Abstract
Lung-protective ventilation (LPV) strategies refer to the ventilator settings that allow a protection of the lungs from injuries related to high volumes and consequently high alveolar and transpulmonary pressures during invasive mechanical ventilation. Lung-protective ventilation proved benefits on mortality in ARDS patients and in patients without ARDS. The first component of LPV is the reduction of the tidal volumes, but other ventilator settings such as increased respiratory rate, protective oxygenation and optimized PEEP are also part of LPV. In addition to the ventilator settings, the total dead space involved in CO2 elimination is frequently overlooked. In this regard, the humidification strategy should prioritize heated humidification to minimize instrumental dead space. Indeed, dead space is part of the formula of the alveolar ventilation: Valv = (tidal volume − total dead space) × respiratory rate. This formula reflects the effective ventilation for CO2 clearance. The different components of the total dead space (alveolar dead space, anatomic dead space and instrumental dead space) must be known to optimize mechanical ventilation during lung-protective ventilation. This is particularly true in most severe patients when tidal volumes are low or very low (below 6 ml/kgPBW) and respiratory rate is high (above 25 breaths/min). In this situation, if dead space is not minimized, there is a risk of CO2 accumulation leading to hypercapnic acidosis. While “permissive hypercapnia” has been the first name of lung-protective ventilation, severe hypercapnia has been initialy accepted and encouraged, and associated severe respiratory or mixed acidosis in ICU patients was tolerated. Progressively, this tolerance for high PaCO2 and severe acidosis has been questioned. Recent data highlight the deleterious effects of excessively high PaCO2 leading to increased arterial pulmonary hypertension, right ventricle failure and possibly increased mortality. Other unfavourable effects of hypercapnia have been described, and the current trend is to be more cautious with excessively high PaCO2. The current management in most ICU patients with or without ARDS includes lung-protective ventilation and should also incorporate heart-protective ventilation with optimization of CO2 removal to target normal PaCO2 or mild hypercapnia. In this regard, the humidification strategy is critical through the limitation of instrumental dead space that is mainly related to heat and moisture exchangers and other connectors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- ARDS
- Lung-protective ventilation
- Permissive hypercapnia
- Right heart failure
- Humidification
- Dead space
- Heat and moisture exchangers
- Heated humidifiers
- Carbon dioxide
1 Lung-Protective Ventilation Is Not Only Tidal Volume Reduction
Lung-protective ventilation (LPV) strategies refer to the ventilator settings that allow a protection of the lungs from injuries related to high volumes and consequently high alveolar and transpulmonary pressures that occur during invasive mechanical ventilation [1]. Lung-protective ventilation proved benefits on mortality and is recommended in ARDS patients [2,3,4,5] and in patients without ARDS [6,7,8]. The first component of LPV is the reduction of the tidal volume, but this is not the only parameter involved in LPV. There are other important ventilator settings to consider as well as airway management to optimize.
To ensure adequate carbon dioxide removal, the reduction in tidal volume should be associated with increasing of the respiratory rate. The tidal volumes have progressively been decreased over time in the operating room and in critically ill patients [9]. Similarly, respiratory rates have been progressively increased, up to 30–35 breath/min in most severe patients [10], and low or very low tidal volumes (below 6 ml/kg PBW) must be associated with high or very high respiratory rates (25 breaths/min or even higher) (Fig. 8.1). In those situations, the impact of dead space on CO2 removal is critical [10].
This figure is a schematic representation of the findings based on the analysis of more than 30 studies providing respiratory rate and tidal volumes in different settings (intensive care units and operating room) for more than 40,000 patients [10]. Usual respiratory rates and tidal volumes are represented for surgical patients (planned surgery and one-lung surgery with protective ventilation) and critically ill patients (non-ARDS, ARDS with protective and ultra-protective ventilation and CARDS (COVID-19 ARDS) patients). The targeted minute ventilations are very different as well as the tidal volume and respiratory rate based on the category of patients. In the operating room for planned surgery, the patient’s metabolism is usually low, and the body temperature is frequently below or equal to 36 °C. The CO2 production is therefore low, and minute ventilation around 100 ml/kg/min PBW as shown by Radford in 1955 and used for a long time, is still adequate [10, 44, 67]. In addition, the recommended target tidal volume has progressively been reduced and is now around 8 ml/kg PBW or below; consequently, respiratory rate should be set between 12 and 16 breaths/min. In patients with one-lung ventilation (targeted tidal volume 4–6 ml/kg PBW), the respiratory rate should be set between 16 and 22 breaths/min. In critically ill patients, the metabolism is high and body temperature may be elevated. The CO2 production is high, the dead space is high (including instrumental dead space), and ventilation needs to allow CO2 elimination are higher than normal. In our study, we showed that in mechanically ventilated patients in ICU, minute ventilation was around 150 ml/kg/min PBW (25 studies conducted in ICUs) [10]. The respiratory rate must be frequently set above 20 breaths/min in critically ill patients. It is logical to use high respiratory rate after intubation of septic patients (with pneumonia or other cause of SIRS) breathing above 30/min before intubation. Some patients are ventilated after intubation with both reduced tidal volume and low respiratory rates (15 or below), which can result in severe acidosis
FiO2 and positive end-expiratory pressure (PEEP) settings are mainly focusing on oxygenation control but may also have an impact on CO2 removal. High PEEP levels and low compliance may lead to alveolar distention and alveolar capillaries compression that may be responsible for an increase in alveolar dead space, a marker of ARDS severity [11, 12]. High FiO2, when associated with hyperoxaemia, will be responsible for the Haldane effect, the reduction in haemoglobin affinity for CO2 leading to increased PaCO2 [13]. PEEP and FiO2 settings are part of LPV and may have a role to explain severe hypercapnia during LPV but will not be discussed here.
The other frequently overlooked parameter involved in the CO2 control is the total dead space that is part of the formula of the alveolar ventilation (Valv) that reflects the part of the effective ventilation for CO2 clearance. Noteworthy, dead space is frequently described as physiological and alveolar dead space, and instrumental dead space is usually neglected [14, 15], while it may represent the main dead space volume [16, 17].
The different parts of the total dead space (alveolar dead space, anatomic dead space and instrumental dead space) must be known to optimize mechanical ventilation during lung-protective ventilation (Fig. 8.2) [18]. This is particularly true in most severe patients when tidal volumes are low or very low and respiratory rate is high (Fig. 8.1). Consequently, the humidification strategy is critical through the limitation of instrumental dead space that is mainly related to connectors after the Y-piece and frequently to heat and moisture exchangers [18,19,20]. The current management in most ICU patients with or without ARDS must include lung-protective ventilation and should also incorporate heart-protective ventilation with optimization of CO2 removal (Fig. 8.3).
Different portions of the dead space in the intubated patient. Dead space may be divided into instrumental dead space and physiological dead space (including airway and alveolar dead space). Part of the instrumental dead space may be easily limited by reducing the number of useless connections and by using a heated humidifier instead of a heat and moisture exchanger (HME) for gas humidification. Part of the instrumental dead space is not easily reduced: the endotracheal tube (ETT) may be changed for a tracheostomy tube to reduce the dead space by 10–12 ml, or ETT may be cut but the gain is very limited (2–4 ml)
Concept of heart- and lung-protective mechanical ventilation. Respiratory parameters to manage oxygenation (PEEP, FiO2) and the parameters involved in carbon dioxide clearance (tidal volume (TV), respiratory rate (RR) and total dead space (VD)) may all have an impact both on lung and heart protection by different mechanisms. PEEP positive end-expiratory pressure, FiO2 fraction of inspired oxygen, TV tidal volume, RR respiratory rate, VD total dead space, Valv alveolar ventilation, ROS reactive oxygen species
2 From Lung-Protective Ventilation to Lung- and Heart-Protective Ventilation
The concept of heart-protective ventilation, and especially right ventricle-protective ventilation, is derived from an abundant literature that describes the impact of mechanical ventilation, acidosis and hypercapnia on heart function [21] (Fig. 8.3). There was a gradual shift from tolerance of severe acidosis associated with promotion of lung-protective ventilation and “permissive hypercapnia” to more cautious management and recommendations to avoid severe respiratory acidosis, especially in the case of right ventricular dysfunction.
While “permissive hypercapnia” has been the first name of lung-protective ventilation [22, 23], high levels of hypercapnia have been accepted and encouraged with associated respiratory or mixed acidosis in ICU patients [24]. In addition to the beneficial impact of reduced tidal volumes, hypercapnia could have additional benefits in experimental studies [25]. The questions regarding the haemodynamic impact of metabolic and respiratory acidosis have been debated for a long time [26,27,28]. Although hypercapnic acidosis reduces myocardial contractility and reduces the effect of epinephrine on contractility [26] and reduces systemic vascular resistance [29,30,31], the net impact of hypercapnia is an increase in cardiac output [28, 31] through sympatho-adrenal mechanisms. Oxygen delivery is further increased in hypercapnic acidosis as a result of a rightward shift in the oxyhaemoglobin dissociation curve [32].
However, recent data have highlighted the deleterious effects of excessively high PaCO2 leading to increased arterial pulmonary hypertension [31, 33, 34], right ventricle failure and possibly increased mortality [31, 35,36,37]. Other unfavourable effects of hypercapnia have been described [15], and the current trend is to be more cautious with excessively high PaCO2. “Too little of a good thing” [24] progressively shifted to “too much or too little of a good thing” [15], and it may be now discouraged to keep the PaCO2 above 50 mmHg [35, 36]. There is a strong physiological rationale to avoid severe hypercapnia, leading to increased pulmonary hypertension, right ventricle dysfunction and peripheral vasodilatation [17, 21, 31]. However, the maximum PaCO2 or minimum pH that may be tolerated is still debated. The values of 48 or 50 mmHg above which there is an increase in mortality came from observational studies that showed an association between severe hypercapnia with acidosis [35, 36, 38, 39] and mortality, but the direct causal effect remains unclear [40]. The severity of the acidosis and hypercapnia are certainly related in part to the severity of the patients.
In this regard, the negative impacts of hypocapnia are very well described [41], and the clinical impact may be at least as relevant [38, 42] and must be kept in mind when setting the ventilator. In conclusion, both severe hypocapnia and severe hypercapnia should be avoided. Therefore, optimized ventilator settings immediately after intubation and throughout the duration of invasive mechanical ventilation are required. For this, in addition to the reduced tidal volume, optimal settings of the respiratory rate, taking into account the dead space, must be put in place.
3 How to Set the Initial Respiratory Rate in Critically Ill Patients with Low or Very Low Tidal Volumes?
To ensure adequate CO2 removal and to target moderately increased (below 50 mmHg) or normal PaCO2, several actions are possible. The main ones are the increase in the respiratory rate and the minimization of the instrumental dead space [10].
It is easy to provide charts for the tidal volume based on gender and height and predicted body weight (PBW) to provide 6 or 8 ml/kg PBW to the patients. However, there are no clear recommendation and clues for the initial setting of the respiratory rate and therefore minute ventilation. This may be more a habit or intuitions and by experience: RR is set around 10 breaths/min in the operating room and around 20 breaths/min in newly intubated critically ill patients and sometimes increased to 25 or 30 in ARDS patients. A classical recommendation for minute ventilation is 100 ml/kg PBW/min (for instance, used to set the ASV mode [43] and recommended since 1955 [44]). However, in order to get a reasonable level of PaCO2, 100 ml/kg PBW/min is not appropriate for most critically ill patients [10]. Ventilator settings in the operating room or in critically ill patients (in the emergency department and in the ICU) are very different, leading to minute ventilation around 100 ml/kg/min PBW in the operating room and at least 150 ml/kg/min PBW in critically ill patients. To reach 100 ml/kg PBW/min with 8 ml/kg PBW, a respiratory rate around 12 breaths/min should be used. In most severe patients, such as ARDS patients, a tidal volume of 6 ml/kg PBW associated with a respiratory rate of 25 breaths/min allows to get a minute ventilation of 150 ml/kg PBW/minute. These are two different worlds in terms of minute ventilation to match with patient’s needs (Fig. 8.1). It should be noted that in case of high respiratory rate (greater than 20 breaths/min), the inspiratory flow must be kept high (greater than 40 l/min and up to 80 l/min) to promote low inspiratory time and sufficient expiratory time to avoid intrinsic PEEP [45].
Other measures to reduce PaCO2 such as the use of an inspiratory pause have been proposed [46,47,48], but the effects are marginal compared to the increase in respiratory rate and the decrease in dead space and contradictory with the use of a high respiratory rate. The risk of an end-inspiratory pause prolonging the inspiratory time and reducing the expiratory time is to promote intrinsic PEEP in the case of high respiratory rate [45]. The utilization of ECMO or ECCO2R has been proposed to manage severe hypercapnia or to implement ultra-protective ventilation [49,50,51,52]. However, these complex and expensive techniques, associated with significant complications, should only be used if the simple measures described here (increase in respiratory rate and optimization of instrumental dead space) have been implemented [18, 53, 54].
In addition to the tidal volume and respiratory rate, the other major parameter to consider when initiating mechanical ventilation is the total dead space, including instrumental dead space. For this last parameter, the humidification strategy has a major impact.
4 What Is the Dead Space During Invasive Mechanical Ventilation?
The instrumental dead space is frequently overlooked during mechanical ventilation. Yet, many studies showed its large impact on the work of breathing during assisted ventilation [55,56,57] and on alveolar ventilation (CO2 elimination) during controlled ventilation [16, 58,59,60,61]. Surprisingly, however, in many studies evaluating respiratory mechanics in ARDS or in COVID-19 patients, the instrumental dead space is not provided nor mentioned, even when VD/VT is evaluated.
The different parts of the dead space in mechanically ventilated patients are shown in Fig. 8.2. From the lungs to the Y-piece, this volume represents the “volume with CO2 rebreathing” and the “wasted part of the respiration”, which makes the gas exchanges less efficient [14, 62]. The alveolar dead space is the part of the lung that is ventilated but not perfused (capillary micro-thrombosis, capillary compression by overdistention), and it may be reduced by limiting overdistention; the dead space of the airways is difficult to modify and is mildly increased by PEEP and bronchodilation; the instrumental dead space is the easiest to modify and may account for almost half of the total dead space [16, 17]. The instrumental dead space includes the heat and moisture exchanger at the Y-piece, the CO2 sensor, the connections, the catheter mount, the flex tube, etc. Using a heated humidifier instead of a heat and moisture exchanger is a very efficient way to reduce this dead space [16, 58,59,60,61]. This is recommended in the most recent guidelines to manage ARDS patients [5].
5 Impact of the Instrumental Dead Space on VD/VT and Alveolar Ventilation During Lung-Protective Ventilation
Alveolar ventilation (Valv) is the efficient part of the minute ventilation for gas exchange and CO2 elimination [62].
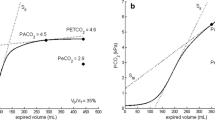
The utilization of small tidal volumes (VT) and high respiratory rates (RR) has several consequences in terms of alveolar ventilation and impact of the dead space. Firstly, it is easy to understand that VD/VT increases as tidal volume decreases if VD remains constant (Fig. 8.4a). The weight of dead space increases in proportion of tidal volume decrease for a constant minute ventilation. Secondly, the dead space which is the “wasted part of the breath” intervenes more frequently when respiratory rate increases.
Impact of instrumental dead space on VD/VT (a) and on alveolar ventilation (b) in critically ill patients with different instrumental dead spaces. The example used for the calculations is the case of a woman of 165 cm, PBW 57 kg. The blue line represents the iso-minute ventilation for 150 ml/kg PBW/min (8.5 l/min with PBW of 57 kg). In setting ❶, with a VT of 8 ml/kg and a RR of 19 breaths/min, VD/VT is 17% with the lowest instrumental dead space and 43% with a higher dead space; alveolar ventilation went from 4.9 l/min to 7.1 l/min. When increasing the respiratory rate and decreasing the tidal volume (settings ❷ and ❸), the difference is even more striking. In the most severe situation, reflecting a low compliance requiring ultra-protective ventilation (case ❸) with a TV of 4.4 ml/kg and a RR of 34 breaths/min, VD/VT is 31% with the lowest instrumental dead space and 77% with a higher dead space. In this situation, alveolar ventilation goes from 6.0 to 2.0 l/min. HH heated humidifiers HME heat and moisture exchangers, CM catheter mount
Consequently, for a steady minute ventilation, when the respiratory rate or the dead space is increased, alveolar ventilation is reduced (Fig. 8.4b). If the respiratory rate is increased in proportion of the decrease in tidal volume, the alveolar ventilation will be reduced, and PaCO2 will be increased. For example, if the settings are modified from 6 ml/kg PBW × 25 (150 ml/kg/min of minute ventilation) to 5 ml/kg PBW × 30 (150 ml/kg/min of minute ventilation), the alveolar ventilation will be lower. With an average instrumental dead space, to keep Valv constant with 5 ml/kg PBW of tidal volume, the respiratory rate should be 34/min (with 170 ml/kg PBW/min). This explains why reduction of the instrumental dead space is recommended in the situations of lung-protective ventilation [5] (i) by removing useless connectors (only closed-suction connector is really necessary) and (ii) by using HH instead of HME to humidify gases. This is also why ultra-protective lung ventilation may be implemented without ECMO or ECCOR, only when the instrumental dead space is minimized [53, 54].
6 Impact of Dead Space Reduction on Respiratory Parameters with Constant Alveolar Ventilation
The previous figures showed the impact of the dead space on alveolar ventilation (CO2 clearance). Figure 8.5a and b shows that with a constant alveolar ventilation, it is possible to substantially decrease the respiratory rate (with constant tidal volume) (Fig. 8.5a) or the tidal volume (with constant respiratory rate) (Fig. 8.5b) when decreasing the dead space.
Impact of different instrumental dead space on the respiratory rate (a) and the tidal volume (b) to maintain a constant alveolar ventilation in critically ill patients. The example used for the calculations is the case of a woman of 165 cm, PBW 57 kg. The target alveolar ventilation is 4.7 l/min which is the alveolar ventilation in this patient with a minute ventilation of 150 ml/kg/min PBW and with a medium instrumental dead space (HME 50 ml, catheter mount and connections 20 ml). The different lines represent the iso-alveolar ventilation lines (4.7 l/min) and the different combinations of respiratory rate and tidal volumes to attain this alveolar ventilation. Based on the application VentilO calculations. (a) This figure shows the potential reduction of respiratory rate when reducing the instrumental dead space to keep constant alveolar ventilation (4.7 l/min) for a constant tidal volume. For example, for a tidal volume of 6 ml/kg PBW (blue lines), the respiratory rate required is 32 breaths/min with the highest dead space and 18 breaths/min with the lowest dead space. For a tidal volume of 5 ml/kg PBW (orange lines), the respiratory rate required is very high (above 40 breaths/min) with the highest dead space, 34 breaths/min with intermediate dead space and 23 breaths/min with the lowest dead space. HH heated humidifiers, HME heat and moisture exchangers, CM catheter mount. (b) This figure shows the potential tidal volume reduction when reducing the instrumental dead space to keep constant alveolar ventilation (4.7 l/min) for a constant respiratory rate. For example, for a respiratory rate of 20 breaths/min (blue lines), the tidal volume required is 7.5 ml/kg PBW with the highest dead space and 5.5 ml/kg with the lowest dead space. This will translate in a gain in plateau pressure or driving pressure related to the pulmonary compliance. For a respiratory rate of 28 breaths/min (orange lines), the tidal volume required is 6.3 ml/kg with the highest dead space and 4.2 ml/kg with the lowest dead space. Ultra-protective ventilation with tidal volumes around 4 ml/kg cannot be achieved with excessive dead space as previously shown [54]. HH heated humidifiers, HME heat and moisture exchangers, CM catheter mount
If the PaCO2 is maintained within reasonable values (<50 mmHg based on several authors [35, 36]), the reduction of the instrumental dead space will allow a reduction of the respiratory rate (Fig. 8.5a) or a reduction of the tidal volumes (and plateau pressures [16, 59]) (Fig. 8.5b) while maintaining constant the alveolar ventilation (and PaCO2). Both reduction of the respiratory rate and tidal volume associated with reduced instrumental dead space would also reduce mechanical power [19]. In addition, the reduction of the instrumental dead space reduces the ventilatory ratio [19, 63]. In the same patient, after reduction of the dead space, the ventilatory ratio would drop significantly, as the PaCO2 will decrease. Similarly, the mechanical power which is associated with mortality in patients with ARDS will decrease just by decreasing the instrumental dead space if the PaCO2 is maintained constant with reducing the respiratory rates. High mechanical power likely reflects a more severe disease with higher pressures, lower compliance requiring lower tidal volumes and higher respiratory rates. There is no evidence that the reduction of this parameter would decrease mortality, more than a decrease of the plateau pressure or driving pressure would decrease mortality. Ventilatory ratio [64] and mechanical power [65] are new markers of severity of ARDS but cannot be determined without taking into account the instrumental dead space (and mainly the humidification strategy used).
We have developed a free educational application, VentilO, to facilitate the initial management of protective mechanical ventilation (tidal volume, respiratory rate and dead space optimization). This tool evaluates the alveolar ventilation required based on the height, the gender (providing the predicted body weight), the actual weight, the temperature, the type of patient and the estimated dead space. Based on these data, it provides recommendations for tidal volume and respiratory rates.
In summary, in critically ill patients, the minute ventilation necessary to maintain PaCO2 within a reasonable range is frequently at or above 150 ml/kg PBW/min. In non-ARDS patients if 8 ml/kg PBW is the targeted volume, a respiratory rate around 20 breaths/min may be adequate; with a tidal volume of 6 ml/kg PBW, respiratory rate around 25 breaths/min may be necessary (e.g., COVID patients). In severe ARDS with low compliance, requiring tidal volumes of 6 ml/kg PBW or lower to maintain plateau pressure below 30 cmH2O, respiratory rate should be set at 25–30 breaths/min or even higher. The utilization of a heated humidifier in these situations to humidify and warm gases delivered to intubated patients allows minimizing the instrumental dead space and a better control of the PaCO2. In most severe patients, with tidal volumes equal or below 6 ml/kg PBW, the minimization of the dead space is mandatory [54]. In CARDS patients (COVID-19 ARDS) , the same principles apply [20, 66].
Instrumental dead space may be very high (above 100 ml) when counting HME, catheter mount, connectors and endotracheal tube. Most efficient HMEs have usually a volume above 50 ml (up to 90 ml) [68], catheter mount may have a volume of 20–60 ml, and many connectors may be used in patients (CO2 cuvette, closed suction and other adaptors for inhalation therapies) and may represent an important additional dead space.
References
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2014;370(10):980.
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network. N Engl J Med. 2000;342(18):1301–8.
Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319(7):698–710.
Fan E, Del Sorbo L, Goligher EC, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–63.
Papazian L, Aubron C, Brochard L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69.
Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308(16):1651–9.
Lellouche F, Lipes J. Prophylactic protective ventilation: lower tidal volumes for all critically ill patients? Intensive Care Med. 2013;39(1):6–15.
Rubenfeld GD, Shankar-Hari M. Lessons from ARDS for non-ARDS research: remembrance of trials past. JAMA. 2018;320(18):1863–5.
Schaefer MS, Serpa Neto A, Pelosi P, et al. Temporal changes in ventilator settings in patients with uninjured lungs: a systematic review. Anesth Analg. 2019;129(1):129–40.
Lellouche F, Delorme M, Brochard L. Impact of respiratory rate and dead space in the current era of lung protective mechanical ventilation. Chest. 2020;158(1):45–7.
Matamis D, Lemaire F, Harf A, Teisseire B, Brun-Buisson C. Redistribution of pulmonary blood flow induced by positive end-expiratory pressure and dopamine infusion in acute respiratory failure. Am Rev Respir Dis. 1984;129(1):39–44.
Nuckton TJ, Alonso JA, Kallet RH, et al. Pulmonary dead-space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med. 2002;346(17):1281–6.
Haldane J. The relation of the action of carbonic oxide to oxygen tension. J Physiol. 1895;18(3):201–17.
Sinha P, Flower O, Soni N. Deadspace ventilation: a waste of breath! Intensive Care Med. 2011;37(5):735–46.
Marhong J, Fan E. Carbon dioxide in the critically ill: too much or too little of a good thing? Respir Care. 2014;59(10):1597–605.
Pitoni S, D'Arrigo S, Grieco DL, et al. Tidal volume lowering by instrumental dead space reduction in brain-injured ARDS patients: effects on respiratory mechanics, gas exchange, and cerebral hemodynamics. Neurocrit Care. 2021;34(1):21–30.
Mekontso Dessap A, Charron C, Devaquet J, et al. Impact of acute hypercapnia and augmented positive end-expiratory pressure on right ventricle function in severe acute respiratory distress syndrome. Intensive Care Med. 2009;35(11):1850–8.
Lellouche F. Decrease dead space prior to calling the ECMO! Chest. 2021;159(4):1682–3.
Lavoie-Bérard CA, Lefebvre JC, Bouchard PA, Simon M, Lellouche F. Impact of the airway humidification strategy in mechanically ventilated COVID-19 patient. Retrospective analysis and literature review. Respir Care. 2021;67(2):157–66. https://pubmed.ncbi.nlm.nih.gov/34670857/.
Lellouche F, Grieco DL, Maggiore SM, Antonelli M. Instrumental dead space in ventilator management. Lancet Respir Med. 2021;9(3):e22.
Paternot A, Repesse X, Vieillard-Baron A. Rationale and description of right ventricle-protective ventilation in ARDS. Respir Care. 2016;61(10):1391–6.
Hickling KG, Henderson SJ, Jackson R. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med. 1990;16(6):372–7.
Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med. 1994;22(10):1568–78.
Laffey JG, Kavanagh BP. Carbon dioxide and the critically ill--too little of a good thing? Lancet. 1999;354(9186):1283–6.
Curley GF, Laffey JG, Kavanagh BP. CrossTalk proposal: there is added benefit to providing permissive hypercapnia in the treatment of ARDS. J Physiol. 2013;591(11):2763–5.
Bendixen HH, Laver MB, Flacke WE. Influence of respiratory acidosis on circulatory effect of epinephrine in dogs. Circ Res. 1963;13:64–70.
Viitanen A, Salmenpera M, Heinonen J. Right ventricular response to hypercarbia after cardiac surgery. Anesthesiology. 1990;73(3):393–400.
Andersen MN, Mouritzen C. Effect of acute respiratory and metabolic acidosis on cardiac output and peripheral resistance. Ann Surg. 1966;163(2):161–8.
McIntyre RC Jr, Haenel JB, Moore FA, Read RR, Burch JM, Moore EE. Cardiopulmonary effects of permissive hypercapnia in the management of adult respiratory distress syndrome. J Trauma. 1994;37(3):433–8.
Pfeiffer B, Hachenberg T, Wendt M, Marshall B. Mechanical ventilation with permissive hypercapnia increases intrapulmonary shunt in septic and nonseptic patients with acute respiratory distress syndrome. Crit Care Med. 2002;30(2):285–9.
Gendreau S, Geri G, Pham T, Vieillard-Baron A, Mekontso DA. The role of acute hypercapnia on mortality and short-term physiology in patients mechanically ventilated for ARDS: a systematic review and meta-analysis. Intensive Care Med. 2022;48(5):517–34.
Severinghaus JW. Oxyhemoglobin dissociation curve correction for temperature and pH variation in human blood. J Appl Physiol. 1958;12(3):485–6.
Feihl F, Eckert P, Brimioulle S, et al. Permissive hypercapnia impairs pulmonary gas exchange in the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2000;162(1):209–15.
Amato MB, Barbas CS, Medeiros DM, et al. Beneficial effects of the "open lung approach" with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med. 1995;152(6 Pt 1):1835–46.
Nin N, Muriel A, Penuelas O, et al. Severe hypercapnia and outcome of mechanically ventilated patients with moderate or severe acute respiratory distress syndrome. Intensive Care Med. 2017;43(2):200–8.
Mekontso Dessap A, Boissier F, Charron C, et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42(5):862–70.
Repesse X, Charron C, Vieillard-Baron A. Acute cor pulmonale in ARDS: rationale for protecting the right ventricle. Chest. 2015;147(1):259–65.
Tiruvoipati R, Serpa Neto A, Young M, et al. An exploratory analysis of the association between hypercapnia and hospital mortality in critically ill patients with sepsis. Ann Am Thorac Soc. 2022;19(2):245–54.
Tiruvoipati R, Pilcher D, Botha J, Buscher H, Simister R, Bailey M. Association of Hypercapnia and Hypercapnic Acidosis with Clinical Outcomes in mechanically ventilated patients with cerebral injury. JAMA Neurol. 2018;75(7):818–26.
Tiruvoipati R, Gupta S, Pilcher D, Bailey M. Hypercapnia and hypercapnic acidosis in sepsis: harmful, beneficial or unclear? Crit Care Resusc. 2018;20(2):94–100.
Laffey JG, Kavanagh BP. Hypocapnia. N Engl J Med. 2002;347(1):43–53.
Madotto F, Rezoagli E, McNicholas BA, et al. Patterns and impact of arterial CO2 Management in Patients with Acute Respiratory Distress Syndrome: insights from the LUNG SAFE study. Chest. 2020;158(5):1967–82.
Arnal JM, Wysocki M, Nafati C, et al. Automatic selection of breathing pattern using adaptive support ventilation. Intensive Care Med. 2008;34(1):75–81.
Radford EP Jr. Ventilation standards for use in artificial respiration. J Appl Physiol. 1955;7(4):451–60.
Brochard L. Intrinsic (or auto-) PEEP during controlled mechanical ventilation. Intensive Care Med. 2002;28(10):1376–8.
Devaquet J, Jonson B, Niklason L, et al. Effects of inspiratory pause on CO2 elimination and arterial PCO2 in acute lung injury. J Appl Physiol (1985). 2008;105(6):1944–9.
Aboab J, Niklason L, Uttman L, Brochard L, Jonson B. Dead space and CO(2) elimination related to pattern of inspiratory gas delivery in ARDS patients. Crit Care. 2012;16(2):R39.
Aguirre-Bermeo H, Moran I, Bottiroli M, et al. End-inspiratory pause prolongation in acute respiratory distress syndrome patients: effects on gas exchange and mechanics. Ann Intensive Care. 2016;6(1):81.
Combes A, Auzinger G, Capellier G, et al. ECCO2R therapy in the ICU: consensus of a European round table meeting. Crit Care. 2020;24(1):490.
Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75.
Combes A, Peek GJ, Hajage D, et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46(11):2048–57.
Combes A, Tonetti T, Fanelli V, et al. Efficacy and safety of lower versus higher CO2 extraction devices to allow ultraprotective ventilation: secondary analysis of the SUPERNOVA study. Thorax. 2019;74(12):1179–81.
Retamal J, Libuy J, Jimenez M, et al. Preliminary study of ventilation with 4 ml/kg tidal volume in acute respiratory distress syndrome: feasibility and effects on cyclic recruitment—derecruitment and hyperinflation. Crit Care. 2013;17(1):R16.
Richard JC, Marque S, Gros A, et al. Feasibility and safety of ultra-low tidal volume ventilation without extracorporeal circulation in moderately severe and severe ARDS patients. Intensive Care Med. 2019;45(11):1590–8.
Girault C, Breton L, Richard JC, et al. Mechanical effects of airway humidification devices in difficult to wean patients. Crit Care Med. 2003;31:1306–11.
Jaber S, Chanques G, Matecki S, et al. Comparison of the effects of heat and moisture exchangers and heated humidifiers on ventilation and gas exchange during non-invasive ventilation. Intensive Care Med. 2002;28(11):1590–4.
Lellouche F, Maggiore SM, Deye N, et al. Effect of the humidification device on the work of breathing during noninvasive ventilation. Intensive Care Med. 2002;28(11):1582–9.
Hinkson CR, Benson MS, Stephens LM, Deem S. The effects of apparatus dead space on P(aCO2) in patients receiving lung-protective ventilation. Respir Care. 2006;51(10):1140–4.
Moran I, Bellapart J, Vari A, Mancebo J. Heat and moisture exchangers and heated humidifiers in acute lung injury/acute respiratory distress syndrome patients. Effects on respiratory mechanics and gas exchange. Intensive Care Med. 2006;32(4):524–31.
Prat G, Renault A, Tonnelier JM, et al. Influence of the humidification device during acute respiratory distress syndrome. Intensive Care Med. 2003;29:2211–5.
Prin S, Chergui K, Augarde R, Page B, Jardin F, Veillard-Baron A. Ability and safety of a heated humidifier to control hypercapnic acidosis in severe ARDS. Intensive Care Med. 2002;28:1756–60.
Lucangelo U, Blanch L. Dead space. Intensive Care Med. 2004;30(4):576–9.
Beloncle F, Studer A, Seegers V, et al. Longitudinal changes in compliance, oxygenation and ventilatory ratio in COVID-19 versus non-COVID-19 pulmonary acute respiratory distress syndrome. Crit Care. 2021;25(1):248.
Sinha P, Fauvel NJ, Singh S, Soni N. Ventilatory ratio: a simple bedside measure of ventilation. Br J Anaesth. 2009;102(5):692–7.
Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75.
Lavoie-Berard CA, Lefebvre JC, Bouchard PA, Simon M, Lellouche F. Impact of airway humidification strategy in the mechanically ventilated COVID-19 patients. Respir Care. 2022;67(2):157–66.
Kenny S. The Adelaide ventilation guide. Br J Anaesth. 1967;39(1):21–3.
Lellouche F, Taille S, Lefrancois F, et al. Humidification performance of 48 passive airway humidifiers: comparison with manufacturer data. Chest. 2009;135(2):276–86.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lellouche, F. (2023). Impact of Humidification Strategy During Lung (and Heart)-Protective Ventilation. In: Esquinas, A.M. (eds) Humidification in the Intensive Care Unit. Springer, Cham. https://doi.org/10.1007/978-3-031-23953-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-23953-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-23952-6
Online ISBN: 978-3-031-23953-3
eBook Packages: MedicineMedicine (R0)