Abstract
The knee can be described as a hinge joint with the main movement of flexion and extension, but we know this to be an oversimplification. The tibia unlocks at the beginning of flexion with external rotation of the joint. This is followed by lateral femoral condylar rollback and medial femoral condylar rotation (Last RJ, J bone joint surg. 32:93–99, 1950; Ahrens P, et al, Int Orthop. 35:1611–1620, 2011; Freeman MA, Pinskerova V, Clinical orthop Related res. 410:35–43, 2003). If the tibiofemoral surfaces of the knee joint were of the same length and radii, evaluating the geometry of its motion would be very straightforward. However, both articulating surfaces have differing radii and lengths (Kim HY et al, Clin Orthop Surg. 7:303–309, 2015). This results in both the sliding and rolling of the extended tibiofemoral joint culminating in external rotation of approximately 15 degrees at terminal extension (Kosel J, J Biomech Eng. 132:091002, 2010; Bytyqi D, Int Orthop. 38(6):1191–1198, 2014).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Visual estimation
- Universal goniometer
- Electrical digital inclinometer
- Digital photographic goniometry
- Cross-sectional imaging
- Radiostereometric analysis (RSA)
- Motion capture analysis
1 Visual Estimation of Knee Range of Movement (KROM)
The knee can be described as a hinge joint with the main movement of flexion and extension, but we know this to be an oversimplification. The tibia unlocks at the beginning of flexion with external rotation of the joint. This is followed by lateral femoral condylar rollback and medial femoral condylar rotation [1,2,3]. If the tibiofemoral surfaces of the knee joint were of the same length and radii, evaluating the geometry of its motion would be very straightforward. However, both articulating surfaces have differing radii and lengths [4]. This results in both the sliding and rolling of the extended tibiofemoral joint culminating in external rotation of approximately 15 degrees at terminal extension [5, 6].
The normal flexion-extension range of movement for the knee is 0–140°. Most clinical tests assess this movement alone, as knee abduction–adduction and axial rotation movements are small and not appreciable with visual estimation [7]. The normal range for extension is 0° to −5° in the hypermobile female [8]. Hyperextension is difficult to appreciate in the supine position and is better measured when prone. Deep flexion is 130–140°. A typical examination of KROM consists of positioning the patient semi-recumbent on an examination table with the pelvis square and both legs extended. In a study by Peters et al. comparing visual estimation of knee range of motion to hand goniometry and radiographic measurements, the following clinical technique was used:
-
To gauge full extension or hyperextension, the examiner places a hand above the knee. The contralateral hand cups the ipsilateral heel to lift it off the table until resistance is felt (Fig. 46.1a).
-
The patient actively flexes their knee.
-
With one hand, the examiner stabilises the thigh. The contralateral hand is placed to the front of the ankle with gentle pressure until an end point is reached. This determines maximal flexion (Fig. 46.1b).
This study noted that visual estimation had high intra-relater reliability (ICC 0.8), consistent with other literature on this method [9, 10] (a satisfactory ICC is generally accepted as >0.70, and excellent >0.90). However, there were some notable differences between visual estimation and other measurement methods. On average, goniometric measurement was 6° less than radiographic measurement and 8° less than visual estimation. They proposed ‘is supine flexion of the knee synonymous with true full flexion?’ as a potential explainer for some of this variation and advocated for not mixing methods [11]. Questions such as these are important as measurement of KROM has ramifications for gait and function. KROM is incorporated into orthopaedic knee scoring tools to assess disease severity and recovery after arthroplasty and other knee surgeries and is frequently used as a benchmark in physiotherapy to assess progress with rehabilitation. Surgeons will typically visually estimate KROM in clinic. However, patients generally see different doctors within most public healthcare settings, and this method is the least accurate between different observers [10].
2 Universal Goniometer (UG)
Goniometry is the measurement of the range of movement of a joint through the use of instruments. There are many instruments and techniques, the most common of which is the universal goniometer (UG). In its most basic form, the industry standard long-arm (50 cm) goniometer or short-arm (30 cm) goniometer gives a quick, gross measurement of static angles [12]. For assessment of the knee, the goniometer is placed with the proximal arm pointing towards the greater trochanter and the distal arm towards the lateral malleolus (Fig. 46.2) [13]. Measurement accuracy is contingent on the alignment of the device arms between bony landmarks [14]. In patients with a bigger soft-tissue envelope, finding the bony landmarks may be difficult and their position can change when cycling through flexion and extension [15]. While the UG does not provide information about dynamic movement, it is widely available, is simple to use and, in experienced hands, has good intra-observer reliability.
As time moves on, the digitised goniometer looks set to replace the manual goniometer at least in research fields, and perhaps, in the not-too-distant future, in clinical practice.
3 Electrical Digital Inclinometers (EDI)
An electrical digital inclinometer is a device that is affixed to bony landmarks and interprets the movement of the knee using the same technology that determines the position in mobile phones, car airbags and aircraft [16]. An accelerometer in the device monitors the effect of gravity on a tiny mass held within an elastic support structure. When the EDI tilts, the suspended mass moves slightly, causing a change in capacitance. The tilt angle is calculated from the measured capacitances. Several EDIs are available, including the Cybex EDI 320 (New York, USA), HALO Digital inclinometer (New South Wales, Australia) (Fig. 46.3) and the Limit Mini Digital Inclinometer (Alingsås, Sweden). When purchasing any equipment or adjunct to aid in clinical practice, the primary question is what does the device add and does it improve on the industry standard? The typical cost of a UG is several pounds (£) compared to several hundred for an EDI. Digital measurements have been reported as having similar validity and reliability as traditional goniometry measurements [17]. Hancock et al. report that an EDI has the smallest minimum significant difference, concluding that it is the most accurate compared to other standard measurements [10]. They did not compare to digital photographic goniometry, another modern modality of measurement in KROM.
HALO Digital inclinometer (New South Wales, Australia). (Reproduced with permission from www.sportsphysio.ie)
4 Digital Photographic Goniometry (DPG)
Digital photographic goniometry has appeared in the literature on knee kinematic measurement as a viable means of measuring KROM over the last 10 years [15, 18, 19].
Recording and measuring knee joint motion using digital imaging were first described by Beverland et al. in 2009. High inter-observer (r > 0.948) and intra-observer repeatability (r > 0.906) was demonstrated in ten patients by two observers. The equipment needed was simply a digital camera and image analysis software (Rhinoceros, Seattle, USA).
The software available for interpreting KROM in DPG can account for variables such as camera lens quality and parallax errors [19]. The main benefit of DPG is that the digital images taken allow for further measurements by a different investigator at a later date and they can be rechecked for reproducibility. Even when the bony landmarks are not overtly identified in the image, the inter-rater reliability remains high [18]. The availability of such serial imaging may serve as a visual cue for the patient of their progress during rehabilitation and may even motivate them to engage in targeted improvements [20]. Use of a designated digital camera and separate software is cumbersome in an age where we strive for technology to work seamlessly across platforms. Smartphone applications look to fill this void by offering the ability to image and interpret the KROM on the device that most people carry in their pockets. In one such application, a virtual goniometer is placed on the image taken of the desired joint, with superimposed markers indicating the joint position and relationship to the floor. Their use has been validated across different joints, albeit only in healthy participants [21,22,23]. A variety of applications are available currently, including DrGoniometer (CDM S.r.L, Cagliari, Italy) (Fig. 46.4), Clinometer (Plaincode Software Solutions, Stephanskirchen, Germany) and ROM© goniometric application (Carci©, São Paulo, Brazil), and it is likely that the market will become saturated with other iterations. In a systematic review by Milani et al., seven different applications were validated for use in lower limb measurements. DrGoniometer is an application that stood out over others for its ability to measure both static and dynamic angles, its potential to blind the rater to the measurement and its telemedicine integration [24].
DrGoniometer application interface. (Reproduced with permission from www.drgoniometer.com)
It is not however available on Android devices for which a viable alternative is the ROM© application. This was used by Dos Santos et al. in healthy female population (n = 34) and demonstrated a high degree of correlation (r ≥ 0.90; p < 0.0001) with the universal goniometer and importantly no significant difference in variation between the two methods in any analysis (p > 0.05) (Fig. 46.5) [25].
Determination of knee angle with smartphone application; (a) initial position (0°); (b) final position; α = final joint angle of knee flexion. (Reprinted from the Journal of Bodywork and Movement Therapies, 21:3, Dos Santos et al., Evaluation of knee range of motion: Correlation between measurements using a universal goniometer and a smartphone goniometric application, p 699–703, Copyright (2017), with permission from Elsevier)
The following techniques in measuring KROM are mostly if not exclusively confined to use in research studies and include fluoroscopy and cross-sectional imaging, radiostereometric analysis and motion capture analysis. These methods lend themselves to an assessment of the nuance of knee movement beyond flexion and extension in the sagittal plane.
5 Fluoroscopy and Cross-Sectional Imaging
Single or biplane fluoroscopy measures in vivo joint kinematics using image intensifier(s) and provides in real time anatomic assessment during dynamic activities [26]. Fluoroscopy can be used to match 3-dimensional models from CT or computer-aided design (CAD) imaging of implants to 2-dimensionally acquired fluoroscopic images [27]. The set-up of the C-arm limits the ability of the imaging to only capture a small portion of the gait cycle, and some laboratories have made their systems mobile [28]. Biplane fluoroscopy has been traditionally used in combination with implanting markers into the bone; however, a number of studies have reported non-invasive model-based tracking techniques that provide submillimetre accuracy [29, 30].
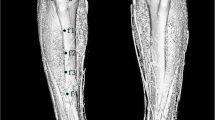
Cross-sectional imaging techniques such as ultra-fast cine computed tomography or kinematic MRI studies can be used to measure KROM. Both modalities when first described in the late 1980s were focused on the evaluation of patellofemoral movement, mainly patellar tracking and subluxation [31, 32].
The first iterations of ultra-fast cine CT consisted of sequential static slices at different angles, and the first truly dynamic kinematic CT protocol was described by Elias et al. (2014) using a 256-multi-detector CT (MDCT) [33]. Compared to 64-MDCT, 256-MDCT is far superior in the acquisition of dynamic images [34]. Protocols are designed to minimise radiation exposure but again are focused on patellar tracking analysis rather than KROM. Kinematic MRI avoids exposure to ionising radiation and details the anatomy of bone and soft tissue in both static and dynamic positions. Dynamic MRI evolved from its initial cardiac applications of blood flow and valvular motion [35] to the measurement of joint movement. Conventional MR imaging is both non-weight bearing and static. Dynamic MRI can be divided into cine PC-MRI and real-time MRI. Cine PC-MRI has been used to measure tibiofemoral kinematics and to visualise cartilage contact during movement by Kaiser et al. In their study, external tibial rotation and anterior tibial translation of the knee were evident from extension to approximately 40° of flexion [36]. A significant rate-limiting step is that cine PC-MRI requires repeated repetitions of the movement cycle. Real-time MRI needs only one motion cycle and is preferable for patients who would be unable to participate in repeated movements due to pain or fatigue [37]. A lack of standardisation in musculoskeletal protocols including optimal acquisition time, field strength parameters, and patient and radiofrequency coil position limits the utility of this modality in standard clinical practice [38].
6 Radiostereometric Analysis (RSA)
Radiostereometric analysis (RSA) is a technique used to predict long-term prosthesis stability by studying its early behaviour. Traditionally, RSA involves the invasive implantation of tantalum beads into a joint at the time of arthroplasty, and subsequently the position of these beads can be evaluated by X-ray images. So how can this technique be applied to measure the ROM of the tibiofemoral joint? There are two obvious problems here: the invasiveness of implanting a foreign body, particularly in the setting where one wants to measure native rather than prosthetic knee joint, and the use of static imaging. Invasive insertion of any device to measure KROM, from tantalum beads to cortical pins, carries with them the inherent risk of infection [39]. In order to address this, a model-based RSA method was introduced in the early 2000s [40, 41]. This allows prosthesis or native knee tracking without the use of markers. This method has been validated by Stentz-Olesen et al., who measured the mean difference between the model method and the marker method for knee movement recorded by static and dynamic radiographs in a cadaveric study. They found that submillimetres of precision are lost compared to standard RSA; however (notwithstanding the added radiation of the CT image), the bone model has the potential to be developed as a clinical tool for measuring KROM [42].
7 Motion Capture Analysis
Modern non-invasive motion capture systems (MoCap) employ skin markers or virtual markers and video or optical sensors to capture trial data from an individual as they move during gait [43] or specific tasks such as squatting [44] or climbing stairs [45]. Indirect measures are taken from these systems to interpret the kinetics and kinematics of the upper or lower limbs. The main purpose of this approach is to determine the six degrees of freedom of different joint kinematics during activities of daily living and yield a more in-depth understanding of KROM than simple flexion and extension. Such systems use anatomical landmarks and functional models to resolve joint centres and axes, from which the range of motion of the joint can be ascertained [46]. The positions of the markers in space are determined using stereophotogrammetry, which requires a minimum of two cameras. In marker-based MoCap, there are issues with soft-tissue artefact, as the markers do not rigidly stay in place over bony landmarks but are mobile due to muscle and skin movement [47]. It is this artefact which renders MoCap less accurate than methods such as biplane fluoroscopy. The coordinate data from the markers is sent to either a commercial programme such as Vicon Plug In Gait (Oxford Metrics Limited, UK) or a bespoke programme to interpret the variables produced by standard coding software, e.g. MATLAB (MathWorks, USA). MoCap studies can determine flexion-extension angles, abduction-adduction angles and internal and external rotation angles. These studies have yielded some useful information, such as continued external rotation of the tibia during stair ascension [48, 49]. In other activities, e.g. squatting, there is no agreement in the literature with respect to abduction or adduction of the femur relative to the tibia [44, 50, 51]. Looking at these studies, the conditions under which MoCap is performed are variable, including some early post-operative patients [44] and stairs of different slopes and heights. A greater number of higher powered studies using standardised conditions and patient cohorts are necessary to make the findings generalisable to a normal population in the future.
8 Conclusion
At its simplest, tibiofemoral motion is measured in day-to-day clinical practice in the sagittal plane. There are devices and applications available, which improve on the universal goniometer and allow record-keeping for posterity and future treatment. Tibiofibular joint motion as well as other tibiofemoral movements (medial and lateral translational and knee abduction-adduction) are not routinely factored into consideration. Six degrees of freedom models consider knee movement in the sagittal, coronal and transverse planes. We have shown that this requires sophisticated and potentially costly equipment, such as fluoroscopy, cross-sectional imaging or motion capture analysis. These technologies are not routinely available and necessarily merited for everyday evaluation, but certainly have their place in a specialist gait laboratory for complex knee pathology.
References
Last RJ. The popliteus muscle and the lateral meniscus. J Bone Joint Surg. 1950;32-B(1):93–9.
Ahrens P, Kirchhoff C, Fischer F, Heinrich P, Eisenhart-Rothe R, Hinterwimmer S, et al. A novel tool for objective assessment of femorotibial rotation: a cadaver study. Int Orthop. 2011;35(11):1611–20.
Freeman MA, Pinskerova V. The movement of the knee studied by magnetic resonance imaging. Clin Orthop Relat Res. 2003;410:35–43.
Kim HY, Kim KJ, Yang DS, Jeung SW, Choi HG, Choy WS. Screw-home movement of the tibiofemoral joint during Normal gait: three-dimensional analysis. Clin Orthop Surg. 2015;7(3):303–9.
Kosel J, Giouroudi I, Scheffer C, Dillon E, Erasmus P. Anatomical study of the radius and center of curvature of the distal femoral condyle. J Biomech Eng. 2010;132(9):091002.
Bytyqi D, Shabani B, Lustig S, Cheze L, Karahoda Gjurgjeala N, Neyret P. Gait knee kinematic alterations in medial osteoarthritis: three dimensional assessment. Int Orthop. 2014;38(6):1191–8.
Desloovere K, Wong P, Swings L, Callewaert B, Vandenneucker H, Leardini A. Range of motion and repeatability of knee kinematics for 11 clinically relevant motor tasks. Gait Posture. 2010;32(4):597–602.
Norkin CC, White DJ, Sawant A. Measurement of joint motion: a guide to goniometry, Third Edition. Physiother Can. 2004;56:250.
Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71(2):90–6. discussion 6–7.
Hancock GE, Hepworth T, Wembridge K. Accuracy and reliability of knee goniometry methods. J Exp Orthop. 2018;5(1):46.
Peters PG, Herbenick MA, Anloague PA, Markert RJ, Rubino LJ 3rd. Knee range of motion: reliability and agreement of 3 measurement methods. Am J Orthop (Belle Mead NJ). 2011;40(12):E249–52.
Richards J, Chohan A, Erande R. Biomechanics. In: Porter SB, editor. Tidy's physiotherapy. 15th ed. London: Churchill Livingstone; 2013. p. 331–68.
Jones A, Sealey R, Crowe M, Gordon S. Concurrent validity and reliability of the simple goniometer iPhone app compared with the universal goniometer. Physiother Theory Pract. 2014;30(7):512–6.
Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ. Measuring flexion in knee arthroplasty patients. J Arthroplast. 2004;19(3):369–72.
Bennett D, Hanratty B, Thompson N, Beverland D. Measurement of knee joint motion using digital imaging. Int Orthop. 2009;33(6):1627–31.
Christ RD, Wernli RL. Navigational sensors. In: Christ RD, Wernli RL, editors. The ROV manual. 2nd ed. Oxford: Butterworth-Heinemann; 2014. p. 453–75.
Tveitå EK, Ekeberg OM, Juel NG, Bautz-Holter E. Range of shoulder motion in patients with adhesive capsulitis; intra-tester reproducibility is acceptable for group comparisons. BMC Musculoskelet Disord. 2008;9:49.
Naylor JM, Ko V, Adie S, Gaskin C, Walker R, Harris IA, et al. Validity and reliability of using photography for measuring knee range of motion: a methodological study. BMC Musculoskelet Disord. 2011;12:77.
Murphy M, Hides J, Russell T. A digital photographic technique for knee range of motion measurement: performance in a total knee arthroplasty clinical population. Open J Orthopedics. 2013;3:4–9.
Blonna D, Zarkadas PC, Fitzsimmons JS, O'Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elb Surg. 2012;21(1):29–35.
Ferriero G, Vercelli S, Sartorio F, Muñoz Lasa S, Ilieva E, Brigatti E, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36(2):146–51.
Mitchell K, Gutierrez SB, Sutton S, Morton S, Morgenthaler A. Reliability and validity of goniometric iPhone applications for the assessment of active shoulder external rotation. Physiother Theory Pract. 2014;30(7):521–5.
Milani P, Coccetta CA, Rabini A, Sciarra T, Massazza G, Ferriero G. Mobile smartphone applications for body position measurement in rehabilitation: a review of goniometric tools. PM R. 2014;6(11):1038–43.
Vercelli S, Sartorio F, Bravini E, Ferriero G. DrGoniometer: a reliable smartphone app for joint angle measurement. Br J Sports Med. 2017;51(23):1703.
Dos Santos RA, Derhon V, Brandalize M, Brandalize D, Rossi LP. Evaluation of knee range of motion: correlation between measurements using a universal goniometer and a smartphone goniometric application. J Bodyw Mov Ther. 2017;21(3):699–703.
Barré A, Aminian K. Error performances of a model-based biplane fluoroscopic system for tracking knee prosthesis during treadmill gait task. Med Biol Eng Comput. 2018;56(2):307–16.
Bonanzinga T, Signorelli C, Bontempi M, Russo A, Zaffagnini S, Marcacci M, et al. Evaluation of RSA set-up from a clinical biplane fluoroscopy system for 3D joint kinematic analysis. Joints. 2016;4(2):121–5.
Guan S, Gray H, Schache A, Feller J, de Steiger R, Pandy M. In vivo knee kinematics and joint centre of rotation in total knee arthroplasty gait quantified by mobile biplane x-ray imaging. Orthop Procs. 2018;100-B(SUPP_6):18.
Giphart JE, Zirker CA, Myers CA, Pennington WW, LaPrade RF. Accuracy of a contour-based biplane fluoroscopy technique for tracking knee joint kinematics of different speeds. J Biomech. 2012;45(16):2935–8.
Anderst W, Zauel R, Bishop J, Demps E, Tashman S. Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys. 2009;31(1):10–6.
Stanford W, Phelan J, Kathol MH, Rooholamini SA, El-Khoury GY, Palutsis GR, et al. Patellofemoral joint motion: evaluation by ultrafast computed tomography. Skelet Radiol. 1988;17(7):487–92.
Shellock FG, Mink JH, Deutsch AL, Foo TK. Kinematic MR imaging of the patellofemoral joint: comparison of passive positioning and active movement techniques. Radiology. 1992;184(2):574–7.
Elias JJ, Carrino JA, Saranathan A, Guseila LM, Tanaka MJ, Cosgarea AJ. Variations in kinematics and function following patellar stabilization including tibial tuberosity realignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2350–6.
Kalia V, Obray RW, Filice R, Fayad LM, Murphy K, Carrino JA. Functional joint imaging using 256-MDCT: technical feasibility. AJR Am J Roentgenol. 2009;192(6):W295–9.
Pettigrew RI. Dynamic cardiac MR imaging. Techniques and applications. Radiol Clin N Am. 1989;27(6):1183–203.
Kaiser J, Bradford R, Johnson K, Wieben O, Thelen DG. Measurement of tibiofemoral kinematics using highly accelerated 3D radial sampling. Magn Reson Med. 2013;69(5):1310–6.
Shapiro LM, Gold GE. MRI of weight bearing and movement. Osteoarthr Cartil. 2012;20(2):69–78.
Garetier M, Borotikar B, Makki K, Brochard S, Rousseau F, Ben SD. Dynamic MRI for articulating joint evaluation on 1.5 T and 3.0 T scanners: setup, protocols, and real-time sequences. Insights into. Imaging. 2020;11(1):66.
Tranberg R, Saari T, Zügner R, Kärrholm J. Simultaneous measurements of knee motion using an optical tracking system and radiostereometric analysis (RSA). Acta Orthop. 2011;82(2):171–6.
Kaptein BL, Valstar ER, Stoel BC, Rozing PM, Reiber JH. A new model-based RSA method validated using CAD models and models from reversed engineering. J Biomech. 2003;36(6):873–82.
Valstar ER, de Jong FW, Vrooman HA, Rozing PM, Reiber JH. Model-based roentgen stereophotogrammetry of orthopaedic implants. J Biomech. 2001;34(6):715–22.
Stentz-Olesen K, Nielsen ET, De Raedt S, Jørgensen PB, Sørensen OG, Kaptein BL, et al. Validation of static and dynamic radiostereometric analysis of the knee joint using bone models from CT data. Bone Joint Res. 2017;6(6):376–84.
Karatsidis A, Bellusci G, Schepers HM, de Zee M, Andersen MS, Veltink PH. Estimation of ground reaction forces and moments during gait using only inertial motion capture. Sensors (Basel). 2016;17(1):75.
Wang J-P, Wang SH, Zhao X, Hu H, Wang YQ, Liu JL, et al. A processing method for kinematics data of human knee joint obtained by motion-capture measurement 2020. https://doi.org/10.21203/rs.3.rs-37194/v1
Konrath JM, Karatsidis A, Schepers HM, Bellusci G, de Zee M, Andersen MS. Estimation of the knee adduction moment and joint contact force during daily living activities using inertial motion capture. Sensors (Basel). 2019;19(7):1681.
Klopfer-Kramer I, Brand A, Wackerle H, Mussig J, Kroger I, Augat P. Gait analysis–available platforms for outcome assessment. Injury. 2020;51(Suppl 2):S90–S6.
Camomilla V, Dumas R, Cappozzo A. Human movement analysis: the soft tissue artefact issue. J Biomech. 2017;62:1–4.
Moglo KE, Shirazi-Adl A. Cruciate coupling and screw-home mechanism in passive knee joint during extension–flexion. J Biomech. 2005;38(5):1075–83.
Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, et al. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech. 2009;42(12):1877–84.
Mizuno Y, Kumagai M, Mattessich SM, Elias JJ, Ramrattan N, Cosgarea AJ, et al. Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res. 2001;19(5):834–40.
Pianigiani S, Chevalier Y, Labey L, Pascale V, Innocenti B. Tibio-femoral kinematics in different total knee arthroplasty designs during a loaded squat: a numerical sensitivity study. J Biomech. 2012;45(13):2315–23.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 ISAKOS
About this chapter
Cite this chapter
Lambert, L.A., McNicholas, M. (2023). Evaluation of Range of Motion of the Tibiofemoral Joint. In: Lane, J.G., Gobbi, A., Espregueira-Mendes, J., Kaleka, C.C., Adachi, N. (eds) The Art of the Musculoskeletal Physical Exam. Springer, Cham. https://doi.org/10.1007/978-3-031-24404-9_46
Download citation
DOI: https://doi.org/10.1007/978-3-031-24404-9_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-24403-2
Online ISBN: 978-3-031-24404-9
eBook Packages: MedicineMedicine (R0)