Abstract
Glenoid-shaft angle and lateralization play an important role in improving shoulder function after a reverse total shoulder arthroplasty (RTSA). As surgical techniques continue to evolve, this chapter considers the evidence that is currently available and offers surgeons a perspective on how these two implant-specific characteristics influence the expected performance of a RTSA.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
As discussed throughout this edition, the shoulder relies on a careful balance of stability and mobility, and while an anatomic total shoulder arthroplasty aims to reproduce normal shoulder kinematics, the reverse total shoulder arthroplasty (RTSA) is a non-anatomic procedure. It draws on a partially constrained design to empower the deltoid and the intact elements of the shoulder girdle to move the humerus around a fixed point, the glenosphere. When the treatment of rotator cuff tear arthropathy was revolutionized by Grammont’s design, the mechanical effect of his design increased the deltoid’s moment arm by 42% [1]. In time, modern reverse designs have maintained the essential elements of his approach to maintain the joint’s stability, while simultaneously seeking a more anatomic position for the resulting shoulder joint to minimize complications and maximize range of motion (external rotation).
The normal inclination of the proximal humerus, or neck-shaft angle (NSA), is approximately 135°. However, person-to-person variability can range from 115 to 148°. When studied, approximately 22% of patients will have a NSA less than 130° or greater than 140°, so careful consideration needs to address the native anatomy and the intended surgical result [2]. The Grammont design had a fixed, 155-degree NSA and enhanced the deltoid moment arm by moving the humerus inferior or distal [3]. This change in position made the deltoid more powerful in forward elevation and abduction, while shifting the center of rotation medially [4]. Grammont achieved success in his design by moving the center of rotation (COR) medial to the interface between the baseplate and glenoid [5].
This change in the COR created a stable foundation for the reverse total shoulder by minimizing sheer and promoting the compression necessary for osteointegration. When combined with a 155-degree angle on the humeral prostheses, these technical considerations addressed the intrinsic disability of rotator cuff arthropathy as long as the glenosphere was placed inferior on the glenoid face and the humeral implant did not impinge.
However, these design choices also result in significant changes to the physiologic function of the shoulder’s muscular supports. The anterior deltoid, the posterior deltoid, and the pectoralis major are more easily recruited as flexors and abductors, improving a patient’s ability to lift the arm. The latissimus dorsi, teres major, and lower part of the pectoralis major have an increased ability to serve in adduction and extension. This change results in a corresponding decrease in their effect on both internal and external rotation [6, 7]. In patients with Grammont-style RSA, the anterior and posterior rotator cuff are weakened by medialization, limiting their active internal and external rotation [8, 9].
In time, the medialization intrinsic to the traditional Grammont design was associated with high rates of scapular notching and concern for baseplate micro-motion, osteolysis, and potential glenoid loosening [10, 11]. This concern combined with the observation that more notching was associated with worse clinical outcomes [12,13,14,15]. To address the concerns associated with the traditional design, lateralized implants have been developed to improve the characteristics of the glenoid component, the humeral stem, or both [16].
Lateralized glenoid components employ modern materials to create a stable implant-bone interface with a COR that is lateral to the surface of the glenoid. This modification preserves rotational moment arms of the subscapularis and teres minor and enhances the active range of motion in the axial plane [17]. While the joint’s COR needs to be more medial than the native, lateralization of the glenosphere from the glenoid enhances the compressive forces at the bone-implant interface and may overcome the shear forces that result from lateralization [18].
As a result, lateralized components have been shown to decrease the impingement between the scapular neck and the humeral prosthesis that results in notching. In a systematic review of 13 studies, the incidence of scapular notching was 5.4% in a lateralized glenoid group compared to 44.9% in a traditional group (p < 0.001) [19]. At the same time, patients with a lateralized prosthesis demonstrated more active external rotation (46° vs. 24°, p < 0.001). In contrast, clinically significant glenoid loosening was found in 1.8% of the traditional compared to 8.8% in the lateralized group (p = 0.003), raising questions of the sheer stress associated with lateralization. When one lateralized design was compared to a Grammont-style prosthesis, the same disparity was confirmed; glenoid loosening occurred in 5.8% of lateralized implants compared to 2.5% [20]. In the lab, lateralized implants have increased micro-motion with a lateralized design, acknowledging that lateralization can be achieved through the implant’s design or with bone grafting and/or bone augmentation of the glenoid [18].
With the ongoing evolution of reverse total shoulder designs, there may be a lag in the maturation of the data available regarding implant behavior. In a 2019 systematic review that included 103 studies, there was no difference in the rate of aseptic loosening for lateralized and medialized glenoids (1.84% vs. 1.15%, respectively) [21]. Correspondingly, patient outcomes were similar for the two designs in a 2018 review, despite a difference in external rotation (lateralized greater than Grammont) and a difference in scapular notching (Grammont greater than lateralized) [22].
In considering the relevant equivalence of the two designs’ results, the debate remains unresolved. The Grammont design medializes the center of rotation, creating a compressive force at the implant-bone interface that may improve the glenoid fixation and implant longevity. Conversely, lateralized designs decrease the incidence of scapular notching and may improve external rotation.
Changes to the humeral component have been introduced to maximize the compression on the glenoid component while increasing the mechanical advantage of a lateralized center of rotation. While 155° is the most common humeral shaft angle, the horizontal cut may increase the impingement [23,24,25,26]. A reduced neck-shaft angle aims to reduce scapular notching, but it may increase the rate of dislocation [3].
In biomechanical studies, a decreased shaft angle will increase the range of motion, while decreasing the potential for contact with the inferior angle of the glenoid [27]. A recent meta-analysis of 2222 shoulders undergoing RTSA compared the rate of scapula notching and dislocation between implants with different neck-shaft angles [28]. While only 20% of the implants included had a neck-shaft angle of 135°, scapular notching was found to be more common with a 155-degree implant (16.80%) than a 135-degree prosthesis (2.83%) (p < 0.01). There was no significant difference in dislocation rate between the two groups (2.33% and 1.74%, respectively). However, lateralization alone has been shown to decrease scapular notching, even with a 155-degree prosthesis, so the neck-shaft angle may not be the salient implant characteristic [29].
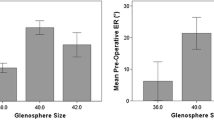
When the impact of neck-shaft angle on range of motion was examined, a similar meta-analysis revealed that a 135-degree prosthesis achieved greater external rotation (33°) than the 155-degree alternative (25°) (p < 0.01) [30]. In this way, modification to the humeral designs that lower the neck-shaft angle may reduce scapula notching and increase external rotation. How this adjustment should be combined with the lateralization of the glenoid component and the risk of loosening warrants further investigation, particularly if the risk of scapula fracture is included in the broader analysis of a patient’s expected clinical result (Figs. 18.1 and 18.2; Table 18.1).
References
Kontaxis A, Johnson GR. The biomechanics of reverse anatomy shoulder replacement: a modelling study. Clin Biomech (Bristol, Avon). 2009;24:254–60.
Jeong J, Bryan J, Iannotti JP. Effect of a variable prosthetic neck-shaft angle and the surgical technique on replication of normal humeral anatomy. J Bone Joint Surg Am. 2009;91-A:1932–41.
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–61S.
Schwartz DG, Kang SH, Lynch TS, et al. The anterior deltoid’s importance in reverse shoulder arthroplasty: a cadaveric biomechanical study. J Shoulder Elbow Surg. 2013;22:357–64.
Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–8.
Ackland DC, Richardson M, Pandy MG. Axial rotation moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2012;94-A:1886–95.
Ackland DC, Roshan-Zamir S, Richardson M, Pandy MG. Moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2010;92-A:1221–30.
Herrmann S, König C, Heller M, Perka C, Greiner S. Reverse shoulder arthroplasty leads to significant biomechanical changes in the remaining rotator cuff. J Orthop Surg Res. 2011;6:42.
Simovitch RW, Helmy N, Zumstein MA, Gerber C. Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89-A:934–9.
Werner CML, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–86.
Roche CP, Stroud NJ, Martin BL, et al. The impact of scapular notching on reverse shoulder glenoid fixation. J Shoulder Elbow Surg. 2013;22:963–70.
Mollon B, Mahure SA, Roche CP, Zuckerman JD. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J Shoulder Elbow Surg. 2017;26:1253–61.
Wellmann M, Struck M, Pastor MF, Gettmann A, Windhagen H, Smith T. Short and midterm results of reverse shoulder arthroplasty according to the preoperative etiology. Arch Orthop Trauma Surg. 2013;133:463–71.
Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588–600.
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–95.
Werthel J-D, Walch G, Vegehan E, Deransart P, Sanchez-Sotelo J, Valenti P. Lateralization in reverse shoulder arthroplasty: a descriptive analysis of different implants in current practice. Int Orthop. 2019;43:2349–60.
Greiner S, Schmidt C, König C, Perka C, Herrmann S. Lateralized reverse shoulder arthroplasty maintains rotational function of the remaining rotator cuff. Clin Orthop Relat Res. 2013;471:940–6.
Harman M, Frankle M, Vasey M, Banks S. Initial glenoid component fixation in ‘reverse’ total shoulder arthroplasty: a biomechanical evaluation. J Shoulder Elbow Surg. 2005;14:162S–7S.
Lawrence C, Williams GR, Namdari S. Influence of glenosphere design on outcomes and complications of reverse arthroplasty: a systematic review. Clin Orthop Surg. 2016;8:288–97.
Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–57.
Rojas J, Choi K, Joseph J, Srikumaran U, McFarland EG. Aseptic glenoid baseplate loosening after reverse total shoulder arthroplasty: a systematic review and meta-analysis. JBJS Rev. 2019;7:e7.
Helmkamp JK, Bullock GS, Amilo NR, et al. The clinical and radiographic impact of center of rotation lateralization in reverse shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2018;27:2099–107.
Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–85.
De Biase CF, Delcogliano M, Borroni M, Castagna A. Reverse total shoulder arthroplasty: radiological and clinical result using an eccentric glenosphere. Musculoskelet Surg. 2012;96:S27–34.
Sayana MK, Kakarala G, Bandi S, Wynn-Jones C. Medium term results of reverse total shoulder replacement in patients with rotator cuff arthropathy. Ir J Med Sci. 2009;178:147–50.
Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93:1915–23.
Oh JH, Shin S-J, McGarry MH, Scott JH, Heckmann N, Lee TQ. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1091–8.
Erickson BJ, Frank RM, Harris JD, Mall N, Romeo AA. The influence of humeral head inclination in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2015;24:988–93.
Boileau P, Moineau G, Roussanne Y, O’Shea K. Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res. 2011;469:2558–67.
Erickson BJ, Harris JD, Romeo AA. The effect of humeral inclination on range of motion in reverse total shoulder arthroplasty: a systematic review. Am J Orthop (Belle Mead NJ). 2016;45:E174–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 ISAKOS
About this chapter
Cite this chapter
DeAngelis, J.P. (2023). Strategies to Improve Function in Reverse Total Shoulder Arthroplasty (RTSA): Glenoid-Shaft Angle and Lateralization. In: Mazzocca, A.D., Calvo, E., Di Giacomo, G. (eds) Shoulder Arthritis across the Life Span. Springer, Cham. https://doi.org/10.1007/978-3-031-33298-2_18
Download citation
DOI: https://doi.org/10.1007/978-3-031-33298-2_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33297-5
Online ISBN: 978-3-031-33298-2
eBook Packages: MedicineMedicine (R0)