Abstract
Malaria is an ancient disease that used to be widespread in most parts of China, dominated by Plasmodium vivax and P. falciparum, seriously threatening people’s health. In this chapter, the malaria epidemic in China from ancient times to the present was briefly reviewed. The Chinese nation has made important contributions to the fight against malaria, especially after the founding of the People’s Republic of China. No indigenous malaria cases have been reported since 2017 after nearly 70 years of unremitting efforts, and China officially achieved the elimination of malaria on June 30, 2021. However, China will likely see a resurgence in malaria cases due to the thousands of imported cases and the distribution of the malaria vector Anopheles mosquitoes in the defined areas. Therefore, it is essential to maintain and strengthen the sensitivity of surveillance and response through capacity building and the research and development of new technologies based on the established and improved multisectoral cooperative mechanism under the unified leadership of the government, thereby effectively consolidating the achievements of malaria elimination in China.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Malaria is an ancient disease that is caused by Plasmodium parasites transmitted by female Anopheles mosquitoes, and the history of malaria outbreaks is thought to date back to the beginnings of civilization. It is a devastating and life-threatening disease with global distribution, resulting in many people losing lives, and is even considered the cause of major military defeats and the disappearance of some nations. Fortunately, with the advancement of the global malaria control process (Litsios 2020), an increasing number of countries have entered the malaria preelimination stage or the elimination stage, and a total of 25 countries have been considered to be on track to reduce indigenous malaria cases to zero by 2025 in the E-2025 initiative after the E-2020 initiative, which was launched by the World Health Organization (WHO) (WHO 2021b, 2021d), although progress has stalled according to the malaria cases and deaths estimated in the world malaria reports in recent years and the negative impact of the coronavirus disease 2019 (COVID-19) pandemic on the implementation of malaria prevention and control measures and the availability of antimalarial treatment (WHO 2021c). For instance, the estimated number of cases in 85 endemic countries in the world reached 241 million, and the estimated number of deaths reached 627,000 in 2020 according to the latest World Malaria Report 2021 (WHO 2021c).
Looking back at the history of malaria, the earliest record of malaria was found in the inscriptions on oracle bones and bronze wares during the Shang-Yin period, which had the pictograph of “malaria” in Chinese, indicating that malaria was prevalent in China 3000 years ago (Tang et al. 2012). Moreover, Hippocrates, a Greek physician in the fourth century BC, linked malaria to the summer/fall, marshes, and splenomegaly and first described the different types of malaria depending upon the periodicity of the fever, thereby completely rejecting its demonic origin (Cunha and Cunha 2008). This explanation remained until 1880 when Laverin discovered that the malaria parasite in the blood of people with malaria was the cause of the disease (Cox 2010; Hempelmann and Krafts 2013). Laverin also won a Nobel Prize for this work in 1907. Another four Nobel Prizes associated with malaria were awarded: Youyou Tu in 2015 for the discovery of artemisinin, a drug that is now the dominant treatment for malaria (Tu 2011, 2016); Paul Müller in 1947 for the synthetic pesticide formula dichlorodiphenyltrichloroethane; Julius Wagner-Jauregg in 1927 for the induction of malaria as a pyrotherapy procedure in the treatment of paralytic dementia; and Ronald Ross in 1902 for the discovery and significance of mosquitoes in the biology of the causative agents in malaria (Talapko et al. 2019).
In the long-term struggle against malaria, the Chinese nation has made outstanding contributions to human understanding of malaria and the prevention and treatment of malaria. In more than 2000 years since the Qin and Han Dynasties, there have been many records about malaria from the earliest medical classic “Huangdi Neijing, Inner Casnon of the Yellow Emperor” to the Ming and Qing dynasties, which described the malaria causes, symptoms, diagnosis, and treatment methods (Tu 2016). In particular, the records of Qinghao in A Handbook of Prescriptions for Emergencies by Ge Hong in the Eastern Jin Dynasty (approximately 317–420 AD) provide important inspiration for the method of extracting active ingredients in the early stage of artemisinin development in China (Ge 300–400 A.D.), and the artemisinin-based antimalarial drug has been developed, which has made a proud contribution to the world (Chen 2014).
China was certified malaria-free by the WHO on June 30, 2021 (Feng et al. 2021; Zhou 2021). In this chapter, we briefly review the malaria epidemic in China from ancient times to the present.
1.2 Malaria Epidemiology Before the Founding of the People’s Republic of China
Malaria is also commonly known as “miasma” and some other dialects in China, and it is an ancient parasitic disease that was distributed extensively throughout history, although there was a lack of systematic epidemic statistical reports before the founding of the People’s Republic of China. Fortunately, the historical records and documents of serious epidemics in different regions have been collected and reviewed by Prof. Zujie Zhou and Prof. Linghua Tang, et al. in Chinese (Tang et al. 2012; Zhou 1991). It was recorded that the prevalence of malaria increased from north to south and from west to east, and Plasmodium vivax, P. falciparum, and P. ovale were identified in surveys conducted in some representative malaria transmission areas, including Yunnan, Guangxi, Guizhou, Guangdong, Fujian, Jiangxi, Sichuan, Zhejiang, Anhui, Jiangsu, Hebei, and Liaoning, from 1924 to 1947. Furthermore, the epidemic could be exacerbated by population movements due to wars, natural disasters, large-scale construction projects, etc., resulting in economic decline and people’s livelihood withering. In this section, we reorganize and briefly describe the epidemiological history of malaria in different geographical and administrative divisions in the Chinese mainland before the founding of the People’s Republic of China mainly based on two books (Tang et al. 2012; Zhou 1991).
1.2.1 Malaria in Southwest China (Yunnan, Guizhou, Tibet, Sichuan, and Chongqing)
In Yunnan, there were records of malaria infections and epidemics among soldiers as early as the Three Kingdoms period. In the poem “Xin Feng Zhe Bi Weng,” written by the Tang Dynasty poet Juyi Bai, he heard that there was a river named Lu in Yunnan, and it would be filled with miasmas when the pepper flowers wither in summer, which was a sight ravaged by malaria. Taihe (now Dali) experienced heavy malaria epidemics in the thirteenth year of Tianbao (AD 754) in the Tang Dynasty recorded in the “Zi Zhi Tong Jian (Comprehensive Mirror for Aid in Government)”(Guang 2012). Since then, there have been many records about the rampant prevalence of malaria in the local areas in the history books and local chronicles of various dynasties. During the 7 years of the construction of the Yunnan section of the Yunnan-Vietnam Railway, which began in 1904, a total of 200,000–300,000 migrant workers from Yunnan, Sichuan, Guangdong, Guangxi, and other places were recruited and severely affected by malaria without enough medical protection, resulting in 60,000–70,000 people dying of malaria (https://baijiahao.baidu.com/s?id=1715864376600876896&wfr=spider&for=pc). In Simao, the trade center in the southern part of Yunnan, the malaria outbreak in 1919 lasted for 30 years, and the malaria parasite rate of the surveyed residents was 76.5% in 1936, while the incidence rate of malaria from January to September of the previous year was 72.9%, resulting in many deaths and serious population reduction (only 944 people left in 1949 from more than 30,000original population of the urban area). Likewise, more than 30,000 people died due to a malaria epidemic in Yunxian County in a few years since 1933, the incidence of malaria in this county was 94.9%, and the rate of malaria parasites reached 49.1% in 1941 (Tang et al. 2012; Zhou 1991).
The annals of Guizhou Province also recorded malaria as early as the Warring States Period (Tang et al. 2012; Zhou 1991). In the Ming Dynasty, Shouren Wang, a Chinese philosopher, was demoted to Longchang, and he wrote in the “Xiuwen County Chronicle” that so many miasmas were distributed in Guizhou and that people living there were very afraid of malaria. Furthermore, there was a folk song in the southern part of Guizhou Province that says, “When you walk to Shimenkan, the ghost will shout behind you; when you walk to Meizikou, the ghost will wait behind you; when you walk to Sanmengou, the King of Hell will take his life.” At the end of the Qing Dynasty, more than 3000 people among more than 5000 cavalrymen stationed in Pojiao Village under Anlong County in southwestern Guizhou died of malaria in a few years. In 1936, Prof. Yongzheng Yao and others found that the splenomegaly rate of school children was 35.9%, and the malaria parasite rate was 50.4%, of which P. falciparum accounted for 72.9%, in Pojiao, Sandaokou and other places in Guizhou. In the following 2 years, Prof. Huaijie Gan surveyed more than 5,800 school children in more than 10 counties in southwestern, northern, and central Guizhou. The malaria parasite rate varied from 1.8% to 51.3%, and P. falciparum was the most common, especially in the southwest and south. From 1939 to 1940, Prof. Jingsheng Guo surveyed 24 counties and cities and found that malaria infection was the most serious in southwestern and southern Guizhou. Among the three counties of Luodian, Ceheng, and Wangmo, the malaria parasite rate of children under 12 years old was more than 25%, and falciparum malaria accounted for 75%. In Songtao County, which is close to Hunan in the northeast, the malaria parasite rate in children could also be as high as 29.3%, and more than half were P. falciparum.
In Tibet, malaria cases were distributed in Moutuo, Chayu, and other counties in the Yarlung Zangbo River and Chayu River valleys in southeastern Tibet, as well as in areas below the altitude of 1500 m in the southern Himalayas, with Moutuo being the majority.
Malaria was endemic throughout the basin and periphery of Sichuan Province. In the 23rd year of Guangxu’s reign (1897), malaria was prevalent in Chongqing, and nearly half of the population fell ill. Between 1934 and 1937, malaria cases accounted for approximately 1.4–2.1% of the inpatients, with vivax malaria accounting for approximately 53%, falciparum malaria accounting for 41%, and malariae malaria accounting for 6% in more than 10 hospitals in Chongqing, Yibin, Kangding, Fuling, Mianzhu, Guanghan, Leshan, Ya’an, and Chengdu. Meanwhile, the malaria species were distributed significantly differently in different areas; the proportion of falciparum malaria ranged from 1.9% to 69.1%, with the highest in Ya’an, Mianzhu, Guanghan, Fuling, and Leshan counties and the lowest in Zhong County. Furthermore, malaria was prevalent, and the splenomegaly rate of adolescents reached 18% in Chongqing in the autumn of 1939 due to the internal relocation of government agencies and the westward migration of refugees. Malaria cases accounted for 20% of the total number of patients, and the highest rate reached 42% in the eight relocation areas. After that, the number of falciparum malaria cases in the suburbs of Gele Mountain increased greatly between 1940 and 1945, and the mortality rate reached 7.7%. In other parts of the province, malaria was also widespread. In 1948, it was reported that falciparum malaria accounted for 93.3% of the malaria cases in Luzhou, and vivax malaria accounted for 97.4% in Chengdu, and some malariae malaria cases were also present.
1.2.2 Malaria in South Central China (Henan, Hubei, Hunan, Guangxi, Guangdong, and Hainan)
In Henan Province, “malaria is in Zheng” was recorded in the “Zuo Spring and Autumn Period”(Zuo), which indicated that malaria was prevalent in Xinzheng more than 2000 years ago. In 1815, during the reign of Emperor Jiaqing of the Qing Dynasty, the malaria epidemic in southern and eastern Shandong also spread to Shangqiu and Luyi in eastern Henan. The malaria epidemic caused by the flood in 1931 had a great impact on the eastern and central parts of Henan Province, and the frequent mobilization of the army led to a major malaria epidemic in the province. For instance, a malaria outbreak occurred in Kaifeng, Henan Province, due to the heavy rain in July and August and the mobilization of soldiers. Moreover, among the positive blood samples for Plasmodium, P. vivax, P. falciparum, and P. malariae accounted for 77.8%, 17.39%, and 4.44%, respectively. In addition, there were also a certain number of falciparum malaria cases in Xinyang, Queshan, Zhumadian, and Dengxian. Since then, many malaria epidemics have occurred in Xinyang, Zhengzhou, Kaifeng, and Xichuan County in the mountainous area of southwestern Henan.
In the Yuan Dynasty, famous Medical Scientists of Danxi Zhu once listed Hubei Province as one of the places with a serious malaria epidemic. Taking Yichang as an example, malaria epidemics occurred successively in the ninth to sixteenth years of Guangxu (1883–1890), 1911, 1916, and 1938. In 1931, when the Yangtze River flooded, falciparum malaria was widespread among the malaria cases in Hankou, accounting for 69.4%. Usually, malaria cases in Hankou accounted for approximately 1.9–2.3% of the hospitalized patients, and falciparum malaria and vivax malaria accounted for approximately 40% each, with some infections of P. malariae and mixed infections.
Malaria was endemic throughout Hunan Province. During the Guangxu period of the Qing Dynasty, severe malaria epidemics occurred in Guiyang County in 1875, Jiahe in 1893, and Changde in 1901, and many cases died. After that, there were serious outbreaks of malaria in Hengnan in 1918, Guidong in 1924, Ningyuan in 1926, Huitong on the border of Hunan and Guizhou in 1931, Pingjiang in 1935, Liuyang in 1937, Leiyang in 1944, Rucheng and Linglingin 1945, Guidong in 1947, and Chenxian in 1949. Among them, the incidence of malaria among residents in Lingling and Guidong counties exceeded 50%, with many deaths in the year of the outbreak. Furthermore, the splenomegaly rate of urban primary school students in Chenxian was as high as 69%, the malaria parasite rate was 63%, and those of rural primary school students were as high as 74% and 81%, respectively, being both dominated by vivax malaria, as well as malariae malaria and falciparum malaria.
Guangxi has been also commonly suffered from malaria epidemics for many years. In 1924, more than a thousand of soldiers died of malaria in the troops in Baise, Guangxi, on their march from Guizhou to Guangdong. In 1935, Prof. Lanzhou Feng conducted surveys in 8 counties, including Enyang and Baise in Guangxi, and found that the splenomegaly rate was 3%–58%, and the malaria parasite rate was 7.1%–84.9%. In particular, falciparum malaria accounted for 59% and 37% in Enyang and Longsheng counties, respectively. In 1942, among the 33 households with 115 people in Zhelang Township, Longlin County, northwest Guangxi, 92 people from 20 households suffered from malaria, and 25 people died, of which 5 households died. It was estimated that there were no less than 5 million malaria cases in Guangxi at that time.
The area of Qiong (Hainan Island) and Lei (Leizhou Peninsula) has been called the hometown of miasma since ancient times (Office 2013; Zhang et al. 1901; Zhang 1841). The local chronicles in the Sui Dynasty recorded that “most areas in more than twenty counties in the Lingnan were under the wet and were almost suffered from miasma” (Wei 629). In the autumn of 1923, the Dongjiang River in Guangdong was flooded, and the northern soldiers stationed in Heyuan County on the right bank of the river were suffered an outbreak of malaria (Zhou 1991). Approximately 300–400 patients poured into the hospital every day, and many died. Moreover, more than 700 local residents (only more than 1000 residents in the county) also died of malaria. In addition, malaria epidemics continuously occurred in Qiongzhong County and Chengmai County on Hainan Island in 1925, Shantou City and Chaoan County in 1939, Foshan County, Taishan County, and Baisha County on Hainan Island in 1943, and Zhuhai County and Baoting County on Hainan Island in 1944 (Tang et al. 2012; Zhou 1991).
1.2.3 Malaria in Eastern China (Fujiang, Shanghai, Jiangsu, Zhejiang, Anhui, Jiangxi, and Shandong)
It was recorded that “Yubo was appointed to Central Fujian and often supported soldiers to catch mountain bandits, but the soldiers all felt malaria when they passed through Zhangpu” in “Su Shen Liang Fang” written by Kuo Shen and Shi Su in the Song Dynasty (Shen and Su). Danxi Zhu described malaria transmission in the south of the Yangtze River in China in the 12th century, with many malaria cases in Fujian, which was in line with the reality that people were more likely to suffer from malaria during the long summer. In the 34th year of Jiajing in the Ming Dynasty, General Jiguang Qi’s troops garrisoned in Pantuoling, southern Fujian, and malaria was rampant in the army, resulting in a large number of deaths of soldiers, which seriously affected the war. In 1932, Prof. Lanzhou Feng conducted malaria investigations in Xiamen and found that the rate of splenomegaly among residents was 75%, and the rates of Plasmodium infection among migrant workers and farmers in mountainous areas were 83.3% and 58.1%, respectively, of which P. falciparum accounted for 63.5%. Moreover, the sporozoite infection rate of Anopheles minimus was 8.6%, and the rate of gastric oocyst infection was 29.8%. Years later, the Fujian Provincial Health Laboratory reported in 1938 that malaria had been prevalent and spread in eastern and southern Fujian and throughout the province in those years, rather than mostly being confined to the mountainous areas of northwestern Fujian in the past. It was estimated that there were at least 4 million malaria cases throughout the year, and the fatality rate was as high as 3% according to the outpatient statistics of the county health centers at that time. In 1948, more than 30,000 people suffered from malaria in Jianning County, which accounted for almost half of the county’s population.
In Jiangsu, there was a serious epidemic of malaria in Suzhou at the beginning of the twentieth century. In the early 1920s, the prevalence of malaria among students at Soochow University was 37.8%, and P. falciparum accounted for half of the cases. According to the annual report of Suzhou Hospital in 1930, among the 249 Plasmodium-positive cases in blood tests, 39.8% were P. falciparum, 49.4% were P. vivax, and 10.8% were P. malariae. In 1930, malaria was prevalent among people from Anhui, and six other provinces went to Nanjing to build the Sun Yat-Sen Cemetery. The incidence rate reached 71.3% in 1933, of which 84.2% was the first onset after arriving in Nanjing, the rate of splenomegaly was 53.8%, and falciparum malaria accounted for 58.3%. After the Yangtze River flooded in 1931, the rate of splenomegaly was 2.5%, and the malaria parasite rate was 22.6% in 6039 Nanjing residents surveyed by the Department of Health. Moreover, falciparum malaria accounted for half of them, vivax malaria accounted for nearly half, and some sporadic malariae malaria. In the second year, 6976 residents in Nanjing and its suburbs were surveyed; 47% of them had a history of malaria, the splenomegaly rate was 18%, the malaria parasite rate was 13%, and vivax malaria accounted for 65%. However, from August to September in the same year, falciparum malaria accounted for 52%, twice as many as that in other months. Additionally, malaria cases accounted for 2.6% of hospitalized cases in Wuxi and 1.6% in Nanjing according to incomplete statistics. P. vivax malaria, falciparum malaria, and malariae malaria were found, with vivax malaria being the majority.
Zhejiang was once a province with a serious epidemic of falciparum malaria. In Wenzhou, Zhejiang, in the eighth year of Emperor Guangxu’s reign (1882), nearly half of the population was infected with malaria. After the Yangtze River flooded in 1931, the splenomegaly rate of the Hangzhou population was 7.2%, and the malaria parasite rate was 39.5%, with P. falciparum mainly accounting for 82.4%, as well as P. vivax and P. malariae according to the surveys conducted by the Department of Health in November of that year. Meanwhile, the splenomegaly rate was 23% in the population in Wukang (today’s Deqing), the malaria parasite rate was 21%, and falciparum malaria and vivax malaria were equally divided. However, vivax malaria accounted for the majority of 60%, usually followed by falciparum malaria. For instance, the proportion of falciparum malaria in local malaria cases in 1937 was 27.2% in Hangzhou, 38.9% in Ningbo, 24.0% in Wuxing, 26.5% in Shaoxing, and 20.7% in Wukang, respectively.
Malaria was endemic in Shanghai. An epidemic of vivax malaria was recorded in the tenth year of Guangxu (1884) in the Qing Dynasty. In 1931, the Yangtze River and Huaihe River flooded concurrently, and the number of malaria cases in the disaster-stricken areas along the rivers increased sharply, with the incidence rate reaching up to 60% in some areas. During the autumn and winter of this year, a survey of the victims who fled from Hankou to Shanghai found that the malaria parasite rate was 27.4%, of which P. falciparum accounted for 69.4%, P. vivax accounted for 13.7%, and P. malariae accounted for 16.9%. In 1933, in a survey of school children in Gaoqiao, a suburb of Shanghai, 34.8% of them had a history of malaria within a year, 18.4% had splenomegaly, and the malaria parasite rate was 5.2%, of which P. vivax accounted for 59.9%, and P. falciparum accounted for 6.4%. In 1936, a survey in the southwestern suburbs of the city showed that 32.7% of the residents and 42.8% of school children had a history of malaria, the rate of splenomegaly in school children was 28.9%, and the malaria parasite rate was 20%. According to the statistics of patients admitted to the hospitals in the early 1930s, the case proportion of malaria was 0.4%, with P. vivax as the main type, falciparum malaria was approximately half of the number of vivax malaria cases, and there were also malariae malaria cases and mixed infections.
In the southern Anhui and Dabie Mountains in Anhui Province, malaria has been endemic for a long time. In 1931, the Yangtze River and Huaihe River flooded, the number of malaria cases in the disaster-stricken areas along the rivers increased sharply, and the incidence rate in some areas was as high as 60%. In the winter of that year, falciparum malaria cases in Anqing City accounted for 68.6% of the malaria cases, and mixed infections with vivax malaria were also found. According to the statistics of Wuhu Hospital, malaria cases accounted for 2.8% of the total number of hospitalized patients, and the majority suffered from P. vivax, accounting for 84.5%. Meanwhile, there were a few cases infected with P. falciparum and P. malariae.
From the nineteenth year of Guangxu (1893) in the Qing Dynasty to the early years of the Republic of China, malaria continued to be prevalent in Jiangxi Province, especially in mountainous and hilly areas. In some counties in the mountainous areas of southern Jiangxi, the annual incidence of malaria reached 75–80%. In the winter of 1931, it was found that the splenomegaly rate of people in Jiujiang, Hukou, Shahe, Nanchang, and other places along the rivers was between 2.2 and 19.5%. All of the affected children in Jiujiang had cases of falciparum malaria, while those of vivax malaria were more common in Nanchang. According to data from the early 1930s, malaria cases accounted for approximately 3.4% among inpatients in Nanchang. Three types of malaria (vivax malaria, falciparum malaria, malariae malaria) were recorded; the former two types were more common, accounting for approximately 40% each, and mixed infections were also seen from time to time.
In Shandong, malaria epidemics were recorded in the Spring and Autumn Periods and the Warring States Period (Tang et al. 2012; Zhou 1991). In the 20th year of Jiaqing (1815) in the Qing Dynasty, malaria was prevalent in Juye, Caoxian, and Dongping in southwestern Shandong. The Jiaodong Peninsula in the nineteenth year of Guangxu’s reign (1893), Yantai in 1897, Dongping in 1914, and Juye in 1916 all experienced malaria epidemics. The floods in 1931 also resulted in an outbreak of malaria in Shandong. It was recorded in the local chronicles of Dongming County that “malaria was prevalent in the autumn of the 20th year of the Republic of China, with seven or eight cases out of ten persons in a village, and many of them died, and the disease persisted in the following spring.” Subsequently, the malaria epidemic occurred successively in Dong’e in 1932, Dongping in 1937, the whole southwestern Shandong region in 1942, Jinan and other places in 1947.
1.2.4 Malaria in North China (Beijing, Tianjin, Hebei, and Shanxi)
In the tenth year of Tongzhi (1871) in the Qing Dynasty, an outbreak of vivax malaria occurred due to a flood in North China. By 1873, the prevalence of malaria in Beijing and Tianjin reached its peak, with approximately 25–30% of residents getting sick. Reports in 1927 and 1936 showed that there were many cases of vivax malaria, mostly among hospitalized patients in Beijing and its suburbs and Tianjin. In the autumn of 1919, an epidemic of falciparum malaria occurred in nearby local residents of the troops from Hunan and northern Hubei and stationed at the Beijing Racecourse.
In southern Hebei, malaria was severely endemic. For instance, a serious epidemic and many people died of malaria in the ninth year of Jiajing (1530) in the Ming Dynasty were recorded in the chronicle of Xingtai area. In the annals of Lingshou County in the Shijiazhuang area, malaria was prevalent from spring to autumn in the twelfth year of Tongzhi (1873). Furthermore, malaria had spread to every village in this county, and at least one person in one household was sickened, and as many as several family members were affected by malaria from 1940 to 1944. According to a survey conducted by the Southern Hebei Office in 1946, there were more than 540,000 malaria cases in 41 counties, of which there were more than 180,000 cases in 14 counties in the Xingtai area. In 1949, it was estimated that there were 600,000 malaria cases in the province, with an incidence rate of 15 per thousand.
In Shanxi Province, it was recorded that malaria mostly occurred in Linfen, Yuncheng, and other areas in the southwest. During the Anti-Japanese War of Resistance in 1938, a local malaria epidemic was recorded in Pinglu and Ruicheng counties in the Yuncheng area. Between 1940 and 1943, the border regions and counties of Jincheng and Changzhi adjacent to Hebei and Shandong provinces experienced malaria epidemics.
1.2.5 Malaria in Northwest China (Shaanxi, Xinjiang, Gansu, Qinghai, and Ningxia)
Malaria in Shaanxi Province was prevalent in the Guanzhong Plain and south of the Qinling Mountains. According to incomplete statistics from 1940 to 1948, there were more than 47,000 malaria cases in the province, with an average annual incidence rate of 52/10,000, which were commonly distributed in Shangluo, Weinan, and other special areas, and mainly vivax malaria. However, malaria was rare or nonexistent in the northern part of the province due to drought.
In Xinjiang, malaria cases were reported in Shufu County in southern Xinjiang in 1931. Since then, malaria epidemics or malaria cases have been found in other counties in Kashgar, oases in some counties in Hotan, and counties along the Ili River Basin. Among them, the counties in the Yili region had the largest number of malaria cases, accounting for approximately 64% of the total malaria cases in the autonomous region. Moreover, malaria was scattered along the Kashgar River, Yarkand River, and Hotan River Basin.
In Gansu, Qinghai, and Ningxia, there were no or very few historical data about the prevalence of malaria, mostly due to drought or cold weather.
1.2.6 Malaria in Northeast China (Liaoning, Heilongjiang, Jilin, and Inner Mongolia)
In 1924, there was an epidemic of malaria in Tieling, Liaoning Province, and hundreds of people were affected. After the victory of the Anti-Japanese War of Resistance, malaria was brought into Liaoning with frequent population movements inside and outside the customs, coupled with the swarming transfer of the troops, which led to a severe epidemic of malaria in the local area.
According to records in Heilongjiang Province, there were local epidemics of malaria on the Songnen Plain and Sanjiang Plain. Falciparum malaria has also been found in the Heilongjiang Basin, but it was not endemic.
In Jilin and Inner Mongolia, there are no or very few historical records about malaria, mostly due to drought or cold weather.
1.3 Trend of Malaria Epidemiology in the People’s Republic of China (1949–2020)
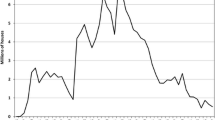
Before 1949, it was estimated that more than 30 million cases of malaria occurred nationwide each year, and mortality was approximately 1% (Tang et al. 2012). However, through sustained efforts in different control phases, malaria has declined dramatically, to less than 15,000 cases in 2009, and the endemic areas have shrunk greatly (Zhou et al. 2011b). Immediately after, the Chinese government initiated the National Malaria Elimination Programme (NMEP) in 2010, and no indigenous malaria cases have been reported since 2017. China officially achieved the elimination of malaria on June 30, 2021, contributing to the Millennium Development Goals and global eradication of malaria. However, the control and elimination of malaria in China is a tortuous road, and challenges still exist in the post-elimination phase; thus, a systematic review of its roadmap can provide a reference for countries experiencing malaria elimination.
The main objective of this section is to briefly review malaria epidemiology in the different malaria control and elimination phases in P.R. China. In general, there are five phases in the country, namely, (1) the key-point investigation and control phase (1949–1959), (2) the phase in the control of severe epidemics (1960–1979), (3) phase of reducing the incidence rate (1980–1999), (4) phase of consolidating control achievements (2000–2009), and (5) malaria elimination phase (2010–2020).
1.3.1 The Key-Point Investigation and Control Phase (1949–1959)
At the beginning of the founding of the People’s Republic of China, there was still a lack of detailed malaria epidemiological data and related information and a serious lack of specialized malaria prevention and control institutions and technical teams. Fortunately, malaria was designated a notifiable disease in 1956, a malaria-reporting mechanism was implemented nationwide, and malaria was listed as one of the diseases to be controlled and eliminated within a set time in the first 5-year National Malaria Control Programme (MOH 1956). Moreover, several baseline data on malaria epidemiology were collected through many surveys in some endemic areas for pilot studies conducted by continuously established professional bodies. In 1958, the malaria incidence rate in China dropped to 215.83/100,000, which declined by 57.2% compared with that in 1956 (505.23/100,000). In addition, four different malaria transmission zones were divided in the country, with different malaria parasite compositions and transmission seasons (MOH 1956; Tang et al. 2012; Yin et al. 2014; Zhou 1981, 1991).
1.3.2 Phase in the Control of Severe Epidemics (1960–1979)
Although the large-scale malaria outbreaks were controlled with a great reduction in malaria morbidity and mortality through the control strategy focusing on mass drug administration and infectious source control, malaria transmission in this phase was unstable, especially the pandemic transmission of vivax malaria that occurred in the Huang-Huai Plain and central China, including Jiangsu, Shandong, Henan, Anhui, and Hubei Provinces, and there were more than 18,000,000 malaria cases accumulatively reported from each of these five provinces in this phase (Shang et al. 2007; Tang et al. 2012; Zhou 1991). Furthermore, more than 1,000,000 cases were reported from Jiangxi, Zhejiang, Sichuan, Hunan, Fujian, Guangdong, Hebei, Guangxi, Shanghai, and Yunnan, and approximately 1,000,000 cases were reported in other endemic areas (Tang et al. 2012). Additionally, the malaria incidence (257.54/100,000) in 1979 declined by 91.3% compared with that in 1970.
1.3.3 Phase of Reducing Incidence Rate (1980–1999)
In this phase, the integrated control strategies dominated by infectious source management and/or vector control were adopted in mainly accordance with both malaria epidemic characteristics and the distribution of different vectors (mainly An. sinensis, An. minimus, An. dirus, and An. anthropophagus) (MOH 1983, 1984, 1986, 1990, 1996). As a result, malaria transmission declined gradually, with case reduction rates of 30–43% during 1982–1988 (Expert Advisory Committee on Parasitic Diseases 1988, 1989; Malaria Commission 1984, 1985, 1986, 1987; MOH 1983, 1986) and approximately 15–25% during 1990–1996, except for 1994 (Expert Advisory Committee on Malaria 1993, 1994; Expert Advisory Committee on Malaria 1995; Expert Advisory Committee on Parasitic Diseases 1991, 1992, 1996, 1997). Moreover, more than 40% of cases were reported from the above five provinces in central China in the first 10 years, while more than 40% of cases were from southern China in the latter 10 years. In endemic areas, P. vivax was the predominant malaria parasite species and was widely distributed, and the transmission of P. falciparum was successfully blocked in central China in 1995 and has been confined to Yunnan and Hainan Provinces since 1995 (Expert Advisory Committee on Parasitic Diseases 1996, 1997). By 1999, a total of 1321 counties and cities with an incidence rate less than 1 per 10 000 individually, had been confirmed to meet the standard of “effective malaria elimination” (Expert Advisory Committee on Malaria 2000). In addition, malaria deaths dramatically decreased, with less than 70 deaths reported annually.
1.3.4 Phase of Consolidating Control Achievements (2000–2009)
Malaria transmission was unstable, with an incidence between 0.11 per 10,000 and 0.49 per 10,000 in this phase (Expert Advisory Committee on Malaria, 2001; Sheng et al. 2003; Zhou et al. 2005; Zhou et al. 2006a; Zhou et al. 2008, 2009; Zhou et al. 2006b, 2007; Zhou et al. 2011b). Particularly, a resurgence of vivax malaria occurred in Anhui, Henan, Hubei, and Jiangsu Provinces along the Huang-Huai River but was effectively controlled in 2008 through the control strategy of timely diagnosis and standardized treatment with the strengthened mass antimalarial drug administration for risk groups, vector control, and health education. Furthermore, the direct reporting of any malaria case within 24 h after the finding was realized through the Chinese Information System for Disease Control and Prevention, which was established in 2004. However, there were a large number of suspected malaria cases nationwide. The transmission of P. falciparum was still confined to Yunnan and Hainan Provinces and has been interrupted in Hainan since 2010 (Zhou et al. 2011a; Zhou et al. 2011b). Even greater success was that a total of 1687 counties, cities, and districts had not reported 1 indigenous malaria case for at least 3 consecutive years by 2009 (Zhou et al. 2008, 2009, 2011b), and only four counties throughout the country were at an incidence rate of more than 10/10,000. Additionally, less than 100 deaths due to malaria were reported annually.
1.3.5 Malaria Elimination Phase (2010–2020)
The Chinese government initiated the National Malaria Elimination Programme (NMEP) in 2010 with the issue of the “Action Plan for Malaria Elimination in China (2010–2020)” (MOH 2010), and counties in China were stratified into four types (Type I–IV) based on the malaria epidemic reports of 2006–2008, and specific strategies were implemented in each type stratum for better resource allocation (Yin et al. 2013). In 2011, malaria surveillance information management was greatly improved by the establishment of the “National Information Management System for Parasitic Disease Control and Prevention” (Feng et al. 2014). Moreover, a strategy focusing on the “1-3-7” approach in surveillance and response based on the nature of malaria transmission and the biological characteristics of malaria parasites was put forward and implemented successfully between 2013 and 2020 (Cao et al. 2014). In addition, the national malaria diagnosis reference laboratory network has been under establishment since 2011 and has historically covered malaria-endemic provinces by 2016, mainly responsible for the quality control and assurance, training, and maintenance of laboratory competency in malaria parasitological testing (Yin et al. 2022a; Yin et al. 2015). As a result, indigenous cases significantly declined from 1308 in 2011 to 36 in 2015, and the last case was reported from Yunnan Province in April 2016 (Huang et al. 2022), although thousands of imported cases still occur annually and are extensively distributed in every province and each month (Zhang et al. 2019b). Such achievements were inseparable from the high-quality implementation of the “1-3-7” approach, with a full percentage of malaria cases reported within 24 h, 94.5% of them investigated within three days after case reporting, and 93.4% of foci disposed within a week after case reporting (Huang et al. 2022). In addition, each historically malaria-endemic province successfully passed the subnational verification of malaria elimination.
1.4 Conclusions and Perspectives
Malaria has a long history in China and was widely distributed in most parts of the country. Four types of local malaria parasites have been recorded, among which P. vivax and P. falciparum were the main parasites that seriously threaten people’s health. From ancient times to the present, the Chinese nation has made important contributions to the fight against malaria, especially traditional Chinese medicine represented by artemisinin. In addition, after the founding of the People’s Republic of China, with nearly 70 years of tremendous investments and intensive interventions, no indigenous malaria cases have been reported since 2017, and China officially achieved the elimination of malaria on June 30, 2021 (Feng et al. 2021; Zhou 2021), contributing to the global eradication of malaria. However, thousands of imported cases were reported annually and were extensively distributed in China, particularly in historically malaria-endemic areas; thus, China will likely see a resurgence in malaria cases if there is persistent importation of malaria cases under the condition that the distribution of the malaria vector Anopheles mosquitoes in the defined areas. Therefore, there are still some technical and managerial challenges in the post elimination of malaria in China.
1.4.1 High Burden of Imported Cases, Including Border Malaria
Before the COVID-19 pandemic, approximately 3000 cases annually were reported mainly from Africa and Southeast Asia (Huang et al. 2022), with P. falciparum being the most prevalent, followed by P. vivax, and the proportion of P. ovale has been on the rise for several years and was widely distributed across China throughout the year, particularly in historically malaria-endemic provinces (Zhang et al. 2019b). Moreover, China is severely suffered from border malaria, especially in counties on the China–Myanmar border (Huang et al. 2021a; Huang et al. 2021b; Xu et al. 2021). In addition, malaria infection caused by the bite of positive Anopheles mosquitoes after crossing the border has been found at a Chinese construction site on the China–Myanmar border (Yin et al. 2022b).
1.4.2 Undetermined Sources of Malaria Infection
Asymptomatic malaria infections are easily missed by traditional diagnostics in all intensities of malaria transmission, but they contribute far more to the malaria reservoir than previously thought, resulting in the continuous spread of malaria, and symptomatic cases are just the tip of the iceberg of malaria transmission (Cheaveau et al. 2019). Meanwhile, all Plasmodium species have asymptomatic infections (Roucher et al. 2014; Tadesse et al. 2017), and asymptomatic infections of P. falciparum and P. vivax have been reported in some Chinese border counties on the China–Myanmar border (Huang et al. 2017), but no data have been reported in other areas. In addition, the gene deletion of P. falciparum histidine-rich protein (HRP) 2/3 making the RDT detection reagent based on HRP2unable to detect P. falciparum very well has been reported in an increasing number of countries around the world, especially African countries (WHO 2021a), but Africa is the main source of imported cases in China.
1.4.3 Maintenance of Human Resources for Prevention of Malaria Re-Establishment
As a disease is eliminated, there may be less attention to it and fewer resources. However, there is a high risk of malaria re-establishment in China if imported malaria cases cannot be found under the condition that the distribution of the malaria vector Anopheles mosquitoes in the defined areas, and the introduced cases have been reported in China and abroad (Sun et al. 2017; Wang et al. 2015; Zhang et al. 2019a). In response to the prevention of malaria re-establishment, human resources for timely detection and appropriate treatment of imported cases, investigation and assessment of transmission risk caused by imported cases, and timely handling of foci or susceptible populations with a re-established transmission risk should be maintained and strengthened (Nasir et al. 2020; Yin et al. 2022b).
In summary, it is essential to maintain and strengthen the sensitivity of surveillance and response to imported malaria through capacity building of malaria diagnosis and treatment, case investigation, laboratory confirmation, epidemiological investigation, and foci disposal, as well as the research and development of new technologies, based on the established and improved multisectoral cooperative mechanism under the unified leadership of the government, thereby effectively consolidating the achievements of malaria elimination in China.
References
Cao J, Sturrock HJ, Cotter C, Zhou S, Zhou H, Liu Y, Tang L, Gosling RD, Feachem RG, Gao Q (2014) Communicating and monitoring surveillance and response activities for malaria elimination: China’s “1-3-7” strategy. PLoS Med 11:e1001642
Cheaveau J, Mogollon DC, Mohon MAN, Golassa L, Yewhalaw D, Pillai DR (2019) Asymptomatic malaria in the clinical and public health context. Expert Rev Anti-Infect Ther 17:997–1010
Chen C (2014) Development of antimalarial drugs and their application in China: a historical review. Infect Dis Poverty 3:9
Cox FE (2010) History of the discovery of the malaria parasites and their vectors. Parasit Vectors 3:5
Cunha CB, Cunha BA (2008) Brief history of the clinical diagnosis of malaria: from Hippocrates to Osler. J Vector Borne Dis 45:194–199
Expert Advisory Committee on Malaria, MoH (1993) [Malaria situation in the People’s Republic of China in 1992]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 11:161–164
Expert Advisory Committee on Malaria, MoH (1994) [Malaria situation in the People’s Republic of China in 1993]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 12:161–164
Expert Advisory Committee on Malaria, MoH (1995) [Malaria situation in the People’s Republic of China in 1994]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 13:161–164
Expert Advisory Committee on Malaria, MoH (2000) [Malaria situation in the People’s Republic of China in 1999]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 18:129–131
Expert Advisory Committee on Malaria, MoH (2001) Malaria situation in the People’s Republic of China in 2000. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 19:257–259
Expert Advisory Committee on Parasitic Diseases, MoH (1988) [Malaria situation in China, 1987]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 6:241–244
Expert Advisory Committee on Parasitic Diseases, MoH (1989) [Malaria situation in China, 1988]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 7:241–244
Expert Advisory Committee on Parasitic Diseases, MoH (1991) [Malaria situation in the People’s Republic of China in 1990]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 9:250–253
Expert Advisory Committee on Parasitic Diseases, MoH (1992) [Malaria situation in the People’s Republic of China in 1991]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 10:161–165
Expert Advisory Committee on Parasitic Diseases, MoH (1996) [Malaria situation in the People’s Republic of China in 1995]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 14:169–172
Expert Advisory Committee on Parasitic Diseases, MoH (1997) [Malaria situation in the People’s Republic of China in 1996]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 15:129–132
Feng J, Zhang L, Xia ZG, Zhou SS, Xiao N (2021) Malaria-free certification in China: achievements and lessons learned from the National Malaria Elimination Programme. Zoonoses 1. https://doi.org/10.15212/ZOONOSES-2021-1002
Feng XY, Xia ZG, Vong S, Yang WZ, Zhou SS (2014) Surveillance and response to drive the national malaria elimination program. Adv Parasitol 86:81–108
Ge H (300–400 A.D.) [A handbook of prescriptions for emergencies]
Guang SM (2012) Comprehensive mirror for aid in government. China Pictorial Publishing House, Beijing
Hempelmann E, Krafts K (2013) Bad air, amulets and mosquitoes: 2,000 years of changing perspectives on malaria. Malar J 12:232
Huang F, Feng XY, Zhou SS, Tang LH, Xia ZG (2022) Establishing and applying an adaptive strategy and approach to eliminating malaria: practice and lessons learnt from China from 2011 to 2020. Emerg Microbes Infect 11:314–325
Huang F, Li SG, Tian P, Guo XR, Xia ZG, Zhou SS, Zhou HN, Zhou XN (2021a) A retrospective analysis of malaria epidemiological characteristics in Yingjiang County on the China-Myanmar border. Sci Rep 11:14129
Huang F, Takala-Harrison S, Liu H, Xu JW, Yang HL, Adams M, Shrestha B, Mbambo G, Rybock D, Zhou SS et al (2017) Prevalence of clinical and subclinical Plasmodium falciparum and Plasmodium vivax malaria in two remote rural communities on the Myanmar-China border. Am J Trop Med Hyg 97:1524–1531
Huang F, Zhang L, Tu H, Cui YW, Zhou SS, Xia ZG, Zhou HN (2021b) Epidemiologic analysis of efforts to achieve and sustain malaria elimination along the China-Myanmar border. Emerg Infect Dis 27:2869–2873
Litsios S (2020) The World Health Organization’s changing goals and expectations concerning malaria, 1948-2019. Hist Cienc Saude Manguinhos 27:145–164
Malaria Commission, C.o.M.S. (1984) [Malaria control and morbidity in China in 1982]. Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 2:1–2
Malaria Commission, C.o.M.S. (1985) [The malaria situation in 1984 in the People’s Republic of China]. Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 3:241–243
Malaria Commission, C.o.M.S. (1986) [The malaria situation in China, 1985]. Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 4:241–243
Malaria Commission, C.o.M.S. (1987) [Malaria situation in China. 1986]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 5:241–243
MOH (1956) [Malaria control programme]
MOH (1983) [Malaria control programme in China, 1983–1985]
MOH (1984) [Malaria control management regulation]
MOH (1986) [Malaria control programme in China, 1986–1990]
MOH (1990) [Malaria control programme in China, 1991–1995]
MOH (1996) [Malaria control programme in China, 1996–2000]
MOH (2010) [Action Plan of China Malaria Elimination (2010–2020)]
Nasir SMI, Amarasekara S, Wickremasinghe R, Fernando D, Udagama P (2020) Prevention of re-establishment of malaria: historical perspective and future prospects. Malar J 19:452
Office, HPLC (2013) Annals of Hainan Province: Annals of Science and Technology. Chapter 6: Medical and health technology. Section 3: Disease prevention and control
Roucher C, Rogier C, Sokhna C, Tall A, Trape JF (2014) A 20-year longitudinal study of Plasmodium ovale and Plasmodium malariae prevalence and morbidity in a West African population. PLoS One 9:e87169
Shang LY, Chen JS, Li DF, Li P, Su YP, Liu H (2007) Studies on distribution, ecological feature and malaria transmission effect of Anopheles anthropophagus in Henan province, China. J Pathog Biol 2:304–306
Shen K, Su S (960-1127 AD) [Su Shen Liang Fang]
Sheng HF, Zhou SS, Gu ZC, Zheng X (2003) [Malaria situation in the People’s Republic of China in 2002]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 21:193–196
Sun YW, Yu DM, Chen J, Li X, Wang B, Wang ZJ, Mao LL, Yao WQ (2017) Two individual incidences of vivax malaria in Dandong municipality of Liaoning province. Chin J Public Health 33:314–316
Tadesse FG, van den Hoogen L, Lanke K, Schildkraut J, Tetteh K, Aseffa A, Mamo H, Sauerwein R, Felger I, Drakeley C et al (2017) The shape of the iceberg: quantification of submicroscopic Plasmodium falciparum and Plasmodium vivax parasitaemia and gametocytaemia in five low endemic settings in Ethiopia. Malar J 16:99
Talapko J, Skrlec I, Alebic T, Jukic M, Vcev A (2019) Malaria: the past and the present. Microorganisms 7:179
Tang LH, Xu LQ, Chen YD (2012) Parasitic disease control and research in China. Beijing Science & Technology Press, Beijing
Tu Y (2011) The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat Med 17:1217–1220
Tu Y (2016) Artemisinin-A gift from traditional Chinese medicine to the world (nobel lecture). Angew Chem 55:10210–10226
Wang D, Li S, Cheng Z, Xiao N, Cotter C, Hwang J, Li X, Yin S, Wang J, Bai L et al (2015) Transmission risk from imported Plasmodium vivax malaria in the China-Myanmar border region. Emerg Infect Dis 21:1861–1864
Wei Z (629) [Sui Chronicle]
WHO (2021a) Statement by the Malaria Policy Advisory Group on the urgent need to address the high prevalence of pfhrp2/3 gene deletions in the Horn of Africa and beyond
WHO (2021b) World Malaria Day: WHO launches effort to stamp out malaria in 25 more countries by 2025
WHO (2021c) World Malaria Report 2021. World Health Organization, Geneva
WHO (2021d) Zeroing in on malaria elimination: final report of the E-2020 initiative. World Health Organization, Geneva
Xu JW, Lin ZR, Zhou YW, Lee R, Shen HM, Sun XD, Chen QY, Duan KX, Tian P, Ding CL et al (2021) Intensive surveillance, rapid response and border collaboration for malaria elimination: China Yunnan’s “3 + 1” strategy. Malar J 20:396
Yin J, Li M, Yan H, Zhou S, Xia Z (2022a) Laboratory diagnosis for malaria in the elimination phase in China: efforts and challenges, vol 16. Front Med, p 10
Yin J, Yan H, Li M (2022b) Prompt and precise identification of various sources of infection in response to the prevention of malaria re-establishment in China. Infect Dis Poverty 11:45
Yin JH, Yan H, Huang F, Li M, Xiao HH, Zhou SS, Xia ZG (2015) Establishing a China malaria diagnosis reference laboratory network for malaria elimination. Malar J 14:40
Yin JH, Yang MN, Zhou SS, Wang Y, Feng J, Xia ZG (2013) Changing malaria transmission and implications in China towards National Malaria Elimination Programme between 2010 and 2012. PLoS One 8:e74228
Yin JH, Zhou SS, Xia ZG, Wang RB, Qian YJ, Yang WZ, Zhou XN (2014) Historical patterns of malaria transmission in China. Adv Parasitol 86:1–19
Zhang L, Feng J, Zhang SS, Xia ZG, Zhou SS (2019a) Epidemiological characteristics of malaria and the progress towards its elimination in China in 2018. Chin J Parasit Parasitic Dis 37:241–247
Zhang SS, Feng J, Zhang L, Ren X, Geoffroy E, Manguin S, Frutos R, Zhou SS (2019b) Imported malaria cases in former endemic and non-malaria endemic areas in China: are there differences in case profile and time to response? Infect Dis Poverty 8:61
Zhang Y, Xing DL, Zhao YQ (1901) [Yazhou Chronicle]
Zhang YS (1841) [Daoguang Qiongzhou Prefecture Chronicle]
Zhou SS, Tang LH, Sheng HF (2005) [Malaria situation in the People’s Republic of China in 2003]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 23:385–387
Zhou SS, Tang LH, Sheng HF, Wang Y (2006a) [Malaria situation in the People’s Republic of China in 2004]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 24:1–3
Zhou SS, Wang Y, Fang W, Tang LH (2008) [Malaria situation in the People’s Republic of China in 2007]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 26:401–403
Zhou SS, Wang Y, Fang W, Tang LH (2009) [Malaria situation in the People’s Republic of China in 2008]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 27:457, 455–456
Zhou SS, Wang Y, Li Y (2011a) [Malaria situation in the People’s Republic of China in 2010]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 29:401–403
Zhou SS, Wang Y, Tang LH (2006b) [Malaria situation in the People’s Republic of China in 2005]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 24:401–403
Zhou SS, Wang Y, Tang LH (2007) [Malaria situation in the People’s Republic of China in 2006]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 25:439–441
Zhou SS, Wang Y, Xia ZG (2011b) [Malaria situation in the People’s Republic of China in 2009]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 29:1–3
Zhou XN (2021) China declared malaria-free: a milestone in the world malaria eradication and Chinese public health. Infect Dis Poverty 10:98
Zhou ZJ (1981) The malaria situation in the People’s Republic of China. Bull World Health Organ 59:931–936
Zhou ZJ (1991) Malaria control and research in China. People’s Medical Publishing House, Beijing
Zuo QM [Zuo Spring and Autumn Period]. https://so.gushiwen.cn/mingjus/default.aspx?tstr=%e5%b7%a6%e4%bc%a0
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yin, J. (2023). Malaria Epidemiology in China: A Historical Review. In: Mehlhorn, H., Li, J., Wu, K. (eds) Malaria Control and Elimination in China. Parasitology Research Monographs, vol 18. Springer, Cham. https://doi.org/10.1007/978-3-031-32902-9_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-32902-9_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-32901-2
Online ISBN: 978-3-031-32902-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)