Abstract
Idiopathic granulomatous mastitis is a rare granulomatous inflammation of the breast. Granulomatous mastitis of the breast was first described by Milward and Gough in 1970. A similar definition was redefined by Kessler and Wolloch in 1972, while Cohen detailed it in 1977.The etiology of idiopathic granulomatous mastitis (IGM), which is an entity that has been known for about 5 decades, is still unknown, the diagnosis is made by distinguishing it from other granulomatous inflammations of the breast, and also, an ideal approach for its treatment has not been established yet. In this book, all the features of IGM are reviewed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Milward and Gough [1] described granulomatous lesions in the breast that were confused with breast carcinoma in 1970. The entity “idiopathic granulomatous mastitis” (IGM) was first reported by Kessler and Wolloch [2] in five cases. These patients were defined as cases with suspected breast cancer, but characterized by granulomas and abscesses on pathological examination. Later in 1977, Cohen [3] detailed this clinical entity.
Many factors such as α1-antitrypsin deficiency, oral contraceptive drug use, smoking, pregnancy, childbirth and breastfeeding, hyperprolactinemia, ethnic origin, and autoimmunity have been blamed in the etiopathogenesis of IGM until today. However, the etiopathogenesis has not been explained exactly yet. Recently, some associations and findings in IGM, such as coexistence with erythema nodosum and arthritis, which are more common in rheumatological diseases such as Sjögren’s syndrome, and the increase in the use of steroids in treatment, suggest autoimmunity and immune dysregulation more likely in the etiopathogenesis [4,5,6,7,8,9,10,11].
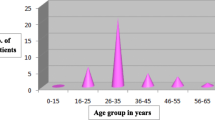
Idiopathic granulomatous mastitis is a mysterious disease that continues to attract many researchers’ attention, with many unknowns. Unfortunately, the pathogenesis and an ideal treatment approach of IGM, a disease known for nearly half a century, are still unknown. Many unknowns about the etiology of the disease also persist. For example, these questions should be answered: (i) Why is IGM more frequently observed in countries such as Turkey, China, South Korea, and Saudi Arabia? (ii) Why is it more common in premenopausal women? As emphasized above, although it has been known for half a century as a clinical entity, it still remains as a mystery.
2 Definition
There are various causes of granulomatous inflammation in the breast. The conditions that cause granulomas are shown in Table 1 [5, 12,13,14].
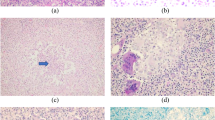
Generally, idiopathic granulomatous mastitis, a rare disease, may be confused with breast carcinomas. Patients with IGM present with a mass accompanied by inflammation manifestations such as erythema and pain. In order to diagnose IGM, histologically, there should be a non-caseous granulomatous inflammation. In addition, other causes of granulomatous inflammation should be ruled out including infectious diseases such as tuberculosis, fungi, parasites, or a systemic granulomatous disease, for example, sarcoidosis and Wegener’s granulomatosis [5, 10, 12,13,14]. Briefly, IGM is a diagnosis of exclusion when other causes of granulomatous mastitis cannot be detected after demonstrating non-caseous granulomas histopathologically. The pathological features of IGM are discussed in detail in the “pathology and differential diagnosis” section.
3 Historical Perspective
Granulomatous mastitis was first defined by Milward and Gough [1]. In 1967, the authors performed a biopsy on a patient with a clinical suspicion of breast cancer. They froze this section; however, they could not find any evidence of carcinoma in the patient.
Pathologically, they found granulomatous inflammation in the patient. The authors retrospectively reviewed 691 patients who underwent local or radical mastectomy with a clinical diagnosis of breast cancer between 1960 and 1967 at United Oxford Hospitals. During this period, no evidence of breast carcinoma was detected in eight patients who were operated with a clinical diagnosis of breast carcinoma. The authors found a condition unlike the known noninfective inflammatory breast diseases including fat necrosis and periductal mastitis in four patients. There was a condition in the breast that was accompanied by granulomatous inflammation.
In 1972, Kessler and Wolloch [2] described five patients who were clinically similar to breast carcinoma, but had no evidence of breast carcinoma on pathological examination, similar to Milward and Gough [1]. Multiple granulomas and abscesses were observed in these patients. All patients were women in childbearing age, and they had given birth. The age of the patients was found to be between 27 and 40 years.
In two patients, a preoperative punch biopsy had been performed and they were diagnosed with carcinoma and received preoperative radiotherapy. However, as a result of the definitive surgery of these two patients, no finding of carcinoma had been found. “Lipid crystals” were investigated to rule out fat necrosis. In addition, Ziehl-Neelsen stain for acid-fast bacilli, Gram staining for bacteria, and periodic acid-Schiff reaction for fungi were used. No positivity was found in any of the patients. In conclusion, Kessler and Wolloch [2] used the term “idiopathic granulomatous mastitis” for the first time.
Cohen [3] reviewed 67 patients diagnosed with granulomatous tuberculosis, or fungal mastitis, and revealed five patients with granulomatous mastitis as described by Kessler and Wolloch [2]. The patients with granulomatous mastitis that fit the definition of Kessler and Wolloch accounted for 7.5% of all granulomatous mastitis patients. Cohen’s patients were young women of childbearing age, as were the patients of Kessler and Wolloch [2]. The patients’ age ranged between 17 and 34 years old. Cohen [3] described the pathological characteristics of patients with idiopathic granulomatous mastitis.
References
Milward TM, Gough MH. Granulomatous lesions in the breast presenting as carcinoma. Surg Gynecol Obstet. 1970;130:478–82.
Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58:642–6. https://doi.org/10.1093/ajcp/58.6.642.
Cohen C. Granulomatous mastitis. A review of 5 cases. S Afr Med J. 1977;52:14–6.
Akın M, Karabacak H, Esendağlı G, Yavuz A, Gültekin S, Dikmen K, et al. Coexistence of idiopathic granulomatous mastitis and erythemanodosum: successful treatment with corticosteroids. Turk J Med Sci. 2017;47:1590–2. https://doi.org/10.3906/sag-1611-100.
Altintoprak F, Kivilcim T, Ozkan OV. Aetiology of idiopathic granulomatous mastitis. World J Clin Cases. 2014;2:852–8. https://doi.org/10.12998/wjcc.v2.i12.852.
Benson JR, Dumitru D. Idiopathic granulomatous mastitis: presentation, investigation and management. Future Oncol. 2016;12:1381–94. https://doi.org/10.2217/fon-2015-0038.
Sheybani F, Naderi HR, Gharib M, Sarvghad M, Mirfeizi Z. Idiopathic granulomatous mastitis: long-discussed but yet-to-be-known. Autoimmunity. 2016;49:236–9. https://doi.org/10.3109/08916934.2016.1138221.
Vural S, Ertop P, Ceyhan K, Şanli H. An unusual cause of oligoarthritis and erythema nodosum: idiopathic granulomatous mastitis. Arch Rheumatol. 2017;32:71–5. https://doi.org/10.5606/ArchRheumatol.2017.5952.
Yazigi G, Trieu BH, Landis M, Parikh JG, Mangal M. Granulomatous mastitis: a rare case with Sjogren's syndrome and complications. Cureus. 2019;11:e5359. https://doi.org/10.7759/cureus.5359.
Yin Y, Liu X, Meng Q, Han X, Zhang H, Lv Y. Idiopathic granulomatous mastitis: etiology, clinical manifestation, diagnosis and treatment. J Investig Surg. 2022;35(3):709–20. https://doi.org/10.1080/08941939.2021.1894516.
Zabetian S, Friedman BJ, McHargue C. A case of idiopathic granulomatous mastitis associated with erythema nodosum, arthritis, and reactive cough. JAAD Case Rep. 2016;2:125–7. https://doi.org/10.1016/j.jdcr.2016.01.011.
Bakaris S, Yuksel M, Ciragil P, Guven MA, Ezberci F, Bulbuloglu E. Granulomatous mastitis including breast tuberculosis and idiopathic lobular granulomatous mastitis. Can J Surg. 2006;49:427–30.
Hoda SA. Inflammatory and reactive tumors. In: Hoda SA, Koerner FC, Brogi E, Rosen PP, editors. Rosens’s breast pathology. 4th ed. Philadelphia: Wolters Kluwer; 2015a. p. 37–77.
Hoda SA. Inflammatory and reactive tumors. In: Hoda SA, Koerner FC, Brogi E, Rosen PP, editors. Rosens’s breast pathology. 4th ed. Philadelphia: Wolters Kluwer; 2015b. p. 79–94.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Koksal, H. (2023). Overview on Idiopathic Granulomatous Mastitis. In: Koksal, H., Kadoglou, N. (eds) Idiopathic Granulomatous Mastitis. Springer, Cham. https://doi.org/10.1007/978-3-031-30391-3_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-30391-3_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-30390-6
Online ISBN: 978-3-031-30391-3
eBook Packages: MedicineMedicine (R0)