Abstract
Infections are common in patients with chronic kidney disease (CKD). Alterations in immune system, need of invasive dialysis access procedures, frequent contact with healthcare services and poor response to vaccination increase risk of infections. Urinary tract infections, pneumonia and bacteremia or sepsis are common types of infections in patients with CKD. Infection-related hospitalisations have also been associated with future risk of adverse cardiovascular events and re-hospitalisation in CKD. The recent human coronavirus disease 2019 (COVID-19) pandemic led to significantly increased morbidity and mortality in patients with kidney disease. Acute kidney injury (AKI), hyponatremia, glomerular diseases and asymptomatic urinary abnormalities have been reported in patients with COVID-19. In certain regions like sub-Saharan Africa, human immunodeficiency virus (HIV) infection leading to kidney disease and management of HIV infection in patients with kidney disease are clinical challenges. Tuberculosis is common in patients with CKD and its diagnosis needs high index of suspicion. Drug dose modification is an important consideration while managing infections in patients with kidney disease. In addition to usual infection control practices, vaccinations against vaccine-preventable diseases are important. Though responses might be suboptimal, vaccinations do prevent or decrease the severity of infectious complications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic kidney disease
- Vaccination
- Urinary tract infections
- Human coronavirus disease 2019 (COVID-19)
- Dialysis
-
Infections are the second most common cause of morbidity and mortality in chronic kidney disease (CKD) patients.
-
Infections increase the risk of adverse cardiovascular events in CKD.
-
Uraemia-induced immune dysfunction, frequent visits to health-care facilities, frequent hospitalisation, need for vascular catheters and extracorporeal treatment increase infection risk.
-
Preventing infections is of utmost importance both in pre-dialysis and dialysis-dependent CKD patients.
19.1 Infections and Chronic Kidney Disease
Chronic kidney disease (CKD) is recognised as an important global health-care concern. The Global Burden of Disease (GBD) 2017 study estimated global prevalence of CKD at 9.1% (95% CI: 8.5–9.8%) in 2017 with major burden in regions with lower socio-demographic indices [1]. Between 1990 and 2017, the global all age mortality due to CKD increased by 41.3%. In the United States (US), the National Chronic Kidney Fact Sheet 2017 released by Centers for Disease Control and Prevention (CDC) estimated that approximately 96% of those with mildly reduced kidney function or kidney damage were unaware of their CKD status [2]. Besides being common, CKD also has major impact on the outcome of other major non-communicable diseases like diabetes and hypertension, 35 and 20% of whom develop CKD.
Infection control remains a major public health goal worldwide. Over the last few decades, a complex interplay between infections and CKD has become evident. A number of infections can cause kidney disease, and CKD predisposes patients to various infections. Chronic infections with organisms like hepatitis C virus (HCV), hepatitis B virus (HBV), and human immunodeficiency virus (HIV) are still responsible for a substantial proportion of CKD in some parts of the world. In addition, infection-related acute kidney injury may not recover completely and lead to CKD. Since 2020, the human coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has led to significant addition in the overall burden of both acute and chronic kidney diseases and increased the morbidity and mortality in patients with pre-existing kidney disease.
The high incidence of infections in CKD patients, including those on dialysis and after kidney transplantation, has been known for decades. Infections are the second most common cause of morbidity and mortality in these patients after cardiovascular disease. A number of risk factors increase the risk for infections in patients with kidney disease (Box 19.1). These include alterations in specific functions of various components of innate and adaptive immune system (Box 19.2). These changes are also responsible for poor response to vaccinations and failure to maintain protective antibody titres in CKD.
Box 19.1 Risk Factors for Infections in Kidney Disease
-
1.
Old age
-
2.
Female sex
-
3.
African American race
-
4.
Presence of diabetes mellitus
-
5.
Malnutrition
-
6.
Hypoalbuminaemia
-
7.
Impaired cutaneous defence
-
(a)
Severe oedema
-
(b)
Use of vascular access and peritoneal dialysis catheters
-
(c)
Needlestick injury for native arteriovenous fistulae or grafts
-
(a)
-
8.
Therapy related
-
(a)
Use of immunosuppressive drugs for treatment of basic disease
-
(b)
RBC or blood products transfusion
-
(c)
Contaminated caregiver’s hands or gloves, equipment, supplies and environmental surfaces
-
(d)
Use of iron preparationsFootnote 1
-
(e)
Bioincompatible dialysis (footnote 1)
-
(a)
-
9.
Increased hospitalisation for non-infectious complications
-
10.
Immunological dysfunction
-
11.
Poor vaccine response
Box 19.2 Immune System Alterations in CKD
-
1.
Polymorphonuclear leucocyte dysfunction
-
(a)
Increased reactive oxygen species production
-
(b)
Increased apoptosisSpontaneous activation and degranulation
-
(c)
Decreased phagocytosis
-
(a)
-
2.
Depletion of antigen presenting cells
-
3.
Monocyte dysfunction
-
(a)
Increased circulating monocytes (especially CD14+CD16+ monocytes)
-
(b)
Increased reactive oxygen species production
-
(c)
Increased basal integrin, toll-like receptor (TLR)-2 and TLR-4 expression
-
(d)
Increased cytokine production
-
(e)
Decreased phagocytosis
-
(a)
-
4.
T-cell dysfunction
-
(a)
Decreased regulatory T (Treg) cells
-
(b)
Reduced CD4/CD8 T-cell ratio
-
(c)
Decreased memory T cells (both central and naïve)
-
(a)
-
5.
B-cell dysfunction
-
(a)
Decreased B-cell number
-
(b)
Decreased antibody production
-
(a)
Though infections and cardiovascular disease may appear to be distinct clinical problems, modulation of underlying inflammatory state may be a common denominator linking the two in CKD. Data from United States Renal Data System (USRDS) Wave 2 study showed that the presence of bacteremia or septicaemia was associated with increased risk of death [hazard ratio (HR) 2.33, 95% confidence interval (CI) 1.38–2.28], myocardial infarction (HR 1.78, 95% CI 1.38–2.28), heart failure (HR 1.64, 95% CI 1.39–1.95), peripheral vascular disease (HR 1.64, 95% CI 1.34–2.0) and stroke (HR 2.04, 95% CI 1.27–3.28) [3]. Analysis of USRDS data revealed that the risk of cardiovascular events was increased by 25 and 18% at 1 and 3 months after an episode of infection-related hospitalisation compared to control periods [4]. Recent data on risk of cardiovascular disease in patients with CKD who were discharged after hospitalisation for sepsis also showed subsequent high risk of major adverse cardiovascular events (HR 1.42, 95% CI 1.37–1.47), myocardial infarction (HR 1.39, 95% CI 1.32–1.47), ischemic stroke (HR 1.46, 95% CI 1.40–1.52), hospitalisation for heart failure (HR 1.55, 95% CI 1.51–1.59) and all-cause mortality (HR 1.56, 95% CI 1.54–1.58) [5]. Data from the Canadian Study of Prediction of Risk and Evolution to Dialysis, Death and Interim Cardiovascular Events Over Time (CanPREDDICT), a prospective cohort study of patients with pre-dialysis CKD, showed independent association of infection with increased risk of cardiovascular ischemia (HR 1.80, 95% CI 1.24–2.60), congestive heart failure (HR 3.2, 95% CI 2.25–4.61), end-stage kidney disease (HR 1.58, 95% CI 1.22–2.05) or mortality (HR 3.39, 95% CI 2.65–4.33) in future [6]. These observational studies lend support to the intriguing hypothesis that the superimposition of macro-inflammatory events like bacterial infections over the persistent micro-inflammatory state of CKD might increase cardiovascular disease risk, despite apparent recovery from the infectious episode.
19.2 Epidemiology of Infections in CKD
For the purposes of discussion of infections, it is useful to divide the CKD population into two groups: pre-dialysis CKD and dialysis-dependent CKD. Besides becoming a defining moment for patient and treating physician as this change affects patient’s daily lifestyle and management, initiation of dialysis also alters the risk and consequences of infection by repeatedly breaching the physical defences and altering immune functions.
Pre-dialysis CKD patients have three times more risk of developing infectious complications as compared to general population [7]. Medicare data showed that urinary tract infection (UTI), pneumonia and bacteraemia or sepsis were four times, three times and four times, respectively, more common in pre-dialysis CKD population in the USA compared to the general population [7]. Sepsis and pneumonia were encountered in end-stage renal disease (ESRD) patients ten times and five times more commonly than general population [7]. Data from Cardiovascular Health Study (CHS) showed that after a median follow-up of 11.5 years, risk of all-cause hospitalisation secondary to infectious events increased 16, 37 and 64% in participants over the age of 65 with estimated glomerular filtration rate (eGFR) of (calculated using serum cystatin C level) 60–89, 45–59 and 15–44 mL/min/1.73 m2, respectively, as compared to those with eGFR ≥90 mL/ min/1.73 m2 [8]. The risks of UTI and pneumonia were 160 and 80% more in patients with eGFR 15–44 mL/min/1.73 m2 when compared to those with eGFR ≥90 mL/min/1.73 m2 [8]. Recent data from the CanPREDDICT cohort has shown infection rate of 14.3 infections/100 patient-years in patients with pre-dialysis CKD. Respiratory tract and urinary tract infections were the commonest, being recorded in 11.6% and 10.6% of the study cohort, respectively [6].
As per the latest 2021 USRDS Annual Data Report, adjusted hospitalisation rate for infection in 2019 in older patients (≥66 years, Medicare FFS beneficiaries) with CKD was 133 events per 1000 person-years [9]. This had declined by 10.7% between 2009 and 2019. The hospitalisation rate remained stable in patients with stage 3 CKD between 2009 and 2019. However, it decreased by 9% between 2009 and 2013 for patients with CKD stages 4–5 followed by 14% increase between 2014 and 2019. In 2019, hospitalisation rates for infection in patients with CKD stages 3 and 4–5 were 129 and 199 events per 1000 person-years, respectively. The overall hospitalisation rate for infection in patients with CKD was approximately 2.9 times higher as compared to those without CKD.
For adult patients with ESRD, USRDS reports that the adjusted rates of infection-related hospitalisation in 2019 in patients on haemodialysis, peritoneal dialysis and those with kidney transplant were 0.34, 0.44 and 0.24 admission events per person-year [9]. The adjusted rates for vascular access-related infections (in patients on haemodialysis) and peritonitis (in patients on peritoneal dialysis) were 0.14 and 0.03 admission events per person-year. These rates have largely remained stable over last 5 years since 2016. Sepsis was recorded as cause of death in 6.5%, 9.4% and 12.5% of patients who were receiving haemodialysis, peritoneal dialysis or were kidney transplant recipients, respectively, and had died during 2019. Previous USRDS reports have shown that rehospitalisation rate during transition to dialysis was highest if the index hospitalisation was infection related. During the quarter before initiation of dialysis, 44% of patients were readmitted within 30 days of discharge after an infection-associated hospitalisation. In the quarter after dialysis initiation, 44% of patients died or needed rehospitalisation within 30 days of discharge after infection-associated hospitalisation. Therefore, it appears that infections not only lead to acute problems but may also identify patients at higher risk of repeated hospitalisations. Whether this risk is related to infections or is a marker of otherwise poor underlying state is not clear.
19.2.1 Urinary Tract Infections
Urinary tract infections (UTI) are more common in certain subpopulations with CKD. These include patients with vesicoureteric reflux; interference with the normal flow of urine, either due to structural lesions, stricture, renal stone disease or secondary to functional problems like neurogenic bladder and diabetic cystopathy; or specific abnormalities like polycystic kidney disease. In addition to the frequency, some conditions can lead to more severe and/or special forms of UTI such as acute pyelonephritis, renal abscesses, renal papillary necrosis, emphysematous and xanthogranulomatous pyelonephritis or renal mucormycosis. In patients with CKD and UTI, presence of diabetes mellitus, indwelling catheter, length of hospital stay and infection with Klebsiella spp. have been independently associated with development of septicemia/urosepsis [10].
Another important consideration is distinguishing colonisation from true UTI especially in patients with underlying risk factors. A diagnosis of UTI should be made only when a patient is symptomatic, urinalysis shows significant pyuria (≥5 pus cells/hpf in centrifuged urine sample) and urine culture shows a significant growth. Asymptomatic bacteriuria is treated only in pregnant females and patients who have to undergo either surgery or instrumentation of the urinary tract which may involve mucosal breach. The 2019 Infectious Diseases Society of America (IDSA) update recommends starting broad spectrum antimicrobial treatment directed against urinary source in older patients with functional or cognitive impairment and bacteriuria, fever and other systemic signs consistent with sepsis but without any other localising features [11].
Established UTI in patients with CKD is treated as in general population. However, certain important considerations apply in this situation. First, if the basic disease leading to CKD is associated with any structural or functional alteration in the urinary tract, the initial treatment course is given for extended period (2–4 weeks depending on whether it is lower or upper UTI), and prophylaxis is given for 6–12 months if there are recurrent episodes of UTI. Second, the choice of antibiotics and their dosage may have to be changed in accordance with the degree of renal dysfunction. Nitrofurantoin which is commonly used for treatment and prophylaxis of UTI in general population is contraindicated in patients with eGFR <50 mL/min/1.73 m2. Third, risk of other complications like hyperkalaemia in CKD patients especially those on angiotensin-converting enzyme inhibitors or angiotensin receptor blockers may forbid long-term use of drugs like trimethoprim-sulfamethoxazole which are commonly used in general population for prophylaxis. Fourth, cyst infection is a unique form of kidney infection seen in polycystic kidney disease patients which requires prolonged course of antibiotics (up to 6 weeks) and at times may be refractory and thus require surgical intervention. Whereas trimethoprim-sulfamethoxazole remains the first choice in acute, uncomplicated, lower UTI in patients with CKD stage 3a, either ciprofloxacin or extended spectrum penicillin like pivmecillinam (especially in European countries where it is available) are recommended in CKD stages 3b–5. Local patterns of urinary tract pathogens and their drug sensitivities may be considered to modify recommendations in local context. It is important to note that the duration of treatment of acute, uncomplicated, lower UTI in females and males without any predisposing factors is different at 3 and 7 days, respectively. It is very important that attempts at modifying risk factors for recurrent UTI (e.g. surgical relief of obstruction, clean intermittent self-catheterisation in large volume neurogenic bladder) are made early as treatment becomes increasingly difficult because of urinary tract colonisation with drug-resistant organisms.
19.2.2 Pneumonia
Community-acquired pneumonia is a common cause of hospitalisation in general population. The risk of pneumonia increases progressively with fall in GFR. Compared to those without kidney disease, the incidence of pneumonia in patients with CKD is 2.3 times higher [12]. This risk further translates into increased severity of disease at admission and higher mortality rates during admission and at 1 month after discharge. Streptococcus pneumoniae is the most common cause of community-acquired pneumonia in CKD patients. Vaccination against pneumococcus has been shown to be beneficial in improving outcomes. It has also been shown to be cost effective in adults aged 50 years or older [13]. CKD patients are also at increased risk of developing severe forms of influenza.
19.2.3 COVID-19
Since early in 2020, the SARS-CoV2 virus infection became an important cause of morbidity and mortality in patients with kidney disease. COVID-19, which started in late 2019, has had direct and indirect effects which have greatly impacted the care of patients with kidney disease. Patients with CKD, ESRD on dialysis or kidney transplants are variably immunosuppressed, and hence, at high risk of acquiring this infection as well as development of complications. Though pneumonia leading to respiratory failure is the most important complication, COVID-19 is now recognised as a multi-system disease with both short- and long-term implications. Renal manifestations include proteinuria, microscopic haematuria, pyuria, tubular dysfunction, hyponatremia, occasional glomerular syndromes like podocytopathy, collapsing glomerulopathy, etc. and AKI. Though the reported incidences vary with the type of setting and study population, AKI has been reported to be a common complication in patients hospitalised with COVID-19. A recent meta-analysis reported overall incidence of AKI as 12.3% (95% CI 7.3–20.0%) [14]. Majority (77%) with AKI were critically ill and almost one-fourth needed dialysis. Not surprisingly, mortality was 13 times higher in patients with AKI as compared to those without AKI. Recent data on long-term renal outcomes after COVID-19 suggest that these patients, particularly those with AKI or long COVID, are at risk of major adverse kidney events (MAKE) in future. Data from a large cohort of US Veterans showed that for patients who survived beyond 30 days after COVID-19, the adjusted risk for AKI (HR, 1.94; 95% CI, 1.86–2.04), eGFR decline ≥30% (HR, 1.25; 95% CI, 1.14–1.37), eGFR decline ≥40% (HR, 1.44; 95% CI, 1.37–1.51), eGFR decline ≥50% (HR, 1.62; 95% CI, 1.51–1.74), ESRD (HR, 2.96; 95% CI, 2.49–3.51) and MAKE (HR, 1.66; 95% CI, 1.58–1.74) were higher as compared to non-infected controls [15]. The treatment guidelines for COVID-19 are no different in patients with kidney disease except for the fact that caution may be needed with respect to drug interactions and dosing. For newer drugs, use in experimental settings is advocated till definite data becomes available.
Patients on maintenance haemodialysis constituted a special group that was hugely impacted by the COVID-19 pandemic. Disruption of medical facilities and diversion of resources towards containment of pandemic impaired access to dialysis. Overall, mortality in dialysis patients due to COVID-19 ranged between 20 and 30% which was almost four times higher than what was recorded in patients with pre-dialysis CKD [16]. In a meta-analysis that included kidney transplant recipients with COVID-19, AKI and mortality were reported in 50% and 23% of patients, respectively [17].
19.2.4 HIV Infection
The prevalence of CKD is increased in incident patients of HIV infection starting antiretroviral therapy. About one-third of patients with HIV infection have CKD. The spectrum of kidney involvement in HIV infection ranges from asymptomatic proteinuria to nephrotic syndrome, acute kidney injury or progressive decrease in GFR. A pathologic classification based on dominant involvement of glomerular or tubulo-interstitial or vascular compartments or kidney disease due to other aetiologies in HIV has been proposed [18]. The majority of patients have HIV-associated nephropathy (HIVAN) which most frequently presents as nephrotic syndrome and is characterised histologically by collapsing glomerulopathy and variable tubulo-interstitial involvement. African American race, APOL1 high-risk variants, decreased CD4 counts and family history of kidney disease are risk factors for development of HIVAN. All patients with HIVAN should be given antiretroviral therapy irrespective of their eGFR. In CKD patients, the presence of HIV infection is considered a risk factor for accelerated decline in GFR. Conversely, presence of CKD is also a risk factor for progression of HIV infection. Drug interactions and drug-induced kidney injury are very important treatment considerations in patients with HIV and CKD. In patients with reduced eGFR, proteinuria, age >60 years or comorbidities like HCV co-infection, diabetes mellitus, uncontrolled hypertension or history of cardiovascular disease, the following nephrotoxic drugs may be avoided: atazanavir, lopinavir, indinavir and tenofovir disoproxil fumarate. The risk of lactic acidosis does not forbid the use of nucleoside analogues in patients with CKD, but careful monitoring is advisable. Though annual screening for kidney involvement by urine protein and eGFR estimation is recommended, this frequency should be increased to biannually in patients at risk of drug-induced kidney injury or those with presence of other comorbidities that predispose to kidney disease. Finally, as the life expectancy of HIV-infected population on therapy has progressively increased, unrelated risk factors for CKD, e.g. diabetes, hypertension, etc., have also become important now. Effectively treated ESRD patients for ≥6 months and without any opportunistic infections or malignancy may be candidates for kidney transplantation.
19.2.5 Vascular Access-Related Infections
Patients with CKD are at risk of potentially lethal vascular access-related infections later in the course of disease because attention is not paid to timely creation of appropriate access. As a result, large proportions of CKD patients start dialysis with central venous catheters. The risk is highest for non-tunnelled central venous catheters followed by tunnelled ones, arteriovenous grafts and native arteriovenous (AV) fistulae [19]. Amongst 1846 participants in the HEMO study, of whom only 7.6% were using catheters, first infection-related hospitalisation was due to non-access-related infection in 79% patients [20]. However, in HD population using catheters for vascular access at a large centre in the USA, non-access-related infections accounted for just 12% of all proven infectious episodes [21]. Staphylococcus aureus, coagulase-negative staphylococci and enterococci are the most common organisms responsible for access-related bloodstream infections and may become complicated by infective endocarditis or osteomyelitis. Recent data highlight that increasing proportion of such infections are now being caused by gram negative organisms [19]. Of particular concern are infections with multidrug-resistant bacteria and nosocomial transmission to other patients. As a result of these problems, timely creation of AV fistulae, dubbed the ‘Fistula First’ initiative, is targeted at reducing catheter usage.
19.2.6 Blood-Borne Infections
Patients with CKD are at risk of acquiring blood-borne infections like hepatitis B and C due to repeated skin punctures, need of blood or blood products and sharing of contaminated machines, surfaces or supplies in hospitals. Better staff training, improved infection control practices, regular screening and universal vaccination of patients and staff have reduced the HBV prevalence and seroconversion rates [22]. HCV infection, an important problem with prevalence ranging from 0.7 to 18.1% in Asia-Pacific countries and 2.7 to 20% in Europe till few years back, is now being treated effectively with the advent of directly acting antiviral agents (DAA). The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines were updated in 2018 in view of new evidence that showed high effectiveness of DAA based therapies in patients with varying degrees of kidney dysfunction [23] (see Chap. 20). As is true for antiretroviral therapy, drug interactions need to be kept in mind while prescribing DAAs. KDIGO recommends strict infection control measures as the most important tool for preventing its spread.
19.2.7 Tuberculosis
Tuberculosis is an important infection in patients with CKD, with up to five times higher risk as compared to general population [24,25,26]. The risk is even higher in kidney transplant recipients at almost 11 times as compared to general population [24]. The diagnosis is not straightforward as the disease is more commonly extra-pulmonary with variable nonspecific manifestations like fever, weight loss, malaise, etc., which frequently delay diagnosis. Therefore, a high index of suspicion is required. As definitive diagnosis by culture takes a long time and absence of acid-fast bacilli on staining does not rule out tuberculosis, treatment is often started empirically in a significant proportion of patients on the basis of strong clinical suspicion and suggestive investigations, e.g. granulomatous inflammation on histopathology. There is controversy about the need and optimal method of screening for latent tuberculosis. However, the utility of screening in endemic regions with high prevalence of this disease is not clear. Interferon gamma assays like QuantiFERON-TB Gold test have been shown to be better than tuberculin skin test for detecting latent tuberculosis. Tuberculosis is treated as in non-CKD population, but drug dose modification for level of eGFR is recommended.
19.2.8 Other Infections
The incidences of dyspepsia and gastroduodenal disease are more in CKD patients as compared to general population. Though Helicobacter pylori infection has been found to be less prevalent in patients with chronic kidney disease, whenever present, it is treated as in patients with normal renal function [27]. Similarly, infective endocarditis is also treated as in general population. Patients with CKD and risk factors for development of infective endocarditis (prosthetic heart valves, valvular heart disease, valvular calcification, etc.) should receive antibiotic prophylaxis (amoxicillin 2 g or clindamycin 600 mg) prior to invasive dental and periodontal procedures.
It has been shown that mortality after septic shock due to various reasons is significantly more in patients with reduced GFR. In fact, eGFR <60 mL/min/1.73 m2 remains an independent predictor of early and late mortality in patients with septic shock even after correction for comorbidities like diabetes, hypertension and cardiovascular disease.
The treatment of essentially all infectious diseases is same as in general population. However, drug dose modification or choosing alternative drug may be required as per patient’s eGFR.
19.3 Infection Control in CKD
Globally, infection control and prevention is one of the biggest goals of public health. According to the World Health Organization (WHO), the objective of infection prevention and control is to ensure protection of those who might be vulnerable to an infection either in general community or while utilising health-care facilities. WHO identifies hygiene as the basic principle of infection prevention and control. Patients with CKD are treated in the same manner as are general non-CKD population for established infections. Important considerations in this population include the assessment of comorbidities and risk factors, antimicrobial dose adjustment for level of kidney function, consideration of drug interaction and preventing superimposed acute kidney injury due to infections or use of radiocontrast agents or drugs used to treat the infection.
19.3.1 Vaccination in Patients with CKD
In addition to general measures, timely vaccination is important in infection control (Box 19.3). The impact of vaccination in preventing, eliminating and eventually eradicating the disease has been convincingly demonstrated throughout the world through the universal immunisation programmes. The Advisory Committee on Immunization Practices (ACIP) in the US annually updates and recommends immunisation schedules for children and adults. Kidney disease patients are classified at having high infection risk. Although vaccination is effective in CKD, these patients mount an inferior response to vaccination and suffer relatively rapid decline in protective antibody titres as compared to general population.
Box 19.3 Measures Aimed at Reducing Infections in CKD Patients
-
1.
Vaccination against vaccine-preventable diseases
-
2.
Timely creation of dialysis access
-
3.
Maximising use of native arteriovenous fistulae in prevalent and incident haemodialysis patients
-
4.
Universal precautions to be followed at health-care facilities
-
5.
Rationalising antibiotic use according to local antimicrobial resistance data
-
6.
Practising hand hygiene by patient and caregiver
It is important to assess and record immunisation history of every CKD patient at initial presentation. Physicians should be aware of differences between contraindications and precautions with respect to vaccination. While a contraindication precludes vaccination because of significant risk of adverse events, a precaution either means slightly increased risk of adverse events or decreased immune response to vaccine.
Severe allergic reaction or anaphylactic response to a vaccine or its constituents (e.g. egg, gelatin, latex, adjuvants) is a contraindication. Usually, vaccines are not administered even in situations where precaution is advised. It is important to note that not all contraindications or precautions are permanent. Mild acute febrile illnesses, previous mild local reactions and breast-feeding are not contraindications to vaccination. Vaccination should be deferred for 4 weeks after recovery from acute febrile illnesses. Live virus vaccines (varicella, zoster and MMR) are contraindicated in pregnancy and states of severe immunosuppression, e.g. primary or acquired immunodeficiency, steroid dose equivalent of prednisolone dose ≥20 mg/day for ≥2 weeks, malignancies involving the bone marrow or lymphatic system, etc. Particular attention should be paid to storage conditions, vaccine diluents, dose, site and mode of administration. Adult vaccines are usually administered by intramuscular route except varicella, zoster, MMR and inactivated meningococcal polysaccharide vaccine which are given by subcutaneous route. Multiple vaccines can be administered simultaneously, but sites should be separated by at least 1–2 in. However, if immune globulin is also administered, a different anatomic site should be used.
All HbsAg-negative and anti-HBs negative patients must be vaccinated against HBV at the time of initial diagnosis irrespective of the stage of CKD. Higher dose of 40 μg in a four-dose schedule (0, 1, 2 and 6 months) has been shown to achieve higher seroconversion rates [28]. Though seroconversion rates in pre-dialysis stages of CKD are better, they are still suboptimal as compared to general population. An anti-HBs titre of >10 IU/L is considered protective and titre below this level warrants booster dose. A number of strategies have been used to increase the immunogenicity: these include increasing dose and frequency of vaccination, intradermal route of administration, using pre-S2/S antigens, use of adjuvants like 3-0-desacyl-4′-monophosphoryl lipid A adsorbed on aluminium phosphate and immunostimulants like levamisole and granulocyte macrophage colony stimulating factor. The data, however, is inconclusive because of small sample sizes, variable doses and schedules and conflicting results. The antibody titres should be monitored annually in all previously vaccinated patients to ensure maintenance of protective levels.
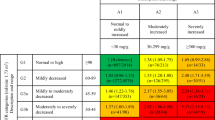
Annual vaccination against influenza decreases the risk of hospitalisation and death in CKD patients. Only inactivated influenza vaccine is recommended. Pneumococcal vaccination is also recommended for all patients with renal failure. A large retrospective analysis of about 37,000 patients on dialysis in the US has shown that vaccination against influenza and pneumococcus was independently associated with survival [29]. As compared to no vaccination, adjusted odds ratio of all-cause mortality amongst patients vaccinated for influenza alone and both influenza and pneumococcal vaccination were 0.79 (95% CI, 0.72–0.86) and 0.70 (95% CI, 0.62–0.78), respectively. The KDIGO clinical practice guidelines for management of CKD also recommend vaccination against influenza, pneumococcus and HBV. ACIP recommends that except for meningococcal, Haemophilus influenzae type b and hepatitis A vaccines, all other recommended vaccines should be considered in adult patients with CKD if they have not received them (Table 19.1). Vaccination against Staphylococcus aureus has not been found to be effective in preventing septicaemia in dialysis patients and is not recommended. Routine paediatric immunisation schedule should be followed in children with CKD. Only inactivated polio vaccine should be used in patients with renal failure. As previously stated, live influenza vaccine is contraindicated, and caution is required before use of other live vaccines in children with CKD.
All patients with advanced CKD should preferably be vaccinated before kidney transplantation. The seroconversion rates come down drastically if vaccines are administered after transplantation. Live vaccines are contraindicated in kidney transplant recipients, and it is preferable to postpone other vaccinations till 6 months after transplant.
Vaccination is strongly advocated against COVID-19 in patients with CKD, ESRD or kidney transplant recipients, as these groups are at higher risk of developing severe COVID-19. As is expected, the response to vaccination is inferior as compared to that in normal individuals. Nevertheless, the neutralising antibody response improves with booster doses given after usual two-dose schedule for most of the vaccines. The emergence of newer variants of concern, higher likelihood of their antibody escape and possible waning of pre-existing antibody titres also speak for periodic booster doses, especially as vaccines are updated to provide protection against the new variants. Vaccine hesitancy was identified as an important barrier to vaccination, especially in poorly informed and under-privileged groups. Currently, four main types of vaccines are available: mRNA, killed whole virus, purified virus component and replication defective viral vector carrying pathogen gene vaccine. Access is variable depending on availability and local regulatory approvals. Preliminary data suggest that mRNA vaccines may be more immunogenic as compared to adenoviral vector vaccines in dialysis patients [31]. However, patients should be encouraged to take vaccines as per availability and prevailing dosing recommendations. Decisions need to be individualised in cases with active autoimmune kidney diseases or on significant immunosuppressive therapy. Despite inferior immunogenic responses, vaccination does protect these patients against severe disease.
Despite recommendations, the overall vaccination rates remain low, varying from 26 to 65% and 15 to 46% in dialysis and pre-dialysis CKD patients, respectively. Targeted interventions at educating health-care staff coupled with regular monitoring and review have been shown to improve vaccination rates.
19.4 Conclusion
Infections are common cause of morbidity and mortality in CKD patients. Increasing patient age, presence of multiple comorbidities, the underlying immunosuppressive uraemic milieu and the use of dialysis catheters contribute to the infection risk, complicate clinical presentation and make management complex. Prevention of infections requires institution and implementation of appropriate guidelines including vaccination (Boxes 19.4 and 19.5). Tuberculosis is an important infection in certain geographic areas and requires high degree of clinical suspicion for timely diagnosis.
Box 19.4 What the Guidelines Say You Should Do?
-
1.
All general principles of infection control and management apply in CKD population.
-
2.
Always consider drug dose modifications and try to prevent drug-induced nephrotoxicity in patients with CKD.
-
3.
Trimethoprim-sulfamethoxazole is the drug of choice for acute, uncomplicated, lower UTI in patients with CKD stage 3a.
-
4.
Ciprofloxacin or extended spectrum penicillin like pivmecillinam is the drug of choice for acute, uncomplicated, lower UTI in patients with CKD stage 3b to 5.
-
5.
Tuberculosis in CKD
-
(a)
Tuberculin skin testing may be negative in CKD patients despite infection.
-
(b)
Patients with active tuberculosis should receive standard chemotherapeutic agents for standard duration with drug dose modifications for level of eGFR.
-
(a)
-
6.
HIV in CKD
-
(a)
All patients with HIVAN should be given antiretroviral therapy irrespective of their eGFR.
-
(b)
Annual screening for renal involvement by urine protein and eGFR estimation is recommended. However, this frequency should be increased to biannually in patients who are at risk of drug-induced kidney injury or have other risk factors for kidney disease.
-
(c)
Drug dose modification and interactions should be considered before prescribing drugs in CKD patients with HIV infection.
-
(a)
-
7.
Vaccination in CKD
-
(a)
Consider individual’s immune status and specific vaccine recommendations before using live vaccines in CKD patients.
-
(b)
All CKD patients should be vaccinated against hepatitis B virus, pneumococcus and influenza virus at diagnosis, if they are vaccination naive.
-
(c)
Revaccinate annually against influenza virus and every 5 years against pneumococcus.
-
(d)
Monitor anti-HBs titres annually and revaccinate with booster dose if titres are below <10 IU/L.
-
(e)
All patients should be encouraged to get COVID-19 vaccines as per prevailing recommendations.
-
(a)
Box 19.5 Relevant Guidelines
-
1.
KDIGO Clinical Practice Guideline for Hepatitis C in Chronic Kidney Disease
Executive summary of the 2018 KDIGO Hepatitis C in CKD Guideline: welcoming advances in evaluation and management. Kidney Int. 2018;94(4):663–73. (https://www.sciencedirect.com/science/article/pii/S0085253818304484?via%3Dihub)
-
2.
Scottish Intercollegiate Guidelines Network
Management of suspected bacterial urinary tract infection in adults. Scottish Intercollegiate Guideline Network Guideline No.88 July 2012 (http://www.sign.ac.uk/pdf/sign88.pdf).
-
3.
Advisory Committee on Immunization Practices (ACIP) Guideline
Advisory Committee on Immunization Practices Recommended Immunization Schedule for Adults Aged 19 Years or Older - United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(7):229–33.
(https://www.cdc.gov/mmwr/volumes/71/wr/mm7107a1.htm?s_cid=mm7107a1_w)
-
4.
Infectious Diseases Society of America Guideline
Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D, et al. Clinical Practice Guideline for the Management of Asymptomatic Bacteriuria: 2019 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2019;68(10):e83–e110. (https://academic.oup.com/cid/article/68/10/e83/5407612?login=true)
-
5.
British Thoracic Society Guideline
Milburn H, Ashman N, Davies P, Doffman S, Drobniewski F, Khoo S, et al. Guidelines for the prevention and management of Mycobacterium tuberculosis infection and disease in adult patients with chronic kidney disease. Thorax. 2010;65(6):557–70. (http://thorax.bmj.com/content/65/6/559.long)
NICE Guideline for tuberculosis (2016) (https://www.nice.org.uk/guidance/ng33/resources/tuberculosis-pdf-1837390683589)
Before You Finish: Practice Pearls for the Clinician
-
Despite decrease in the rate of access-related and blood-borne infections, the overall rate of infections in dialysis patients remains high.
-
Improving native arteriovenous fistula utilisation, reducing catheter use, timely vaccination and implementation of infection control guidelines are important for preventing access-related infections.
-
CKD patients need to be vaccinated against hepatitis B virus, pneumococcus, COVID-19 and influenza as early as possible.
-
Vaccination response may be suboptimal and needs monitoring in subjects with CKD.
-
Management considerations include measures to prevent acute kidney injury and drug toxicity.
-
Tuberculosis is important in certain geographic areas and requires high degree of clinical suspicion for timely diagnosis.
Notes
- 1.
Increase oxidative stress.
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.
National Chronic Kidney Disease fact sheet 2017: CDC; [cited 2022 July 13]. https://www.cdc.gov/diabetes/pubs/pdf/kidney_factsheet.pdf.
Ishani A, Collins AJ, Herzog CA, Foley RN. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS Wave 2 study. Kidney Int. 2005;68(1):311–8.
Dalrymple LS, Mohammed SM, Mu Y, Johansen KL, Chertow GM, Grimes B, et al. Risk of cardiovascular events after infection-related hospitalizations in older patients on dialysis. Clin J Am Soc Nephrol. 2011;6(7):1708–13.
Shih CJ, Chao PW, Ou SM, Chen YT. Long-term risk of cardiovascular events in patients with chronic kidney disease who have survived sepsis: a Nationwide Cohort Study. J Am Heart Assoc. 2017;6(2):e004613.
Cheikh Hassan HI, Tang M, Djurdjev O, Langsford D, Sood MM, Levin A. Infection in advanced chronic kidney disease leads to increased risk of cardiovascular events, end-stage kidney disease and mortality. Kidney Int. 2016;90(4):897–904.
Naqvi SB, Collins AJ. Infectious complications in chronic kidney disease. Adv Chronic Kidney Dis. 2006;13(3):199–204.
Dalrymple LS, Katz R, Kestenbaum B, de Boer IH, Fried L, Sarnak MJ, et al. The risk of infection-related hospitalization with decreased kidney function. Am J Kidney Dis. 2012;59(3):356–63.
USRD System. 2021 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2021.
Dimitrijevic Z, Paunovic G, Tasic D, Mitic B, Basic D. Risk factors for urosepsis in chronic kidney disease patients with urinary tract infections. Sci Rep. 2021;11(1):14414.
Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D, et al. Clinical practice guideline for the Management of Asymptomatic Bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis. 2019;68(10):e83–e110.
Chou CY, Wang SM, Liang CC, Chang CT, Liu JH, Wang IK, et al. Risk of pneumonia among patients with chronic kidney disease in outpatient and inpatient settings: a nationwide population-based study. Medicine (Baltimore). 2014;93(27):e174.
Ishigami J, Padula WV, Grams ME, Chang AR, Jaar B, Gansevoort RT, et al. Cost-effectiveness of pneumococcal vaccination among patients with CKD in the United States. Am J Kidney Dis. 2019;74(1):23–35.
Oliveira CB, Lima CAD, Vajgel G, Campos Coelho AV, Sandrin-Garcia P. High burden of acute kidney injury in COVID-19 pandemic: systematic review and meta-analysis. J Clin Pathol. 2021;74(12):796–803.
Bowe B, Xie Y, Xu E, Al-Aly Z. Kidney outcomes in long COVID. J Am Soc Nephrol. 2021;32(11):2851–62.
El Karoui K, De Vriese AS. COVID-19 in dialysis: clinical impact, immune response, prevention, and treatment. Kidney Int. 2022;101(5):883–94.
Kremer D, Pieters TT, Verhaar MC, Berger SP, Bakker SJL, van Zuilen AD, et al. A systematic review and meta-analysis of COVID-19 in kidney transplant recipients: lessons to be learned. Am J Transplant. 2021;21(12):3936–45.
Swanepoel CR, Atta MG, D’Agati VD, Estrella MM, Fogo AB, Naicker S, et al. Kidney disease in the setting of HIV infection: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) controversies conference. Kidney Int. 2018;93(3):545–59.
Crowe K, White B, Khanna N, Cooke B, Kingsmore DB, Jackson A, et al. Epidemiology of bloodstream infections in a Scottish haemodialysis population with focus on vascular access method. J Hosp Infect. 2021;110:37–44.
Allon M, Depner TA, Radeva M, Bailey J, Beddhu S, Butterly D, et al. Impact of dialysis dose and membrane on infection-related hospitalization and death: results of the HEMO study. J Am Soc Nephrol. 2003;14(7):1863–70.
Al-Solaiman Y, Estrada E, Allon M. The spectrum of infections in catheter-dependent hemodialysis patients. Clin J Am Soc Nephrol. 2011;6(9):2247–52.
Li PK, Chow KM. Infectious complications in dialysis--epidemiology and outcomes. Nat Rev Nephrol. 2011;8(2):77–88.
Jadoul M, Berenguer MC, Doss W, Fabrizi F, Izopet J, Jha V, et al. Executive summary of the 2018 KDIGO hepatitis C in CKD guideline: welcoming advances in evaluation and management. Kidney Int. 2018;94(4):663–73.
Al-Efraij K, Mota L, Lunny C, Schachter M, Cook V, Johnston J. Risk of active tuberculosis in chronic kidney disease: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2015;19(12):1493–9.
Min J, Kwon SK, Jeong HW, Han JH, Kim YJ, Kang M, et al. End-stage renal disease and risk of active tuberculosis: a Nationwide Population-Based Cohort Study. J Korean Med Sci. 2018;33(53):e341.
Ruzangi J, Iwagami M, Smeeth L, Mangtani P, Nitsch D. The association between chronic kidney disease and tuberculosis; a comparative cohort study in England. BMC Nephrol. 2020;21(1):420.
Shin SP, Bang CS, Lee JJ, Baik GH. Helicobacter pylori infection in patients with chronic kidney disease: a systematic review and meta-analysis. Gut Liver. 2019;13(6):628–41.
Reddy S, Chitturi C, Yee J. Vaccination in chronic kidney disease. Adv Chronic Kidney Dis. 2019;26(1):72–8.
Bond TC, Spaulding AC, Krisher J, McClellan W. Mortality of dialysis patients according to influenza and pneumococcal vaccination status. Am J Kidney Dis. 2012;60(6):959–65.
Murthy N, Wodi AP, Bernstein H, Ault KA, Advisory Committee on Immunization Practices, Advisory Committee on Immunization Practices. Recommended adult Immunization schedule, United States, 2022. Ann Intern Med. 2022;175(3):432–43.
Windpessl M, Bruchfeld A, Anders HJ, Kramer H, Waldman M, Renia L, et al. COVID-19 vaccines and kidney disease. Nat Rev Nephrol. 2021;17(5):291–3.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kumar, V., Jha, V. (2023). Infectious Complications and Vaccination in Chronic Kidney Disease. In: Arıcı, M. (eds) Management of Chronic Kidney Disease. Springer, Cham. https://doi.org/10.1007/978-3-031-42045-0_19
Download citation
DOI: https://doi.org/10.1007/978-3-031-42045-0_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42044-3
Online ISBN: 978-3-031-42045-0
eBook Packages: MedicineMedicine (R0)