Abstract
One of the most effective global public health initiatives is vaccination. But despite the abundance of extremely effective vaccines, there are still some infectious diseases for which there are no vaccines. To fully realize the potential of vaccine development for both newly emerging infectious diseases and illnesses for which there are currently no vaccines available, new technologies are required. The COVID-19 mRNA vaccines’ success demonstrates that nanoscale platforms are promising delivery vectors for efficient and secure vaccines. The development of drugs is significantly influenced by nanotechnology. Polymeric nanoparticles can transport drugs, proteins, and vaccine antigens to the desired site of action. Through mucosal administration, polymeric nanoparticles with lower cytotoxicity can shield drugs or antigens from degradation in unfavorable conditions. In addition, the uptake of nanoparticles by antigen-presenting cells can boost and trigger powerful immune responses. Nanomaterials are also frequently used in vaccine delivery systems because they can extend the half-life of the vaccine antigen. Inorganic nanoparticles, polymer-based nanoparticles, nanomaterial vaccines, the idea behind nanomaterial-based vaccines, and applications of nanomaterial-based vaccines in healthcare are the main topics of this review. In the context of drugs and vaccines, the use and potential of nano bases as delivery vehicles and adjuvants are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Few preventive health initiatives are as successful as vaccine development. Active acquired immunity to a specific disease is provided by vaccines, which are biological preparations. Vaccines come in a wide range of forms, such as attenuated, inactivated, DNA, vector, live, and toxoid vaccines (Li et al., 2016). In the past two decades, vaccines based on nanomaterials have emerged as an innovative vaccination strategy (Butkovich et al., 2021). It has been shown that nanomaterials as vaccine carriers or delivery vehicles have significant adjuvant effects than solid particles with diameters ranging from 1 to 1000 nanometers (Sun & Xia, 2016). Infectious diseases, including viral, bacterial, parasitic, and cancer, have been controlled by effective vaccines. Developing next-generation vaccines requires the development of adjuvants and delivery systems that can be applied to next-generation molecules (O’Hagan & Valiante, 2003). As vaccine use enters the fourth century, it faces numerous challenges in protecting against many complex infectious diseases (Harandi et al., 2010). Due to the problems associated with conventional vaccines, new delivery systems and adjuvants have been developed to address those issues (Rice-Ficht et al., 2010). It has been reported that polymer particles have elicited the most protective immune response among all the delivery systems developed so far (Look M et al., 2010).
Polymer particle-based delivery systems have primarily been investigated for developing single-dose vaccines for various diseases. However, as nanotechnology has advanced, the scope and application of vaccine development have expanded significantly. One of the major applications of nanomaterials is drug, vaccine, and therapeutic delivery, where systems such as nanoemulsion, liposomes, nanoparticles, polymer micelles, dendrimers, and others provide higher therapeutic indices. Using a nanomaterial-based particulate system to entrap a candidate vaccine, an adjuvant/immunomodulator and a dendritic cell activator provide an enormous opportunity for vaccine development (Draper & Heeney, 2010). The development of a universal vaccine is challenging since it does not utilize live pathogens to induce sustained immune responses. A biodegradable nanoparticle that mimics a virus’ structure and function but is not contagious and does not reproduce might serve this need (Basu et al., 2018).
1.2 Role of Nanoparticles as Adjuvants in Vaccines
1.2.1 Nanoparticles in Vaccine
Vaccine development is increasingly relying on nanotechnology. Formulations that increase antigen effectiveness are required more and more as vaccine development shifts toward “minimalist” compositions that are less immunogenic. Improved immunogenicity and antigen stability are made possible by the use of nanoparticles in vaccine formulations, along with targeted delivery and slow release. There are many different types of nanoparticle vaccines that have been approved for use in humans, and the number of candidates is growing. It is fundamentally important to understand how nanoparticles behave in vivo, whether they are used as delivery systems for antigens or as immunostimulant adjuvants to enhance immunity. In-depth summaries of recent advances in preventative nanovaccinology are provided in this review. Various types of nanoparticles that are used are described, along with how they interact with immune cells and the biosystem. Developing rational vaccines containing nanoparticles will be more effective when we know more about nanoparticle mechanisms of action both in immunostimulatory and delivery modes, and also how nanoparticles distribute and behave in vivo (Zhao et al., 2014).
1.2.1.1 Nanoparticles as Adjuvants in Vaccines
An excellent foundation for creating a new generation of vaccines is provided by nanotechnology, which are based on nucleic acids, proteins, and synthetic peptides made from recombinant DNA, polysaccharides, or purified subunit proteins. These vaccines might not be sufficiently immunogenic, so adjuvants that boost their immunogenicity are necessary. An adjuvant (NA) is a nanoparticle (NP) that can act as an adjuvant for a vaccine (NA). In a suitable formulation, vaccine antigen or DNA can be encapsulated or adsorbed by nanoparticles, enhancing stability, cellular uptake, and immunogenicity. Different NA formulations can also be used to regulate a vaccine’s biodistribution and systemic release (Garg & Dewangan, 2020).
1.2.2 Role of Metallic Nanoparticle
For subunit vaccines, the adjuvant choice is crucial for boosting immunogenicity, directing innate immunity stimulation, and creating the proper protective response to fight the target microorganism. Adjuvants can be immunomodulatory molecules, particulate formulations, or a combination of the two. A number of ways in which they may function include reducing the vaccine dose, enhancing the immune response, or extending the immune response, as well as providing a variety of immune responses, including humoral and cellular responses. Of the seven vaccine adjuvants that have been approved for use in humans, three are categorized as particulate formulations: aluminum salts (alum), extended immune response emulsions (like MF59), and virosomes. Alum increases antibody production as well as T-helper 1 (Th1) and Th2 responses, while the other two can also stimulate these responses. A TLR4 agonist, monophosphoryl lipid A, was combined with immunomodulatory molecules in AS 01 and 04, along with a particulate formulation of this molecule. As01 combined saponin (QS-21) with liposomes to favor Th1 responses, whereas ASo4 contained alum to enhance humoral responses. As agonists of TLR7 and TLR8, imidazoquinolines, as well as lipid A analogs, can trigger a Th1 response through their immunomodulatory effects (Marques et al., 2017).
-
1.
Vaccines serve as essential triggers for activating both the innate and adaptive defenses of the body, enabling a robust response against infections. As a result, vaccines emerge as highly valuable and effective tools in promoting public health. By harnessing the power of vaccination, we can enhance the body’s natural ability to combat diseases and significantly reduce their impact on communities, thereby safeguarding the well-being of the population. With increased knowledge about cancer and how it affects the immune system, the goal of activating host immune defenses to provide a targeted and comprehensive antitumor response is becoming more important. It is promising to use nanoparticle systems as vaccines to deliver antigens efficiently and as adjuvants to enhance immune responses (Wen et al., 2019).
-
2.
Mucosal tract pathogenic infiltrations cause most infectious diseases. There is extensive research underway on vaccinations to prevent a number of diseases, including infectious diseases, infertility, immune disorders, cancer, and allergies. It has been investigated how to stimulate the immune system more effectively against particular antigens using broad-spectrum adjuvant substances. Adjuvants have been developed that are inorganic, emulsion-based, oil-based, and bacterial-derived, both with cytosine-guanine dinucleotide motifs and with cytokines. Delivery of vaccines through the mucosa is an alternative to trigger cellular and humoral immune reactions. Antigen stability and immunogenicity can be increased, and targeted delivery and concentration of antigens are enhanced when nanoparticles are incorporated into vaccine formulations. Chitosan nanoparticles have mucoadhesive and immunologically active characteristics. Many antigens have served as a mucosal vaccine delivery system (Mehrabi et al., 2018).
-
3.
There is a need for improvements in traditional vaccines due to their low immunogenicity, toxicity, instability, and multiple vaccination administration requirements. Recently, nanotechnology has been incorporated into vaccine development to address the aforementioned issues. The development of vaccines using nanocarrier-based delivery systems, which provide a chance to boost cellular and humoral immune responses, is becoming increasingly dependent on nanotechnology. Nanoparticles enable targeted delivery, slow release, and improved immunogenicity and antigen stability in vaccine formulations. Polymeric, inorganic nanoparticles, ISCOMs, virus-like particles, liposomes, and emulsions are examples of nanoscale-size materials that have drawn attention as potential vaccine antigen delivery systems because they can both stabilize vaccine antigens and function as adjuvants. This benefit is due to the nanoscale particle size, which makes it easier for antigen-presenting cells (APCs) to absorb the material, resulting in effective antigen recognition and presentation. By adding various targeting moieties to the surfaces of nanoparticles, it is possible to deliver antigens to particular cell surface receptors, inducing specialized immune responses (Kheirollahpour et al., 2020).
1.2.3 Carbohydrates Containing Nanoparticles as Vaccines
Vaccine adjuvants are necessary for immunopotentiation, which induces the production of protective immunity. Unfortunately, traditional aluminum-based adjuvants are only capable of stimulating limited cellular responses. Developing vaccines against emerging pathogens requires adjuvants with better profiles in order to be effective. A greater balance of humoral and cellular immune responses can be stimulated by carbohydrate-containing nanoparticles (NPs) with immunomodulatory activity. We looked at a number of carbohydrates that have immunomodulatory effects. They include mannan, saponins, glucan, chitosan, and others that have been incorporated into vaccine formulations. These carbohydrate-containing NPs’ mode of action, preparation techniques, characterization, and associated vaccines are presented. Numerous NPs that contain carbohydrates have either reached the clinical stage or have been included in approved human vaccines. A vaccine against the pathogen responsible for the global pandemic, SARS-CoV-2, is being tested that contains saponin. Preclinical research and late-stage clinical trials are both stages of the development process for vaccines containing NPs that contain carbohydrates. The development of next-generation vaccines against cancer and infectious diseases may benefit from understanding the mechanism of action of carbohydrate-containing nanoparticles as carriers and immunostimulants (Smith et al., 2015).
1.2.4 Polymer-Based Nanoparticles
Polymer-based nanoparticles are solubilized, stable, safe, and have a sustained release, they are able to enhance drug absorption, protect them from deterioration, so that they can travel through the body for a longer period of time, and can increase targeted drug delivery. Vaccination is the best method of preventing and managing infectious diseases. There are several drawbacks to vaccines, including immunity tolerance, low immunogenicity, low expression levels, and the induction of pathological changes in respiration, including live attenuated vaccines, inactivated vaccines, protein subunit vaccines, recombinant subunit vaccines, and synthetic peptide vaccines. The antigens of vaccines are released more slowly through the use of biodegradable natural and synthetic polymers. Furthermore, these polymers enhance vaccine immunogenicity as well as act as adjuvants (Guo et al., 2019).
1.2.5 Nanomaterial Vaccines
As engineering devices have been modified to deliver drugs to and interact with cell environments, nanomedicines have gained increasing interest from the medical community in recent years (Shah et al., 2015). A wide variety of biodegradable materials, including cholesterol, phosphatidylserine, and other lipids, have been used to manufacture nanoparticles (NP) in addition to natural and synthetic polymers (PLGA) and metals (gold, copper oxide, silver, zinc oxide, and aluminum oxide) (Pati et al., 2018).
It is widely accepted that nanoparticles (NPs) and microparticles (MPs) are useful methods for delivering drugs, especially cytotoxic drugs or immunosuppressing treatments for organ transplants. Drug delivery is controlled using these NPs as they target specific organs to distribute medications. In transporting drugs to cancerous sites or other diseased organs, these carriers protect drugs from degradation (He et al., 2011). Metal nanoparticles themselves may work as carriers and targets for the delivery of tumor-associated markers since they are incorporated into the membranes of cancer cells. The outer layer of PLGA nanoparticles was coated with membranes derived from mouse melanoma cancer cells, according to Fang et al. 2014. In response to these molecules, cellular endocytosis caused dendritic cells to mature, presenting a special presentation to T cells with TCRs that bind to gp100 and produce IFN-γ.
A second finding was that PLGA-covered membranes were equipped with receptors for interacting with cancer cells and allowing drugs to be delivered (Fan et al., 2019). To prevent the rejection of organs, drugs were delivered through the NPs to the transplant site. The use of immunosuppressive agents in high doses is harmful to organ transplant recipients, as it can lead to infection and even death. Researchers have previously established that rapamycin MPs prevent islet rejection in vivo in diabetic mice with islets transplanted into the eye. Islets transplanted into immunosuppressive drug MPs survived for more than a month, while islets transplanted into a control group (empty MPs) were rejected after the second week (Sridhar et al., 2015). We have gained a greater understanding of infectious diseases and immune evasion mechanisms in the past few decades. Designing new vaccines and adjuvants to combat antibiotic-resistant pathogenic microorganisms is becoming increasingly challenging. It is currently possible to develop vaccines from live-attenuated microorganisms or killed pathogens (first-generation vaccines) (Lugade et al., 2013). In the third generation, there are DNA vaccines (Levine & Sztein, 2004), subunit vaccines (Levine & Sztein, 2004), and synthetic peptides (second-generation vaccines). In addition to these three vaccine types, an adequate adjuvant or delivery system is required to eliminate the risk of developing the disease (Eidi et al., 2010).
There should be no strict storage requirements for the vaccine and adjuvant combined, and it should induce long-lasting memory B and T cell responses (Levine & Sztein, 2004). The vaccine should be safe, stable, and able to induce memory B and T cell responses. The last three vaccine types must be combined with an adequate adjuvant or delivery system to eliminate the risk of developing the disease (Eidi et al., 2010). Recombinant proteins or DNA from another vector are needed to boost DNA and RNA vaccines. Some studies have demonstrated that nanoparticles improve vaccine efficacy by slowing antigen release, allowing for easy antigen uptake, and inducing humoral and cellular responses (Lugade et al., 2013).
1.2.5.1 Concept of Nanomaterial-Based Vaccines
One of the best methods for triggering immune responses that protect against infectious diseases is vaccination (Whitney et al., 2001; Pulendran 2006). Vaccination has prevented millions of deaths since Edward Jenner used cowpox materials to treat smallpox in 1796. It has virtually eradicated poliomyelitis and smallpox and significantly reduced the prevalence of diseases like hepatitis A, hepatitis B, diphtheria, tetanus, pertussis, measles, and others (Rappuoli et al., 2011). Additionally, vaccinations can ward off conditions that can result in cancer. In terms of preventing infections, chronic disease, and liver cancer, the hepatitis B vaccine has a 95% success rate. A vaccine for human papillomavirus (HPV) that prevents HPV-related vulvar cancer, vaginal cancer, and cervical cancer can prevent 50% of these diseases. Gardasil is effective against two varieties of HPV. To achieve optimum and long-lasting immunogenicity, vaccines need protective antigens and adjuvants (Wegmann et al., 2012). Vaxjo, a website that houses vaccine adjuvants and their uses in vaccine development, reports the use of 93 vaccine adjuvants in 379 vaccines designed to combat 78 pathogens, cancers, and allergies (Sayers et al., 2012). Adjuvants for vaccines are only approved for use in humans in a limited number of cases. A total of four adjuvants have been approved by the U.S. Food and Drug Administration (FDA), including aluminum salts, AS03, AS04, and MF59. Whether they enhance innate or adaptive immune responses or improve antigen delivery to the immune system, nanomaterials act as adjuvants (Smith et al., 2013). To elicit robust immune responses, researchers have developed different ENM-based adjuvants. Alum-based vaccine adjuvants have been used for many years in vaccinations for hepatitis A and B, human papillomavirus, pneumococcal disease, and DTaP (Diphtheria, Tetanus, and Acellular Pertussis) (Baylor et al., 2002). In addition to aluminum hydroxide (Alhydrogel), aluminum phosphate (Adju-Phos), aluminum potassium sulfate (Alum), and aluminum hydroxy phosphate sulfate (AHSA), some commercial sources offer aluminum and magnesium hydroxide mixtures (Inject Alum) (Baylor et al., 2002).
These aluminum salts that are offered for sale have various physicochemical characteristics. In-depth research is being done on gold nanoparticles (AuNPs) with controlled physicochemical properties for use in biology and medicine (H. Sawa et al., 2013). Silver nanoparticles are widely used in commercial products due to their special antimicrobial properties, and more than 30% of consumer products based on nanomaterials contain nano-silver (Niikura et al., 2013). It is important to get vaccinated against infectious diseases and conditions that may lead to cancer in order to prevent these diseases and conditions. It is common for vaccine formulations to include adjuvants because many recombinant and synthetic antigens are not immunogenic, improve immune response, and reduce antigen requirement for protective immunity. More than 400 vaccines are either in development or commercially available, employing over 100 different types of adjuvants. In addition to nanomaterial-based vaccines that enhance immunity caused by different antigens, there are many vaccines under development or on the market today. A better understanding of the molecular mechanisms is required, however, in order to ensure safety (Sun et al., 2016).
1.2.5.2 Current Market Scenario of Nanomaterial-Based Vaccines
A potential strategy for creating efficient and secure vaccinations against a variety of infectious illnesses is the use of nanomaterials. Due to the rising incidence of infectious diseases, the demand for targeted drug delivery systems, and the expansion of research and development efforts in the field of nanotechnology, it is anticipated that the global market for nanomaterial-based vaccines will experience significant growth in the upcoming years. The COVID-19 pandemic has also sped up the development and usage of vaccines based on nanomaterials, with a number of candidates now in clinical studies or authorized for use in an emergency. Nevertheless, in the near future, market expansion can be hampered by the high cost of production, regulatory obstacles, and the lack of knowledge and infrastructure in developing nations (Datta & Mandal, 2020).
Nanotechnology is used in vaccinations made of nanomaterials to increase their effectiveness. There are currently just a few vaccines in clinical trials, and the market for vaccines based on nanomaterials is still in its infancy. Yet, given the potential benefits of these vaccines, including enhanced stability, tailored distribution, and greater immunogenicity, there is a rising interest in this subject. As the need for safe and efficient immunizations increases, it is projected that the market for vaccines based on nanomaterials would expand fast in the future years (Bachmann & Jennings, 2019).
There were a number of nano material-based vaccines being developed, some of which were for COVID-19 and some of which had previously received emergency use authorization, but their market performance and effect were still in the early stages and were still being studied (Pardi et al., 2018).
The pharmaceutical industry’s field of nanomaterial-based vaccine research was one that was expanding quickly. These vaccines include nanotechnology to increase their potency and the antigens’ ability to reach the immune system, potentially enhancing vaccination effectiveness and lowering adverse effects. There were several nanomaterial-based vaccinations for infectious illnesses such as COVID-19, influenza, and cancer that were in various phases of clinical studies. Yet, regulatory clearance and consumer and healthcare professional acceptability might be determining factors in their commercial availability and market penetration (Dadu et al., 2021).
1.2.6 Inorganic Nanoparticles
There have been studies on the delivery of vaccines using silica, carbon, and gold, and these are biocompatible inorganic NPs (Wang et al., 2011). There are various forms, sizes, and surface modifications that can be used to synthesize these nanoparticles. It has been demonstrated that inorganic nanoparticles can successfully deliver viral antigens. Proteolytic enzymes couldn’t prematurely digest antigens this way. When influenza, immunodeficiency virus, foot and mouth disease, and TB antigens were delivered with gold nanoparticles, a robust immune response was induced in mice (Villa et al., 2011). In mice infected with Mycobacterium tuberculosis, the causative agent of human tuberculosis, gold nanoparticles encapsulating plasmid DNA encoding the hsp65 antigen reduced the burden of the bacterium by a significant amount (Silva et al., 2005). As adjuvants for enhancing immunogenicity and antigen delivery, hollow mesoporous silica, nanotubes, and spherical carbon nanoparticles have been used in many studies (Kawano et al., 2013). A significant amount of silanol groups can be introduced on the surfaces of silica-derived nanoparticles to provide access to the target cells for vaccine molecules (He et al., 2003). Inorganic nanoparticles have the advantages of being low-cost, reproducible, and safe.
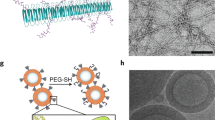
1.2.6.1 Liposomes
Among the nanomedicine delivery vehicles, liposomes are the second most widely tested after polymeric nanoparticles. It is through liposome fusion that vaccines are delivered to target cells. Both hydrophilic and hydrophobic substances can be encapsulated by structurally flexible liposomes. An aqueous core can accommodate hydrophilic molecules, while phospholipid bilayers enclose hydrophobic molecules. Multilamellar lipid vesicles have previously been shown to elicit strong T- and B-cell responses when they transport antigenic proteins (Moon et al., 2011). APCs readily internalized phosphatidylserine liposomes containing antigenic peptides to potentiate T-helper cell-mediated immunity (Ichihashi et al., 2013). Vaccine DNA encoding heat shock proteins delivered using liposomes induced strong protection against fungal infections (Ribeiro et al., 2013). Clinical trials of liposome-based vaccine nano-formulations against intracellular pathogens have been approved as a result of their expected applications, including viruses and M. tuberculosis (Watson et al., 2012). The effectiveness of liposomal aerosol carriers has already been demonstrated for the generation of protective immunity against Mycobacterium tuberculosis infection (Vyas et al., 2005). DDA-lipid liposomes and various immunomodulators have also been used in other studies to boost immunity against influenza and chlamydia (Alving et al., 2016). The delivery of lipid-DNA complexes to monkey lungs has been successful in the context of DNA vaccines.
1.2.6.2 VLPs (Virus-Like Particles)
VLPs have been demonstrated to be capable of serving as vaccine carriers and stimulating host immune responses in several studies. An immunologically active VLP consists of an epitope-rich monomeric complex viral membrane that self-assembles (Grgacic & Anderson, 2006). Fusing proteins with the particles can also enable VLPs to endogenously express multiple antigens, as well as express additional proteins. The surface of VLPs can also be chemically conjugated to produce bioconjugates with nonprotein antigens (Patel & Swartz, 2011). This distinguishing feature of VLPs enables them to provide both virus and antigen protection (Grgacic & Anderson, 2006). When SV40 virus capsid protein is delivered to mammalian cells, a specific immune response is induced (Kawano et al., 2013). The immunogenicity of weak antigens was also increased by VLPs. Salmonella typhi membrane antigens, the influenza A M2 protein, and GnRH-assembled VLPs from H1N1 Nef all evoked antigen-specific humoral and cellular immune responses (Gao et al., 2018). According to some theories, VLP-based nanoformulations can help antigens to produce conformations that are similar to those of native antigens, thus stimulating the immune system more effectively (Gao et al., 2018).
1.2.6.3 Dendrimers
Benzene amines and amides are the essential ingredients in dendrimers, which are three-dimensional, monodisperse, and hyperbranched nanostructures. Dendrimers have been used to deliver antigenic molecules in a few studies. PPI and PAMAM dendrimers are two of the most widely used dendrimers for vaccine delivery. It was found that dendrimers encapsulating multiple antigens produced well-trained antibodies and T cells against the Ebola virus, H1N1 influenza, and Toxoplasma gondii (Chahal et al., 2016). Dendrimers are efficiently absorbed by the host cells, generating robust immune responses. In a similar study, increased cellular uptake of PMAM dendrimers led to significant improvements in HIV transactivator of transcription (TAT)-based DNA vaccine efficacy (Bahadoran et al., 2016). Dendrimers have proven to be a promising candidate for developing new-generation vaccines with enhanced immunogenic properties because they can be tailored to achieve specific biological and physicochemical properties and are capable of conjugating multiple ligands into one molecule.
1.3 Applications of Nanomaterials-Based Vaccines in Healthcare
-
(a)
Viral Diseases
Before a vaccine is approved for production and marketing, it must undergo several preclinical and clinical testing stages. An infectious agent is screened for immunogenic antigens at the beginning of the vaccine development process, which stimulates an immune response in the host. Once clinical studies have been reviewed by the regulator, the developer will be allowed to begin clinical trials if the potential benefits of the new vaccine outweigh the risks of toxic or unpleasant side effects (Kim et al., 2020). Three phases of clinical trials are used to evaluate the effects of vaccines currently being developed on human subjects. The effects of vaccines currently being developed on human subjects are examined in three phases throughout clinical trials.
Phase 1 of vaccine development involves testing the vaccine on a small group of healthy adult volunteers to evaluate the induced immune response and address any safety concerns. The phase 2 trials begin with a pilot efficacy study, which confirms safety. Potential vaccines will be enrolled in phase 3 clinical trials if they demonstrate efficacy and low toxicity risks. As part of phase 3 trials, a wider number of people from a wide range of populations are involved to confirm the safety, efficacy, and dose levels of the vaccine in these groups. Tens of thousands of volunteers are often recruited from regions where viral transmission is prevalent. The higher the rate, the older the age. This includes individuals over the age of 18, as well as those suffering from underlying health issues. Phase 3 vaccines that are effective can apply to regulatory agencies for marketing approval before being produced in large quantities and marketed. Phase 4 of pharmacovigilance, during which the vaccine product is continuously and carefully monitored for safety and efficacy, will begin after marketing authorization is granted (Shin et al., 2020). It is possible to develop a vaccine under an emergency use authorization (EUA) to make it available for mass vaccination in emergencies and pandemics like the current COVID-19, even if a clinical trial is still ongoing (Kuwentrai et al., 2020). Almost 320 SARS-CoV-2 vaccine products are currently in development, with about 126 undergoing clinical trials and 194 undergoing preclinical testing (Chen et al., 2019). Only eight candidates, though, have entered phase 4 clinical trials. Because more candidates must be developed and marketed before being evaluated in real-world situations and for population-wide effects (Boopathy et al., 2019), out of these eight, only Pfizer-BNT162b2 BioNTech’s and Moderna’s mRNA-1273 are nonviral vector nanocarriers that rely on LNPs.
Despite the drawbacks of traditional vaccines, such as time-consuming manufacturing, very few fully approved vaccines against viruses are developed and delivered using advanced biomaterials or nonviral nanocarriers. Process, toxicity, and over infection are ongoing concerns (Tebas et al., 2021), especially the prophylactic HPV vaccines, virosomes, and VLP systems, as well as the HAV, HBV, and influenza vaccines in the past (Petkar et al., 2021). As an alternative, Shingrix®, which contains a liposomal carrier that delivers the viral antigen cargo, is authorized for clinical use by GlaxoSmithKline, a manufacturer of nano vaccines (Petkar et al., 2021). Therefore, developing clinically approved nano vaccines that meet regulators’ strict quality, safety, and efficacy requirements still requires much work. SARS-CoV-2 vaccines based on LNPs, which are undergoing phase 4 clinical evaluation, have made it possible to develop additional nano vaccines using cutting-edge nanotechnological methods (Gutjahr et al., 2016). BNT162b2 and mRNA-1273 contain nucleoside-modified mRNA encoding SARS-CoV-2 spike (S) glycoproteins. As a result of these vaccines, SARS-CoV-2 was protected from infection by both humoral and cell-mediated responses. It is the stability of Pfizer-BioNTech and Moderna vaccines that makes them the most difficult to store at temperatures below 80 to 60 °C or 50 to 15 °C. It is only possible to freeze the Pfizer-BioNTech vaccine for two weeks at 25 to 15 °C, which necessitates specialized transportation and storage equipment (Sulczewski et al., 2018).
-
(b)
Bacterial Diseases
As a result of the global pandemic caused by SARS-CoV-2, antiviral defenses are urgently needed. Public health measures such as vaccination are effective. There is evidence that these vaccines are effective against specific species of Mycobacterium, Burkholderia, Listeria monocytogenes, Chlamydia trachomatis, Borrelia burgdorferi, Brucella abortus, and Shigella flexneri, but not against other species of bacteria (Palmer et al., 2016). During their invasion and persistence inside host cells, intracellular bacterial pathogens create a blockage to the development of defense mechanisms, which explains their success. It is common for bacteria to take advantage of nutrients, environments, locomotion potential, or other properties of host cells by exploiting antigen-presenting cells (APCs) or epithelial stromal cells. Antigenic variation, the release of immunomodulators, or the suppression of immune responses are some of the tactics bacteria can employ to evade detection inside the host cell (Chai et al., 2020). Thus, bacterial invasion of the host cell creates a safe environment that enables some bacteria to develop long-lasting or persistent and hard-to-treat infections (Thakur et al., 2019). There are multiple strains of bacteria that are drug-resistant, which complicates treatment and contribute to ongoing transmission. Despite the fact that these bacterial infections can sometimes be treated with antibiotics, new classes of antibiotics are slow to reach the clinic.
Subunit vaccines and attenuated or inactivated organisms are used in conventional vaccination methods. Live attenuated vaccines, such as the oral typhoid vaccine and Mycobacterium bovis bacillus Calmette-Guarin (BCG), may be dangerous in susceptible populations (such as the immunocompromised) (Acosta et al., 2005; Hanley, 2011). However, inactivated organisms are usually at low risk of losing their immunogenicity due to the inactivation process. Subunit vaccines are significantly less dangerous than live attenuated vaccines, but they must also be administered with adjuvants because of their low immunogenicity. In developing vaccines, the challenge is to maintain safety while delivering potent cell-mediated and humoral responses (González-Miró et al., 2018).
-
(c)
Parasitic Diseases
TBV targets the sexual stages of malaria transmission and is the ideal intervention to lessen the disease’s impact by preventing the vector-mediated spread and eventually eradicating the parasite from the population in endemic areas (Ariey et al., 2014). The parasite development inside the mosquitoes is hampered by immune reactions to sexual-stage antigens, which reduces transmission. Pfs230, Pfs48/45, and Pfs25 are three of the primary target antigens for TBVs, and their orthologs exist in P. vivax. Pfs25, which is expressed on the surface of zygotes and ookinetes, is one of the most promising targets for TBV development. Clinical trials in phase 1 and preclinical models have been conducted on the drug (Nunes et al., 2014). Recombinant Pfs25 expression in yeast and cell-free translation using wheat germ, plants, and algae has all been reported in some studies with varying degrees of transmission-blocking efficacy in preclinical studies and phase 1 clinical trials has been reported (Kumar et al., 2014). Generating Pfs25 in its native form in any heterologous expression system has been difficult due to its complex tertiary structure, which is characterized by 22 conserved cysteine residues important for the structural integrity of the antigen (Kumar et al., 2013). An antigen formulation must trigger potent and, ideally, long-lasting antibody responses to be a successful vaccine. Effective adjuvants are incorporated, delivery methods are optimized, and particulate vaccine size is adjusted to modulate immune responses (Jones et al., 2013). Since there are no reliable adjuvants or delivery mechanisms, vaccine development has been generally difficult. Nanoparticles can be used to deliver antigens faster, resulting in a better immune response than soluble antigens (Reed et al., 2013). This is because gold nano (GN)-particles can be molded into various particle shapes and sizes, are biocompatible, and have unique physicochemical properties (Rana et al., 2012). Dendritic cells and other antigen-presenting cells can easily take up GN particles because they are nontoxic and can enhance vaccine antigen delivery. Few studies have reported GN particles’ ability to deliver vaccine antigens, despite their enormous potential in biomedical imaging and diagnostics (Arnáiz et al., 2012).
-
(d)
Cancer Diseases
Cancer, a major public health concern, is now seriously threatened by people’s safety and health. In addition to vaccination, vaccines have also been found effective in treating cancer to reduce the risk of contracting infectious diseases. Vaccines that are known as cancer vaccines prevent both infections with cancer-causing viruses and prevent cancer from developing known as prophylactic vaccines) and treat cancer that has already developed known as therapeutic cancer vaccines (Bolhassani et al., 2011). In 2010, sipuleucel-T (Provenge), the first therapeutic cancer vaccine, received US approval to treat prostate cancer (Melief et al., 2015). Recent clinical findings suggest that cancer vaccines can improve overall survival and reduce cancer recurrence. Therefore, the clinical value of therapeutic cancer vaccines has been proven. Various methods are used in cancer vaccination to produce, enhance, or skew antitumor immunity (or a combination of these) (Jia et al., 2017). Creating more effective cancer vaccines requires a thorough understanding of how they work. Cancer vaccines are exposed to APCs when administered intradermally, subcutaneously, or intramuscularly. Vaccine antigens are presented on MHC class I or II by APCs after they have ingested the vaccine.
APCs enter the lymph nodes via the afferent lymph, prime, and activate T cells. The activated effector T cells recognize the cancer cells in the tumor bed as they move through the efferent lymph and into the blood (Chen & Mellman, 2013). Among the various cell types that can serve as APCs, dendritic cells (DCs), B cells, and macrophages are the most effective (Schlom, 2012). Two main pathways are thought to be involved in DCs’ mediation of antigen presentation. In the first pathway, proteasomes in the cytosol of DCs break down endogenous antigenic proteins. CD8+ cytotoxic T lymphocytes (CTLs), the primary immunosuppressive cells that kill tumors, are stimulated by MHC-I molecules and their peptide fragments (Gordon et al., 2014). On the other hand, exogenous antigenic proteins are taken up by DCs via endocytosis and degraded by lysosomes after they’ve been tinged with endosomes. The peptide fragments present in MHC-II molecules activate CD4 T lymphocytes, allowing lymphocytes to become activated, function, and survive (Alloatti et al., 2016). As such, CD4+ T cells and CTLs must be activated in order to effectively administer cancer vaccines for antitumor immunotherapy.
1.4 Challenges in the Development of Nano-Based Vaccines
Vaccination is an effective solution in fighting infectious diseases by activating immune responses for more than 200 years; however, the advancement in immunology and molecular biology demands improvement regarding the adjuvant and immunostimulant properties of vaccines. The use of nanotechnology in vaccine development provides numerous benefits over conventional vaccines (Panda, 2012a). Nano-based vaccines are the modern generation of vaccines developed by using nanoparticles as a carrier or adjuvants which have multiple benefits including improved immunogenicity, lower dosing frequency, optimum size, stability of vaccine, excellent presentation of antigen with the loading of antigen in an optimum way (Yin et al., 2022). Undoubtedly, the use of nanocarrier-based vaccines is a quite effective tool to combat infectious diseases.
This safety risk is probably the main public concern regarding nano-based vaccines. The application history of the nanoparticles with short history produces some serious concerns about long-lasting safety profiles. The prolonged exposure of inorganic nanoparticles might cause inherent toxicity while it can also cause cytotoxicity in dose-dependent manner. The biocompatibility and biodegradability profiles of nanoparticles are also important for the development of future vaccines. The scaling-up process after manufacturing is another barrier to nanovaccine development. The nanoparticles can cause unexpected immune responses after biodegradation due to varying physicochemical properties of these particles after manufacturing. Lack of guidelines regarding nanoparticle production can cause certain degrees of ambiguity for developers. The elevated production cost of nanoparticles, such as liposomes, along with various other drawbacks associated with these particles, may hinder the progress of vaccine development (Vincken et al., 2007).
The unforeseen safety risks can be compensated through the use of nanotechnology that requires good considerate of the nanoparticle’s effects on immune response (Azharuddin et al., 2022). Vaccines could potentially face various types of vaccine-dependent problems and challenges including storage, administration, manufacturing, administration, acceptability, ethical considerations, and adverse reactions (Helmy et al., 2022).
The commercialization of the nano-based vaccine, cost of production, and increased complexity are also significant challenges in vaccine development. While the toxicity, lack of regulatory framework, and scaling-up process are even more important limiting factors for nanovaccine development (Bhardwaj et al., 2020).
Furthermore, lack of safety testing and analytical procedures for nano-based vaccine development regarding various compositions are to be focused for future considerations (Azharuddin et al., 2022).
1.5 Future Perspectives
Nano-based vaccines have many advantages over traditional vaccines including adjuvancity, controlled release of antigen, antigenicity, efficiency, dose regimes, nanoparticles variety, biodegradability, and administration routes. These vaccines are developed against highly infectious diseases including COVID-19, HIV, and influenza. While traditional vaccines typically necessitate frequent booster doses, nano-based vaccines have the potential to induce memory effector responses, along with humoral and cellular immune responses. Consequently, frequent boosters are not required. Various nano-based vaccines are being studied in pre-clinical trials to combat the future pandemics but the adaptation of these vaccines is not reasonable. The slow adaptation is mainly ascribed to certain issues including regulatory framework, manufacturing, and safety risks. The application of the nanoparticles in terms of their safety profiles is not well studied and, therefore, detailed studies and clinical trials are necessary to ensure the safety of nanoparticles for vaccine delivery. The provision of good regulatory framework for vaccine developers can be helpful in the development of good standard vaccines in future. Nevertheless, the successful utilization of nano-based vaccines such as the Pfizer/BioNTech and Moderna mRNA COVID-19 vaccines has provided valuable experience and highlights the potential future applications of nanobased vaccines in combating infectious diseases (Vincken et al., 2007).
Nanotools are helpful in developing seasonal or personalized vaccines to generate better immunity with broader spectrum. However, certain issues necessitate the development of an optimal solution, which should be determined through a comprehensive risk-benefit analysis. The safety testing of nano-based vaccines against various risk factors and development of analytical procedures for development of the vaccines will be required to be prioritized (Azharuddin et al., 2022). However, the advancement in nanoparticle design and upgraded knowledge of virus entry will provide further improvement in future to develop nano-based vaccines with advanced features (Ftouh et al., 2021). This advanced nanotechnology will provide innovative vaccine formulations against infectious, metabolic, and complex diseases as well as cancer (Panda, 2012b). Future vaccines are expected to be safe and more stable with strong antitumor responses (Yin et al., 2022).
1.6 Conclusions
Vaccines activate the immune system and produce adaptive immunity against a pathogen; a person is vaccinated by injecting an antigenic substance into their body.
It will be advantageous to use NPs to deliver vaccine components because they can easily encapsulate target antigens, proteins, bacteria, and parasites. NPs can also deliver a sustained release of vaccine payload into immune cells and produce long-lasting immunological effects after crossing biological barriers. Although these NP vehicles might offer promising possibilities for upcoming vaccination strategies, it’s important to be aware of any potential risks, particularly those related to cytotoxicity. The recent medical history of NPs makes them unfit for long-term human use. However, the medical community has become more confident about nanovaccines with high efficacy and even a good safety profile as a result of the recent success of LNP-based COVID-19 vaccines.
References
Acosta, C. J., Galindo, C. M., Deen, J. L., Ochiai, R. L., Lee, H. J., von Seidlein, L., et al. (2005). Vaccines against cholera, typhoid fever and shigellosis for developing countries. Expert Opinion on Biological Therapy, 4, 1939–1951. https://doi.org/10.1517/14712598.4.12.1939
Alloatti, A., Kotsias, F., Magalhaes, J. G., & Amigorena, S. (2016). Dendritic cell maturation and cross-presentation: Timing matters! Immunological Reviews, 272(1), 97–108.
Alving, C. R., Beck, Z., Matyas, G. R., & Rao, M. (2016). Liposomal adjuvants for human vaccines. Expert Opinion on Drug Delivery, 13, 807–816. https://doi.org/10.1517/17425247.2016.1151871
Ariey, F., Witkowski, B., Amaratunga, C., Beghain, J., Langlois, A., Khim, N., et al. (2014). A molecular marker of artemisinin-resistant plasmodium falciparum malaria. Nature, 505, 50–55.
Arnáiz, B., Martínez-Ávila, O., Falcon-Perez, J. M., & Penadés, S. (2012). Cellular uptake of gold nanoparticles bearing HIV gp120 Oligomannosides. Bioconjugate Chemistry, 23(4), 814–825.
Azharuddin, M., Zhu, G. H., Sengupta, A., Hinkula, J., Slater, N. K., & Patra, H. K. (2022). Nano toolbox in immune modulation and nanovaccines. Trends in Biotechnology.
Bachmann, M. F., & Jennings, G. T. (2019). Vaccine delivery: A matter of size, geometry, kinetics and molecular patterns. Nature Reviews Immunology, 10, 1–15. https://doi.org/10.1038/s41577-019-0144-4
Bahadoran, A., Moeini, H., Bejo, M. H., Hussein, M. Z., & Omar, A. R. (2016). Development of Tat-conjugated dendrimer for transdermal DNA vaccine delivery. Journal of Pharmacy & Pharmaceutical Sciences, 19, 325–338. https://doi.org/10.18433/J3G31Q
Basu, R., Zhai, L., Contreras, A., & Tumban, E. (2018). Immunization with phage virus-like particles displaying Zika virus potential B-cell epitopes neutralizes Zika virus infection of monkey kidney cells. Vaccine, 36, 1256–1264. https://doi.org/10.1016/j.vaccine.2018.01.056
Baylor, N. W., Egan, W., & Richman, P. (2002). Aluminum salts in vaccines—US perspective. Vaccine, 20, S18–S23.
Bhardwaj, P., Tripathi, P., Gupta, R., & Pandey, S. (2020). Niosomes: A review on niosomal research in the last decade. Journal of Drug Delivery Science and Technology, 56, 101581.
Bolhassani, A., Safaiyan, S., & Rafati, S. (2011). Improvement of different vaccine delivery systems for cancer therapy. Molecular Cancer, 10, 3.
Boopathy, A. V., Mandal, A., Kulp, D. W., Menis, S., Bennett, N. R., Watkins, H. C., Wang, W., Martin, J., Thai, N. T., He, Y., et al. (2019). Enhancing humoral immunity via sustained-release implantable microneedle patch vaccination. Proceedings of the National Academy of Sciences, 116, 16473–16478.
Butkovich, N., Li, E., Ramirez, A., Burkhardt, A. M., & Wang, S. W. (2021). Advancements in protein nanoparticle vaccine platforms to combat infectious disease. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 13(3), e1681. https://doi.org/10.1002/wnan.1681
Chahal, J. S., Khan OF, Cooper, C. L., McPartlan, J. S., Tsosie, J. K., Tilley, L. D., et al. (2016). Dendrimer-RNA nanoparticles generate protective immunity against lethal Ebola, H1N1 influenza, and Toxoplasma gondii challenges with a single dose. Proceedings of the National Academy of Sciences USA, 113, E4133–E4142. https://doi.org/10.1073/pnas.1600299113
Chai, Q., Wang, L., Liu, C. H., & Ge, B. (2020). New insights into the evasion of host innate immunity by mycobacterium tuberculosis. Cellular & Molecular Immunology, 17, 901–913. https://doi.org/10.1038/s41423-020-0502-z
Chen, D. S., & Mellman, I. (2013). Oncology meets immunology: The cancer-immunity cycle. Immunity, 39(1), 1–10.
Chen, Y.-H., Lai, K.-Y., Chiu, Y.-H., Wu, Y.-W., Shiau, A.-L., & Chen, M.-C. (2019). Implantable microneedles with an immune-boosting function for effective intradermal influenza vaccination. Acta Biomaterialia, 97, 230–238.
Dadu, A., Kumar, P., & Kumar, A. (2021). Nanoparticle-based vaccines for infectious diseases: A review. Journal of Biomedical Nanotechnology, 17(8), 1425–1450. https://doi.org/10.1166/jbn.2021.3089
Datta, P., & Mandal, A. K. (2020). Nanotechnology-based approaches in anticancer research. International Journal of Pharmaceutical Sciences and Research, 11(7), 3072–3087. https://doi.org/10.13040/IJPSR.0975-8232.11(7).3072-87
Draper, S. J., & Heeney, J. L. (2010). Viruses as vaccine vectors for infectious diseases and cancer. Nature Reviews. Microbiology, 8, 62–73.
Eidi, H., Joubert, O., Attik, G., Duval, R. E., Bottin, M. C., Hamouia, A., et al. (2010). Cytotoxicity assessment of heparin nanoparticles in NR8383 macrophages. International Journal of Pharmaceutics, 396(1–2), 156–165.
Fan, Y., Zheng, X., Ali, Y., Berggren, P. O., & Loo, S. C. J. (2019). Local release of rapamycin by microparticles delays islet rejection within the anterior chamber of the eye. Scientific Reports, 9(1), 1–9.
Fang, R. H., Hu, C. M. J., Luk, B. T., Gao, W., Copp, J. A., Tai, Y., et al. (2014). Cancer cell membrane-coated nanoparticles for anticancer vaccination and drug delivery. Nano Letters, 14(4), 2181–2188.
Ftouh, M., Kalboussi, N., Abid, N., Sfar, S., Mignet, N., & Bahloul, B. (2021). Contribution of nanotechnologies to vaccine development and drug delivery against respiratory viruses. PPAR Research, 2021.
Gao, Y., Wijewardhana, C., & Mann, J. F. S. (2018). Virus-like particle, liposome, and polymeric particle-based vaccines against HIV-1. Frontiers in Immunology, 9, 345. https://doi.org/10.3389/fimmu.2018.00345
Garg, A., & Dewangan, H. K. (2020). Nanoparticles as adjuvants in vaccine delivery. Critical Reviews™ in Therapeutic Drug Carrier Systems, 37(2).
González-Miró, M., Rodríguez-Noda, L., Fariñas-Medina, M., Cedré-Marrero, B., Madariaga-Zarza, S., Zayas-Vignier, C., et al. (2018). Bioengineered polyester beads co-displaying protein and carbohydrate-based antigens induce protective immunity against bacterial infection. Scientific Reports, 8, 1–15. https://doi.org/10.1038/s41598-018-20205-7
Gordon, J. R., Ma, Y., Churchman, L., Gordon, S. A., & Dawicki, W. (2014). Regulatory dendritic cells for immunotherapy in immunologic diseases. Frontiers in Immunology, 5, 7.
Grgacic, E. V. L., & Anderson, D. A. (2006). Virus-like particles: passport to immune recognition. Methods, 40, 60–65. https://doi.org/10.1016/j.ymeth.2006.07.018
Guo, S., Fu, D., Utupova, A., Sun, D., Zhou, M., Jin, Z., & Zhao, K. (2019). Applications of polymer-based nanoparticles in vaccine field. Nanotechnology Reviews, 8(1), 143–155.
Gutjahr, A., Phelip, C., Coolen, A.-L., Monge, C., Boisgard, A.-S., Paul, S., & Verrier, B. (2016). Biodegradable polymeric nanoparticles-based vaccine adjuvants for lymph nodes targeting. Vaccine, 4, 34.
Hanley, K. A. (2011). The double-edged sword: How evolution can make or break a live-attenuated virus vaccine. Evolution: Education and Outreach, 4, 635. https://doi.org/10.1007/S12052-011-0365-Y
Harandi, A. M., Medaglini, D., & Shattock, R. J. (2010). Vaccine adjuvants: A priority for vaccine research. Vaccine, 28, 2363–2366.
He, X., Wang, K., Tan, W., Liu, B., Lin, X., et al. (2003). Bioconjugated nanoparticles for DNA protection from cleavage. Journal of the American Chemical Society, 125, 7168–7169. https://doi.org/10.1021/ja034450d
He, Q., Gao, Y., Zhang, L., Zhang, Z., Gao, F., Ji, X., et al. (2011). A pH-responsive mesoporous silica nanoparticles-based multi-drug delivery system for overcoming multi-drug resistance. Biomaterials, 32(30), 7711–7720.
Helmy, M. T., Sroor, F. M., Mahrous, K. F., Mahmoud, K., Hassaneen, H. M., Saleh, F. M., ... & Mohamed Teleb, M. A. (2022). Anticancer activity of novel 3‐(furan‐2‐yl) pyrazolyl and 3‐(thiophen‐2‐yl) pyrazolyl hybrid chalcones: Synthesis and in vitro studies. Archiv der Pharmazie, 355(3), 2100381
Ichihashi, T., Satoh, T., Sugimoto, C., & Kajino, K. (2013). Emulsified phosphatidylserine, simple and effective peptide carrier for induction of potent epitope-specific T cell responses. PLoS One, 8, e60068. https://doi.org/10.1371/journal.pone.0060068
Jia, Y., Omri, A., Krishnan, L., & McCluskie, M. J. (2017). Potential applications of nanoparticles in cancer immunotherapy. Human Vaccines & Immunotherapeutics, 13(1), 63–74.
Jones, R. M., Chichester, J. A., Mett, V., Jaje, J., Tottey, S., Manceva, S., et al. (2013). A plant-produced Pfs25 VLP malaria vaccine candidate induces persistent transmission blocking antibodies against Plasmodium falciparum in immunized mice. PLoS One, 8(11), e79538.
Kawano, M., Matsui, M., & Handa, H. (2013). SV40 virus-like particles as an effective delivery system and its application to a vaccine carrier. Expert Review of Vaccines, 12, 199–210. https://doi.org/10.1586/erv.12.149
Kheirollahpour, M., Mehrabi, M., Dounighi, N. M., Mohammadi, M., & Masoudi, A. (2020). Nanoparticles and vaccine development. Pharmaceutical Nanotechnology, 8(1), 6–21.
Kim, J. S., Choi, J., Kim, J. C., Park, H., Yang, E., Park, J. S., Song, M., & Park, J. (2020). Microneedles with dual release pattern for improved immunological efficacy of hepatitis B vaccine. International Journal of Pharmaceutics, 591, 119928.
Kumar, R., Nyakundi, R., Kariuki, T., Ozwara, H., Nyamongo, O., Mlambo, G., et al. (2013). Functional evaluation of malaria Pfs25 DNA vaccine by in vivo electroporation in olive baboons. Vaccine, 31(31), 3140–3147.
Kumar, R., Angov, E., & Kumar, N. (2014). Potent malaria transmission-blocking antibody responses elicited by plasmodium falciparum Pfs25 expressed in Escherichia coli after successful protein refolding. Infection and Immunity, 82(4), 1453–1459.
Kuwentrai, C., Yu, J., Rong, L., Zhang, B., Hu, Y., Gong, H., Dou, Y., Deng, J., Huang, J., & Xu, C. (2020). Intradermal delivery of receptor-binding domain of SARS-CoV-2 spike protein with dissolvable microneedles to induce humoral and cellular responses in mice. Bioengineering & Translational Medicine, 6, e10202.
Levine, M. M., & Sztein, M. B. (2004). Vaccine development strategies for improving immunization: The role of modern immunology. Nature Immunology, 5(5), 460–464.
Li, J., Yu, J., Xu, S., Shi, J., Xu, S., Wu, X., Fu, F., Peng, Z., Zhang, L., & Zheng, S. (2016). Immunogenicity of porcine circovirus type 2 nucleic acid vaccine containing CpG motif for mice. Virology Journal, 13, 1–7.
Look, M., Bandyopadhyay, A., Blum, J. S., & Fahmy, T. M. (2010). Application of nanotechnologies for improved immune response against infectious diseases in the developing world. Advanced Drug Delivery Reviews, 62, 378–393.
Lugade, A. A., Bharali, D. J., Pradhan, V., Elkin, G., Mousa, S. A., & Thanavala, Y. (2013). Single low-dose un-adjuvanted HBsAg nanoparticle vaccine elicits robust, durable immunity. Nanomedicine: Nanotechnology, Biology and Medicine, 9(7), 923–934.
Marques Neto, L. M., Kipnis, A., & Junqueira-Kipnis, A. P. (2017). Role of metallic nanoparticles in vaccinology: Implications for infectious disease vaccine development. Frontiers in Immunology, 8, 239.
Mehrabi, M., Montazeri, H., Mohamadpour Dounighi, N., Rashti, A., & Vakili-Ghartavol, R. (2018). Chitosan-based nanoparticles in mucosal vaccine delivery. Archives of Razi Institute, 73(3), 165–176.
Melief, C. J., van Hall, T., Arens, R., Ossendorp, F., & van der Burg, S. H. (2015). Therapeutic cancer vaccines. Journal of Clinical Investigation, 125(9), 3401–3412.
Moon, J. J., Suh, H., Bershteyn, A., Stephan, M. T., Liu, H., Huang, B., et al. (2011). Interbilayer-crosslinked multilamellar vesicles as synthetic vaccines for potent humoral and cellular immune responses. Nature Materials, 10, 243–251. https://doi.org/10.1038/nmat2960
Niikura, K., Matsunaga, T., Suzuki, T., Kobayashi, S., Yamaguchi, H., Orba, Y., ... & Sawa, H. (2013). Gold nanoparticles as a vaccine platform: influence of size and shape on immunological responses in vitro and in vivo. ACS Nano, 7(5), 3926–3938.
Nunes, J. K., Woods, C., Carter, T., Raphael, T., Morin, M. J., Diallo, D., et al. (2014). Development of a transmission-blocking malaria vaccine: Progress, challenges, and the path forward. Vaccine, 32(43), 5531–5539.
O’Hagan, D. T., & Valiante, N. M. (2003). Recent advances in the discovery and delivery of vaccine adjuvants. Nature Reviews. Drug Discovery, 2, 727–735.
Palmer, G. H., Bankhead, T., & Seifert, H. S. (2016). Antigenic variation in bacterial pathogens. Microbiology Spectrum, 4, 4.1.03. https://doi.org/10.1128/microbiolspec.VMBF-0005-2015
Panda, M., Abraham, A., & Patra, M. R. (2012a). A hybrid intelligent approach for network intrusion detection. Procedia Engineering, 30, 1–9.
Panda, M. K., Ladomenou, K., & Coutsolelos, A. G. (2012b). Porphyrins in bio-inspired transformations: Lightharvesting to solar cell. Coordination Chemistry Reviews, 256(21–22), 2601–2627.
Pardi, N., Hogan, M. J., Porter, F. W., & Weissman, D. (2018). mRNA vaccines — a new era in vaccinology. Nature Reviews Drug Discovery, 17(4), 261–279.
Patel, K. G., & Swartz, J. R. (2011). Surface functionalization of virus-like particles by direct conjugation using azide–alkyne click chemistry. Bioconjugate Chemistry, 22, 376–387. https://doi.org/10.1021/bc100367u
Pati, R., Shevtsov, M., & Sonawane, A. (2018). Nanoparticle vaccines against infectious diseases. Frontiers in Immunology, 9, 2224.
Petkar, K., Patil, S., Chavhan, S., Kaneko, K., Sawant, K., Kunda, N., & Saleem, I. (2021). An overview of nanocarrier-based adjuvants for vaccine delivery. Pharmaceutics, 13, 455.
Pulendran, B. (2006). Division of labor and cooperation between dendritic cells. Nature Immunology, 7(7), 699–700.
Rana, S., Bajaj, A., Mout, R., & Rotello, V. M. (2012). Monolayer coated gold nanoparticles for delivery applications. Advanced Drug Delivery Reviews, 64(2), 200–216.
Rappuoli, R., Mandl, C. W., Black, S., & De Gregorio, E. (2011). Vaccines for the twenty-first century society. Nature Reviews Immunology, 11(12), 865–872.
Reed, S. G., Orr, M. T., & Fox, C. B. (2013). Key roles of adjuvants in modern vaccines. Nature Medicine, 19(12), 1597–1608.
Ribeiro, A. M., Souza, A. C. O., Amaral, A. C., Vasconcelos, N. M., Jeronimo, M. S., Carneiro, F. P., et al. (2013). Nanobiotechnological approaches to delivery of DNA vaccine against fungal infection. Journal of Biomedical Nanotechnology, 9, 221–230. https://doi.org/10.1166/jbn.2013.1491
Rice-Ficht, A. C., Arenas-Gamboa, A. M., Kahl-McDonagh, M. M., & Ficht, T. A. (2010). Polymeric particles in vaccine delivery. Current Opinion in Microbiology, 13, 106–112.
Sayers, E. W., Barrett, T., Benson, D. A., Bolton, E., Bryant, S. H., Canese, K., ... & Ye, J. (2012). Database resources of the national center for biotechnology information. Nucleic Acids Research, 40(D1), D13–D25.
Sawa, T., Ihara, H., Ida, T., Fujii, S., Nishida, M., & Akaike, T. (2013). Formation, signaling functions, and metabolisms of nitrated cyclic nucleotide. Nitric Oxide, 34, 10–18.
Schlom, J. (2012). Therapeutic cancer vaccines: Current status and moving forward. Journal of the National Cancer Institute, 104(8), 599–613.
Shah, M. A. A., Ali, Z., Ahmad, R., Qadri, I., Fatima, K., & He, N. (2015). DNA-mediated vaccines delivery through nanoparticles. Journal of Nanoscience and Nanotechnology, 15(1), 41–53.
Shin, M. D., Shukla, S., Chung, Y. H., Beiss, V., Chan, S. K., Ortega-Rivera, O. A., Wirth, D. M., Chen, A., Sack, M., Pokorski, J. K., et al. (2020). COVID-19 vaccine development and a potential nanomaterial path forward. Nature Nanotechnology, 15, 646–655.
Silva, C. L., Bonato, V. L. D., Coelho-Castelo, A. A. M., De Souza, A. O., Santos, S. A., Lima, K. M., et al. (2005). Immunotherapy with plasmid DNA encoding mycobacterial hsp65 in association with chemotherapy is a more rapid and efficient form of treatment for tuberculosis in mice. Gene Therapy, 12, 281–287. https://doi.org/10.1038/sj.gt.3302418
Smith, P., Haberl, H., Popp, A., Erb, K. H., Lauk, C., Harper, R., ... & Rose, S. (2013). How much land‐based greenhouse gas mitigation can be achieved without compromising food security and environmental goals?. Global Change Biology, 19(8), 2285–2302.
Smith, J. D., Morton, L. D., & Ulery, B. D. (2015). Nanoparticles as synthetic vaccines. Current Opinion in Biotechnology, 34, 217–224.
Sridhar, S., Brokstad, K. A., & Cox, R. J. (2015). Influenza vaccination strategies: Comparing inactivated and live attenuated influenza vaccines. Vaccine, 3(2), 373–389.
Sulczewski, F., Liszbinski, R. B., Romão, P. R. T., & Junior, L. C. R. (2018). Nanoparticle vaccines against viral infections. Archives of Virology, 163, 2313–2325.
Sun, L., Campbell, M. G., & Dincă, M. (2016). Electrically conductive porous metal–organic frameworks. Angewandte Chemie International Edition, 55(11), 3566–3579.
Sun, B., & Xia, T. (2016). Nanomaterial-based vaccine adjuvants. Journal of Materials Chemistry B, 4(33), 5496–5509. https://doi.org/10.1039/c6tb01131d
Tebas, P., Yang, S., Boyer, J. D., Reuschel, E. L., Patel, A., Christensen-Quick, A., Andrade, V. M., Morrow, M. P., Kraynyak, K., Agnes, J., et al. (2021). Safety and immunogenicity of INO-4800 DNA vaccine against SARS-CoV-2: A preliminary report of an open-label, phase 1 clinical trial. EClinicalMedicine, 31, 100689.
Thakur, S., Singh, A. K., Ghrera, S. P., & Elhoseny, M. (2019). Multi-layer security of medical data through watermarking and chaotic encryption for tele-health applications. Multimedia Tools and Applications, 78, 3457–3470.
Villa, C. H., Dao, T., Ahearn, I., Fehrenbacher, N., Casey, E., Rey, D. A., et al. (2011). Single-walled carbon nanotubes deliver peptide antigen into dendritic cells and enhance IgG responses to tumor-associated antigens. ACS Nano, 5, 5300–5311. https://doi.org/10.1021/nn200182x
Vincken, P. W., ter Braak, A. P., van Erkel, A. R., Coerkamp, E. G., de Rooy, T. P., de Lange, S., ... & Bloem, J. L. (2007). MR imaging: effectiveness and costs at triage of patients with nonacute knee symptoms. Radiology, 242(1), 85–93.
Vyas, S., Quraishi, S., Gupta, S., & Jaganathan, K. (2005). Aerosolized liposome-based delivery of amphotericin B to alveolar macrophages. International Journal of Pharmaceutics, 296, 12–25. https://doi.org/10.1016/j.ijpharm.2005.02.003
Wang, T., Zou, M., Jiang, H., Ji, Z., Gao, P., & Cheng, G. (2011). Synthesis of a novel kind of carbon nanoparticle with large mesopores and macropores and its application as an oral vaccine adjuvant. European Journal of Pharmaceutical Sciences, 44, 653–659. https://doi.org/10.1016/j.ejps.2011.10.012
Watson, D. S., Endsley, A. N., & Huang, L. (2012). Design considerations for liposomal vaccines: Influence of formulation parameters on antibody and cell-mediated immune responses to liposome associated antigens. Vaccine, 30, 2256–2272. https://doi.org/10.1016/j.vaccine.2012.01.070
Wegmann, F., Gartlan, K. H., Harandi, A. M., Brinckmann, S. A., Coccia, M., Hillson, W. R., ... & Sattentau, Q. J. (2012). Polyethyleneimine is a potent mucosal adjuvant for viral glycoprotein antigens. Nature Biotechnology, 30(9), 883–888.
Wen, R., Umeano, A. C., Kou, Y., Xu, J., & Farooqi, A. A. (2019). Nanoparticle systems for cancer vaccine. Nanomedicine, 14(5), 627–648.
Whitney, S. M., Baldet, P., Hudson, G. S., & Andrews, T. J. (2001). Form I Rubiscos from non‐green algae are expressed abundantly but not assembled in tobacco chloroplasts. The Plant Journal, 26(5), 535–547.
Yin, W., Xu, Y., Xu, P., Cao, X., Wu, C., Gu, C., ... & Xu, H. E. (2022). Structures of the Omicron spike trimer with ACE2 and an anti-Omicron antibody. Science, 375(6584), 1048–1053.
Zhao, L., Seth, A., Wibowo, N., Zhao, C. X., Mitter, N., Yu, C., & Middelberg, A. P. (2014). Nanoparticle vaccines. Vaccine, 32(3), 327–337.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Aqib, A.I. et al. (2023). Diversities of Various Nanomaterials-Based Vaccines for Healthcare Applications. In: Pal, K. (eds) Nanovaccinology. Springer, Cham. https://doi.org/10.1007/978-3-031-35395-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-35395-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-35394-9
Online ISBN: 978-3-031-35395-6
eBook Packages: MedicineMedicine (R0)