and Macpherson 2010). In order to break through the epithelial barrier, pathogens have evolved virulence systems and/or factors. In this process, the pathogens meet obstacles of the epithelial barrier, where AMPs are included as one part. Upon challenge the peptides are mobilized by protease cleavage of an inactive precursor or released from storage in the mucus or vacuoles. Thus, the activation is rapid and immediate. AMPs limit the access to tissues for the pathogens and define a protective zone. During evolution the pathogens have adopted approaches in order to escape initial defenses of the host such as degrading the peptides by secreted proteases, i.e., Streptococcus (Frick et al. 2003), modifying phospholipids rendering resistance through reduced AMP affinity, i.e., Salmonella (Prost et al. 2007), downregulating peptide expression, i.e., Shigella (Islam et al. 2001; Sperandio et al. 2008), and utilizing advanced pump systems, i.e., Neisseria (Shafer et al. 1998). By these strategies, pathogens are more resistant and can break through the complex defense barrier of the host. Additional factors of importance include the nutritional status of the host, where components of the diet influence the level of AMP expression directly or indirectly such as Zn, vitamin D3, and butyrate (Steinmann et al. 2009; Talukder et al. 2011). Thus, the prediction is that the barrier may be strengthened by increased production of AMPs. The diverse virulence mechanisms for different pathogens underline the importance of complete gene characterization for every pathogen. Detailed knowledge of host–microbe interaction is also essential to be defined in addition to environmental signals at different epithelial surfaces.
A key question in this connection is if a strategy can be designed and utilized in therapy based on neutralizing pathogenic offense such as counteracting the downregulation of AMPs or inhibiting microbial proteases that degrade these defense effectors. If the escape routes are blocked, the pathogens will be exposed to the full arsenal of the innate defense barrier and can be eliminated in an efficient way. In this chapter, we will discuss the regulation of AMPs associated with innate defenses. Furthermore, inducers that are able to enhance the production of AMPs and can be drug candidates will also be discussed. Maybe a combination of compounds, where one inhibits virulence and the other induces AMP production, is an optimal solution? A strategy, where we can induce and control the production of AMPs at tissue sites of pathogen entry, has the potential to be a therapeutic complement to classical antibiotic treatment. A system that has survived during evolution will most likely not have the problem with microbial resistance that is an increasing problem in modern healthcare.
2 Regulatory and Signaling Pathways of Endogenous Antimicrobial Peptides
The expression of defensins and cathelicidin in human tissue is constitutive or induced by external and/or internal signals. The induced AMP expression is included in the enhanced defense programs initiated upon exposure to danger signals, sensing the presence of bacteria, or intrinsic signals from pro-inflammatory cytokines.
The constitutive expression of AMPs is a part of cellular differentiation and thus included in the normal developmental program of cells and organisms. In insects, the link between development and immunity is recognized, where the transcription factor dorsal is important not only in the development of the body axis but also a key factor in induced immunity (Hoffmann and Reichhart 2002). This transcription factor in Drosophila melanogaster is indeed related to the mammalian transcription factor NF-κB, a key regulator of inflammation in mammals.
In bone marrow, AMP genes are constitutively expressed with transcription in progenitor cells of mainly neutrophils and eosinophils. Indeed, neutrophils are the major innate defense cells in blood with a high turnover rate. The human α-defensins HNP1–4 are estimated to constitute 20 % of total vacuolar proteins and are thus major components of neutrophils (Ganz 2003). The proforms of defensins are stored in granules of mature neutrophils cells and are immediately available for processing in order to eliminate microbial intruders. The human cathelicidin is also present in neutrophils but in lower amount compared to α-defensins. The cathelicidin proform hCAP18 has been suggested to be secreted from the neutrophilic progenitors into the bloodstream and to be the main source of hCAP18 found in plasma (Borregaard 2010).
The constitutive expression of AMPs in bone marrow leading to storage in or secretion from neutrophils is included in the differentiation program of these cells. This applies also to AMPs of the Paneth cells in the crypt of Liberkühn in the small intestine. Paneth cells are derived from the crypt stem cells and are unique with respect to the expression of α-defensins, since human defensins 5 and 6 (HD5 and 6) are only present in this cell type, representing a lineage-restricted expression. This cell-specific transcription resides mainly in the proximal promoter that is incorporated in the humanized HD5 mouse, resulting in Paneth cell-specific expression of HD5 in the DEFA5-transgenic mice (Salzman et al. 2003). Paneth cells express many other defense proteins in addition to the HD5 and 6 including lysozyme, secretory phospholipase A2, RegIII-gamma, and matrix metalloproteinase 7 (MMP7), in addition to pro-inflammatory mediators such as interleukin-17A (IL-17A), tumor necrosis factor-alpha (TNF-α), and IL-1β (Ouellette 2010). The defense function of Paneth cells protects the niche of the stem cells in the crypt, and secreted factors of Paneth cells affect the composition of the microbial community in the gut (Salzman et al. 2010). Indeed, the Paneth cells represent the defense concept with multiple effectors working in synergy. During development, the progenitors of Paneth cells enter the base of the crypt in a process governed by the Wnt signaling pathway, influencing HD5 and 6 expression through the transcription factors β-catenin and T-cell factor-4 (TCF-4) (Ouellette 2010). These transcription factors are included in the differentiation program and contribute to the constitutive expression of innate effectors independent of bacterial components, since this expression takes place also in germ-free mice (Ouellette 2010).
In contrast to the α-defensins, the β-defensins are mainly expressed in epithelial cells. Transcription factors of importance for the expression of β-defensins have not yet been characterized in details except for NF-κB that is essential for the induced expression of β-defensin 2 (O’Neil et al. 1999; Duits et al. 2002). In cell lines, the expression of β-defensin-1 (hBD-1) has been linked to c-Myc regulation and certain binding sites in the promoter connected to regulators of circadian rhythms (Sherman and Froy 2008). This regulation might reflect the in vivo situation of the constitutive epithelial expression of hBD-1.
The expression pattern of the human cathelicidin LL-37 seems unique, since it is expressed both in pro-granulocytic cells (undifferentiated neutrophils and eosinophils) and epithelial cells. Essential transcription factors, activating the CAMP gene encoding LL-37, have only been partially defined. The initial study indicated several binding sites in the promoter of the CAMP gene, and an enhancer element was identified in intron 2 (Gudmundsson et al. 1996; Termen et al. 2008).
PU.1 is one transcription factor that is related to AMP gene expression and was first indicated to be important for the expression of α-defensins of neutrophils (Ma et al. 1998). Notably, PU.1 is essential for myeloid lineage commitment, and together with C/EBP, it is a determinant for the monocytic or granulocytic decision (Borregaard 2010). In relation to cathelicidins, PU.1 was first found to regulate the prophenin gene in pigs (Ramanathan et al. 2005). PU.1 is also crucial for epithelial expression of LL-37, where it is involved in both constitutively and induced expression by butyrate (Termen et al. 2008). Thus, both PU.1 and C/EBP are examples of transcription factors, essential for development and immunity.
Functional importance of transcriptional regulation of AMP encoding genes was first reported, when a conserved binding site for a C/EBP family member in mouse and human promoter of the cathelicidin genes was studied. Subsequently, it was found that the C/EBPε knockout mice did not express cathelicidin in bone marrow and suggested to contribute to the susceptibility of these mice to gram-negative bacteria (Verbeek et al. 1999). Later, binding of C/EBPε to the CAMP promoter was confirmed in expression studies in the monocytic cell line U937 (Gombart et al. 2005). In this study, binding of the vitamin D receptor (VDR) to the CAMP gene promoter was also established. The effects of vitamin D in relation to the induction of AMPs will be discussed below. VDR is a nuclear receptor binding 1,25 dihydroxyvitamin D3 and lithocholic acid (LCA). Recently additional ligands of VDR have been identified such as ω3- and ω6-essential polyunsaturated fatty acids (PUFAs), i.e., docosahexaenoic acid (DHA) and arachidonic acid, respectively, and the vitamin E derivative γ-tocotrienol (Haussler et al. 2008). Additional nuclear receptors directly linked to AMP expression are farnesoid X receptor (FXR) (D’Aldebert et al. 2009) and peroxisome proliferator-activated receptor gamma (PPAR-γ) (Dai et al. 2010). FXR regulates CAMP gene expression and has been claimed important for biliary tract sterility and partially explaining the beneficiary effects of ursodeoxycholic acid (UDCA) against inflammatory biliary disease. The induced expression of hBD-3 and cathelicidin is also regulated by PPAR-γ signaling via AP-1 and p38 activity (Dai et al. 2010).
The involvement of nuclear receptors in innate immunity emphasizes the recent linkage to the diet, where ligands to these receptors are derived from the diet, mediating effects on innate defenses. Interestingly, nuclear receptors are direct targets of several drugs that are utilized in therapy today, such as the PPAR-γ agonist pioglitazone, which is FDA-approved for use in diabetes type 2 patients (Gillies and Dunn 2000).
Intracellular mediators of signals linked to AMP expression upstream of the transcription factors have also been identified. By using specific inhibitors, it has been shown in several studies that signaling pathways, involving MAP kinases, are central for CAMP gene expression (Schauber et al. 2003; Termen et al. 2008). It is clear that the current knowledge of signaling pathways associated to AMPs is fragmentary. However, the emerging picture indicates signaling modules including nuclear receptors and MAP kinases that may represent adaptation to bacterial challenge. This might be a result of positive selection in host cells, avoiding bacterial strategies to escape innate effectors by turning off signaling pathways. Despite variation in the structure of AMPs, where divergence is the hallmark, the regulation is linked to vital conserved processes, and hence, one would expect similar regulatory circuits in various species but linked to different effectors.
2.1 Epigenetic Control of AMP Expression
In gene regulation, the structure of chromatin is an additional regulatory level, determining the accessibility of transcription factors to specific binding sites, and controlled by histone modifications. Recently, this has been studied in relation to effectors of innate immunity upon LPS response and tolerance in mouse macrophages (Foster et al. 2007). Genes of innate effectors can be divided into two categories with respect to secondary responses, i.e., silenced or amplified. The mouse cathelicidin gene was demonstrated to belong to the latter category with enhanced secondary response, indicating transcriptional memory. This epigenetic control may be viewed as an adaptation to repeated infections and is relevant associated to immune regulation (Foster and Medzhitov 2009) (Fig. 1).
Inducers, receptors, and effectors in host-bacterial cross talk. This schematic figure describes the main components discussed in this chapter. Bacteria carry chemical signatures, which are recognized by pattern recognition receptors (PRRs) on the cell surface or on the endosome, whereas NLRs are located in the cytoplasm. Commensal bacteria produce butyrate and lithocholic acid; the latter binds FXR in the cytosol. In addition, cytokines and exogenous drugs can affect AMP expression, a response that is mediated via specific receptors. Additional transcription factors, such as C/EBP, PU.1, and AP-1, have also been shown to be involved in AMP expression. The storage form, 25-OH vitamin D3, is converted by 1-alpha-hydroxylase (CYP27B1) to the active form 1,25-(OH)2-vitamin D3, which binds to the vitamin D receptor (VDR). TLRs Toll-like receptors, NLRs nucleotide oligomerization domain-like receptors, HDACi histone deacetylase inhibitor and PBA phenylbutyrate
3 Inducers of Antimicrobial Peptide Expression
The production of AMPs can be stimulated by bacterial products and cytokines, leading to signals that induce clearance of microbes and hence prevent infection. Initially it was reported that IL-1alpha stimulation or an infection with enteroinvasive Salmonella upregulated the expression of human β-defensin-2 (hBD-2) in colon epithelial cells (O’Neil et al. 1999). The human β-defensin-1 (hBD-1) was found to be constitutively expressed and not affected by cytokine stimulation or infection. A similar pattern was demonstrated in gastric epithelial cells, where hBD-2 is induced by IL-1alpha or infection with Helicobacter pylori (O’Neil et al. 2000). Also in these gastric cells, hBD-1 exhibited a constitutively expression. Later in another study, LL-37 was demonstrated to be induced by H. pylori in gastric epithelial cells (Hase et al. 2003). In human tracheobronchial epithelial cells, the induction of hBD-2 was shown dependent on TLR-2 by bacterial lipopeptides (Hertz et al. 2003). Also the bacterial products lipopolysaccharide (LPS) and lipoteichoic acid increased the production of LL-37 in sinus epithelial air-liquid tissue culture (Nell et al. 2004). A role of hBD-2 in CNS pathogenesis was indicated when astrocytes in culture were treated with LPS, IL-1beta, or TNF-α with subsequent production of hBD-2 (Hao et al. 2001). We found the mouse cathelicidin upregulated in the blood–brain barrier by Neisseria meningitidis infection (Bergman et al. 2006). However, the role of the mouse cathelicidin was not linked to CNS protection; although, the number of bacteria in blood was significantly increased in the cathelicidin-deficient mice (Bergman et al. 2006). Recently, it was shown that flagellin from Pseudomonas aeruginosa stimulated the secretion of both LL-37 and hBD-2 in corneal epithelial cells (Gao et al. 2010). Flagellin binds to TLR-5 and trigger inflammatory responses via NF-κB in different epithelial cells (Ramos et al. 2004). Notably, flagellin has been demonstrated to induce a protective response against Pseudomonas aeruginosa that is dependent on the release of cathelicidin from lung epithelial cells (Yu et al. 2010). Furthermore, the peptide LL-37 in lung epithelia activates a metalloprotease that in turn liberates a ligand to the epidermal growth factor receptor (EGFR). Subsequently the EGFR dimerizes, resulting in intracellular MEK activation (Tjabringa et al. 2003). This links antimicrobial activity and epithelial repair in one response. Importantly, AMPs have evolved additional functions that are receptor mediated and relevant to defenses such as chemotaxis, angiogenesis, and cell proliferation. These properties are also fundamental in wound healing and tissue repair.
Interestingly, some pathogens escape elimination by the antimicrobial defense system at epithelial surfaces by downregulating the expression of AMPs (Islam et al. 2001). The downregulation represents an initial step in breaking through the mucus for the pathogen to gain access to the epithelial cells. By this strategy, pathogens come into proximity to the epithelial cell membrane, utilizing their virulence tools such as the type-three-secretion system. In this connection, inducers of AMP expression are of interest as they counteract the pathogenic downregulation of AMPs, and the pathogen cannot interact with the cell. Instead, the pathogen is killed by the AMPs present. The short-chain fatty acid butyrate was one of the first molecules that were found to exhibit these inducing properties (Hase et al. 2002; Schauber et al. 2003). Interestingly, butyrate was earlier shown to affect clinical symptoms and decrease inflammation and bacterial load in experimental shigellosis in a rabbit model (Rabbani et al. 1999). Later we demonstrated a causative link between butyrate and AMP expression in shigellosis (Raqib et al. 2006). The counteraction by butyrate resulted in pathogen elimination from epithelial surfaces and recovery of the rabbits from the infection (Raqib et al. 2006). In normal colon function, butyrate is a byproduct of dietary fiber digestion and contributes to the important communication between the host and the microbial community, regulating AMP expression. Detailed knowledge of the mechanism is unknown but butyrate is known as an inhibitor of histone deacetylase (HDACi). In relation to the CAMP gene regulation, the HDACi activity has been suggested to be direct (Kida et al. 2006). However, also a secondary effect has been indicated, where the initial effect is the induction of a protein needed for the expression of the CAMP gene in lung epithelial cells (Steinmann et al. 2009). In general HDACi affects the packing of chromatin, keeping it open, and hence giving transcription factors access to their binding sites on target genes. However, for butyrate an alternative or complimentary mechanism involves the G-protein-coupled receptors GPR43 and GPR41 that have been shown to be important in mediating butyrate responses (Brown et al. 2003). The GPR43 receptor has recently been confirmed important for inflammatory regulation in mouse models and was suggested as a molecular link between diet, gastrointestinal bacterial metabolism, and immunological inflammatory responses (Maslowski et al. 2009).
In a search for additional inducers, phenylbutyrate (PBA) was found to be an interesting candidate with pronounced activity. Butyrate is a foul-smelling compound, and in that respect, PBA is a more suitable drug candidate. In addition PBA is a registered drug for the treatment of urea cycle disorders, working as a scavenger for ammonia (Brusilow 1991; Burlina et al. 2001). This offers an opportunity to use PBA in clinical trials, since safety measures have already been carried out.
Further research showed PBA to improve recovery from shigellosis in the rabbit model (Sarker et al. 2011). In this study, we also observed a systemic effect of butyrate, indicating that the inducers are not only working locally but also enter the bloodstream, since the rabbit cathelicidin CAP-18 also was induced in lung epithelia (Sarker et al. 2011).
Interestingly 1,25-dihydroxyvitamin D3, the hormonal form of vitamin D3, has been promoted as a therapeutic approach against infections due to its ability to induce AMP expression. This bioactive form of vitamin D3 also stimulated the defB2 gene encoding the antimicrobial peptide hBD-2 in monocytes and neutrophils (Wang et al. 2004). It has also been reported that vitamin D induces the expression of LL-37 in acute myeloid leukemia bone marrow cells, keratinocytes, colon cancer cell lines, and bone marrow-derived macrophages (Gombart et al. 2005). Interestingly, activation of Toll-like receptors (TLRs) in human macrophages upregulates the vitamin D receptor (VDR) and the vitamin D3 hydroxylase genes, leading to the induction of LL-37 with subsequent killing of intracellular Mycobacterium tuberculosis (Liu et al. 2006). The 1-alpha-hydroxylase is responsible for generating the biological active form of vitamin D3 by transforming the proform 25-hydroxyvitamin D3 into 1,25-dihydroxyvitamin D3. In the study of Liu et al., it was also shown that low levels of 25-hydroxyvitamin D3 in sera of African-American individuals, who are more susceptible to tuberculosis, correspond to lower induction of LL-37 in macrophages (Liu et al. 2006). This indicates a link to low LL-37 levels and susceptibility to tuberculosis and that vitamin D plays a key role in the production of LL-37, which can kill mycobacteria. In a recent randomized multicenter trial of vitamin D3 as adjunctive therapy for active tuberculosis, it was found that vitamin D3 did not significantly affect time to sputum culture conversion in the whole study population, but it did significantly hasten sputum culture conversion in participants with a specific genotype of the vitamin D receptor (Martineau et al. 2011).
We have recently shown that PBA and the active form of vitamin D act synergistically in inducing the expression of LL-37 (Steinmann et al. 2009), which might be utilized in therapy. Most recently, it was demonstrated that 1,25-dihydroxyvitamin D3 significantly enhances hBD-3 and LL-37 expression in keratinocytes. This upregulation was shown to be mediated via the nuclear receptor PPAR-γ where AP-1 and p38 activity was shown to be involved (Dai et al. 2010).
More recently, we have found that lithocholic acid (LCA) also induces antimicrobial peptide expression (Termen et al. 2008). LCA has some characteristics of both butyrate and vitamin D3. It is a bacterial product like butyrate made by bacteria from bile acid in the colon, and it is a known ligand to VDR like vitamin D (Adachi et al. 2005). A bacterial-derived bile acid with affinity to VDR is possibly involved in the physiology of the gut, affecting the microbial flora.
4 Role of Endogenous Antimicrobial Peptides in Human Diseases
Already in 1997, we demonstrated that the human cathelicidin LL-37 is upregulated in keratinocytes of psoriatic lesions (Frohm et al. 1997). This observation was confirmed by Ong et al. (2002), also showing that hBD-2 was upregulated in the lesions of psoriatic patients. In contrast, a downregulation of both LL-37 and hBD-2 was shown in the lesions of atopic dermatitis. The authors claimed that the low expression of these defense peptides in atopic dermatitis was the reason why these patients very often are infected in their lesions. This is not the case for psoriatic patients, who rarely get infections in their lesions. Psoriasis is a multifactorial autoimmune disease with unknown etiology. The trigger for the induced expression of LL-37 and hBD-2 has not been resolved. Interestingly, it was recently demonstrated that LL-37 can drive autoimmunity in psoriasis by binding to self-DNA. The complex of LL-37 and self-DNA is sensed by plasmacytoid dendritic cells (DCs) as a danger signal, and hence, this complex is translocated to endocytic compartments, where it is recognized by Toll-like receptor 9 (TLR-9), and a production of α-interferon is initiated (Lande et al. 2007). Normally, TLR-9 recognizes bacterial and/or viral DNA present in the endosomes. If LL-37 is a transporter of self-DNA into the endosomes in other autoimmune diseases needs to be investigated.
LL-37 is expressed also in atherosclerotic lesions more specifically in macrophages and endothelial cells. Its involvement in this disease is unclear. However, LL-37 induces the expression of the adhesion molecule intercellular adhesion molecule-1 (ICAM-1) and the chemokine monocyte chemotactic protein-1 (MCP-1) in endothelial cells (Edfeldt et al. 2006). Since ICAM-1 and MCP-1 promote atherosclerotic lesion development, LL-37 may accelerate the disease progress under conditions of chronic inflammation. Furthermore, it is well established that leukotriene B4 (LTB4) a powerful pro-inflammatory lipid mediator is involved in the development of atherosclerosis (Funk 2005). Recently, we reported that LL-37 can activate human neutrophils to promote synthesis and release of LTB4, and one mechanism behind this response is the ability of LL-37 to elicit translocation of 5-lipoxygenase to the nuclear membrane (Wan et al. 2007). On the other hand, LTB4 can trigger the release of LL-37 in neutrophils, an effect that is mediated via the leukotriene B4 receptor type 1 (BLT1) receptor (Wan et al. 2007). This cross talk between LTB4 and LL-37 may constitute an important parameter in inflammatory diseases.
During certain conditions, the delicate balance between bacteria and host can be disturbed, which may result in clinical symptoms and disease such as Crohn’s disease (CD). This clinical entity belongs to the inflammatory bowel disorders, where also ulcerative colitis (UC) belongs. However, these two diseases are distinctly different with the most obvious difference being that UC is strictly located to the colon, whereas CD can involve the entire gastrointestinal system from esophagus to rectum. A general hypothesis in CD pathogenesis is that gut bacteria are physically located too close and even adhere to epithelial cells, which drive a chronic inflammatory process (Sartor 2001). Several lines of research support the hypothesis that the normal flora is not recognized properly and a large genetic screen has identified mutations in NOD2 among a subgroup of patients with ileal CD (Hugot et al. 2001; Ogura et al. 2001). NOD2 is the receptor for muramyl dipeptide (MDP), which is a cell wall fragment shared by many bacterial species, including the normal flora. The downstream effect of a NOD2 mutation has been shown to result in a lack of Paneth cell defensin expression (Wehkamp et al. 2004). Indeed, Wehkamp et al. reported in 2004 that patients with ileal CD exhibited low expression of α-defensins in Paneth cells of the ileum (Wehkamp et al. 2004). Notably, the expression levels of eight other Paneth cell components remained unchanged, and the decrease of α-defensins was not observed in the colon of Crohn’s patients, in UC, or in pouchitis, indicating a very specific effect on Paneth cell alpha-defensins in ileal CD (Wehkamp et al. 2005). However, later studies showed that NOD2 mutations only could explain a fraction of all CD cases, which suggested the involvement of other genes (Hugot 2006). Indeed, a decrease of the HD5 and HD6 regulatory gene TCF7L2 (TCF-4) has been demonstrated to be associated with ileal CD (Wehkamp et al. 2007). Another gene important for Paneth cell biology is the autophagy-related gene ATG16L1, which has been linked to ileal CD (Hampe et al. 2007; Cadwell et al. 2008). Recently, a connection between NOD2 and the autophagic process has been established (Cooney et al. 2010; Travassos et al. 2010), suggesting that aberrant bacterial sensing and intracellular processing are tightly linked and that errors in these processes may result in CD. Finally, novel data has shown that vitamin D can induce NOD2 expression in monocytic cells and that vitamin D together with MDP—the ligand for NOD2 – synergistically increased expression levels of hBD-2 (Wang et al. 2010; Verway et al. 2010). Taken together, mutations in a gene encoding a bacterial sensing system (NOD2), in a Paneth cell–associated gene (TCF4) and in an autophagic machinery gene (ATG16L1) have been implicated in CD. The final effects of these mutations appear to involve a low expression of the antimicrobial peptides (HD5 and HD6), which result in a compromised barrier function. Thus, there is a solid rationale for therapeutic attempts to restore the antimicrobial capacity of the mucosal barrier with exogenous compounds such as vitamin D, PBA, and/or LCA.
5 Final Comments
In summary, several active molecular inducers have been identified, which can enhance the production of AMP, working together to strengthen epithelial repair and defenses. In animal models, we have demonstrated that several inducers affect elimination of enteroinvasive pathogens such as Shigella. Thus, these inducers are possible drug candidates against infections and might also be useful in preventive medicine. Due to induction of multiple factors with different mechanisms of action, the risk of developing bacterial resistance can be considered low. This is an important advantage of utilizing induced endogenous defense molecules to fight infections. Elucidating the components of constitutively and induced expression of AMPs may open new avenues for pharmaceutical intervention in the treatment of infections. Important motive for future research is to understand basic defenses and host pathogen interaction together with the interaction between the host and the natural bacterial flora. Further, a detailed knowledge about transcriptional pathways dictating AMP expression in different tissues and during specific infectious or inflammatory conditions is necessary.
References
Adachi R, Honma Y et al (2005) Selective activation of vitamin D receptor by lithocholic acid acetate, a bile acid derivative. J Lipid Res 46(1):46–57
Bergman P, Johansson L et al (2006) Induction of the antimicrobial peptide CRAMP in the blood–brain barrier and meninges after meningococcal infection. Infect Immun 74(12):6982–6991
Borregaard N (2010) Neutrophils, from marrow to microbes. Immunity 33(5):657–670
Bosch TC, Augustin R et al (2009) Uncovering the evolutionary history of innate immunity: the simple metazoan Hydra uses epithelial cells for host defence. Dev Comp Immunol 33(4):559–569
Brown AJ, Goldsworthy SM et al (2003) The Orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem 278(13):11312–11319
Brusilow SW (1991) Phenylacetylglutamine may replace urea as a vehicle for waste nitrogen excretion. Pediatr Res 29(2):147–150
Burlina AB, Ogier H et al (2001) Long-term treatment with sodium phenylbutyrate in ornithine transcarbamylase-deficient patients. Mol Genet Metab 72(4):351–355
Cadwell K, Liu JY et al (2008) A key role for autophagy and the autophagy gene Atg16l1 in mouse and human intestinal Paneth cells. Nature 456(7219):259–263
Cederlund A, Agerberth B et al (2010) Specificity in killing pathogens is mediated by distinct repertoires of human neutrophil peptides. J Innate Immun 2(6):508–521
Cooney R, Baker J et al (2010) NOD2 stimulation induces autophagy in dendritic cells influencing bacterial handling and antigen presentation. Nat Med 16(1):90–97
D’Aldebert E, Biyeyeme Bi Mve MJ et al (2009) Bile salts control the antimicrobial peptide cathelicidin through nuclear receptors in the human biliary epithelium. Gastroenterology 136(4):1435–1443
Dai X, Sayama K et al (2010) PPARgamma mediates innate immunity by regulating the 1alpha,25-dihydroxyvitamin D3 induced hBD-3 and cathelicidin in human keratinocytes. J Dermatol Sci 60(3):179–186
Duits LA, Ravensbergen B et al (2002) Expression of beta-defensin 1 and 2 mRNA by human monocytes, macrophages and dendritic cells. Immunology 106(4):517–525
Edfeldt K, Agerberth B et al (2006) Involvement of the antimicrobial peptide LL-37 in human atherosclerosis. Arterioscler Thromb Vasc Biol 26(7):1551–1557
Foster SL, Hargreaves DC et al (2007) Gene-specific control of inflammation by TLR-induced chromatin modifications. Nature 447(7147):972–978
Foster SL, Medzhitov R (2009) Gene-specific control of the TLR-induced inflammatory response. Clin Immunol 130(1):7–15
Frick IM, Akesson P et al (2003) SIC, a secreted protein of Streptococcus pyogenes that inactivates antibacterial peptides. J Biol Chem 278(19):16561–16566
Frohm M, Agerberth B et al (1997) The expression of the gene coding for the antibacterial peptide LL-37 is induced in human keratinocytes during inflammatory disorders. J Biol Chem 272(24):15258–15263
Funk CD (2005) Leukotriene modifiers as potential therapeutics for cardiovascular disease. Nat Rev Drug Discov 4(8):664–672
Ganz T (2003) Defensins: antimicrobial peptides of innate immunity. Nat Rev Immunol 3(9):710–720
Gao N, Kumar A et al (2010) Flagellin-induced corneal antimicrobial peptide production and wound repair involve a novel NF-kappaB-independent and EGFR-dependent pathway. PLoS One 5(2):e9351
Gillies PS, Dunn CJ (2000) Pioglitazone. Drugs 60(2):333–43, discussion 344–345
Gombart AF, Borregaard N et al (2005) Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3. FASEB J 19(9):1067–1077
Gudmundsson GH, Agerberth B et al (1996) The human gene FALL39 and processing of the cathelin precursor to the antibacterial peptide LL-37 in granulocytes. Eur J Biochem 238(2):325–332
Gudmundsson GH, Bergman P et al (2010) Battle and balance at mucosal surfaces–the story of Shigella and antimicrobial peptides. Biochem Biophys Res Commun 396(1):116–119
Hampe J, Franke A et al (2007) A genome-wide association scan of nonsynonymous SNPs identifies a susceptibility variant for Crohn disease in ATG16L1. Nat Genet 39(2):207–211
Hao HN, Zhao J et al (2001) Induction of human beta-defensin-2 expression in human astrocytes by lipopolysaccharide and cytokines. J Neurochem 77(4):1027–1035
Hase K, Eckmann L et al (2002) Cell differentiation is a key determinant of cathelicidin LL-37/human cationic antimicrobial protein 18 expression by human colon epithelium. Infect Immun 70(2):953–963
Hase K, Murakami M et al (2003) Expression of LL-37 by human gastric epithelial cells as a potential host defense mechanism against Helicobacter pylori. Gastroenterology 125(6):1613–1625
Haussler MR, Haussler CA et al (2008) Vitamin D receptor: molecular signaling and actions of nutritional ligands in disease prevention. Nutr Rev 66(10 Suppl 2):S98–S112
Hertz CJ, Wu Q et al (2003) Activation of Toll-like receptor 2 on human tracheobronchial epithelial cells induces the antimicrobial peptide human beta defensin-2. J Immunol 171(12):6820–6826
Hoffmann JA, Reichhart JM (2002) Drosophila innate immunity: an evolutionary perspective. Nat Immunol 3(2):121–126
Hooper LV (2009) Do symbiotic bacteria subvert host immunity? Nat Rev Microbiol 7(5):367–374
Hooper LV, Macpherson AJ (2010) Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol 10(3):159–169
Hugot JP (2006) CARD15/NOD2 mutations in Crohn’s disease. Ann N Y Acad Sci 1072:9–18
Hugot JP, Chamaillard M et al (2001) Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature 411(6837):599–603
Islam D, Bandholtz L et al (2001) Downregulation of bactericidal peptides in enteric infections: a novel immune escape mechanism with bacterial DNA as a potential regulator. Nat Med 7(2):180–185
Kida Y, Shimizu T et al (2006) Sodium butyrate up-regulates cathelicidin gene expression via activator protein-1 and histone acetylation at the promoter region in a human lung epithelial cell line, EBC-1. Mol Immunol 43(12):1972–1981
Lande R, Gregorio J et al (2007) Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature 449(7162):564–569
Liu PT, Stenger S et al (2006) Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 311(5768):1770–1773
Ma Y, Su Q et al (1998) Differentiation-stimulated activity binds an ETS-like, essential regulatory element in the human promyelocytic defensin-1 promoter. J Biol Chem 273(15):8727–8740
Martineau AR, Timms PM et al (2011) High-dose vitamin D(3) during intensive-phase antimicrobial treatment of pulmonary tuberculosis: a double-blind randomised controlled trial. Lancet 377(9761):242–250
Maslowski KM, Vieira AT et al (2009) Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461(7268):1282–1286
Mygind PH, Fischer RL et al (2005) Plectasin is a peptide antibiotic with therapeutic potential from a saprophytic fungus. Nature 437(7061):975–980
Nell MJ, Tjabringa GS et al (2004) Bacterial products increase expression of the human cathelicidin hCAP-18/LL-37 in cultured human sinus epithelial cells. FEMS Immunol Med Microbiol 42(2):225–231
Nizet V, Ohtake T et al (2001) Innate antimicrobial peptide protects the skin from invasive bacterial infection. Nature 414(6862):454–457
O’Neil DA, Cole SP et al (2000) Regulation of human beta-defensins by gastric epithelial cells in response to infection with Helicobacter pylori or stimulation with interleukin-1. Infect Immun 68(9):5412–5415
O’Neil DA, Porter EM et al (1999) Expression and regulation of the human beta-defensins hBD-1 and hBD-2 in intestinal epithelium. J Immunol 163(12):6718–6724
Ogura Y, Bonen DK et al (2001) A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature 411(6837):603–606
Ong PY, Ohtake T et al (2002) Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med 347(15):1151–1160
Ouellette AJ (2010) Paneth cells and innate mucosal immunity. Curr Opin Gastroenterol 26(6):547–553
Prost LR, Sanowar S et al (2007) Salmonella sensing of anti-microbial mechanisms to promote survival within macrophages. Immunol Rev 219:55–65
Rabbani GH, Albert MJ et al (1999) Short-chain fatty acids improve clinical, pathologic, and microbiologic features of experimental shigellosis. J Infect Dis 179(2):390–397
Ramanathan B, Minton JE et al (2005) PU.1-mediated transcriptional regulation of prophenin-2 in primary bone marrow cells. Gene 352:1–9
Ramos HC, Rumbo M et al (2004) Bacterial flagellins: mediators of pathogenicity and host immune responses in mucosa. Trends Microbiol 12(11):509–517
Raqib R, Sarker P et al (2006) Improved outcome in shigellosis associated with butyrate induction of an endogenous peptide antibiotic. Proc Natl Acad Sci USA 103(24):9178–9183
Salzman NH, Ghosh D et al (2003) Protection against enteric salmonellosis in transgenic mice expressing a human intestinal defensin. Nature 422(6931):522–526
Salzman NH, Hung K et al (2010) Enteric defensins are essential regulators of intestinal microbial ecology. Nat Immunol 11(1):76–83
Sarker P, Ahmed S et al (2011) Phenylbutyrate counteracts Shigella mediated downregulation of cathelicidin in rabbit lung and intestinal epithelia: A potential therapeutic strategy. PLoS One 3(6):e20637
Sartor RB (2001) Induction of mucosal immune responses by bacteria and bacterial components. Curr Opin Gastroenterol 17(6):555–561
Schauber J, Svanholm C et al (2003) Expression of the cathelicidin LL-37 is modulated by short chain fatty acids in colonocytes: relevance of signalling pathways. Gut 52(5):735–741
Schneider T, Kruse T et al (2010) Plectasin, a fungal defensin, targets the bacterial cell wall precursor Lipid II. Science 328(5982):1168–1172
Sels J, Mathys J et al (2008) Plant pathogenesis-related (PR) proteins: a focus on PR peptides. Plant Physiol Biochem 46(11):941–950
Shafer WM, Qu X et al (1998) Modulation of Neisseria gonorrhoeae susceptibility to vertebrate antibacterial peptides due to a member of the resistance/nodulation/division efflux pump family. Proc Natl Acad Sci USA 95(4):1829–1833
Sherman H, Froy O (2008) Expression of human beta-defensin 1 is regulated via c-Myc and the biological clock. Mol Immunol 45(11):3163–3167
Sperandio B, Regnault B et al (2008) Virulent Shigella flexneri subverts the host innate immune response through manipulation of antimicrobial peptide gene expression. J Exp Med 205(5):1121–1132
Steinmann J, Halldorsson S et al (2009) Phenylbutyrate induces antimicrobial peptide expression. Antimicrob Agents Chemother 53(12):5127–5133
Talukder P, Satho T et al (2011) Trace metal zinc stimulates secretion of antimicrobial peptide LL-37 from Caco-2 cells through ERK and p38 MAP kinase. Int Immunopharmacol 11(1):141–144
Termen S, Tollin M et al (2008) PU.1 and bacterial metabolites regulate the human gene CAMP encoding antimicrobial peptide LL-37 in colon epithelial cells. Mol Immunol 45(15):3947–3955
Tjabringa GS, Aarbiou J et al (2003) The antimicrobial peptide LL-37 activates innate immunity at the airway epithelial surface by transactivation of the epidermal growth factor receptor. J Immunol 171(12):6690–6696
Travassos LH, Carneiro LA et al (2010) Nod1 and Nod2 direct autophagy by recruiting ATG16L1 to the plasma membrane at the site of bacterial entry. Nat Immunol 11(1):55–62
Wan M, Sabirsh A et al (2007) Leukotriene B4 triggers release of the cathelicidin LL-37 from human neutrophils: novel lipid-peptide interactions in innate immune responses. FASEB J 21(11):2897–2905
Wang TT, Dabbas B et al (2010) Direct and indirect induction by 1,25-dihydroxyvitamin D3 of the NOD2/CARD15-defensin beta2 innate immune pathway defective in Crohn disease. J Biol Chem 285(4):2227–2231
Wang TT, Nestel FP et al (2004) Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol 173(5):2909–2912
Wehkamp J, Harder J et al (2004) NOD2 (CARD15) mutations in Crohn’s disease are associated with diminished mucosal alpha-defensin expression. Gut 53(11):1658–1664
Wehkamp J, Salzman NH et al (2005) Reduced Paneth cell alpha-defensins in ileal Crohn’s disease. Proc Natl Acad Sci USA 102(50):18129–18134
Wehkamp J, Wang G et al (2007) The Paneth cell alpha-defensin deficiency of ileal Crohn’s disease is linked to Wnt/Tcf-4. J Immunol 179(5):3109–3118
Verbeek W, Lekstrom-Himes J et al (1999) Myeloid transcription factor C/EBPepsilon is involved in the positive regulation of lactoferrin gene expression in neutrophils. Blood 94(9):3141–3150
Verway M, Behr MA et al (2010) Vitamin D, NOD2, autophagy and Crohn’s disease. Expert Rev Clin Immunol 6(4):505–508
Yu FS, Cornicelli MD et al (2010) Flagellin stimulates protective lung mucosal immunity: role of cathelicidin-related antimicrobial peptide. J Immunol 185(2):1142–1149
Zanetti M (2004) Cathelicidins, multifunctional peptides of the innate immunity. J Leukoc Biol 75(1):39–48
Zasloff M (2002) Antimicrobial peptides of multicellular organisms. Nature 415(6870):389–395
Zhu S (2008a) Did cathelicidins, a family of multifunctional host-defense peptides, arise from a cysteine protease inhibitor? Trends Microbiol 16(8):353–360
Zhu S (2008b) Discovery of six families of fungal defensin-like peptides provides insights into origin and evolution of the CSalphabeta defensins. Mol Immunol 45(3):828–838
Acknowledgments
The authors’ research is supported by the Swedish Foundation for Strategic Research, the Torsten and Ragnar Söderbergs Foundation, the Swedish Research Council, the Swedish International Development Cooperation Agency (SIDA), the Swedish Cancer Society and Karolinska Institutet, the Icelandic Centre for Research (RANNIS) and University of Iceland, and the Foundations of Magnus Bergwall, Åke Wiberg, and DA Hagelén.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Basel AG
About this chapter
Cite this chapter
Agerberth, B., Bergman, P., Gudmundsson, G.H. (2013). Helping the Host: Induction of Antimicrobial Peptides as a Novel Therapeutic Strategy Against Infections. In: Hiemstra, P., Zaat, S. (eds) Antimicrobial Peptides and Innate Immunity. Progress in Inflammation Research. Springer, Basel. https://doi.org/10.1007/978-3-0348-0541-4_14
Download citation
DOI: https://doi.org/10.1007/978-3-0348-0541-4_14
Published:
Publisher Name: Springer, Basel
Print ISBN: 978-3-0348-0540-7
Online ISBN: 978-3-0348-0541-4
eBook Packages: MedicineMedicine (R0)