Abstract
The emergence of multi-drug resistant strains of Plasmodium falciparum has rendered many affordable antimalarials, such as chloroquine, much less effective in addressing the severe health issues in sub-Saharan Africa, Southeast Asia and the Amazon region. In order to overcome the neurotoxicity of an initial series of artemisinin-derived drugs and their relatively high production costs, an intensive and all-inclusive research programme to develop new derivatives has been undertaken. Two efficient antimalarial drug candidates of different chemotype have been devised, the artemisinin derivative artemisone and 1,2,4-troxolane OZ277. Both are nontoxic, more potent than artemisinin and should be affordable to people of endemic regions. The same may hold for the backup candidates artemiside and OZ439.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Great efforts have been expended over the last 30 years to discover new and efficacious endoperoxide antimalarials based on a natural product isolated from sweet wormwood – artemisinin, and related derivatives (collectively known as artemisinins) - primarily because, until very recently [1, 2], resistance to this type of drug had not been observed (Fig. 1) [3].
The main drawback of the initial series of artemisinin derivatives (Fig. 1) is their relative metabolic instability, i.e., susceptibility to hydrolysis (esters), or oxidative-dealkylation (ethers) to dihydroartemisinin [4]. Dihydroartemisinin, apart from being a more potent antimalarial than artemisinin [5], was found to be neurotoxic in vitro [6, 7] and in mice [8]. However, similar neurotoxicity has not been observed in humans [9]. Although embryotoxicity has been detected within a narrow window of embryogenesis, this has not been convincingly observed in clinical trials from 1,837 pregnant women [10].
These potential toxicity issues provoked an extensive search for metabolically stable artemisinin derivatives and two major semi-synthetic artemisinin sub-classes were developed: C(10) deoxyartemisinin derivatives usually functionalized at C(9) or at C(14) (5) [11], and derivatives possessing a new C(10)-NR, or C(10)-C bond (6–8) [12–15]. The second sub-class is more diversified with artemisinin-derived dimers and artemisone (9e) as the most prominent members (Figs. 2 and 3).
The quest for efficacious and cheap antimalarial drugs that can be administered as a single dose, preferably orally, is not limited to natural product-derived semi-synthetic artemisinins, like artemisone, but also to other classes of peroxide antimalarials. Of these, the most prominent peroxide classes are the fully synthetic 1,2,4-trioxanes[16, 17], 1,2,4-trioxolanes (ozonides, OZs) and mixed 1,2,4,5-tetraoxanes [18–20]. Two representatives of this class that have entered studies in humans are discussed below in detail.
2 Artemisone (Artemifon)
With the aim of preventing metabolic transformation of artemisinins to dihydroartemisinin (1, Fig. 1) and the drive to improve pharmacokinetic characteristics, several 10-(alkylamino)artemisinins 9 were designed (Fig. 3) [21, 22]. All the tested compounds showed excellent in vivo activities against P. berghei (9c was the most active derivative, almost 25 times (given s.c.) and 7 times (given p.o.) more active than artesunate 4). Unfortunately, 9c suffers from serious neurotoxicity issues even at low doses, thus indicating, that more lipophilic artemisinins are more toxic [21, 23].
A detailed antimalarial efficacy and drug–drug interaction study of artemisone (a drug examined recently in clinical Phase II trials [24]) was performed (9e, Fig. 3) [25]. It was shown that the in vitro antimalarial activities of artemisone against 12 different P. falciparum strains were comparable (exhibiting a mean IC50 value of 0.83 nM), independent of their drug-susceptibility profile to other antimalarial drug classes [21, 25]. During examination of the in vitro drug–drug interaction against drug sensitive 3D7 and multi-drug resistant K1 strains, it was noticed that artemisone showed slight antagonistic effects with chloroquine, amodiaquine, tafenoquine, atovaquone or pyrimethamine, and slight synergism with mefloquine. In vivo screening using the 4-day Peters test against drug-susceptible (NY), primaquine-resistant (P) and sulphadoxine/pyrimethamine-resistant (KFY) lines of P. berghei, chloroquine-resistant (NS) and artemisinin-resistant lines of P. yoelii NS and drug-susceptible P. chabaudi (AS) showed artemisone has superior ED50 and ED90 activity in comparison with artesunate (4, Fig. 1). Artemisone exhibited a 7-times greater activity (lower dosage) than artesunate (artemisone ED90 = 12.13 mg/kg vs. artesunate ED90 = 87.50 mg/kg) against the P. yoelii artemisinin-resistant line. The above results appear quite important in light of the recent in vitro isolation of artemether-resistant P. falciparum strains from humans [26] and emerging evidence for resistance in vivo [1, 2], suggesting more potent derivatives may be efficacious where first generation compounds are failing.
During in vivo drug–drug interaction examinations against the drug-susceptible P. berghei NY and the mefloquine-resistant P. berghei N1100 lines, artemisone showed synergism with mefloquine against both parasite lines. In combination with chloroquine, no interaction against drug-susceptible P. berghei NY parasites was detected; however, a synergistic effect against the chloroquine-resistant line, P. yoelii NS, was observed.
No dihydroartemisinin had been produced after 30 min, when isotopically labelled artemisone 9e* (Scheme 1) was incubated with human liver microsomes. Only dehydrogenated 12 and mono-hydroxylated metabolites 10 and 11 and 13 and 14, with syn-hydroxyl and peroxide groups were observed (Scheme 1) [21], clearly distinguishing artemisone and similar compounds from the first-generation artemisinins.Footnote 1 Incubation with microsomes and 14 recombinant CYP isoforms, together with selective inhibitors of CYP, showed that artemisone was primarily metabolised by recombinant CYP3A4. Interestingly, artemisinin induces its own metabolism [27] and is metabolised principally by CYP2B6 [28]. These results indicate that artemisone and artemisinin, in spite of being structurally similar, have a different metabolic profile in P. falciparum; therefore, it is possible that they can exert their antimalarial activity through similar but not identical mechanisms (vide infra). Isolated artemisone metabolites were tested against the P. falciparum K1 strain and were also found to be potent antimalarials, with 11 and 12 being the most active (11: IC50 = 5.51 nM and 12: IC50 = 4.26 nM, artemisone: IC50 = 1.99 nM) [21, 29].
In preclinical studies, artemisone showed enhanced efficacy and improved pharmacokinetics in comparison with artesunate and did not demonstrate neurotoxicity in vitro and in vivo [21, 29], which is a characteristic of the current artemisinin derivatives used in clinical treatment [30]. Administration of artemisone as a single dose (10–80 mg) or multiple doses (40 mg or 80 mg given once daily for 3 days) was well tolerated. It appears that artemisone is devoid of time-dependent pharmacokinetics (unlike artemisinin and artemether), with comparable C max, AUC and t ½ values after the first and third doses following the 3-day courses of artemisone. Although not being so active in vitro as the parent drug, the relatively high concentrations of metabolites obtained after artemisone administration probably add to the overall parasiticidal effect of artemisone [29]. In vivo testing on non-immune Aotus monkeys infected with P. falciparum showed that a single dose of artemisone (10 mg/kg) in combination with single doses of mefloquine (12.5 mg/kg or 5 mg/kg) cleared parasitaemia by day 1, with complete cure for all four monkeys tested [31]. With a single dose of mefloquine (2.5 mg/kg) parasitaemia was cleared by day 1 but without cure. For 3 days of treatment with a combination of artemisone (10 mg/kg/day) and amodiaquine (20 mg/kg/day), all three monkeys tested were cured, in contrast to those that were administered with the individual drugs for 3 days. From this study, it is clear that various total dosages of artemisone (20–90 mg/kg) alone, administered over 1–3 days, were unable to cure non-immune Aotus monkeys infected with P. falciparum. However, cure can be achieved when artemisone is combined with a single, sub-curative dose of mefloquine, or with a 3-day treatment course of amodiaquine (or clindamycin).
Efficacy of several artemisinin derivatives was examined for the treatment of murine cerebral malaria, CM, ECM [32]. It was shown that artemisone and artemiside (9d, Fig. 3) were more effective in the treatment of ICR and C57BL mice in comparison with dihydroartemisinin or artesunate. In all experiments performed on P. berghei-infected mice, treatment with artemisone led to complete cure (at least parasitaemia was reduced to an undetectable level). The observed recrudescent parasites were successfully eradicated by repeating the treatment with artemisone without selecting for parasite resistance. In addition, it was shown that complete cure of infected mice could be achieved even when treatment with artemisone was commenced at late stages of pathogenesis, 6 days post-infection. These results opened a considerable time window for adequate treatment, since human malaria is diagnosed after clinical symptoms are apparent. Following WHO’s instructions for artemisinin combination therapy (ACT), the efficacy of artemisone–CQ combination was examined and it was shown that this combination was more successful than single therapy of both drugs individually. Combination of these two drugs prevented recrudescence and cured all mice (2 × 5 mg/kg/day artemisone + 15 mg/kg CQ). In this study, artemiside appeared to be even more successful then artemisone, but this derivative has to be submitted to more detailed preclinical toxicological evaluation. However, the preliminary results suggest that artemiside may represent a new option for antimalarial therapy based on artemisinin derivatives [32].
2.1 Possible Mechanisms: Fe(II) Interaction and the Peroxide Bond
In an effort to define more clearly a reasonable mechanism for the action of artemisone and related derivatives, experiments with various Fe(II) salts were performed [33]. It was found that artemisone, unlike other examined aminoartemisinin derivatives 9a, 9b (Fig. 3) and 15–17 (Fig. 4), reacts with Fe(II) salts under aqueous conditions to afford the products 18–20, which are structurally similar to the ones obtained from artemisinin and dihydroartemisinin. The relative ratio of products 18–20 (Scheme 2) depends on the employed salts and solvent mixtures. A reasonable mechanism was proposed for Fe(II)-induced generation of the products, including artemisone → 18, 19 formation via iminium cations. Evidence that a primary C-radical is generated during Fe(II) peroxide scission came from the isolation of adduct 22 (Scheme 2), arising from reaction in the presence of the radical trapper 4-oxo-TEMPO. However, the yield of this product is low (10%) and the authors argued that the role of Fe(II) is during decomposition rather than activation of artemisone [33].
Others have shown that artemisone readily reacts with haem in vitro producing alkylated products [34] very similar to artemisinins [35]. The ability of artemisinin itself to alkylate haem has been confirmed in vitro [36, 37] and in vivo [38]. These data indicate that Fe(II) species are able to activate artemisinins, including artemisone, in their antimalarial action. However, it should be noted that the conditions used to determine alkylation by artemisinins have been questioned, in particular the use of dimethyl sulphoxide that produces a reducing environment [39, 40], and, currently, there is no evidence that artemisone alkylates haem in vivo. In addition, the theory of Fe(II)-initiated activation of artemisinins could not explain the pronounced antimalarial activity of 5-nor-4,5-seco-artemisinin 23 [41–43], which is clearly less capable of forming C radicals upon peroxide bridge cleavage by Fe(II). Another inconsistency in applying the general Fe(II) mechanism (vide supra) to artemisinin and artemisone, and their derivatives, arises from their activities in the presence of desferrioxamine B (DFO). DFO acts as a free radical scavenger (for hydroxyl and peroxyl radicals) and as a Fe(III) chelator and reduces artemisinin inhibition of PfATP6 (a proposed site of action; see below) [44]. In contrast, artemisone, which exhibits approximately the same reactivity with aqueous Fe(II) as artemisinin, retains inhibition potency towards PfATP6 in the presence of DFO [33]. This detail strongly indicates that although the compounds are of similar structure, they might not exert their antimalarial activity by sharing the same mechanism of action.
In order to understand better the manner in which artemisinins exert their antimalarial activity, extensive research was launched bearing in mind that cleavage of the peroxide bridge via an iron-dependent mechanism (as the sole mechanism) does not provide complete answers to observed peroxide drug behaviour. Based on the finding that the in vitro antimalarial activity of artemisinin was significantly increased under a 2% carbon monoxide atmosphere (by 40–50%) and under a 20% oxygen atmosphere (by 20–30%) [45], a detailed study of the interaction of artemisone and related derivatives with various forms of haemoglobin (Hb), haem, as well as an analysis of their antimalarial activity was performed [39]. In contrast to artemisinin, artemisone does not react with Hb–Fe(II) and oxyHb–Fe(II) to produce metHb–Fe(III); in addition, it was shown that both artemisinin and artemisone (and 9a, 9b, 16) are inactive towards Hb–Fe(II) in a 2% carbon monoxide atmosphere. On the other hand, both compounds induced the oxidation of the haemoglobin catabolic product, haem–Fe(II), to produce haem–Fe(III). In addition, on exposure of haem–Fe(II) and Hb–Fe(II) to carbon monoxide, stable complexes were formed, which are also inactive for reactions with peroxide antimalarials. However, in a biologically relevant experiment, both compounds showed increased antimalarial activity against P. falciparum W2 strain under a 2% carbon monoxide atmosphere, while the activity of chloroquine remained unchanged. The authors suggested [39] that peroxide antimalarials behave as reactive oxygen species (ROS), or that they produce ROS via Haber–Weiss chemistry. Furthermore, it was concluded that passivation of haem–Fe(II) by its conversion into the CO complex results in decreased decomposition of artemisinins (artemisone included), thus making them more available for reaction with their actual target. The authors proposed that Fe(II), regardless of its origin (Hb–Fe(II) or haem–Fe(II)), is not the sole initiator of O–O scission, and suggested that another mechanism be sought [39].
2.2 Possible Mechanisms: Primary Targets, Accumulation and Co-Factors
The discovery that artemisinins target SERCA orthologues in P. falciparum (PfATP6) and P. vivax (PvSERCA) [44] shed new light and encouraged research towards the same and other novel targets for peroxide antimalarials. Thus, it was found that artemisone is more potent against plasmodial SERCA orthologues [K i = 1.7 ± 0.6 nM (PfATP6) and K i = 0.072 ± 0.012 nM (PvSERCA)], as compared with values for artemisinin [K i = 169 ± 31 nM (PfATP6) and K i = 7.7 ± 4.9 nM (PvSERCA)] [46].
In order to better understand the mechanism of the accumulation into infected and uninfected erythrocytes, radiolabelled artemisone 9e* was submitted to uptake assays [47]. It was found that artemisone was accumulated in infected erythrocytes at significantly higher levels than in uninfected ones, by a saturable, competitive, time- and temperature-dependent mechanism. Most radioactivity was detected in pellet fractions which predominantly contain proteins suggesting that artemisone is probably associated with proteins [48]. The distribution of artemisone is dependent on the stage of parasite maturation: after incubation with immature parasites, which are highly susceptible to action of artemisinins in vitro, as well as in vivo, most artemisone was found in a Triton-soluble fraction, which contains proteins, DNA and RNA. In mature parasites most artemisone was found in the Triton-insoluble fraction, which predominantly contains haemozoin. This finding suggests that mature infected erythrocytes can act by removing the artemisinins. This was further supported by the observation that mature infected erythrocytes take up artemisone much faster than do the more sensitive ring-stage-infected erythrocytes.
Methylene blue (MB) was the first synthetic drug ever used in humans, and it was Paul Erlich who cured two patients from malaria using MB in 1891 [49]. The discovery that artemisinin and artemether exhibit synergic effects with methylene blue [50], unlike chloroaminoquinolines, initiated systematic examination of reactivity relationships between the drugs with the aim to possibly correlate their mechanism of antimalarial action. Subsequent research by the same group [51] revealed MB as a redox-cycling agent that produces H2O2 at the expense of O2 and of NADPH in each cycle (Fig. 5). Thus, MB consumes NADPH and O2 needed for the pathogen’s metabolism, with probably serious consequences to the NADPH/NADP ratio.
The results of subsequent research revealed that artemisone, other artemisinins [52] and other peroxide antimalarials like ozonides and tetraoxanes [53] are active in the presence of MB-ascorbic acid, MB–N-benzyl-1,4-dihydronicotinamide (BNAH), riboflavin–BNAH and riboflavin–NADPH systems and yield identical products to those that were isolated from the reaction of the same antimalarials with Fe(II). According to this proposal, antimalarial peroxides act as oxidants re-oxidising LMB and FADH2, so contributing to depletion of NADPH (Scheme 3).
The observed results suggest that peroxide antimalarials disrupt a highly sensitive redox balance established in the parasite and thereby cause its death. The results also correlate well with the observed SAR of artemisinins, i.e., artemisinins that exhibited low antimalarial activity, like 9-epiartemisinin [54, 55], also show low reactivity under the applied reaction conditions. In addition, high antimalarial activity of 5-nor-4,5-seco-artemisinin 23 can easily be comprehended using the new mechanism proposal. The proposed explanation involves iron-free reactions; however, Fe(III) rapidly oxidises FADH2, and thus contributes to redox cycling without interfering with artemisinins.
3 ,2,4-Trioxolanes (Ozonides)
1,2,4-Trioxolanes are a very well-known class of organic compounds. They are intermediates in the transformation of olefins into carbonyls during ozonolysis. It was an unexpected and surprising discovery [56] that ozonides are relatively stable and that many of them express excellent activity against malaria parasites, as do the structurally similar 1,2,4-trioxanes.
3.1 Development of 1,2,4-Trioxolanes: OZ209, OZ277 and OZ339
Preparation of 1,2,4-trioxolanes is relatively simple and relies on the Griesbaum co-ozonolysis of suitable methyl oximes and ketones (Scheme 4) [57–59]. This method provides a highly applicable synthetic approach to tetrasubstituted 1,2,4-trioxolanes (ozonides), otherwise accessible only with great difficulty by ozonolysis of the corresponding alkenes, or by other means.
The synthesis of the final OZ antimalarial drug significantly benefits from the stability of the ozonide peroxide bridge to reduction and alkylation conditions, as well as to other standard reaction conditions. This enables transformation of the initial co-ozonolysis products into a vast array of unsymmetrically substituted ozonides (n > 500!) [60]. Usually, the final 1,2,4-trioxolane antimalarials are prepared in 1–4 steps, depending on the modifications required [57–59, 61–63], affording the final products in yields up to 75%. The vast majority of these antimalarials are achiral, which greatly facilitates production in the developmental step. A substantial improvement in drug design in the antimalarial field was the development of the 4-substituted cyclohexyl-adamantyl ozonide (adamantane-2-spiro-3′-1′,2′,4′-trioxaspiro[4.5]decane) chemotype. The advantage of OZ antimalarials is the use of the adamantane moiety that has lipophilic functionality, allowing the opposite part of the molecule to be fine-tuned using a number of polar functional groups, preferably basic in nature [56, 58–62]. Many of the OZ compounds obtained in this way were active in all stages of development of the malaria parasite and are more active than artemether and artesunate, both in vivo and in vitro. All these findings, gathered during much experimentation, contributed to the discovery of amines OZ209 (24 as mesylate, Fig. 6) and OZ277 (25 as tosylate, Fig. 6) as the best drug candidates.
In comparison with other OZ compounds, trioxolanes OZ209 and OZ277 showed superior pharmacokinetic results, such as prolonged half-life and enhanced bioavailability after a single oral dose. Compound OZ209 had somewhat better antimalarial results and a lower recrudescence level. However, OZ277 was chosen as the development candidate, primarily because of its improved toxicological profile and reduced concentrations in brain tissue after oral dosing [56]. For example, 2 h after dosing, both OZ209 and OZ277 were distributed throughout the liver, kidney, lung and heart, while after 18 h, OZ277 was detected only in the lungs and in several-fold lower concentrations than OZ209.
Unlike OZ209, which was quantified in brain tissue after both 2 h and 18 h, trioxolane OZ277 could not be quantified in this organ at all. In view of potential neurotoxicity issues, these findings were taken as a considerable advantage of OZ277 over OZ209. Trioxolane OZ277 appeared quite stable to metabolic transformation (t ½ = 17 h, p.o. in healthy rats) [56]. The metabolic profile of OZ277 was studied with human liver microsomes and only two, monohydroxylated derivatives at the adamantane angular positions (32 and 33, Fig. 7), were identified as major metabolites, thus confirming the stability of the trioxolane moiety to metabolic transformation. Interestingly, both metabolites were inactive against the P. falciparum K1 strain (IC50 > 100 ng/ml), thus demonstrating the indispensability of the unsubstituted spiro-adamantane moiety to the antimalarial activity of OZ277 (IC50 (K1) = 1.0 ng/ml) [64]. Unlike the artemisone products (Scheme 1), OZ metabolic derivatives 32 and 33 very probably lower the overall OZ277 antimalarial activity. The other derivatives 26–29 (Fig. 5) afforded further insight into SAR in the context of the physico-chemical, biopharmaceutical and toxicological profiles of trioxolanes [61].
Recently, the same authors revealed data for a series of OZ compounds with weak base functional groups, which were responsible for a high antimalarial efficacy in P. berghei-infected mice [65]. Their antimalarial efficacy and ADME profiles are equal or superior to OZ277. One of the most promising is OZ339 (as tosylate salt). The two trioxolanes, OZ339 and OZ277 are evaluated in Table 1, with artesunate added for comparison. Despite the obvious difference in in vitro activity, both ozonides eradicate parasitaemia below the detectable level 1 day after administration (99.9%, 1 ×10 mg/kg, and 3 × 3 mg/kg). The drug candidate OZ277 is a powerful fast-acting antimalarial with a 67% cure record at a 3 × 10 mg/kg dosage (mice) [56]. However, at a 3 × 3 mg/kg dosage, the same compound cured no mice, while trioxolane OZ339 cured 3/5 mice with an excellent survival time of 27 days (OZ277 had a 2.4 times lower survival time). These good pharmacokinetic characteristics are additionally enhanced by the favourable bioavailability data for OZ339 (78%, Table 1). In all experiments, artesunate showed inferior activity. Inhibition assays revealed that OZ339, like OZ277, did not inhibit CYP3A4, CYP2C9 and 2D6CYP450 at concentrations up to 50 μM. Finally, preliminary toxicological experiments indicated that OZ339 was minimally toxic (liver) and, similar to OZ277, demonstrated no detectable signs of neurotoxicity.
As mentioned above, the tolerance of the 1,2,4-trioxolane moiety to diverse reaction conditions [57] and resistance to metabolic transformation [64] enabled the synthesis of a significant number of derivatives and many of them showed very good antimalarial activity, e.g., derivatives 34–38 (Fig. 8) [66], and derivatives which contain aliphatic and aromatic amino functional groups or azole heterocycles as substituents (39–45) (Fig. 8) [62].
The lack of activity of trioxolane 46 [62], and the isolation of inactive hydroxylated OZ277 metabolites [64], point to the essential contribution of an unsubstituted spiro-adamantane system to the antimalarial properties of this class of compounds.
Many of the examined derivatives exhibited excellent in vitro results, but failed during in vivo tests, toxicity trials or metabolic stability and bioavailability tests. More lipophilic trioxolanes tend to have better oral activities and are metabolically less stable than their more polar counterparts. Such behaviour is consistent with results obtained for other classes of synthetic peroxides. Trioxolanes with a wide range of neutral and basic groups had good antimalarial profiles, unlike derivatives with acidic groups. Based on the collected extensive screening results, the authors concluded that in vitro activities of 1,2,4-trioxolanes are not (always) a reliable predictor of in vivo potency [66]. Rather, their experiments in P. berghei-infected mice confirmed that in vivo results were essential for compound differentiation and selection for further metabolic and pharmacokinetic profiling [65].
Trioxolane OZ277 alkylates haem (Fig. 9) [67], and its in vitro activity against P. falciparum is antagonised by DFO [68]. In vitro, artesunate and OZ277 act antagonistically against P. falciparum. These findings, together with only weak interaction with the proposed artemisinin target PfATP6 [44], unlike artemisone [33], suggest that interaction with food vacuole-generated haem is probably how trioxolanes are activated. Further support can be found in the fact that the stereochemistry of a given compound has little effect on the in vitro potency of trioxolane antimalarials, thereby strongly pointing to the interaction of an antimalarial peroxide (chiral or achiral) with an achiral target (haem). The selectivity of trioxolanes towards infected and not-healthy erythrocytes may be explained based on their reactivity towards free haem and stability in the presence of oxy- and deoxyHb [69].
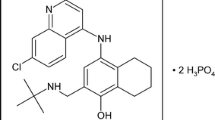
Based on the concept that compounds with two integrated pharmacophores might have enhanced activity [70], the chimaeric trioxolane OZ258 was prepared (Fig. 10) [58, 59]. Although it is very active in vitro against the K1 and NF54 strains of P. falciparum and in vivo against the ANKA strain of P. berghei, OZ258 did not achieve the synergic effect of two pharmacophores, especially when compared with trioxolanes 39 and 43. The same holds for other chloroaminoquinoline and acridine chimaeras [71].
Very often, promising peroxide drugs eradicate parasitaemia quickly, which is crucial for rapid treatment of life-threatening cerebral malaria, and this property is inherently protective against the development of resistance. Since the drugs are typically administered for only a few days and they have short half-lives, the recrudescence of malaria parasites occurs frequently (artemisone cf. [24, 32]; OZ277 cf. [58]). In an attempt to overcome this problem, artemisinin-based combination therapies (ACTs) are recommended (as indicated for artemisone, see above) by the WHO. The WHO currently distributes, under a no-loss and no-profit agreement with Novartis, the fixed-dose ACT drug Coartem® (artemether 20 mg/lumefantrine 120 mg) [72]. The drug has been recently approved by the FDA for the treatment of acute, uncomplicated malaria infections [73]. Although each ACT is specific [73, 74], the following concept can be applied to all: antimalarial peroxides eliminate most of the infection and the remaining parasites are then exposed to high concentrations of the slow-acting partner drugs; because of the rapid reduction in parasites, the selective pressure for the emergence of mutant parasites is greatly reduced. In accord, OZ277 (RBX-11160) entered Phase III clinical trials in combination with piperaquine (arterolane maleate + piperaquine phosphate) [75].
3.2 The Second Generation of 1,2,4-Trioxolane Drug Candidates: OZ439
In Phase I clinical trials, the half-life of OZ277 in healthy volunteers was only about two- to threefold longer than that of dihydroartemisinin. OZ277’s possible first-generation ozonide alternative, OZ339, only has a slightly higher t½ value (Table 1); so the search for an ozonide with significantly increased half-life continued.
As a result, screening of the second generation of ozonide antimalarials has been completed, recently [76]. Of the several very active OZ compounds of undisclosed structure it appears that the most promising antimalarial candidate is OZ439 (Table 2) [76]. Initial results indicate that this compound provides single-dose oral cure in a murine malaria model at 20 mg/kg, a situation not known for any of the peroxide antimalarials except for artelininc acid at >7 times higher dose [76]. The second-generation ozonide OZ439 completed Phase I studies and is currently undergoing Phase IIa clinical trials. In accord with other ozonide antimalarials, OZ439 is considered to be an Fe(II)-initiated pro-drug. However, it is >50-fold more stable to Fe(II)-mediated degradation compared with OZ277 [76]. Consistent with proposed Fe(II) degradation of ozonides [67] is the significantly enhanced stability (15–20 times) of OZ439 over OZ277 in healthy and infected human and rat blood. This prolonged blood stability and improved pharmacokinetic characteristics (Table 2) led to the positioning of OZ439 as the current major OZ drug candidate – with respect to post-infection cure (3 × 5 mg/kg/day and 20 mg/kg single dose), and exclusive prophylactic characteristics (Table 2). The absence of metabolic products significantly contributes to overall activity (prophylactic and post-infection) of OZ439 relative to other peroxide antimalarial drugs [76].
To conclude, as a consequence of intensive and comprehensive research, efficient antimalarial drug candidates of different chemotype have been devised: artemisone and 1,2,4-trioxolane OZ277. They are nontoxic, effective at small doses and very probably inexpensive to produceFootnote 2 [77]. The same may hold for a prospective backup candidate artemiside and the newest breakthrough drug candidate OZ439. It would be of benefit if their combination partner would cure malaria through different mechanisms, since resistance is then less likely to occur.
Notes
- 1.
However, dihydroartemisinin was detected in plasma during assessment of the safety of artemisone [27]. The concentrations were low, with geometric mean C max values of 10 ng/ml after an 80 mg dose.
- 2.
The annual demand for artemisinin as a starting material for transformation into semi-synthetic products amounts to ca. 114 tonnes for Coartem® production only. Since synthesis of artemisinin is uneconomical currently, Novartis initiated an increase of the agricultural cultivation of Artemisia annua in Kenya, Tanzania and Uganda and extraction of artemisinin therefrom, in addition to Chinese supplies of artemisinin.
References
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, Lwin KM, Ariey F, Hanpithakpong W, Lee SJ et al (2009) Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med 361:455–467
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM (2008) Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med 359:2619–2620
Jefford CW (2007) New developments in synthetic peroxidic drugs as artemisinin mimics. Drug Discov Today 12:487–495
Lin AJ, Miller RE (1995) Antimalarial activity of new dihydroartemisinin derivatives. 6. alpha-Alkylbenzylic ethers. J Med Chem 38:764–770
Lin AJ, Lee M, Klayman DL (1989) Antimalarial activity of new water-soluble dihydroartemisinin derivatives. 2. Stereospecificity of the ether side chain. J Med Chem 32:1249–1252
Fishwick J, McLean WG, Edwards G, Ward SA (1995) The toxicity of artemisinin and related compounds on neuronal and glial cells in culture. Chem Biol Interact 96:263–271
Wesche DL, DeCoster MA, Tortella FC, Brewer TG (1994) Neurotoxicity of artemisinin analogs in vitro. Antimicrob Agents Chemother 38:1813–1819
Nontprasert A, Pukrittayakamee S, Prakongpan S, Supanaranond W, Looareesuwan S, White NJ (2002) Assessment of the neurotoxicity of oral dihydroartemisinin in mice. Trans R Soc Trop Med Hyg 96:99–101
Davis TM, Binh TQ, Ilett KF, Batty KT, Phuong HL, Chiswell GM, Phuong VD, Agus C (2003) Penetration of dihydroartemisinin into cerebrospinal fluid after administration of intravenous artesunate in severe falciparum malaria. Antimicrob Agents Chemother 47:368–370
Li Q, Weina PJ (2010) Severe embryotoxicity of artemisinin derivatives in experimental animals, but possibly safe in pregnant women. Molecules 15:40–57
Avery MA, Alvim-Gaston M, Vroman JA, Wu B, Ager A, Peters W, Robinson BL, Charman W (2002) Structure-activity relationships of the antimalarial agent artemisinin. 7. Direct modification of (+)-artemisinin and in vivo antimalarial screening of new, potential preclinical antimalarial candidates. J Med Chem 45:4321–4335
Chadwick J, Mercer AE, Park BK, Cosstick R, O’Neill PM (2009) Synthesis and biological evaluation of extraordinarily potent C-10 carba artemisinin dimers against P. falciparum malaria parasites and HL-60 cancer cells. Bioorg Med Chem 17:1325–1338
Pacorel B, Leung SC, Stachulski AV, Davies J, Vivas L, Lander H, Ward SA, Kaiser M, Brun R, O’Neill PM (2010) Modular synthesis and in vitro and in vivo antimalarial assessment of C-10 pyrrole mannich base derivatives of artemisinin. J Med Chem 53:633–640
Posner GH, Parker MH, Northrop J, Elias JS, Ploypradith P, Xie S, Shapiro TA (1999) Orally active, hydrolytically stable, semisynthetic, antimalarial trioxanes in the artemisinin family. J Med Chem 42:300–304
Posner GH, Ploypradith P, Parker MH, O’Dowd H, Woo SH, Northrop J, Krasavin M, Dolan P, Kensler TW, Xie S et al (1999) Antimalarial, antiproliferative, and antitumor activities of artemisinin-derived, chemically robust, trioxane dimers. J Med Chem 42:4275–4280
Jefford CW (2001) Why artemisinin and certain synthetic peroxides are potent antimalarials. Implications for the mode of action. Curr Med Chem 8:1803–1826
McCullough KJ, Nojima M (2001) Recent advances in the chemistry of cyclic peroxides. Curr Org Chem 5:601–636
O’Neill PM, Amewu RK, Nixon GL, Bousejra ElGarah F, Mungthin M, Chadwick J, Shone AE, Vivas L, Lander H, Barton V et al (2010) Identification of a 1,2,4,5-tetraoxane antimalarial drug-development candidate (RKA 182) with superior properties to the semisynthetic artemisinins. Angew Chem Int Ed Engl 49:5693–5697
Opsenica I, Opsenica D, Smith KS, Milhous WK, Šolaja BA (2008) Chemical stability of the peroxide bond enables diversified synthesis of potent tetraoxane antimalarials. J Med Chem 51:2261–2266
Šolaja B, Opsenica DM, Pocsfalvi G, Milhous WK, Kyle DE (2005) Mixed steroidal 1,2,4,5-tetraoxane compounds and methods of making and using thereof. US Patent 6906098 B2
Haynes RK, Fugmann B, Stetter J, Rieckmann K, Heilmann HD, Chan HW, Cheung MK, Lam WL, Wong HN, Croft SL et al (2006) Artemisone–a highly active antimalarial drug of the artemisinin class. Angew Chem Int Ed Engl 45:2082–2088
Haynes RK, Ho WY, Chan HW, Fugmann B, Stetter J, Croft SL, Vivas L, Peters W, Robinson BL (2004) Highly antimalaria-active artemisinin derivatives: biological activity does not correlate with chemical reactivity. Angew Chem Int Ed Engl 43:1381–1385
Bhattacharjee AK, Karle JM (1999) Stereoelectronic properties of antimalarial artemisinin analogues in relation to neurotoxicity. Chem Res Toxicol 12:422–428
http://www.public-health.tu-dresden.de/dotnetnuke3/Portals/0/VKliPhaDresden%202005.pdf. Accessed 04 Jan 2011
Vivas L, Rattray L, Stewart LB, Robinson BL, Fugmann B, Haynes RK, Peters W, Croft SL (2007) Antimalarial efficacy and drug interactions of the novel semi-synthetic endoperoxide artemisone in vitro and in vivo. J Antimicrob Chemother 59:658–665
Jambou R, Legrand E, Niang M, Khim N, Lim P, Volney B, Ekala MT, Bouchier C, Esterre P, Fandeur T et al (2005) Resistance of Plasmodium falciparum field isolates to in-vitro artemether and point mutations of the SERCA-type PfATPase6. Lancet 366:1960–1963
Ashton M, Hai TN, Sy ND, Huong DX, Van Huong N, Nieu NT, Cong LD (1998) Artemisinin pharmacokinetics is time-dependent during repeated oral administration in healthy male adults. Drug Metab Dispos 26:25–27
Svensson US, Ashton M (1999) Identification of the human cytochrome P450 enzymes involved in the in vitro metabolism of artemisinin. Br J Clin Pharmacol 48:528–535
Nagelschmitz J, Voith B, Wensing G, Roemer A, Fugmann B, Haynes RK, Kotecka BM, Rieckmann KH, Edstein MD (2008) First assessment in humans of the safety, tolerability, pharmacokinetics, and ex vivo pharmacodynamic antimalarial activity of the new artemisinin derivative artemisone. Antimicrob Agents Chemother 52:3085–3091
Brewer TG, Grate SJ, Peggins JO, Weina PJ, Petras JM, Levine BS, Heiffer MH, Schuster BG (1994) Fatal neurotoxicity of arteether and artemether. Am J Trop Med Hyg 51:251–259
Obaldia N 3rd, Kotecka BM, Edstein MD, Haynes RK, Fugmann B, Kyle DE, Rieckmann KH (2009) Evaluation of artemisone combinations in Aotus monkeys infected with Plasmodium falciparum. Antimicrob Agents Chemother 53:3592–3594
Waknine-Grinberg JH, Hunt N, Bentura-Marciano A, McQuillan JA, Chan HW, Chan WC, Barenholz Y, Haynes RK, Golenser J (2010) Artemisone effective against murine cerebral malaria. Malar J 9:227
Haynes RK, Chan WC, Lung CM, Uhlemann AC, Eckstein U, Taramelli D, Parapini S, Monti D, Krishna S (2007) The Fe2+-mediated decomposition, PfATP6 binding, and antimalarial activities of artemisone and other artemisinins: the unlikelihood of C-centered radicals as bioactive intermediates. ChemMedChem 2:1480–1497
Bousejra-El Garah F, Meunier B, Robert A (2008) The antimalarial artemisone is an efficient heme alkylating agent. Eur J Inorg Chem 2008:2133–2135
Laurent SA, Loup C, Mourgues S, Robert A, Meunier B (2005) Heme alkylation by artesunic acid and trioxaquine DU1301, two antimalarial trioxanes. ChemBioChem 6:653–658
Robert A, Cazelles J, Meunier B (2001) Characterization of the alkylation product of heme by the antimalarial drug artemisinin. Angew Chem Int Ed Engl 40:1954–1957
Robert A, Coppel Y, Meunier B (2002) Alkylation of heme by the antimalarial drug artemisinin. Chem Commun 2002:414–415
Robert A, Benoit-Vical F, Claparols C, Meunier B (2005) The antimalarial drug artemisinin alkylates heme in infected mice. Proc Natl Acad Sci USA 102:13676–13680
Coghi P, Basilico N, Taramelli D, Chan WC, Haynes RK, Monti D (2009) Interaction of artemisinins with oxyhemoglobin Hb-FeII, Hb-FeII, carboxyHb-FeII, heme-FeII, and carboxyheme FeII: significance for mode of action and implications for therapy of cerebral malaria. ChemMedChem 4:2045–2053
Haynes RK (2005) Reply to comments on “Highly antimalaria-active artemisinin derivatives: biological activity does not correlate with chemical reactivity”. Angew Chem Int Ed Engl 44:2064–2065
Avery MA, Chong WKM, Bupp JE (1990) Tricyclic analogues of artemisinin: synthesis and antimalarial activity of (+)-4,5=secoartemisinin and (−)-5-nor-4,5-secoartemisinin. J Chem Soc Chem Commun 1487–1489
Avery MA, Gao F, Chong WKM, Hendrickson TF, Inman WD, Crews P (1994) Synthesis, conformational analysis, and antimalarial activity of tricyclic analogs of artemisinin. Tetrahedron 50:952–957
Haynes RK, Vonwiller SC (1996) The behaviour of qinghaosu (artemisinin) in the presence of non-heme iron(II) and (III). Tetrahedron Lett 37:257–260
Eckstein-Ludwig U, Webb RJ, Van Goethem ID, East JM, Lee AG, Kimura M, O’Neill PM, Bray PG, Ward SA, Krishna S (2003) Artemisinins target the SERCA of Plasmodium falciparum. Nature 424:957–961
Parapini S, Basilico N, Mondani M, Olliaro P, Taramelli D, Monti D (2004) Evidence that haem iron in the malaria parasite is not needed for the antimalarial effects of artemisinin. FEBS Lett 575:91–94
Uhlemann AC, Cameron A, Eckstein-Ludwig U, Fischbarg J, Iserovich P, Zuniga FA, East M, Lee A, Brady L, Haynes RK et al (2005) A single amino acid residue can determine the sensitivity of SERCAs to artemisinins. Nat Struct Mol Biol 12:628–629
Pooley S, Fatih FA, Krishna S, Gerisch M, Haynes RK, Wong HN, Staines HM (2011) Artemisone uptake in Plasmodium falciparum-infected erythrocytes. Antimicrob Agents Chemother 55:550–556
Yang YZ, Little B, Meshnick SR (1994) Alkylation of proteins by artemisinin. Effects of heme, pH, and drug structure. Biochem Pharmacol 48:569–573
Rosenthal PJ (2001) Antimalarial chemotherapy: mechanisms of action, resistance, and new directions in drug discovery. Humana, Totowa, NJ
Akoachere M, Buchholz K, Fischer E, Burhenne J, Haefeli WE, Schirmer RH, Becker K (2005) In vitro assessment of methylene blue on chloroquine-sensitive and -resistant Plasmodium falciparum strains reveals synergistic action with artemisinins. Antimicrob Agents Chemother 49:4592–4597
Buchholz K, Schirmer RH, Eubel JK, Akoachere MB, Dandekar T, Becker K, Gromer S (2008) Interactions of methylene blue with human disulfide reductases and their orthologues from Plasmodium falciparum. Antimicrob Agents Chemother 52:183–191
Haynes RK, Chan WC, Wong HN, Li KY, Wu WK, Fan KM, Sung HH, Williams ID, Prosperi D, Melato S et al (2010) Facile oxidation of leucomethylene blue and dihydroflavins by artemisinins: relationship with flavoenzyme function and antimalarial mechanism of action. ChemMedChem 5:1282–1299
Haynes RK, Cheu KW, Tang MM, Chen MJ, Guo ZF, Guo ZH, Coghi P, Monti D (2011) Reactions of antimalarial peroxides with each of leucomethylene blue and dihydroflavins: flavin reductase and the cofactor model exemplified. ChemMedChem 6:279–291
Avery MA, Gao F, Chong WK, Mehrotra S, Milhous WK (1993) Structure-activity relationships of the antimalarial agent artemisinin. 1. Synthesis and comparative molecular field analysis of C-9 analogs of artemisinin and 10-deoxoartemisinin. J Med Chem 36:4264–4275
Jefford CW, Burger U, Millasson-Schmidt P, Bernardinelli G, Robinson BL, Peters W (2000) Epiartemisinin, a remarkably poor antimalarial: implications for the mode of action. Helv Chim Acta 83:1239–1246
Vennerstrom JL, Arbe-Barnes S, Brun R, Charman SA, Chiu FC, Chollet J, Dong Y, Dorn A, Hunziker D, Matile H et al (2004) Identification of an antimalarial synthetic trioxolane drug development candidate. Nature 430:900–904
Tang Y, Dong Y, Karle JM, DiTusa CA, Vennerstrom JL (2004) Synthesis of tetrasubstituted ozonides by the Griesbaum coozonolysis reaction: diastereoselectivity and functional group transformations by post-ozonolysis reactions. J Org Chem 69:6470–6473
Vennerstrom JL, Dong Y, Chollet J, Matile H (2002) Spiro and dispiro 1,2,4-trioxolane antimalarials. US Patent 6486199
Vennerstrom JL, Tang Y, Dong Y, Chollet J, Matile H, Padmanilayam M, Charman WN (2004) Spiro and dispiro 1,2,4-trioxolane antimalarials. US Patent 6825230
Vennerstrom JL, Dong Y, Charman SA, Wittlin S, Chollet J, Wang X, Sriraghavan K, Zhou L, Matile H, Charman WN (2008) Spiro and dispiro 1,2,4-trioxolane antimalarials. US Patent 2008/0125441 A1
Dong Y, Chollet J, Matile H, Charman SA, Chiu FC, Charman WN, Scorneaux B, Urwyler H, Santo Tomas J, Scheurer C et al (2005) Spiro and dispiro-1,2,4-trioxolanes as antimalarial peroxides: charting a workable structure-activity relationship using simple prototypes. J Med Chem 48:4953–4961
Tang Y, Dong Y, Wittlin S, Charman SA, Chollet J, Chiu FC, Charman WN, Matile H, Urwyler H, Dorn A et al (2007) Weak base dispiro-1,2,4-trioxolanes: potent antimalarial ozonides. Bioorg Med Chem Lett 17:1260–1265
Vennerstrom JL, Dong Y, Chollet J, Matile H, Wang X, Sriraghavan K, Charman WN (2008) Spiro and dispiro 1,2,4-trioxolane antimalarials. US Patent 7371778
Zhou L, Alker A, Ruf A, Wang X, Chiu FC, Morizzi J, Charman SA, Charman WN, Scheurer C, Wittlin S et al (2008) Characterization of the two major CYP450 metabolites of ozonide (1,2,4-trioxolane) OZ277. Bioorg Med Chem Lett 18:1555–1558
Dong Y, Wittlin S, Sriraghavan K, Chollet J, Charman SA, Charman WN, Scheurer C, Urwyler H, Santo Tomas J, Snyder C et al (2010) The structure-activity relationship of the antimalarial ozonide arterolane (OZ277). J Med Chem 53:481–491
Dong Y, Tang Y, Chollet J, Matile H, Wittlin S, Charman SA, Charman WN, Tomas JS, Scheurer C, Snyder C et al (2006) Effect of functional group polarity on the antimalarial activity of spiro and dispiro-1,2,4-trioxolanes. Bioorg Med Chem 14:6368–6382
Creek DJ, Charman WN, Chiu FC, Prankerd RJ, Dong Y, Vennerstrom JL, Charman SA (2008) Relationship between antimalarial activity and heme alkylation for spiro- and dispiro-1,2,4-trioxolane antimalarials. Antimicrob Agents Chemother 52:1291–1296
Uhlemann AC, Wittlin S, Matile H, Bustamante LY, Krishna S (2007) Mechanism of antimalarial action of the synthetic trioxolane RBX11160 (OZ277). Antimicrob Agents Chemother 51:667–672
Creek DJ, Ryan E, Charman WN, Chiu FC, Prankerd RJ, Vennerstrom JL, Charman SA (2009) Stability of peroxide antimalarials in the presence of human hemoglobin. Antimicrob Agents Chemother 53:3496–3500
O’Neill PM, Posner GH (2004) A medicinal chemistry perspective on artemisinin and related endoperoxides. J Med Chem 47:2945–2964
Araujo NC, Barton V, Jones M, Stocks PA, Ward SA, Davies J, Bray PG, Shone AE, Cristiano ML, O’Neill PM (2009) Semi-synthetic and synthetic 1,2,4-trioxaquines and 1,2,4-trioxolaquines: synthesis, preliminary SAR and comparison with acridine endoperoxide conjugates. Bioorg Med Chem Lett 19:2038–2043
WHO. http://www.who.int/malaria/publications/atoz/coa_website5.pdf. Accessed 19 Dec 2010
FDA. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149559.htm. Accessed 19 Dec 2010
MMV. http://www.mmv.org/research-development/project-portfolio/phase-iia. Accessed 20 Dec 2010
Ranbaxy. http://www.ranbaxy.com/socialresposbility/mm.aspx. Accessed 20 Dec 2010
Charman SA, Arbe-Barnes S, Bathurst IC, Brun R, Campbell M, Charman WN, Chiu FC, Chollet J, Craft JC, Creek DJ et al (2011) Synthetic ozonide drug candidate OZ439 offers new hope for a single-dose cure of uncomplicated malaria. Proc Natl Acad Sci USA 108:4400–4405
http://www.corporatecitizenship.novartis.com/patients/access-medicines/intellectual-property/biodiversity.shtml. Accessed 05 Jan 2011
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Basel AG
About this chapter
Cite this chapter
Opsenica, D.M., Šolaja, B.A. (2011). Second-Generation Peroxides: The OZs and Artemisone. In: Staines, H., Krishna, S. (eds) Treatment and Prevention of Malaria. Milestones in Drug Therapy. Springer, Basel. https://doi.org/10.1007/978-3-0346-0480-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-0346-0480-2_10
Published:
Publisher Name: Springer, Basel
Print ISBN: 978-3-0346-0479-6
Online ISBN: 978-3-0346-0480-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)