Abstract
The transition to telemedicine pandemic has expedited recently due to the COVID-19 pandemic, as a precautionary measure to reduce face-to-face interaction with healthcare professionals. The aim of this study is to employ Andersen's Model of Healthcare Utilization in order to identify the key factors that are associated with the utilization of telemedicine during the COVID-19 pandemic. This study aims to attain two main objectives, which are: firstly, to discern the advantages and barriers of adopting telemedicine; and secondly, to appraise the influence of socio-economic and socio-demographic factors in relation to the regular use of telemedicine by patients. The independent variables are categorized as the following: predisposing factors, enabling factors and need for care factors. From January to February in 2023, a cross-sectional survey was conducted. The total number of the online survey responses were 707, out of these, 171 (24.2%) reported to be user of telemedicine. To establish the correlation between telemedicine utilization and other independent variables a binary logistic regression model was used. The results show that there is a significant link between age, education, profession, region, and telemedicine utilization. Being a female, or aged between 30 and 50, having chronic diseases and using both virtual consultation and in-person visits with the doctors was associated with higher odds of telemedicine use. This study can potentially aid insurance companies in enhancing their knowledge and training pertaining to telemedicine. Through collaboration with policy makers, it is advisable to integrate education regarding insurance into the overall education program. Further research is needed to identify how telemedicine may reduce costs, as well as how optimal protocols can be constructed to enhance reimbursement mechanisms associated with said service.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The transition to telemedicine pandemic has expedited recently due to the COVID-19 pandemic, as a precautionary measure to reduce face-to-face interaction with healthcare professionals. Telemedicine is defined as “the use of advanced telecommunications technologies to exchange health information and provide healthcare services across geographic, time, social and cultural barriers [1]. In March 2020, the pandemic found our health system unprepared for such a large number of patients infected by Covid-19, and this forced a large part of Albanians to turn to private clinics and hospitals, paying staggering amounts to save their lives. Telemedicine had not yet been implemented in Albania before the pandemic, but was offered as a service in October 2021 by a private health insurance (Sigal). Telemedicine consultations can assist in upholding the continuity of healthcare for the wider community, particularly in situations where traditional face-to-face consultations are not practically feasible. Concurrently, telemedicine presents a potential solution to alleviate administrative workload by affording patients and healthcare providers the ability to arrange consultations and engage in virtual communication at their own discretion [2]. The availability of telemedicine services is likely to incentivize individuals to seek medical assessment in a timelier manner during the early stages of an illness, thus avoiding the consequences to their physical well-being and financial stability [3]. Virtual care, used in the form of phone calls, video meetings or remote monitoring of the patient can be a good substitute for physical visits to the doctor. This can significantly reduce health care costs especially for that population that has chronic diseases or who live in rural areas where the distance and time to go to the doctor is far [4]. The aim of this study is to employ Andersen's Model of Healthcare Utilization in order to identify the key factors that are associated with the utilization of telemedicine during the COVID-19 pandemic. This study aims to attain two main objectives, which are: firstly, to discern the advantages and barriers of adopting telemedicine; and secondly, to appraise the influence of socio-economic and socio-demographic factors in relation to the regular use of telemedicine by patients. This paper includes 6 sections. It starts with an introductory section providing a comprehensive definition of telemedicine, along with a discussion of the benefits it offers. The following section, the literature review focuses on the latest research endeavors related to telemedicine. Subsequently, the methodology section entails an explanation of the theoretical framework and the research methods that have been employed in this study. According to the findings derived from the binary regression analysis are included in results. In the discussion section, the outcomes of this study are juxtaposed with those of other researchers. The final section of this paper provides a comprehensive summary of the results obtained and their corresponding impact.
2 Literature Review
According to a global survey conducted in May 2021, a substantial 73% of participants reported that telemedicine experienced the largest growth during the pandemic [5]. Multiple studies have reported a notable surge in telemedicine utilization amidst the COVID-19 pandemic across the globe, including Canada and the United States. In Sweden, the employment of telemedicine technologies to establish communication between primary care physicians and their patients was reported to be as high as 95%. Similarly, in Switzerland, 81% of physicians employed comparable means, while in the United States, 79% of medical practitioners were observed to provide such service [6]. In their investigation, [7] found that several factors such as rural areas, patient demographics, and reimbursement regulations have significant impacts on health centers’ choices with regard to the implementation of telemedicine. Cost, reimbursement, and technical issues were described as major barriers. According to the study [8] telemedicine use during the outbreak reaching 21.1% as compared to the pre-pandemic rate of 4.6%.The prominent determinants of telemedicine adoption were need-based circumstances and digital accessibility, rather than demographic factors such as age and income. Moreover, [9] found that telemedicine use increased with age, education level, and with family incomes and was highest in large metropolitan areas. The findings from the study [10] indicate that telemedicine implementation has the potential to augment the efficacy of healthcare provisions through the expedience of both time and cost savings associated with travel. Moreover, it has the potential to reduce the encompassing expenses of treatment, augment patients’ standard of living, and expand access of vital healthcare provisions. Previous research has indicated that the only enabling factor linked to the application of telemedicine is the presence of multiple consistent healthcare providers. This observation may suggest that individuals in greatest need of medical attention are more receptive to novel modes of healthcare delivery. Lower educational attainment was less likely to report the utilization. The research findings in study [11] indicated that approximately fifty-eight percent of respondents agreed or strongly agreed that telemedicine will become an integrated aspect of routine clinical practice. Moreover, the participants of this study identified the need for additional education and training with respect to telemedicine, particularly in the context of consulting with clients. Rural, academic status, were not significantly associated with odds in the results of [12]. In addition, the results of study [13] shows that gender, race, age, and traveling distance were not associated with low telemedicine use. Furthermore, in the study of [14] older age was associated with a significantly lower odds and female gender was related with a higher odds of having a telemedicine experience.
3 Methodology
3.1 Theoretical Framework
The Andersen model of utilization of healthcare is used in this study as a conceptual framework to investigate variables related to the use of telemedicine in Albania during the COVID-19 pandemic [15]. Andersen's conceptual framework posits that the utilization of health services is determined by an individual's predisposing, enabling, and need-based factors (PEN) [16]. Many of the previous studies [15,16,17,18,19] describe the PEN as [17].
-
1.
Predisposing variables including socio-demographic factors (age, gender, etc.) [18]
-
2.
Enabling variables including socio-economic factors (income, region, waiting time)
-
3.
The level of disease experienced and the reasons for seeking medical attention are referred to as the need for care [19]. The aim of this study is to identify factors associated with telemedicine using Andersen’s Model of Healthcare Utilization.
Therefore, we hypothesize existence of predisposing, enabling, and need for care factors.
-
H1: People who are older, female, with higher levels of education or been infected with Covid-19 were more likely to use telemedicine.
-
H2: People who lived in urban area, in Center of Albania, who are employed, or with high income were more likely to use telemedicine.
-
H3: People with chronic diseases, or unhealthy, or who used virtual consultation during pandemic were more likely to use telemedicine.
3.2 Methods
From January to February in 2023, a cross-sectional survey was conducted. The study's participation criteria included being an adult (older than 18) who is a user or non-user of telemedicine in Albania. This survey was conducted in connection to telemedicine and in particular to the “Teleshëndet” application. This application is part of telemedicine and makes it possible to communicate with the doctor online at any time. All data were collected through a self-administered questionnaire using convenience sampling. Out of 1200 distributed questionnaires, only 707 were returned completed. The questionnaire was designed in three parts. The first part includes questions about the frequency (in months) of using Telemedicine, technical problems that they may have occurred during online consultations, etc. The second part consists of questions related to health condition and pandemic Covid-19. The last part included personal socio-demographic and socio-economic characteristics. The present study utilized descriptive statistics for the purpose of providing an overview of the sample characteristics. Furthermore, the study employed binary logistic regression in order to identify the factors that are associated with telemedicine utilization. The outcome variable was whether a respondent used telemedicine or not with (yes or no) being coded as 1 or 0, respectively. The choice of explanatory variables was based on the representation of the three distinct groups of characteristics, namely predisposing, enabling, and need factors. All data analyses in this study were performed using R program.
4 Results
The survey was completed by 707 people. Out of these, 171 (24.2%) reported to be user of telemedicine and 536 (75.8%) non-user of telemedicine. Overall, 58.4% of telemedicine users are women, which is higher percentage than men of 41.6%. Among telemedicine users, 70.7% were married and 57.3% were employed. Surprisingly, about 38% of the respondents who reported to use telemedicine have completed master’s degree or more. Some of the technical problems that the respondents encountered while using telemedicine are: problems with the Internet (32.1%) and difficulty in using the application (15.7%). 95% of respondents of Telemedicine user agree that Telemedicine reduce the time and distance to went to the doctor for consultation and 70% think that the cost of telemedicine is less than visits in person to the doctor. Also, around 24.4% of respondents have been using telemedicine since 6 months, 23.8% since 1 year and 19.4% more than 1 year. Among of telemedicine service offered from insurance, Video and audio consultation was used by majority of the respondents 43.5%, followed by medical recipe 39.1% and check-up (24.2%). About 31% of respondents have used telemedicine once a month, 19% have used it twice a month, 18.4% used 3 times a month and 14.6% more than 3 times per month. Friends and relatives (33.1%) was the main source from which the respondents had received information about telemedicine, followed by media (25.6%) and agents of insurance companies (18.1%).
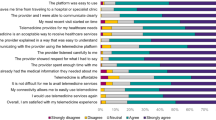
Table 1 shows the results of six items regarding the attitude towards the use of telemedicine. The results indicate that 70% of respondents have declared that virtual consultations with doctor are effective, 77% that would recommend the use of telemedicine to others, 84% have declared that doctors were polite during the online consultations and 74% that the utilize of telemedicine is an successful way to avoid corruption in medicine. Moreover, 52% have declared that replacing the in-person visits with virtual consultations is effective and 71% that the Covid-19 pandemic brought an increase in the use of telemedicine. The reliability of Cronbach’s Alpha coefficient for all items included in the analysis is > 0.82, which is interpreted as good reliability.
Table 2 shows the results of binary logistic regression model. Based on the results of Table 2 we can conclude which of predisposing, enabling and need for care factors are related to the utilization of telemedicine in the binary regression model.
4.1 Predisposing Factors
Utilization of telemedicine was significantly related with a few factors: age (p = 0.000), education (0.043) and profession (0.000) Age group between 30 and 50 was positively related with telemedicine utilization [OR = 1.181, 95% CI: (0.644, 2.163)]. Female were reported to have higher probabilities of using telemedicine than males [OR = 1.272, 95% CI (0.799, 2.025)]. In the binary regression model, Albanians who were infected with Covid-19 [OR = 1.236, 95%CI (0.702, 2.177)] were more likely to use telemedicine services. Respondents who were professor had 3.731 high odds of reporting the utilization of telemedicine. Having a higher education and been married were not associated with telemedicine utilization. These findings partially support hypothesis H1 and are consistent with the results of [4, 14, 20], but inconsistent with results of [9].
4.2 Enabling Factors
Living in urban area (p = 0.038), or in the central of Albania (p = 0.033), or working in the private sector (p = 0.006) were the enabling factor related with the utilization of telemedicine in the binary regression model, in part supporting hypothesis H2. Respondents who lived in an urban region had 1.763 times higher changes of reporting the use of telemedicine compared to those who lived in rural region. Individuals who reported to have spent 100–1000 Euro for check-ups and visits to doctors during the pandemic [OR = 1.015, 95% CI: (0.520, 1.827)] were more likely to use telemedicine service than other who have spent less than 100 Euro, this finding is consistent with the results of [12]. Monthly income and employment status were not associated with telemedicine utilization. These results are consistent with the studies of [7] and [12] and inconsistent with some studies of [4] and [9].
4.3 Need for Care Factors
The only of need factors that is associated with telemedicine utilization is virtual consultations with doctors during pandemic (p < 0.003), partially supporting hypothesis H3. Self-rated health and chronic conditions were not associated with telemedicine utilization. About 45% of respondents have declared that have at least one chronic condition and 36.1% of telemedicine users had virtual consultations with the doctor during Covid-19, followed by in-person (12.2%) and both (22.8%). Respondents who had chronic condition were related with a higher likelihood of telemedicine utilization [OR = 1.060, 95%CI: (0.629–1.710)] compared to those who do not have chronic disease and for respondents who used both virtual and in-person consultation with the doctors during pandemic, the odds increased by 1.283 [CI: (0.688, 2.392)]. The results about chronic disease are consistent with the results of [4].
5 Discussion
Contrary to what we predicted, some of the factors were not significant in the binary regression model analyzing the use of telemedicine. Older age have very lower odds of telemedicine utilization this results are consistent with the studies of [13] and [20] which conclude that difficulties with technologies, smart-phone use, may play a role in this. According to study [21] the expanded utilize of telemedicine services among the younger age group indicate a gap in technical and digital education which should be tended to. In the same line with the results of [14] and [22], adequate technology, lack of training and knowledge among users and internet access are important factors for reducing barriers for telemedicine utilization. In this study, a higher percentage of respondents agreed that telemedicine reduced the time and distance to go to the doctor’s appointment. Prior works of [12] have shown that saving travel time and transportation costs were significant benefits to telemedicine delivery. Moreover, according to the study [2], telemedicine may reduce health care expenditures and improve access to care for underprivileged groups. There are still many debates whether telemedicine should be a replacement or a supplement for face-to-face care. In our study the respondents somewhat agreed to replace the telemedicine with in-person consultations. This results is in accordance with the study of [11] and [23], saying that replacing telemedicine completely with face-to-face care is not reasonable and many clinicians believe that both face-to-face and telemedicine modalities remain essential, and will presumably integrate into a hybrid model subsequent to the COVID-19 era. Including telemedicine services in the health insurance reimbursement system may be a solution to integrate telemedicine into health care system. Future work should examine the role of insurance status in implementing this service and how telemedicine and in-person care may work with each-other. The implementation of telemedicine in the health system will have a very positive impact on the developing countries, where the primary care service is not at the proper level and where corruption in medicine is high, compromising the provision of a quality and equal service for all. In this study, a higher number of respondents agreed that telemedicine can be considered as a way to reduce corruption and out of pocket payment. Moreover, 71% of respondents agree that telemedicine will be the trend of the future in the way medical consultations will be offered. This result is in the same line with the studies of [11] and [24], which maintain that in the upcoming years, telemedicine is anticipated to experience significant growth and could potentially become the new norm in routine practice for Community Health practitioners.
6 Conclusion
Telemedicine can help to bridge gaps in the existing health care system in Albania, by reducing out-of-pocket payments for primary health care. Using Andersen’s Model, our findings show an important association between age, education, profession, region, employment sector (private or public) and telemedicine utilization. Being female, or aged between 30 and 50, or having chronic diseases and using virtual consultation was associated with higher odds of telemedicine use. This study has a few relevant limitations. Firstly, the questionnaire surveys shared online may also be subject to social desirability bias. The sample may not be representative of all populations of Albania because mostly of respondents were from central Albania and who lived in urban areas. Thirdly, this study identifies only some of the factors from Andersen’s framework, but other factors can influence the telemedicine utilization. Despite these restrictions, this study can potentially aid insurance companies in enhancing their knowledge and training pertaining to telemedicine. Through collaboration with policy makers, it is advisable to integrate education regarding insurance into the overall education program. Further research is needed to identify how telemedicine may reduce costs, as well as how optimal protocols can be constructed to enhance reimbursement mechanisms associated with said service.
References
Darkins, A., Cary, M.: Telemedicine and Telehealth, 1st edn. Springer Publishing Company, New York (2000)
Chang, J.E., Lai, A.Y., Gupta, A., Nguyen, A.M., Berry, C.A., Shelley, D.R.: Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post-COVID era. Milbank Quart. 99(2), 340–368 (2021). Author, F.: Article title. Journal 2(5), 99–110 (2016)
Temesgen, Z.M., DeSimone, D.C., Mahmood, M., Libertin, C.R., Varatharaj Palraj, B.R., Berbari, E.F.: Health care after the COVID-19 pandemic and the influence of telemedicine. Mayo Clin. Proceed. 95(9), S66–S68 (2020)
Andersen, J., Felix, H.C., Dejun, S., Selig, J.P., Ratcliff, S., McElfish, P.A.: Factors associated with Arkansans’ first use of telehealth during the COVID-19 pandemic. Int. J. Telemed. Appl. 128, 5953027 (2022)
Research 2 Guidance: Global COVID-19 Survey: One Year into the Pandemic, How has the Digital Health Industry Changed? https://research2guidance.com/product/2021-global-covid-19-survey-one-year-into-the-pandemic-how-has-the-digital-health-industry-changed/. Accessed 20 May 2023
Johnson, C., Dupuis, J.B., Goguen, P., Grenier, G.: Changes to telehealth practices in primary care in New Brunswick (Canada): a comparative study pre and during the COVID-19 pandemic. PLoS ONE 16(11), e0258839 (2021)
Lin, C.C., Dievler, A., Robbins, C., Sripipatana, A., Quinn, M., Nair, S.: Telehealth in health centers: key adoption factors, barriers, and opportunities. Health Aff. 37(12), 1967–1974 (2018)
Choi, N.G., DiNitto, D.M., Marti, C.N., Choi, B.Y.: Telehealth use among older adults during COVID-19: associations with sociodemographic and health characteristics, technology device ownership, and technology learning. J. Appl. Gerontol. 41(3), 600–609 (2022)
Lucas, J.W., Villarroel, M.A.: Telemedicine Use Among Adults: United States, NCHS Data Brief, no 445. National Center for Health Statistics, Hyattsville (2022)
Salsabilla, A., Azzahra, A.B., Syafitri, R.I.P., Supadmi, W., Suwantika, A.A.: Cost-effectiveness of telemedicine in Asia: a scoping review. J. Multidiscip. Healthc. 14, 3587–3596 (2021)
Ervin, K., Weller-Newton, J., Phillips, J.: Primary healthcare clinicians’ positive perceptions of the implementation of telehealth during the COVID-19 pandemic using normalisation process theory. Austr. J. Primary Health 27, 158–162 (2021)
Agrawal, S., Mehta, V., Kumar, N.R.: A study to understand the factors influencing telemedicine utilisation after COVID-19, using the technology acceptance model in Gandhinagar. Int. J. Bus. Anal. Intell. 10(12), 1–9 (2022)
Wei, T.R., Berner, E.S., Qu, H., Agarwal, G.: Factors associated with telemedicine utilization among post-transplant patients at a university kidney and pancreas transplant center. Clin. Transpl. 36(4), e14578 (2022)
Abdool, S., Abdallah, S., Akhlaq, S., Razzak, H.A.: User acceptance level of and attitudes towards telemedicine in the united arab emirates: a quantitative study. Sultan Qaboos Univ. Med. J. 21(2), e203–e209 (2021)
Choi, N.G., DiNitto, D.M., Marti, C.N., Choi, B.Y.: Telehealth use among older adults during COVID-19: associations with sociodemographic and health characteristics, technology device ownership, and technology learning. J. Appl. Gerontol. Off. J. South. Gerontol. Soc. 41(3), 600–609 (2022)
Andersen, R.M., Davidson, P.L.: Improving Access to Care in America: Individual and Contextual Indicators, Changing the US Health Care System: Key Issues in Health Services Policy and Management (2014)
Andersen, R., Newman, J.F.: Societal and individual determinants of medical care utilization in the United States. Milbank Quart 83(4), 428 (2005). https://doi.org/10.1111/j.1468-0009.2005.00428.x
Tomiak, M., Berthelot, J.M., Guimond, E., Mustard, C.A.: Factors associated with nursing-home entry for elders in Manitoba. Canada. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 55(5), 279–287 (2000)
Andersen, R.M.: Revisiting the behavioral model and access to medical care: does it matter? J. Health Soc. Behav. 36(1), 1–10 (1995)
Khatana, S.A.M., Yang, L., Eberly, L.A., Julien, H.M., Adusumalli, S., Groeneveld, P.W.: Predictors of telemedicine use during the COVID-19 pandemic in the United States-an analysis of a national electronic medical record database. PLoS ONE 17(6), e0269535 (2022)
Rahman, S., Amit, S.: Growth in telehealth use in Bangladesh from 2019–2021: a difference-in-differences approach. J. Med. 23, 42–47 (2022)
Sugarman, D., Busch, A., McHugh, R., Bogunovic, O., Trinh, C., Weiss, R., Greenfield, S.: Patients’ perceptions of telehealth services for outpatient treatment of substance use disorders during the COVID-19 pandemic. Am. J. Addict. 30, 13207 (2021). https://doi.org/10.1111/ajad.13207
Ören, M.M., Özgülnar, N., Canbaz, S., Karabey, S., Önal, A.E., Öncül, M.O.: An integrated care model based on hospital and home during the COVID-19 pandemic: telehealth. J. Istanbul Facul. Med. 85(1), 9–14 (2022)
Caron, E.B., Kipp, E.C., Costello, A.H., Bernard, K., Schein, S.S., Roben, C.K.P., Dozier, M.: Parent coaching fidelity trajectories of in-person and telehealth sessions during the COVID-19 pandemic. Evid. Based Pract. Child Adolesc. Mental Health 7(3), 341–348 (2022)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Brati, E. (2024). Factors Affecting the Use of Telemedicine: An Empirical Analysis. In: Alareeni, B., Elgedawy, I. (eds) AI and Business, and Innovation Research: Understanding the Potential and Risks of AI for Modern Enterprises. Studies in Systems, Decision and Control, vol 440. Springer, Cham. https://doi.org/10.1007/978-3-031-42085-6_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-42085-6_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42084-9
Online ISBN: 978-3-031-42085-6
eBook Packages: EngineeringEngineering (R0)