Abstract
A range of antibiotics, in addition to those that target folate metabolism, have demonstrated antimalarial activity. They include those belonging to the lincosamides, tetracyclines and macrolides classes and fosmidomycin, a derivative of phosphonic acid. Predominantly, they target pathways within the apicoplast, a relict plastid found in most apicomplexan parasites including Plasmodium. In general, they are not highly active against malarial parasites and are slow acting but are clinically useful when used in combination with other antimalarial drug classes. In addition, some are safe to use in pregnancy and for the treatment of small children. Here, we review the current understanding of their mechanisms of action and clinical use.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
There are many non-antifolate antibiotics that have antimalarial activity including members belonging to the following classes: fluoroquinolones, lincosamides, tetracyclines and macrolides. The fluoroquinolones will not be discussed further here, as they were moderately active against Plasmodium falciparum in vitro [1, 2], but this property did not extend to useful antimalarial efficacy when tested in vivo [3, 4]. Fosmidomycin is a phosphonic acid derivative that is also included in discussion, as a potentially interesting new class of antimalarial. The lincosamides, tetracyclines and macrolides have established antimalarial properties and are clinically useful in particular circumstances. None of these antibiotics is highly active and rapidly acting; so, their usage requires combination with other rapidly effective classes of antimalarial, where they contribute to increasing cure rates even with shorter courses of treatment. Some antibiotics have the additional advantages of being safe to use in pregnancy or for small children (discussed below).
2 Clindamycin
The lincosamides are named after lincomycin that was extracted from Streptomyces lincolnensis in a soil sample in 1962. The structure of lincosamides is unusual, as are their antimicrobial properties. Clindamycin was the only semi-synthetic lincosamide to be developed for clinical use (Fig. 1). Here, it has activity against Gram-positive bacteria and many anaerobes, but not against Gram-negative aerobes. More relevant to its antimalarial properties, clindamycin is active against several apicomplexans including Plasmodium spp., Toxoplasma gondii and Babesia microti.
2.1 Mechanism of Action
Clindamycin acts at the same site on ribosomes as erythromycin and chloramphenicol. It inhibits protein synthesis in bacteria by binding to the 50S ribosomal unit and it can exert concentration-dependent bactericidal activity beyond its accepted bacteriostatic effects [5]. In its actions against apicomplexans, clindamycin targets their apicoplast organelles and interferes with function and survival after one or two rounds of parasite replication have taken place, resulting in a “delayed-death” phenotype. This is well described for Toxoplasma [6] as well as for P. falciparum with correlations between in vitro and in vivo pharmacodynamics being observed [7–9]. Further evidence for this proposed mechanism of action for clindamycin comes from observations of mutations in the apicoplast genome of parasites obtained from the Peruvian Amazon. A point-mutation in the apicoplast-encoded 23S rRNA gene that confers resistance to lincosamides in other organisms was identified in parasites that were 100-fold more resistant to clindamycin than wild-type parasites [10].
2.2 Pharmacokinetics
Clindamycin has good (>90%) bioavailability after oral dosing, is protein bound (>90%) and widely distributed in tissues and has an elimination half-time of approximately 2–3 h. It is eliminated mainly by biliary excretion (with 20% excreted by kidneys) after metabolism to three major derivatives [11].
2.3 Usage in Malaria
The antimalarial properties of clindamycin have been confirmed in many studies, including earlier studies after the first one in 1975 that used clindamycin as a monotherapy before its more successful use in combination treatment regimens [11]. The interesting mechanism of action of clindamycin and its pharmacokinetic properties suggest that a minimum of 5 days treatment with at least twice-daily dosing is needed to achieve adequate cure rates in uncomplicated malaria [11], a regimen that is not currently recommended.
Table 1 summarises the antimalarial properties of clindamycin combined with quinine. Clindamycin dosages ranging from 5 mg/kg twice daily given with quinine, to 8 mg/kg three times a day or 12 mg/kg twice daily in general give acceptable cure rates. One small study [21] found that a 3-day treatment of the combination was as effective as a 7-day monotherapy regimen with quinine alone in travellers returning with uncomplicated malaria. Clindamycin can be used in children and pregnant women and may be combined with artesunate as a partner antimalarial, although short-course regimens may need further study to confirm efficacy [24].
Clindamycin may be less effective in treating P. vivax infections [11] even when prolonged courses of monotherapy are used, although a later review suggested that clindamycin is more effective than tetracyclines [25]. It also has no apparent synergism with quinine for P. vivax and nor does it have anti-relapse properties [11].
2.4 Tolerance and Safety
Non-specific and relatively common gastro-intestinal side effects of nausea, vomiting, abdominal pain and diarrhoea are associated with clindamycin use. Toxin-producing Clostridium difficile colitis can also complicate clindamycin therapy, most commonly in hospitalised patients treated with prolonged courses of clindamycin, and not with the antimalarial regimes that have been most studied in recent years. Rashes may be relatively common side effects, but severe eruptions are not. Transient reversible neutropenia and thrombocytopenia have also occurred.
3 Tetracyclines Including Doxycycline
The discovery of chlortetracycline in 1948 preceded that of clindamycin, although it was also from another soil organism Streptomyces aureofasciens. Catalytic dehydrogenation of chlortetracycline gave tetracycline in 1953. This class of antibiotic has wide antimicrobial properties, ranging from Gram-positive and Gram-negative bacteria, rickettsiae (where its use can be diagnostic), mycoplasmas, chlamydia and protozoa. Doxycycline is a semi-synthetic derivative of tetracycline first developed in 1967. The structures of tetracycline and doxycycline are given in Fig. 2.
3.1 Mechanism of Action
The tetracyclines including doxycycline act by inhibiting protein synthesis by binding to the 30S ribosomal subunit. They are relatively slow acting as antimalarial agents. Doxycycline is useful as a prophylactic agent on its own, as well as being used in combination treatment regimens to increase cure rates of conventional antimalarial agents [26]. It has limited casual prophylactic activity [26] and does not kill hypnozoites.
3.2 Pharmacokinetics
Doxycyline has ~90% oral bioavailability, which is reduced by food and delayed by alcohol, with peaks without delay occurring at ~2 h after administration [26]. Co-administration with cations such as iron supplements reduces absorption by chelation of the antibiotic, and milk may reduce absorption [26]. Plasma protein binding of doxycycline is 90% and elimination half-time is 18 h, making this one of the most convenient tetracyclines to use in practise. Most elimination of unchanged drug is through the gastrointestinal tract, with about a third being renally excreted.
3.3 Usage in Malaria
Tetracycline requires dosing 4 times as day and is therefore cumbersome to use as an antimalarial. Doxycyline (for adults up to 100 mg base twice daily, with another antimalarial) should only be used in combination with rapidly acting antimalarials such as quinine to increase cure rates, and not on its own. Table 2 summarises antimalarial treatment properties of doxycycline [26]. It can be used as a prophylactic antimalarial (for adults up to 100 mg base once daily starting before travel and continuing for 4 weeks after return), even in areas of multidrug-resistant parasites [26].
3.4 Safety and Toxicity
The tetracyclines are not recommended in pregnancy, and in children whose teeth can be stained (8 years or less). Doxycycline is a photosensitising antibiotic and can also cause oesophageal erosions and heartburn if taken incorrectly. Nausea and abdominal pain are relatively common, but frequency can be reduced by taking doxycycline with food [26].
4 Azithromycin
Azithromycin is a semi-synthetic derivative of erythromycin, whereby a methyl-substituted nitrogen atom is incorporated into the lactone ring system to improve acid stability (Fig. 3). In contrast to doxycycline, azithromycin can be used in younger children and in pregnancy, but its much increased cost compared with doxycycline may limit its applicability for management of malaria. Azithromycin is useful in the management of respiratory tract infections and has activity against Toxoplasma and can be used to treat uncomplicated babesiosis when combined with atovaquone in immunocompetent individuals [32].
4.1 Mechanism of Action
Azithromycin acts by binding to the 50S ribosomal sub-unit of susceptible microorganisms and inhibiting protein synthesis. Consistent with the activities of other antimalarial antibiotics, azithromycin is relatively slow acting and should be used in combination therapies for malaria. There may be some cross-resistance between antibiotics as observed for clindamycin-resistant T. gondii.
4.2 Pharmacokinetics
Azithromycin has moderate oral bioavailability (37% after 500 mg) and this is reduced significantly (by 50%) if given with food; hence, it should be used either 1 h before food or 2 h after. Antacids also reduce availability. The degree of protein binding of azithromycin is dose-dependent, but not usually >50%. The drug is extensively distributed in tissues, which act as a depot with an elimination half-time of ~70 h. Most drugs are probably eliminated unchanged by biliary and gastrointestinal excretion.
4.3 Clinical Studies
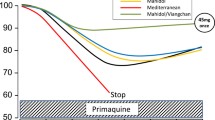
Azithromycin by itself is not useful to treat uncomplicated P. falciparum or P. vivax infections [33] as failure rates can exceed 50% when conventional antibacterial doses for adults of 0.5 g per day for 3 days are used. Cure rates may be increased if the dose of azithromycin is also increased (to for example, 1 g per day) in combination therapies, but comparisons with other antimalarial combinations are not so encouraging (Fig. 4). Current evidence suggests that other combinations should be used to treat malaria unless there is no choice.
Efficacy of azithromycin containing treatment regimens for P. falciparum (28 day follow-up). Abbr: AZ azithromycin, CQ chloroquine, Artm artemether, Art artesunate, dihydroart dihydroartemisinin, Q quinine, CI confidence interval, d days. Symbols: Asterisk PCR-corrected, double asterisk partially PCR-corrected, section sign study conducted in an area without malaria transmission (Bangkok). The AZ dose in the combination with artemisinin (300 mg) was 500 mg at start, followed by 250 mg after 24 h and 48 h. An interrupted line has been drawn at the 90% efficacy level, the minimum level for the 95% confidence interval for a potentially useful drug regimen as recommended by WHO [34]. Taken from [33] with kind permission from the authors and John Wiley & Sons, Ltd on behalf of The Cochrane Collaboration. Copyright Cochrane Collaboration.
4.4 Safety and Toxicity
Azithromycin is relatively well tolerated, with mild gastrointestinal side effects being most commonly reported. Occasional abnormalities in liver function are observed and allergic reactions are rare. Nausea may be more common with higher dose regimens [33].
5 Fosmidomycin
Fosmidomycin is a natural antibiotic, originally derived from Streptomyces lavendulae. It is currently being investigated as a combination partner in antimalarial chemotherapy regimens, with the idea that it represents a non-artemisinin class of antimalarial with an unusual mode of action. Fosmidomycin’s relatively simple chemical structure (Fig. 5) makes it amenable to complete synthesis, which is how it is currently made for investigational studies. Fujisawa Pharmaceutical Company in Osaka, Japan [35], originally developed fosmidomycin as an antibacterial agent [36–39] for treating urinary tract infections approximately three decades ago. It is most effective against enterobacteria and not against Gram-positive organisms or anaerobes. Since its discovery, cephalosporins have emerged as being more effective for recurrent infections and the development of fosmidomycin as an antibacterial agent has not been taken further forward, until it has been repurposed as an antimalarial.
6 Mechanism of Action
The repurposing of fosmidomycin as an antimalarial depended on several advances in understanding the biology of the malarial parasite. One advance lay in the recognition of the plastid organelle as an excellent target for new drugs, as no similar structure exists in animal cells. Another advance was the identification of an alternative [nonmevalonate or 1-deoxy-d-xylulose 5-phosphate (DOXP)] pathway for isoprenoid synthesis in parasites that was hitherto described in plants and eubacteria. Key enzymes forming part of this synthesis pathway include DOXP reductoisomerase and 2C-methyl-d-erythritol-4-(cytidine-5-diphospho) transferase (Fig. 6) and are located in the parasite’s apicoplast. This pathway contributes to many functions such as prenylation of membrane-bound proteins and synthesis of carotenoids and terpenoids.
The 1-deoxy-d-xylulose 5-phosphate (DOXP) pathway for isoprenoid synthesis and the sites of action of fosmidomycin (Fos). GAP glyceraldehyde-3-phosphate, DXS DOXP synthase, DXR DOXP reductoisomerase, MEP 2C-methyl-d-erythritol-4-phosphate, MCT 2C-methyl-d-erythritol-4-(cytidine-5-diphospho) transferase, CDP-ME 4-(cytidine-5-diphospho)-2C-methyl-d-erythritol
Hassan Jomaa and colleagues [40] tested the idea that inhibiting this pathway would prove lethal to parasites by expressing a recombinant version of DOXP reductoisomerase and showing that it was inhibited by fosmidomycin (with an inhibitory constant of ~30 nM). They also showed that fosmidomycin and compound FR-900098 (Fig. 5), a compound that acts as a pro-drug for fosmidomycin, killed cultured P. falciparum, including highly chloroquine-resistant strains (IC50 values ranging from 300 to 1,200 nM), as well as being able to cure mice infected with P. vinckei. Recently, it has been reported that fosmidomycin also targets a second enzyme in the DOXP pathway, 2C-methyl-d-erythritol-4-(cytidine-5-diphospho) transferase (Fig. 6) [41]. Other recent studies have suggested that the uptake of fosmidomycin, which is highly charged, requires specific transport mechanisms [42, 43]. This includes the new permeability pathways (NPP) that are responsible for altered plasma membrane permeability of the host erythrocyte as intracellular plasmodial parasites mature [42, 44]. These new data not only explain the selectively of fosmidomycin for plasmodial parasites over closely related species (e.g. Toxoplasma) but can also be used to test potential resistance mechanisms in Plasmodium spp.
6.1 Pharmacokinetics
Fosmidomycin has relatively poor oral bioavailability (~25%) and is poorly protein bound (<5%) with an elimination half-time of 1.6–1.8 h [45]. This elimination half time is somewhat prolonged in subjects with malaria to 3.4 h (range 1.4–11.8 h) and not altered importantly after co-administration with clindamycin in one study [46], although particular dosing regimens of this combination (fosmidomycin and clindamycin) may influence pharmacokinetic behaviour of each drug [47].
6.2 Fosmidomycin in Malaria
Table 3 summarises studies of fosmidomycin in children and adults with malaria. Monotherapy studies with fosmidomycin have confirmed its antimalarial activity in patients, and also that, unlike clindamycin, it has relatively rapid antimalarial actions. However, recrudescence rates are rather high, compelling the choice of an appropriate combination partner to achieve adequate clinical and parasitological cure rates. Clindamycin has been the most thoroughly studied partner drug and results of various studies are also included in Table 3. In general, a 3-day treatment regimen with 30 mg/kg fosmidomycin and 10 mg/kg clindamycin given in a 8 or 12 h interval and in the populations reported provided adequate responses in adults and children except for one study in children aged <3 years [53]. This combination was also well tolerated, with mild gastrointestinal side effects being some of the most frequent (Table 3).
References
Krishna S, Davis TM, Chan PC, Wells RA, Robson KJ (1988) Ciprofloxacin and malaria. Lancet 1:1231–1232
Tripathi KD, Sharma AK, Valecha N, Biswas S (1993) In vitro activity of fluoroquinolones against chloroquine-sensitive and chloroquine-resistant Plasmodium falciparum. Indian J Malariol 30:67–73
Havemann K, Bhibi P, Hellgren U, Rombo L (1992) Norfloxacin is not effective for treatment of Plasmodium falciparum infection in Kenya. Trans R Soc Trop Med Hyg 86:586
Watt G, Shanks GD, Edstein MD, Pavanand K, Webster HK, Wechgritaya S (1991) Ciprofloxacin treatment of drug-resistant falciparum malaria. J Infect Dis 164:602–604
Reusser F (1975) Effect of lincomycin and clindamycin on peptide chain initiation. Antimicrob Agents Chemother 7:32–37
Fichera ME, Bhopale MK, Roos DS (1995) In vitro assays elucidate peculiar kinetics of clindamycin action against Toxoplasma gondii. Antimicrob Agents Chemother 39:1530–1537
Burkhardt D, Wiesner J, Stoesser N, Ramharter M, Uhlemann AC, Issifou S, Jomaa H, Krishna S, Kremsner PG, Borrmann S (2007) Delayed parasite elimination in human infections treated with clindamycin parallels ‘delayed death’ of Plasmodium falciparum in vitro. Int J Parasitol 37:777–785
Fichera ME, Roos DS (1997) A plastid organelle as a drug target in apicomplexan parasites. Nature 390:407–409
Kohler S, Delwiche CF, Denny PW, Tilney LG, Webster P, Wilson RJ, Palmer JD, Roos DS (1997) A plastid of probable green algal origin in Apicomplexan parasites. Science 275:1485–1489
Dharia NV, Plouffe D, Bopp SE, Gonzalez-Paez GE, Lucas C, Salas C, Soberon V, Bursulaya B, Kochel TJ, Bacon DJ et al (2010) Genome scanning of Amazonian Plasmodium falciparum shows subtelomeric instability and clindamycin-resistant parasites. Genome Res 20:1534–1544
Lell B, Kremsner PG (2002) Clindamycin as an antimalarial drug: review of clinical trials. Antimicrob Agents Chemother 46:2315–2320
Miller LH, Glew RH, Wyler DJ, Howard WA, Collins WE, Contacos PG, Neva FA (1974) Evaluation of clindamycin in combination with quinine against multidrug-resistant strains of Plasmodium falciparum. Am J Trop Med Hyg 23:565–569
Clyde DF, Gilman RH, McCarthy VC (1975) Antimalarial effects of clindamycin in man. Am J Trop Med Hyg 24:369–370
Hall AP, Doberstyn EB, Nanokorn A, Sonkom P (1975) Falciparum malaria semi-resistant to clindamycin. Br Med J 2:12–14
Kremsner PG, Zotter GM, Feldmeier H, Graninger W, Rocha RM, Wiedermann G (1988) A comparative trial of three regimens for treating uncomplicated falciparum malaria in Acre, Brazil. J Infect Dis 158:1368–1371
Kremsner PG, Winkler S, Brandts C, Neifer S, Bienzle U, Graninger W (1994) Clindamycin in combination with chloroquine or quinine is an effective therapy for uncomplicated Plasmodium falciparum malaria in children from Gabon. J Infect Dis 169:467–470
Kremsner PG, Radloff P, Metzger W, Wildling E, Mordmuller B, Philipps J, Jenne L, Nkeyi M, Prada J, Bienzle U et al (1995) Quinine plus clindamycin improves chemotherapy of severe malaria in children. Antimicrob Agents Chemother 39:1603–1605
Metzger W, Mordmuller B, Graninger W, Bienzle U, Kremsner PG (1995) High efficacy of short-term quinine-antibiotic combinations for treating adult malaria patients in an area in which malaria is hyperendemic. Antimicrob Agents Chemother 39:245–246
Vaillant M, Millet P, Luty A, Tshopamba P, Lekoulou F, Mayombo J, Georges AJ, Deloron P (1997) Therapeutic efficacy of clindamycin in combination with quinine for treating uncomplicated malaria in a village dispensary in Gabon. Trop Med Int Health 2:917–919
Pukrittayakamee S, Chantra A, Vanijanonta S, Clemens R, Looareesuwan S, White NJ (2000) Therapeutic responses to quinine and clindamycin in multidrug-resistant falciparum malaria. Antimicrob Agents Chemother 44:2395–2398
Parola P, Ranque S, Badiaga S, Niang M, Blin O, Charbit JJ, Delmont J, Brouqui P (2001) Controlled trial of 3-day quinine-clindamycin treatment versus 7-day quinine treatment for adult travelers with uncomplicated falciparum malaria imported from the tropics. Antimicrob Agents Chemother 45:932–935
McGready R, Cho T, Samuel VL, Brockman A, van Vugt M, Looareesuwan S, White NJ, Nosten F (2001) Randomized comparison of quinine-clindamycin versus artesunate in the treatment of falciparum malaria in pregnancy. Trans R Soc Trop Med Hyg 95:651–656
WHO (1996) Assessment of therapeutic efficacy of antimalarial drugs for uncomplicated falciparum malaria in areas with intense trassmission. World Health Organisation, Geneva
Ramharter M, Oyakhirome S, Klein Klouwenberg P, Adegnika AA, Agnandji ST, Missinou MA, Matsiegui PB, Mordmuller B, Borrmann S, Kun JF et al (2005) Artesunate-clindamycin versus quinine-clindamycin in the treatment of Plasmodium falciparum malaria: a randomized controlled trial. Clin Infect Dis 40:1777–1784
Pukrittayakamee S, Imwong M, Looareesuwan S, White NJ (2004) Therapeutic responses to antimalarial and antibacterial drugs in vivax malaria. Acta Trop 89:351–356
Tan KR, Magill AJ, Parise ME, Arguin PM (2011) Doxycycline for malaria chemoprophylaxis and treatment: report from the CDC expert meeting on malaria chemoprophylaxis. Am J Trop Med Hyg 84:517–531
Clyde DF, Miller RM, DuPont HL, Hornick RB (1971) Antimalarial effects of tetracyclines in man. J Trop Med Hyg 74:238–242
Ponnampalam JT (1981) Doxycycline in the treatment of falciparum malaria among aborigine children in West Malaysia. Trans R Soc Trop Med Hyg 75:372–377
Taylor WR, Widjaja H, Richie TL, Basri H, Ohrt C, Tjitra TE, Jones TR, Kain KC, Hoffman SL (2001) Chloroquine/doxycycline combination versus chloroquine alone, and doxycycline alone for the treatment of Plasmodium falciparum and Plasmodium vivax malaria in northeastern Irian Jaya, Indonesia. Am J Trop Med Hyg 64:223–228
Alecrim MG, Lacerda MV, Mourao MP, Alecrim WD, Padilha A, Cardoso BS, Boulos M (2006) Successful treatment of Plasmodium falciparum malaria with a six-dose regimen of artemether-lumefantrine versus quinine-doxycycline in the Western Amazon region of Brazil. Am J Trop Med Hyg 74:20–25
Ejaz A, Haqnawaz K, Hussain Z, Butt R, Awan ZI, Bux H (2007) Treatment of uncomplicated Plasmodium falciparum malaria with quinine-doxycycline combination therapy. J Pak Med Assoc 57:502–505
Krause PJ, Lepore T, Sikand VK, Gadbaw J Jr, Burke G, Telford SR 3rd, Brassard P, Pearl D, Azlanzadeh J, Christianson D et al (2000) Atovaquone and azithromycin for the treatment of babesiosis. N Engl J Med 343:1454–1458
van Eijk AM, Terlouw DJ (2011) Azithromycin for treating uncomplicated malaria. Cochrane Database Syst Rev CD006688
WHO (2006) Guidelines for the treatment of malaria. World Health Organisation, Geneva
Kamiya T, Hashimoto M, Hemmi K, Takeno H (1980) Hydroxyaminohydrocarbon-phosphonic acids. US Patent 4206156
Kanimoto Y, Greenwood D (1987) Activity of fosmidomycin in an in vitro model of the treatment of bacterial cystitis. Infection 15:465–468
Kuroda Y, Okuhara M, Goto T, Okamoto M, Terano H, Kohsaka M, Aoki H, Imanaka H (1980) Studies on new phosphonic acid antibiotics. IV. Structure determination of FR-33289, FR-31564 and FR-32863. J Antibiot (Tokyo) 33:29–35
Mine Y, Kamimura T, Nonoyama S, Nishida M, Goto S, Kuwahara S (1980) In vitro and in vivo antibacterial activities of FR-31564, a new phosphonic acid antibiotic. J Antibiot (Tokyo) 33:36–43
Okuhara M, Kuroda Y, Goto T, Okamoto M, Terano H, Kohsaka M, Aoki H, Imanaka H (1980) Studies on new phosphonic acid antibiotics. III. Isolation and characterization of FR-31564, FR-32863 and FR-33289. J Antibiot (Tokyo) 33:24–28
Jomaa H, Wiesner J, Sanderbrand S, Altincicek B, Weidemeyer C, Hintz M, Turbachova I, Eberl M, Zeidler J, Lichtenthaler HK et al (1999) Inhibitors of the nonmevalonate pathway of isoprenoid biosynthesis as antimalarial drugs. Science 285:1573–1576
Zhang B, Watts KM, Hodge D, Kemp LM, Hunstad DA, Hicks LM, Odom AR (2011) A second target of the antimalarial and antibacterial agent fosmidomycin revealed by cellular metabolic profiling. Biochemistry 50:3570–3577
Baumeister S, Wiesner J, Reichenberg A, Hintz M, Bietz S, Harb OS, Roos DS, Kordes M, Friesen J, Matuschewski K et al (2011) Fosmidomycin uptake into Plasmodium and Babesia-infected erythrocytes is facilitated by parasite-induced new permeability pathways. PLoS One 6:e19334
Nair SC, Brooks CF, Goodman CD, Strurm A, McFadden GI, Sundriyal S, Anglin JL, Song Y, Moreno SN, Striepen B (2011) Apicoplast isoprenoid precursor synthesis and the molecular basis of fosmidomycin resistance in Toxoplasma gondii. J Exp Med 208:1547–1559
Staines HM, Ellory JC, Chibale K (2005) The new permeability pathways: targets and selective routes for the development of new antimalarial agents. Comb Chem High Throughput Screen 8:81–88
Kuemmerle HP, Murakawa T, De Santis F (1987) Pharmacokinetic evaluation of fosmidomycin, a new phosphonic acid antibiotic. Chemioterapia 6:113–119
Na-Bangchang K, Ruengweerayut R, Karbwang J, Chauemung A, Hutchinson D (2007) Pharmacokinetics and pharmacodynamics of fosmidomycin monotherapy and combination therapy with clindamycin in the treatment of multidrug resistant falciparum malaria. Malar J 6:70
Ruangweerayut R, Looareesuwan S, Hutchinson D, Chauemung A, Banmairuroi V, Na-Bangchang K (2008) Assessment of the pharmacokinetics and dynamics of two combination regimens of fosmidomycin-clindamycin in patients with acute uncomplicated falciparum malaria. Malar J 7:225
Lell B, Ruangweerayut R, Wiesner J, Missinou MA, Schindler A, Baranek T, Hintz M, Hutchinson D, Jomaa H, Kremsner PG (2003) Fosmidomycin, a novel chemotherapeutic agent for malaria. Antimicrob Agents Chemother 47:735–738
Missinou MA, Borrmann S, Schindler A, Issifou S, Adegnika AA, Matsiegui PB, Binder R, Lell B, Wiesner J, Baranek T et al (2002) Fosmidomycin for malaria. Lancet 360:1941–1942
Borrmann S, Adegnika AA, Matsiegui PB, Issifou S, Schindler A, Mawili-Mboumba DP, Baranek T, Wiesner J, Jomaa H, Kremsner PG (2004) Fosmidomycin-clindamycin for Plasmodium falciparum infections in African children. J Infect Dis 189:901–908
Borrmann S, Issifou S, Esser G, Adegnika AA, Ramharter M, Matsiegui PB, Oyakhirome S, Mawili-Mboumba DP, Missinou MA, Kun JF et al (2004) Fosmidomycin-clindamycin for the treatment of Plasmodium falciparum malaria. J Infect Dis 190:1534–1540
Borrmann S, Adegnika AA, Moussavou F, Oyakhirome S, Esser G, Matsiegui PB, Ramharter M, Lundgren I, Kombila M, Issifou S et al (2005) Short-course regimens of artesunate-fosmidomycin in treatment of uncomplicated Plasmodium falciparum malaria. Antimicrob Agents Chemother 49:3749–3754
Borrmann S, Lundgren I, Oyakhirome S, Impouma B, Matsiegui PB, Adegnika AA, Issifou S, Kun JF, Hutchinson D, Wiesner J et al (2006) Fosmidomycin plus clindamycin for treatment of pediatric patients aged 1 to 14 years with Plasmodium falciparum malaria. Antimicrob Agents Chemother 50:2713–2718
Oyakhirome S, Issifou S, Pongratz P, Barondi F, Ramharter M, Kun JF, Missinou MA, Lell B, Kremsner PG (2007) Randomized controlled trial of fosmidomycin-clindamycin versus sulfadoxine-pyrimethamine in the treatment of Plasmodium falciparum malaria. Antimicrob Agents Chemother 51:1869–1871
Acknowledgments
We thank Peter Kremsner and David Hutchinson for useful discussion and the EDTCP (project code: IP.2008.31060.003) for financial support.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Basel AG
About this chapter
Cite this chapter
Krishna, S., Staines, H.M. (2011). Non-Antifolate Antibiotics: Clindamycin, Doxycycline, Azithromycin and Fosmidomycin. In: Staines, H., Krishna, S. (eds) Treatment and Prevention of Malaria. Milestones in Drug Therapy. Springer, Basel. https://doi.org/10.1007/978-3-0346-0480-2_8
Download citation
DOI: https://doi.org/10.1007/978-3-0346-0480-2_8
Published:
Publisher Name: Springer, Basel
Print ISBN: 978-3-0346-0479-6
Online ISBN: 978-3-0346-0480-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)