Abstract
Otitis media is certainly the most advanced field in otorhinolaryngology in terms of evidence-based medicine. In recent years, there has been considerable growth in the number of publications related to otitis media. However, this does not constitute a proportional step up in quality. Unfortunately, there is not enough time available for a critical appraisal of all these publications, and clinicians frequently need to rely on guidelines. However, these reviews and guidelines may be biased by personal positions. So, it is essential that clinicians read the original source, interpret results, and be capable of delving deeper into the data presented in an article. Not everything that is published is necessarily reliable, even if it has been peer-reviewed. Irrespective of the subject being studied, reading any article should always adhere to the principles of reading with critical analysis that takes into account the size of the study, its clinical relevance, and the capacity for generalization of results. This chapter is therefore intended to provide tools and strategies to enable clinicians to conduct their own critical analyses of publications on otitis media and select what they should actually incorporate into their clinical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
While we have witnessed considerable growth in the number of publications related to otitis media, this does not necessarily constitute a proportional step up in the quality of what is being published. Busy clinicians often lack the time required for interpretation and critical appraisal of publications and therefore rely on opinion formers in the area to publish guidelines or review articles. However, delegating interpretation to third parties exposes it to certain risks since such analyses may be biased by personal positions. It is therefore essential that clinicians are trained to be able to go directly to the original source and interpret results in a manner analogous to the approach they adopt when, starting with the clinical examination of a patient, they follow a process culminating in establishing the correct diagnosis. Clinicians should be capable of delving deeper into the data presented in a publication than can be achieved by merely reading the abstract.
One fundamental concept that clinicians must internalize is that not everything that is published is necessarily reliable, even if it has been peer-reviewed, published in a scientific journal of international renown, or has a high impact factor. This chapter is therefore intended to provide tools and strategies to enable clinicians to conduct their own critical analyses of publications on otitis media and select what they should actually incorporate into their clinical practice.
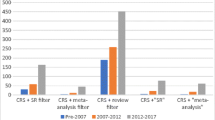
The first task is to select articles that merit reading in depth. On PubMed, a search using the terms “otitis” AND “media” returns a total of 31,347 publications. We must therefore be a little more specific with regard to the subject we are interested in, such as “acute otitis media”, “chronic otitis media”, or “otitis media with effusion”. However, even these terms return lists of thousands of publications, so we need to apply filters based on the period of publication and type of study (meta-analysis, randomized clinical trial, literature review, etc.). This strategy can narrow our search and help us separate out those publications that are worth the effort of exploring in greater detail.
The subject of otitis media is undoubtedly the most advanced area within otorhinolaryngology in terms of incorporating the concepts of evidence-based medicine. For decades, management of acute otitis media and otitis media with effusion has been based on the results of large randomized clinical trials and meta-analyses. As a result, this is where we will find the studies considered to have the highest evidence levels, in particular because of the high prevalence of these diseases in the population. In contrast, in the area of chronic otitis media, it is more difficult to produce large-scale randomized clinical trials, both because of its lower prevalence and also because of the highly heterogeneous nature of clinical presentation and course in this population. The great majority of studies of surgical treatment for chronic otitis media are therefore retrospective observational studies. Even so, several randomized clinical trials have been conducted in the area over recent years, especially for the evaluation of surgical techniques.
Irrespective of the subject being studied, reading any article should always adhere to the principles of reading with critical analysis that takes into account the size of the study, its clinical relevance, and the capacity for generalization of results. The act of reading a scientific article cannot be passive but must include a critical interpretation of the data presented. Furthermore, it is important to emphasize that a single study in isolation should not be enough to definitively change our practice. We need additional evidence that presents the results in a reproducible form and, when possible, in meta-analyses that support the findings.
Which Articles Should I Choose to Read?
Starting from a list of tens or hundreds of publications on otitis media, the initial selection will be based on the titles and abstracts. Providing that the author has been able to express it adequately, the relevance of what an article will present can be discerned from its title. An abstract that manages to clearly summarize the objectives and results increases the probability that the article is of interest for more in-depth reading.
As we select the articles, we can rapidly read through them to identify the basic elements that should be part of all scientific publications. The introduction should be clear, concise, and logical and should end by stating the primary objective of the research. The methods should be described in sufficient detail to enable the study to be reproduced. The results must be well organized and presented. The discussion section should integrate the results with those of the extant literature on the subject. The conclusions must follow the research objectives and be supported by the results.
Gehlbach [1] compares reading an article to eating a meal. The title is the menu, and the abstract is the taster for the dishes. However, this is not close enough to a meal to satisfy. The introduction to the article introduces the appetizers, which, when well served, increase the diner’s appetite for the main course. The methods and results represent the main course and need to be well digested and analyzed. The discussion represents the dessert and can be rich in creativity and speculation. In some cases, it may be the part of the meal that is most appreciated, but it is not the most nutritious.
Once we have chosen which articles we will read in depth, we need to train ourselves to conduct a critical reading of a given publication. These considerations apply equally to articles on otitis media and to those on any other topic.
The impact factor of a given scientific journal may be indicative of an article’s quality, but it is not a determinant factor. This can be exemplified by articles published on the subject of acute otitis media, which have wide coverage in many areas of medicine (otorhinolaryngology, pediatrics, family medicine, etc.), compared with the limited audience for articles on surgical treatment of chronic otitis media, which is restricted in interest to otological surgeons. As a result, it is easier to publish articles on acute otitis media in high-impact scientific journals compared with articles on surgical subjects. It is also important to take into account the credibility of the authors and the institution that promoted the research.
A study’s evidence level may be related to the importance of a given publication. Figure 13.1 shows a diagram illustrating evidence levels, but these are not always a determinant factor in the quality of a publication. The fact is that a randomized clinical trial is not necessarily better than a cohort study. We could have a randomized clinical trial with several selection or measurement biases, for example. Conversely, we could have a large, well-delineated cohort with good follow-up.
Methodology
The methodology is a crucial section of any scientific article, and so here we can already get a good preview of the quality of what will be presented further on. In this section, we will read how the research was conducted, and the proper critical analysis begins with the methods.
The first point is to check how the data were collected. As a general rule, prospective intervention studies yield higher-quality data because data collection is conducted under more carefully controlled conditions, as seen in randomized clinical trials. In contrast, the data used in retrospective studies generally come from medical records or are based on the research participants’ recollections, thus increasing the probability of biases. For example, there will be less precision in a subjective assessment of the degree of otalgia during an episode of acute otitis media that occurred in the past or was recorded in medical records in an uncontrolled manner when compared with the collection of the same data as part of a prospective follow-up of the episode by a single evaluator trained for this purpose. This does not mean that data collected retrospectively is unreliable, but, in general, it is of lower quality when compared to intervention studies.
Articles on the treatment of otitis media should ideally include a group for comparison. If not, the study will simply be a description of a case series without the capacity to provide data on associations or efficacy. A comparison of different clinical and surgical treatments is essential to establishing reliable conclusions. When possible, a placebo control can amplify the assessment of the efficacy of the different treatments studied. Considering that untreated acute otitis media (adopting a “watchful waiting” approach) tends to have favorable outcomes, the inclusion of a control group is considered even more important. Along the same lines, it is to be expected that the number of recurrent infections reduces as children grow and their immune systems mature, and otitis media with effusion can also be expected to resolve as children grow and tube function improves. Therefore, a control group enables an adequate comparison with the natural history of otitis media.
Relationships of causality can be assessed to test hypotheses, either prospectively or retrospectively. Cross-sectional studies do not provide grounds for drawing conclusions of causality but only for the identification of associations, as in research investigating diagnostic tests or prevalence studies.
According to the CONSORT recommendations [2], randomization is generally an excellent strategy for achieving a better balance between potential factors of bias across different groups. This is why nonrandomized studies may need to adjust for confounding factors. However, this does not mean that just because a study is a randomized clinical trial, it is guaranteed to be of good quality; it just means that an observational study is not as reliable. Randomization is only one part of the methodology, and so it is also essential that the other methods are appropriate. In addition to randomization, blinding is also considered important and, preferably, should be conducted in such a manner that neither subjects nor investigators know which group participants are allocated to (“double blinding”). Finally, the analysis should ideally be on an “intention-to-treat” basis, that is, the analysis should include all subjects, even those who did not adhere to the treatment. This is considered very important in studies of acute otitis media because there are often failures to follow the treatment correctly.
As already mentioned, a randomized clinical trial is not always the best study design. For studies investigating treatments, such as the management of acute otitis media, a randomized clinical trial will certainly yield the best evidence. However, a cross-sectional design is more appropriate for studies conducted to evaluate diagnostic tests, such as the determination of the sensitivity and specificity of computed tomography for intracranial complications of acute mastoiditis, for example. In turn, cohort studies may be the most appropriate design if the objective is to assess prognosis, such as the risk of delayed speech acquisition among individuals with otitis media with effusion. As such, the level of evidence does not necessarily prove that a study has a better design. However, as a general rule, when discussing treatments, a randomized clinical trial is considered the most appropriate strategy for assessing the therapeutic effects of a given intervention.
The measurement method is considered an important part of the methodology, especially in relation to otitis media. Standardization of the method is a fundamental element in guaranteeing the reproducibility of the results in other studies. Instruments for documenting otoscopy findings, audiometers, the collection of samples from the middle ear, and imaging exams are some examples of methods frequently used in research into otitis media. Similarly, the methodology for measuring subjective data such as otalgia and other symptoms should also be standardized, whether collected prospectively or retrospectively. For example, it is unacceptable for a study investigating otitis media to assess the degree of otalgia in a haphazard manner. The preferred method is to use a visual analog scale. It is also recommended that a single model of audiometer be employed and that it be duly calibrated.
In surgical studies, such as those of chronic otitis media, standardization of the intervention is very often difficult because neither the surgeons nor the pathologies encountered intraoperatively are uniform. For example, when assessing the surgical treatment of individuals with uncomplicated chronic otitis media, perforations of the tympanum may have different shapes, positions, and sizes. Along the same lines, cholesteatoma is highly variable in terms of the route of formation, its extent, and its aggressiveness. In the case of tympanic membrane retraction, variations can be even greater. As a result, it is very difficult to generalize the conclusions drawn from a limited sample of surgical interventions.
It is important that the methods section present the provenance of the research participants and the inclusion and exclusion criteria. For randomized clinical trials, it is recommended that a flow diagram be constructed to illustrate how individuals were selected and the methods used for randomization. Additionally, the methods used to blind the membership of the intervention and control groups should be covered. When possible, the sample size calculation should be included in the methods because a sample that is too small can lead to type II error, which occurs if a null hypothesis is not rejected despite being false in the population. The statistical analysis methods must also be fully described in the methods section.
Results
It is very important for clinicians to be able to interpret the results through an understanding of the basic concepts of descriptive and analytical statistics.
One important concept is how to differentiate between a statistically significant difference and a clinically relevant difference. We may observe a p-value of <0.05 but find that the difference between groups is small in percentage terms, that is, a large number of individuals would have to be treated to benefit a small number of them. The larger the sample size, the easier it is to attain significant p values with relatively small percentage differences. This is why research into otitis media often employs the number necessary to treat (NNT). This value shows how many people would have to be given a certain intervention to achieve an outcome for one person. This is an important public health strategy. For example, it has been estimated that it is necessary to prescribe 2500 antibiotic courses for acute otitis media to prevent one episode of acute mastoiditis [3]. This is why cases of acute mastoiditis continue to occur during treatment with antibiotics despite the routine use of antibiotics for acute otitis media.
Effect sizes based on NNT are highly relative. These analyses are dependent on the severity of the disease and the side effects of the treatment. In the case of otitis media, and specifically in relation to antibiotic therapy, there is an intense debate about the effects on the community caused by increased bacterial resistance. Often, the NNT may not be available in publications on otitis media; only relative measures of effect size, such as relative risk or odds ratio, are available, which are no help in determining the impact oftreatment on the population level. In such cases, the NNT can be calculated as the inverse of the absolute risk reduction (ARR), that is, the absolute difference in the occurrence of events between the treatment group and the control group.
It is also important that the results are presented well in tables and figures to facilitate understanding of the study findings. Figure legends should be clear.
Internal Validity
Internal validity is related to the measurement methodology and the appropriate analysis of results. In the case of studies of otitis media, audiometric and otoscopic analysis, for example, are often used. These instruments must be valid, precise, and reproducible.
Along the same lines, an appropriate design is crucial for a study to have internal validity. It is also essential that the statistical tests employed are compatible with the analysis proposed. Consideration should be given to whether observations are interrelated or independent samples, whether the objective is to compare groups or associate an outcome with one or more predictive variables, and to the measurement of continuous variables.
External Validity
Assuming that the study has internal validity, the next step is to determine whether the results can be generalized to the universe beyond the study. This is closely related to the sampling process and especially to the use of representative and broad samples. A sample considered representative starts with careful selection on the basis of appropriate inclusion and exclusion criteria. One example of this would be to analyze the efficacy of a new antibiotic for the treatment of acute otitis media using a sample in which 90% of subjects are institutionalized and have Down syndrome. In such a case, the results of the study would not be generalizable to the population. External validity is greatly compromised if the investigators choose their sample based on convenience or subjective judgments. Additionally, highly restrictive exclusion criteria impede adequate generalization of the results.
Precision is a very important aspect and is based on the number of observations, that is, on the sample size. A larger sample size can be associated with reduced variability in observations through increased precision. The result is to narrow the 95% confidence interval and increase our confidence in the results.
The discussion gives the author an opportunity to evaluate the results and relate them to published data. This section may present speculations about the study, limitations, and future directions for a given investigation. It is important that the conclusions be based on the objectives and results of the study. The references should be presented in an up-to-date manner and, preferably, cover what is most relevant in the area.
Studies with In Vivo Experiments
Much important research into otitis media comes from animal experimentation studies. As is the case for clinical studies, guidelines containing recommendations for the publication of experimental research also exist. The ARRIVE 2.0 guidelines [4] deal with the format of scientific articles describing studies with animals. To a certain extent, they stipulate that studies should be reported with sufficient data to contribute to existing knowledge, enabling readers and reviewers to analyze the study in an appropriate manner and assess its methodological rigor while enabling the reproduction of the methods and results.
These guidelines are considered important for any study in the life sciences involving live animals, from mammals to fish. The guidelines are divided into two blocks, with no hierarchy. They are considered useful both when writing a manuscript to guarantee that it contains all of the relevant information and when reviewing a manuscript to check that all of the relevant information is available for assessment of the study.
There is a minimum set of 10 items considered essential to be included in the manuscript. If these data are not provided, readers and reviewers will not be able to assess the reliability of the results.
-
(a)
Study design: When there are comparisons between groups, a control group should be included. If one is not used, this should be justified.
-
(b)
Sample size: The exact number of experimental units in each group and the total number in each experiment should be specified, in addition to the total number of animals used. It should also be demonstrated how the sample size was established using the sample size calculation.
-
(c)
Exclusion and inclusion criteria: It is recommended that any criteria used for including or excluding animals be described, especially if these criteria were defined a priori. For each experimental group, the reasons for exclusions and the exact value of n in each experimental group should be reported.
-
(d)
Randomization: If randomization was used, the method employed to generate the randomization sequence should be described. The strategy used to minimize potential confounding variables, such as animals’ locations in the animal house, should also be described.
-
(e)
Blinding: It is recommended that who was aware of the allocation of experimental units at different stages of the experiment be stated.
-
(f)
Outcomes: All outcomes assessed should be defined, and the primary outcome used to calculate the sample size should be specified.
-
(g)
Statistical methods: It is recommended that details be provided on the statistical methods used for each analysis, especially the software employed.
-
(h)
Experimental animals: Details should be provided of the species of animals used, including strain, substrain, age, and sex. Further information on the provenance of animals should be given and, if possible, health status and genotyping.
-
(i)
Experimental procedures: All procedures should be described in enough detail to allow reproducibility, including materials used, frequency, locations, and reasons.
-
(j)
Results: For each experiment, summary/descriptive statistics should be reported for each experimental group with a measure of variability where possible (mean, standard deviation, and median). The effect size and confidence interval should also be provided.
There is another list of items defined as the recommended set, including elements such as a precise abstract, a clear scientific background, a definition of objectives, an ethical statement, housing and husbandry conditions, care and monitoring of animals, interpretation and scientific implications, applicability and translation, protocol registration, free access to data, and a declaration of interests.
Randomized Clinical Trials
Treatment of otitis media has advanced greatly with the publication of large-scale randomized clinical trials over recent decades. We now have answers to the majority of questions about the treatment of acute otitis media and otitis media with effusion. For chronic otitis media, there is a growing effort to publish more clinical trials on which to base clinical and surgical decisions. However, we must be careful about the quality of randomized clinical trials that are being published. There is a checklist of the information that should be included in the publication that can be used to verify this, based on the CONSORT 2010 Statement [5]. As with ARRIVE 2.0, CONSORT considers that the results of a randomized clinical trial should enable readers to understand the study design, analysis, and interpretation. The checklist covers 25 items, the presentation of which is considered essential to the reliability of the results, especially in relation to the effects of a given treatment.
-
(a)
Title and abstract: It is recommended that the study title identify it as a randomized clinical trial. The abstract should cover the trial design, methods, results, and conclusions.
-
(b)
Introduction: This should include the scientific background and explanation of the rationale, specific objectives, and hypotheses.
-
(c)
Study design: Description of trial design, such as parallel, including allocation ratio. Additionally, important changes to methods after the clinical study’s outset, such as eligibility criteria, are explained.
-
(d)
Participants: The methods section should clearly define the eligibility criteria for participants, with information on the locations where the data were collected.
-
(e)
Interventions: The interventions for each group, with sufficient details to allow replication, including when they took place.
-
(f)
Outcomes: Primary and secondary outcomes were defined in advance, including how they were assessed. Any changes to outcomes after the clinical trial has commenced should also be stated.
-
(g)
Sample size: State how the sample size was determined and whether there were any trial-stopping guidelines.
-
(h)
Randomization sequence generation: Show the method used to generate the allocation randomization sequence. Types of randomization, such as simple or blocking.
-
(i)
Allocation: Mechanism employed to implement the random allocation sequence (such as sequentially numbered containers), describing the steps taken to conceal the sequence until interventions were assigned.
-
(j)
Implementation of allocation: State who generated the random allocation sequence, who enrolled participants, and who assigned participants to interventions.
-
(k)
Blinding: If done, who was blinded after the assignment to interventions, and how was this done?
-
(l)
Statistical methods: Describe the statistical methods used to compare groups for primary and secondary outcomes, as well as for subgroup analyses and adjusted analyses.
-
(m)
Participant flow: It is strongly recommended that a diagram be used. Show the numbers of participants who were randomly assigned, received the treatment assigned, and were analyzed for the primary outcome. For each group, show losses and exclusions after randomization with their respective reasons.
-
(n)
Recruitment: Define when participants were recruited and follow-up times. State the reasons for ending or stopping the trial.
-
(o)
Baseline data: Include a table showing baseline demographic and clinical characteristics for each group.
-
(p)
Numbers analyzed: For each group, the number of participants in each analysis with the denominator.
-
(q)
Outcomes and estimates: For each primary and secondary outcome, the results for each group and the estimated effect size and its respective precision (95% confidence interval). For binary outcomes, it is recommended that both absolute and relative effect sizes are presented.
-
(r)
Ancillary analyses: Subgroup analyses and adjusted analyses, distinguishing prespecified from exploratory.
-
(s)
Harms: All important harms or unintended effects in each group.
-
(t)
Limitations: Indicate trial limitations, including sources of potential bias and imprecision.
-
(u)
Generalization: Describe the external validity and applicability of the clinical trial findings.
-
(v)
Interpretation: Interpretation consistent with the results, with a balance of benefits and harms.
-
(w)
Registration: Registration number and name of the registered clinical trial.
-
(x)
Protocol: State where the full clinical trial protocol can be accessed.
-
(y)
Funding: State the sources of funding and other support, and the role of funders.
This CONSORT checklist enables the reader of a randomized clinical trial of otitis media to check that it meets all of the criteria recommended to consider it an appropriate publication to possibly influence clinical practice.
Systematic Reviews and Meta-Analyses
Systematic reviews and meta-analyses have been crucial in defining otitis media management practice. They are used as the starting point for developing instructions for clinical practices. Guidelines for the publication of systematic reviews and meta-analyses have been constructed based on the definitions used by the Cochrane Collaboration. A systematic review is a review of a clearly formulated question that employs systematic and explicit methods to identify, select, and critically evaluate relevant research and collect and analyze data from these studies, which are included in the review. Statistical methods (meta-analysis) may or may not be used to analyze and summarize the results of the studies included. Meta-analysis is the use of statistical techniques to integrate the results of the studies included in a systematic review.
An executive committee evaluated which items were crucial for systematic reviews and meta-analyses to be considered satisfactory, developing the PRISMA statement [6], which defines the following checklist:
-
(a)
Title: The title should identify the report as a systematic review, meta-analysis, or both.
-
(b)
Abstract: Should include a structured summary covering theoretical background, data sources, eligibility criteria, participants, interventions, study appraisal and synthesis methods, results, limitations, conclusions, and registration number.
-
(c)
Rationale: Describe the rationale for the review in the context of what is already known.
-
(d)
Objectives: Make an explicit statement of questions such as participants, interventions, comparisons, outcomes, and study design.
-
(e)
Protocol and registration: Indicate whether a review protocol exists that can be accessed and provide information about the registration of the review.
-
(f)
Eligibility criteria: Define characteristics of the study and the report, such as eligibility criteria with rationale.
-
(g)
Information sources: Describe all information sources used in the search (database, contact with authors) and the date of the most recent search.
-
(h)
Search: State the complete electronic search strategy, including limits, so it can be repeated.
-
(i)
Study selection: State the process for selecting studies, that is, the search for eligible studies.
-
(j)
Data collection process: Methods for extracting data from articles and processes for obtaining and confirming data from researchers.
-
(k)
List of data items: List all variables collected, with references or simplifications.
-
(l)
Risk of bias in each study: Describe the methods used to assess the risk of bias in each study and how this information was used in the analysis of the data.
-
(m)
Summary measures: Should define the principal measures for summarizing results.
-
(n)
Synthesis of results: Describe the methods for analyzing data and combining the results of studies with measures of consistency for each meta-analysis.
-
(o)
Risk of bias across studies: It is recommended that any assessment of the risk of bias that may affect the cumulative evidence, such as publication bias, be specified.
-
(p)
Additional analyses: All additional methods of analysis should be described, and those that were prespecified should be identified.
-
(q)
Study selection: The results should state the number of studies screened, assessed for eligibility, and included in the review.
-
(r)
Study characteristics: For each study, present characteristics for data extraction with their respective citations.
-
(s)
Risk of bias for each study and between studies: It is recommended that data on risk of bias for each study and outcome be presented in the results.
-
(t)
Results of individual studies: For each study and for all outcomes considered, present a simple summary of data for each intervention group and effect estimates and confidence intervals using forest plots.
-
(u)
Synthesis of results: Present results for each meta-analysis conducted, including confidence intervals and measures of consistency.
-
(v)
Additional analyses: Present additional analyses such as subgroup analyses and meta-regressions.
-
(w)
Summary of evidence: It is recommended that the main findings be summarized, especially the strength of evidence for each outcome and its relevance to key groups.
-
(x)
Limitations: Discuss limitations at the level of studies and outcomes and at the review level.
-
(y)
Conclusions: Give a general interpretation of the results and their relationship to other evidence. Similarly, state the implications for future research.
-
(z)
Funding: Declare sources of funding and the role of funders in the review.
Publications in the form of meta-analyses and systematic reviews are increasingly common in the area of otitis media. We therefore consider that it is important that readers are familiar with the PRISMA guidelines to enable them to use the checklist to critically appraise a meta-analysis or systematic review.
Observational Studies
The majority of studies of otitis media are observational, especially those conducted in the past. Such studies are essential to enable us to understand the many different clinical entities related to otitis media and enable developments in the area to be achieved through intervention studies. However, it is common for observational studies to be conducted inappropriately, making it less likely that correct extrapolation will be possible. An initiative known as Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) published a 22-item checklist named the STROBE Statement, containing recommendations on what should be included in a more precise and complete description of such studies [7].
-
(a)
Title and abstract: Indicate the study design in the title or abstract. Provide an informative and balanced summary in the abstract.
-
(b)
Rationale: Include in the introduction the theoretical background and the reasons for the research.
-
(c)
Objectives: State the specific objectives and hypotheses.
-
(d)
Study design: The methods should describe the key elements of the study design.
-
(e)
Setting: Describe the setting with locations and important dates, with periods of recruitment, exposure, follow-up, and data collection.
-
(f)
Participants: For cohort studies, present the eligibility criteria, sources, and methods of selection of participants and follow-up. For case-control studies, present the eligibility criteria and the sources and diagnostic criteria for the separation of cases from controls. For cross-sectional studies, present the eligibility criteria and the sources and methods of selection of participants. In cohort studies and paired case-control studies, criteria for pairing and the number of exposed and non-exposed participants should be given.
-
(g)
Variables: All outcomes should be clearly defined, with exposures, predictors, confounders, and effect modifiers. Diagnostic criteria likewise.
-
(h)
Data sources and measurement: For each variable, the source of data and details of assessment methods are described.
-
(i)
Bias: List all methods used to avoid potential sources of bias.
-
(j)
Study size: The sample size should be clearly defined.
-
(k)
Quantitative variables: It is recommended that the way that quantitative variables were treated and any categorizations used should be explained.
-
(l)
Statistical methods: It is recommended that all statistical methods and the control of confounding factors be described. Likewise, describes subgroup and interaction analyses, how missing data were dealt with, losses to follow-up in cohort studies, pairing of cases and controls, sampling strategies, and sensitivity analyses.
-
(m)
Participants: Number of participants in each stage and number who completed follow-up.
-
(n)
Descriptive data: Demographic characteristics of participants and information on exposures and confounders. State the number of participants with missing data for each variable. For cohort studies, it is essential to state the follow-up time.
-
(o)
Outcomes: Number of outcome events or summary measures over time for cohort studies. For case-control studies, the number of participants in each exposure category. For cross-sectional studies, the number of outcome events or summary measures.
-
(p)
Main results: Estimates unadjusted and, if necessary, adjusted for confounding variables. If continuous variables were categorized, state the cut-offs used. If possible, transform relative risk estimates into absolute risk.
-
(q)
Other analyses: Report on any analyses of subgroups that have been conducted.
-
(r)
Key results: In the discussion, it is recommended that the main findings be related to the study objectives.
-
(s)
Limitations: In the discussion, it is recommended that limitations be discussed, especially potential biases or imprecision.
-
(t)
Interpretation: The interpretation of results should be cautious, taking into account objectives, limitations, multiplicity of analyses, and results of similar studies.
-
(u)
Generalization: The external validity of the results should be discussed.
-
(v)
Funding: State sources of study funding and the role of funders.
Conclusions
The objective of this chapter was to present an organized strategy for conducting a critical analysis of a scientific publication, specifically for the otitis media area, in which there have been significant increases in both the quantity and quality of publications over recent years. Researchers and clinicians thus have the tools to independently form their own opinions on the scientific content they analyze and incorporate this knowledge into their practice when they consider it truly relevant.
References
Gelbach SH. Interpreting the medical literature. 4th ed. Norwalk: Appleton & Lange; 2002.
Consolidated Standards of Reporting Trials, Altman DG, et al. The revised CONSORT statement for reporting randomized trials. Ann Intern Med. 2001;134:663–94.
Kassirer JP, Campion EW. Peer review: crude and understudied, but indispensable. JAMA. 1994;287:259–60.
Percie du Sert N, Ahluwalia A, Alam S, et al. Reporting animal research: explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol. 2020;18(7):e3000411.
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med. 2007;45(4):247–51.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lavinsky, J., da Silva, V.A.R., Lavinsky, L. (2023). Critical Appraisal of Published Research in Otitis Media or How to Sort the Wheat from the Chaff!. In: Goycoolea, M.V., Selaimen da Costa, S., de Souza, C., Paparella, M.M. (eds) Textbook of Otitis Media. Springer, Cham. https://doi.org/10.1007/978-3-031-40949-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-031-40949-3_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-40948-6
Online ISBN: 978-3-031-40949-3
eBook Packages: MedicineMedicine (R0)