Abstract
The first data on the successful treatment of ROP became known in 1990 thanks to the multicenter CRYO-ROP study, where transscleral cryocoagulation was used as a treatment for the threshold stage of ROP. This study compared results of cryotherapy with no treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
The first data on the successful treatment of ROP became known in 1990 thanks to the multicenter CRYO-ROP study, where transscleral cryocoagulation was used as a treatment for the threshold stage of ROP [1]. This study compared the results of cryotherapy with no treatment. The follow-up of the study lasted for 15 years (examinations were carried out at 3 months, 1; 3.5; 5.5; 10 and 15 years), thus providing the first data on the long-term structural and functional parameters of ROP treatment [2]. CRYO-ROP data showed that in 3 months after cryotherapy, there were fewer undesirable structural outcomes, including retinal detachment in the treatment group than in the naturally occurring ROP group. However, the percentage of eyes with adverse outcomes increased over time in both groups: from 25.1% at one year to 30.0% at 15 years in the group of children receiving cryotherapy; from 44.7% to 51.9% in the group with natural ROP, which prompted the search for new more effective treatment methods [1, 2].
With the advent of laser technologies, a new method of ROP treatment—laser photocoagulation of avascular zones of the retina, gradually began to be introduced into practice [3]. According to long-term structural and functional results, laser coagulation was less traumatic and more effective treatment method than cryotherapy. According to a randomized study of patients with bilateral threshold ROP conducted by Connolly et al., in which cryocoagulation was performed in one eye and transpupillary diode laser photocoagulation—in the fellow eye, the effectiveness of laser treatment exceeded 6,91 times the effectiveness of cryocoagulation during the observation period of 4.3–7.6 years. At the same time, after laser photocoagulation of the retina, higher visual functions are noted, which was also a great advantage of using laser when treating ROP [4]. Differences between laser photocoagulation of the retina and cryocoagulation were most noticeable in eyes with ROP localization in zone I; a favorable anatomical result was observed in 83% of cases of laser treatment, cryocoagulation—only in 25% of eyes with ROP in zone I. After laser photocoagulation, a significantly better indicator of visual acuity was achieved compared with cryotherapy [5]. When performing laser intervention, the risk of postoperative systemic and ocular complications is minimal compared to cryotherapy. In addition, laser applications are visible during treatment, which minimizes the risk of missing areas, that need treatment. Thus, laser photocoagulation of the avascular areas of the retina over the next 10 years almost completely supplanted cryotherapy.
Because of the development and introduction into clinical practice of less invasive methods of treatment, transconjunctival and transpupillary diode laser photocoagulation of the retina has become widely used. But in view of the fact, that a large number of complications were observed during treatment at the threshold stage of ROP, it became necessary to conduct a new large-scale study, during which results of ROP treatment using laser photocoagulation of avascular zones of the retina would be evaluated before the threshold stage of the disease sets in [6]. This is how the study on early treatment of ROP, ETROP, has evolved [6, 7].
The aim of ETROP was to study the effect of early ROP treatment on retinal structural changes and visual acuity. To do this, 401 children with a high risk of progression of bilateral ROP underwent laser photocoagulation of the retina in one eye at the prethreshold stage, in the pair - traditionally (the control group), that is, at the stage of the development of threshold ROP (in 84 cases of asymmetric ROP of high risk, eyes were randomized to early or conventional treatment). As a result of laser photocoagulation by the 9th month of life, functional (visual acuity according to Teller Table) and structural results of treatment were evaluated in 372 children (on 664 and 659 eyes). The highest percentage of ROP cases was recorded with stage 3 in zone II with “Plus” disease (42.1% in the group, where treatment was carried out at the prethreshold stage, and 43.7% in the control group), as well as with stage 1–2 in zone I with no “Plus” disease (27.4% in the group, where treatment was carried out at the prethreshold stage, and 26.1% in the control group). By 9 months of age, there was a significant functional and structural outcome in the high-risk ROP group treated at the prethreshold stage compared with the group treated later (14.3 and 19.8%, (p < 0.005); 9.0% and 15.6%, (p < 0.001)). When evaluating the functional result, a significant difference in the treatment performed at the prethreshold stage rather than at the threshold was noted in eyes with stage 3 ROP in zone I with or without “Plus” disease (30.8% had an unfavorable result versus 53.8%); a relatively significant difference was noted in children with stage 1–2 ROP in zone I without “Plus” disease (10.5% vs. 15.8%), with stage 3 ROP in zone II with “Plus” disease (15.3% vs. 18.0%), with stage 2 ROP in zone II with “Plus” disease (14.7% vs. 17.6%); insignificant difference in children with ROP stage 1–2 in zone I with “Plus” disease (22.2% of adverse outcome for both groups) and ROP stage 3 in zone II without “Plus” disease (no cases of adverse outcome for both groups). When evaluating the structural result, a significant difference in the treatment performed at the prethreshold stage rather than at the threshold was noted in eyes with stage 3 ROP in zone I with or without “Plus” disease (29.6% had an unfavorable result versus 55.6%); a relatively significant difference was noted in children with stage 1–2 ROP in zone I without “Plus” disease (2.7% vs. 9.3%), with stage 3 ROP in zone II with “Plus” disease (7.3% vs. 10.9%); insignificant difference in children with stage 2 ROP in zone II with “Plus” disease (20.6% for both groups), stage 1–2 ROP in zone I with “Plus” disease (22.2% adverse outcome for both groups) [6].
After careful analysis of the data of the ETROP study, two groups of patients with prethreshold ROP were identified: type I (patients in need of early treatment), type II (patients, who can be observed). Such a division into types was not provided before the start of the study and was its result. The analysis of the obtained data became the basis for the creation of a clinical algorithm, where the type I and type II of prethreshold ROP is an indication for either treatment or observation. With the development of type I ROP (zone I, any stage of ROP with signs of “Plus” disease; zone I, stage 3 ROP with or without signs of “Plus” disease; zone II, stage 2 or 3 ROP with signs of “Plus” disease) laser photocoagulation of the retina should be performed. In cases of the development of type II ROP (zone I, stage 1 or 2 ROP without “Plus” disease or zone II, stage 3 ROP without “Plus” disease), it is recommended to continue monitoring and start laser photocoagulation only when the disease progresses into type I.
Clinical use of separating ROP cases into type I and II reduces the number of patients in need of treatment. For type I ROP, this indicator was 31.5%, for type II—77.3% of cases. Thus, the effectiveness of early treatment was statistically proved only for type I ROP [6].
Results of the state of the retina in 6 years confirmed the effectiveness of early treatment of ROP at the prethreshold stage of the disease (type I). Positive dynamics was noted at 6 and 9 months of age and persisted up to 6 years. Thanks to the use of early treatment, high rates of visual acuity were recorded. In 65.4% of cases, its number averaged 0.5. Whether this is due to retinal, cortical, or both groups of factors, it remains unclear.
Thus, early treatment of ROP is most preferable for a number of patients, although it is not always a guarantee of a favorable outcome of ROP and sufficient visual acuity [7].
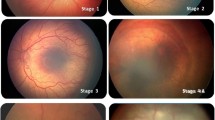
According to Katsan, Pasyechnikova, Adakhovska and others, the effectiveness of the method of retinal laser photocoagulation in ROP is 95.3 ± 1.2% [8]. For treatment, laser with a wavelength of 532 nm was used. Coagulation was carried out throughout avascular retina in front of the ridge, and so that, burns were located at a distance of 0.5 of the width of the burn from each other, while achieving a confluent pattern of applying coagulates. Figure 12.1 shows confluent laser photocoagulation in zones II and III, performed using a diode-pumped Purepoint Laser semiconductor laser with a wavelength of 532 nm.
The model according to which laser photocoagulation of the retina is carried out depends on the choice of the doctor. There is no final consensus regarding the degree of intensity and the interval between applications. However, over time there is a tendency to perform denser retinal coagulation in ROP. In a number of studies, Banach et al. [9], performing laser photocoagulation of the retina in the localization of the pathological process in zone I and II at threshold stages of ROP, it was found that during confluent laser photocoagulation of the retina, the frequency of ROP progression was 3.6% and when applying laser coagulates at a distance of 1–1.5 coagulate diameter—29%. The results indicated, that confluent laser photocoagulation of the retina leads to regression of ROP in a greater percentage of cases and reduces the rate of disease progression when the process is localized in zone II [9]. Similar data were obtained by Axer-Siegel et al. [10] in confluent laser photocoagulation of the retina with ROP localization in zone I and posterior part of zone II when disease regression was achieved in 85.4%. Eye complications—edema, chemosis and maceration of the conjunctiva, the development of cataract, hemorrhages both in the outer and inner membranes, the formation of preretinal membranes, proliferation in the optic disc, macula and rarely on the periphery of the retina, iridocyclitis, closure of the anterior chamber angle with increased intraocular pressure, are comparable for both confluent laser photocoagulation and coagulation with a scattered pattern [10]. The problem of this method is the violation of peripheral vision. According to Quinn et al., treatment at the prethreshold stage of ROP preserves peripheral vision with only a slight decrease in visual field than if treated at the threshold stage [11]. According to McLoon et al., the extent of the visual fields in the eyes using laser photocoagulation of the retina was 3–4% less compared to the eyes, when no intervention was performed [12]. While the concentric narrowing of the visual fields is associated, as a rule, with extensive areas of chorioretinal atrophy after confluent laser photocoagulation of the retina, when was the active phase of ROP, with the localization of the process in zone I-II of the fundus of the eye.
In addition, laser photocoagulation of the retina affects the development of refractive errors, mostly myopia [13], astigmatism [13] and anisometropia [14] usually within the first two years of child's life [15]. According to Quinn et al., myopia progressed in early ROP treatment and at the threshold stage at 3 years of age, the prevalence of myopia was similar in both groups, increasing from approximately 58 to 68% between 6 and 9 months of children’s lives. At the same time, intensive progression of high-grade myopia was noted at the age of 6 months to 3 years [16]. According to Davitt et al., a randomized controlled clinical study of astigmatism in early ROP treatment and threshold stage at 3 years of age, the prevalence of astigmatism ≥ 1.00 dptr was similar in both groups, increasing from about 32% at 6 months up to 42% at 3 years of age, while the main changes were recorded, as a rule, in the period from 6 to 9 months. It should be noted, that regular astigmatism was more often recorded [17]. According to Wiecek et al., the progression of myopia is much faster in the eyes that underwent laser photocoagulation. The number of laser burns resulted in the progression of myopia by approximately 0.16 dptr/100 laser burns. The authors also noted, that the stage and zone of ROP had a significant influence on the progression of ROP, that is, a more severe disease led to a more rapid progression of myopia [18]. According to a study by Tafadzwa et al., by age 6, 50% of children treated with laser photocoagulation developed myopia compared with 19% of preterm infants who did not receive treatment (p = 0.013). In the eyes that had developed myopia, laser burns, on average, occupied 49% (±13) of the retinal area, compared with 43% (±10) in hypermetropia and 42% (±5) in emmetropia (p = 0.030). At the same time, a larger area of laser photocoagulation was associated with a higher degree of myopia and anisometropia (p < 0.050) [19]. It should also be noted, that, according to observations at the Filatov Institute, the risk of failure of laser treatment of ROP was significantly higher for patients with ROP localization in zone I and aggressive ROP. This category of patients has a severe general somatic condition, deep morphofunctional immaturity, are on a respirator for a long time, which aggravates the course of the disease and may affect the outcome of the treatment performed.
In 2007, the anti-VEGF drug, bevacizumab, was first used in the treatment of ROP in order to stop pathological vascular activity. Since then, a new direction in the treatment of ROP has appeared—the intravitreal use of anti-VEGF drugs: bevacizumab, ranibizumab, etc. [20, 21]. The mechanism of their action is based on the inhibition of the main vascular growth factor—VEGF, which significantly reduces the activity of the process and reduces the risk of developing retinal detachment. Thus, in 2011, BEAT-ROP study, among 75 patients with ROP in zone I who received bevacizumab, 6% had a relapse of proliferation versus 42% with disease progression with laser treatment [22]. At the same time, it should be taken into account, that this group of medicine affects only one vascular growth factor—VEGF and in some cases may not provide a complete cure, but lead to the suspension of vascular growth with subsequent neovascularization and, accordingly, the risk of developing retinal detachment at a later period (at postconceptual age up to 69 weeks). Thus, children who received intravitreal injections of anti-VEGF drugs require prolonged dispensary observation due to long-term incomplete retinal vascularization and a high risk of late retinal detachment. Nevertheless, the suspension of ROP activity (especially in very preterm infants) makes it possible to delay the need for retinal coagulation for some time, during which the general condition of the child may improve significantly [23, 24].
The BEAT-ROP group did not observe systemic or local side effects due to the small sample size and short follow-up period. Jalali et al. described serious complications when intravitreal injection of bevacizumab as an adjuvant therapy for laser or surgical intervention, including macular retinal tear, retinal rupture caused by rhegmatogenous retinal detachment, bilateral vascular attenuation, perivascular exudation, optic neuropathy and progression to stage 5 ROP with bilateral retinal detachment. In addition, in one case, a side effect of the medicine was noted as a manifestation of liver dysfunction and a large choroidal rupture in one eye [24].
The VEGF factor is involved in the normal angiogenesis of other organs, that develop simultaneously with the retina. According to Sears (2008) the used dosage is 1000 times the concentration required to neutralize the maximum measured concentration of VEGF in the eye. At the same time, the serum concentration of VEGF in 2 weeks after intravitreal injection is 6 times lower than normal [25].
Undoubtedly, the method of intravitreal injection of anti-VEGF drugs is promising. However, including the potential risk of systemic absorption and subsequent adverse effects due to intravitreal administration of anti-VEGF drugs, evidence of safety outcomes is lacking and that is a major concern.
Laser photocoagulation of the peripheral avascular areas of the retina is a well-established treatment method of ROP. Despite extensive experience with the use of laser photocoagulation of the retina when ROP, discussions regarding indications for its implementation continue. According to Balasubramanian et al., there is no single protocol for laser treatment of ROP [26]. The solution to this problem is the objective monitoring of the disease and the search for accurate markers, the identification of which will be the right indication for laser photocoagulation of the retina. The effectiveness of the method may depend on many factors—the nature of the course of ROP, the localization of the process, the timing of treatment, the morphological and functional immaturity of the child, the presence of concomitant eye pathology, the nature of postoperative treatment [8, 27].
Thus, it is necessary to observe a differential approach in the choice of treatment tactics. The normal course of retinopathy of prematurity (zone II–III): a sparing approach, taking into account vascular activity, reducing trauma, which will reduce the frequency of late complications and improve functional results. Severe forms of ROP (threshold stage of the classic form of ROP and aggressive form of ROP) with extensive avascular zones, require not only to change the technique itself but it is necessary to work together with neonatologists and develop fundamentally new approaches to the prevention and treatment of this severe disease.
References
Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity. One–year outcome–structure and function. Arch Ophthalmol. 1990;108(10):1408–16.
Palmer EA, Hardy RJ, Dobson V, Phelps DL, Quinn GE, Summers CG. Cryotherapy for retinopathy of prematurity cooperative Group.15–year outcomes following threshold retinopathy of prematurity: final results from the multicenter trial of cryotherapy for retinopathy of prematurity. Arch Ophthalmol. 2005;123(3):311–18.
Cavalcanti RP, et al. Efficacy and safety of green laser photocoagulation for threshold retinopathy of prematurity. Arq Bras Oftalmol. 2008;71(1):49–51.
Connolly BP, McNamara JA, Sharma S. A comparison of laser photocoagulation with trans–scleral cryotherapy in the treatment of threshold retinopathy of prematurity. Ophthalmology. 1998;105(9):1628–31.
Connolly BP, Ng EY, McNamara JA, Regillo CD, Vander JF, Tasman WA. Comparison of laser photocoagulation with cryotherapy for threshold retinopathy of prematurity at 10 years: Part 2. Refractive outcome. Ophthalmology. 2002;109(5):936–41.
Good WV. Final results of the early treatment for retinopathy of prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc. 2004;(102):233–48.
Good WV, Hardy RJ, Dobson V. Final visual acuity results in the early treatment for retinopathy of prematurity study. Arch Ophthalmol. 2010;128(6):663–71.
Adakhovska AA, Zaichko ES, Pasechnikova NV, Katsan SV. Risk factors for failure to achieve a positive result in the treatment of retinopathy of prematurity by confluent laser coagulation. Ophthalmol East Eur. 2018;8(1):97–107.
Banach MJ, Ferrone PJ, Trese MT. A comparison of dense versus less dense diode laser photocoagulation patterns for threshold retinopathy of prematurity. Ophthalmology. 2000;107(2):324–327.
Axer-Siegel R, Snir M, Cotlear D, et al. Diode laser treatment of posterior retinopathy of prematurity. Br J Ophthalmol. 2000;84(12):1383–86.
Quinn EG, Dobson V, Hardy RJ, et al. Visual field extent at 6 years of age in children who had high-risk prethreshold retinopathy of prematurity. Arch Ophthalmol. 2011;129(2):127–32.
McLoon E, O'Keefe M, McLoon S, et al. Effect of diode laser retinal ablative therapy for threshold retinopathy of prematurity on the visual field: results of goldmann perimetry at a mean age of 11 years. J Pediatr Ophthalmol Strabismus. 2007;44(3):170–3.
Quinn GE, Dobson V, Davitt BV et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: findings at 4 to 6 years of age. J AAPOS. 2013;(17):124–8.
Gursoy H, Basmak H, Bilgin B, et al. The effects of mild-to-severe retinopathy of prematurity on the development of refractive errors and strabismus. Strabismus. 2014;(22):68–73.
Hsieh C, Liu J, Huang J, et al. Refractive outcome of premature infants with or without retinopathy of prematurity at 2 years of age: a prospective controlled cohort study. Kaohsiung J Med Sci. 2012;28(4):204–11.
Quinn GE, Dobson V, Davitt BV, et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: findings to 3 years of age. Ophthalmology. 2008;115(6):1058–64.
Davitt BV, Dobson V, et al. stigmatism in the early treatment for retinopathy of prematurity study: findings to 3 years of age. Ophthalmology. 2009;116(2):332–9.
Wiecek E, Akula J, Vanderveen D, et al. Longitudinal change of refractive error in retinopathy of prematurity treated with intravitreal bevacizumab or laser photocoagulation. Invest Ophthalmol Vis Sci. 2021;(62):3253.
Tafadzwa Y-Z, Magdalena P, Hazel P, et al. Is the severity of refractive error dependent on the quantity and extent of retinal laser ablation for retinopathy of prematurity? Eye. 2020;(34):740–5.
Gilbert CE, Zin A, Darlow B. Bevacizumab for retinopathy of prematurity. N Engl J Med. 2011;(364):2359–60.
Moshfeghi DM, Berrocal AM. Retinopathy of prematurity in the time of bevacizumab: incorporating the beat-rop results into clinical practice. Ophthalmology. 2011;(118):1227–28.
Mintz–Hittner HA, Kennedy KA, Chuang AZ. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;(364):603–15.
Alba LE, Zaldua RA, Masini RA. Off–label use of intravitreal bevacizumab for severe retinopathy of prematurity. Arch Soc Esp Oftalmol. 2015;90(2):81–6.
Jalali S, Balakrishnan D, Zeynalova Z, Rani TRPK. Serious adverse events and visual outcomes of rescue therapy using adjunct bevacizumab to laser and surgery for retinopathy of prematurity. The Indian twin cities retinopathy of prematurity screening database. Report number 5. Arch Dis Child Fetal Neonatal Ed. 2013;98:327–33.
Sears JE. Anti–vascular endothelial growth factor and retinopathy of prematurity. Br J Ophthalmol. 2008;92(11):1437–38.
Balasubramanian M, Capone, A Jr, Hartnett ME, et al. Photographic screening for retinopathy of prematurity (Photo–ROP). Retina. 2006;26(7):4–10.
Katsan SV. Confluent laser coagulation of the retina in children with aggressive posterior retinopathy of prematurity. Ophthalmol J Kazakhstan. 2019;56(1–2):55–65.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sergey, K., Anastasiia, A., Kozak, I. (2023). Laser Treatment of Retinopathy of Prematurity. In: Grzybowski, A., Luttrull, J.K., Kozak, I. (eds) Retina Lasers in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-031-25779-7_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-25779-7_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-25778-0
Online ISBN: 978-3-031-25779-7
eBook Packages: MedicineMedicine (R0)