Abstract
Critical Care is a multidisciplinary specialty dedicated to the comprehensive management of patients having, or at risk of developing, acute, life-threatening organ dysfunction. This chapter will address the definition of critical care patients in the setting of Emergency General Surgery (EGS), the logistics, technological and workforce needs of the unit, and what we should expect from an Intensive Care Unit (ICU). EGS patients are a special population, presenting with acute physiologic derangements and requiring timely resuscitation even before a definitive diagnosis. Stratification is crucial in defining which EGS patients will require ICU admission. There are different ICU models (open, transitional, or closed) and levels (I, II, III) in terms of providing specialized care with the increasing complexity of monitoring/treatment. The higher the level of the ICU, the higher the share of intensive Care trained physicians should be. Nurses with specific training should provide nurse staffing of ICUs at every level. Monitoring is a cornerstone in the management of critically ill patients. In addition, ICU provides organ support to EGS patients. This chapter will focus on respiratory support in general EGS patients and in challenging settings like intra-abdominal hypertension or traumatic brain injury.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Critical Care Medicine (CCM)
- ICU models
- ICU workforce
- Perioperative care
- Organ support
- Ventilation strategies
After reading this chapter, you should be able to:
-
Define Critical Care Medicine and its role in the setting of Emergency General Surgery
-
Describe different ICU models and their logistics, technological, and workforce need
-
Discuss the principles of management of critically ill EGS patients, focusing on respiratory support.
1 Introduction
Critical Care Medicine (CCM) is a relatively new branch of medicine whose primary focus is treating a patient with the need for invasive organ support or at high risk of needing one.
This situation is an anomaly in the medicine panorama. It accounts for the fact that the definition of critical care medicine is “operative and instrumental.” In contrast with other branches of medicine, it does not focus its interests on treating a single and specific organ- or system-specific disease, but on restoring normal physiology to “gain time” to recover. It focuses on restoring physiologic balance and the process of how to treat the patient rather than on the pathology he may suffer. In contrast, organ- or system-specific failures are still a prerogative of other areas of medicine.
In 2017, the World Federation of Societies of Intensive and Critical Care Medicine (WFSICCM) came out with this definition: “Intensive care, also known as critical care, is a multidisciplinary and interprofessional specialty dedicated to the comprehensive management of patients having, or at risk of developing, acute, life-threatening organ dysfunction.” [1] This definition sums up the different ones given by national or international learned societies (Table 13.1 reports some definitions of CCM and ICUs). Clearly, every “intensive care physician” should conform to local legislation and be aware of the requirements mandatory in his jurisdiction. The intensive care physician must undergo a specific training and certification in Critical Care. He should be able to diagnose, manage, monitor, intervene, arbitrate, and individualize the Care to each critically ill patient affected by single or multiple health care issues [6, 7]. Lastly, the intensive care physician is the coordinator and leader of the multidisciplinary and often multispecialty approach to the critically ill patient [4, 6,7,8].
2 Who Is the Critical Care Patient?
The critical patient is a patient having or at risk of developing acute, life-threatening organ dysfunction [9]. Therefore, the Surgical Intensive Care Unit (SICU) provides constant monitoring, organ support, and possibly emergency interventions to unstable, severely, or potentially severely ill patients in the perioperative setting [10].
Trauma and acute care surgical patients are very different from those presented in the non-acute care setting, and they more often require ICU admission [11, 12]. The lack of preoperative evaluation and optimization exposes these patients to a greater risk of death and complications. In addition, EGS patients present with acute physiologic derangements, requiring aggressive and timely resuscitation even before a definitive diagnosis. When the EGS patients arrive in the ICU, they may need ongoing optimization of tissue perfusion and further investigations/surgery before definitively correcting the “anatomic” disturbances [13].
2.1 The Critical Emergency Surgery Patient
EGS patients represent a unique population with the highest rate of death and complications [14, 15]. Recent studies have shown that EGS patients are six to eight times more likely to die than patients undergoing the same procedure electively [16]. Approximately half of EGS patients experience a postoperative complication [17].
The patient group is highly heterogeneous; therefore, the need for observation and intensive Care will vary [18]. In general, EGS patients are older, have a high fragility incidence, a reduced physiologic reserve, and are significantly more acutely ill at admission [19].
Unsurprisingly, the risk of perioperative death is higher in the elderly emergency laparotomy patient than in younger patients [20]. Green et al. reported an overall mortality of 45%, with 12% intraoperative complications and 70% postoperative complications (including myocardial infarction, wound infection, hematoma, and sepsis) in octogenarians undergoing EGS [21].
Apart from age, several factors can explain the increased risk of death following EGS, among which are the inability to optimize preoperative status before surgery and the time-sensitivity of the pathology. Nevertheless, Havens et al. showed that EGS patients have a worse outcome than non-EGS (NEGS) patients, even after controlling for preoperative variables and different procedure type [16].
A possible explanation can be found in the severe physiologic derangement associated with the acute disease: the physiology of EGS patients differs considerably from that of patients undergoing elective procedures, mainly due to the presence of shock. Indeed, while in NEGS cases, large-volume blood loss and fluid shifts might be anticipated but not yet present, bleeding or infection in EGS patients often results in substantial effective fluid loss already in place at the time of presentation [22].
Privette et al. identify a subgroup of EGS patients with higher acuity, the “acute care surgery” (ACS) patients [23]. The authors defined ACS patients as nonelective, nontrauma patients with significantly altered physiology requiring ICU admission, specific operative interventions, or both. ACS patients were more similar to trauma patients than to elective or EGS patients. They more likely required multiple operations, had longer hospital and ICU stay, higher mortality, and need for post-discharge rehabilitation. Moreover, Lissauer et al. demonstrated that ACS patients need more ICU resources than other general surgical patients: they have longer ICU lengths of stay and more frequently require mechanical ventilation and continuous renal replacement therapy [12, 24]. They do represent a distinct population.
2.2 The Critical Trauma Patient
According to the Trauma ICU Prevalence Project (TRIPP study), trauma patients have high medical acuity, presenting a wide breadth of pathology and requiring different interventions [25]. While no consensus definition for “polytrauma” has been recognized, generally accepted definitions use an Injury Severity Score (ISS) of greater than 15 to 17 or an Abbreviated Injury Scale (AIS) of greater than 2 in at least two body regions [26].
The TRIPP study provided a representation of patient types, injuries, and conditions in ICUs caring for trauma patients. According to this prevalence study, trauma patients can present with multiple high-intensity diagnoses (septic shock, 10.2%; multiple organ failure, 5.58%; adult respiratory distress syndrome, 4.38%). Hemorrhagic shock was present in a high proportion of patients (11.6% of trauma patients and 6.55% of all patients). A wide range of traumatic injuries was documented: head, neck, and thoracic injuries predominated, but spine, orthopedic, vascular, and intra-abdominal injuries were also prevalent. Over 69% of the trauma patients had a major operation, illustrating the ongoing surgical nature of trauma and the importance of surgical subspecialty care at trauma centers. Median ICU length of stay was 9 days; 30-day mortality was 11.2% [25].
Trauma patients present with anatomic and physiologic derangements requiring prompt identification and treatment. Correcting the physiologic derangement is the primary goal, while definitive correction of the anatomic disturbances is usually postponed until physiologic stabilization occurs. Following initial resuscitation and possibly damage control surgery, trauma patients presenting to the ICU may be far from stable with ongoing resuscitative needs and injuries still requiring definitive repair. This group of patients presents unique challenges for the ICU physician, including determining resuscitation endpoints and managing early post-resuscitation complications [27]. Trauma resuscitation has evolved from a one-size-fits-all approach to one tailored to patient physiology [28].
Virtually all critically injured patients require some degree of physiologic support on arrival to the ICU. It is essential to assess active bleeding and the extent of unresolved shock since these two factors will guide ongoing resuscitation [28, 29].
2.3 Stratification of Patients
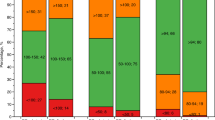
The critical care patient is defined as a patient at risk of or with ongoing organ support. This generic and highly unspecific statement can be applied to an almost moribund trauma patient as well as to an elective surgical patient after an uneventful procedure. In order to compare those two patients, two main artifices have been explored: the use of Severity of Illness Scoring Systems (SISS) and the Nursing Workload Score (NWS).
The SISSs [30] are scoring systems that predict the mortality (usually at discharge from the ICU or hospital) according to the characteristics of the patient (e.g., age, diagnosis of admission, modality of admission, comorbidities, derangement of physiologic parameters at admission or in the first 24-h stay in ICU). The aims of the SISSs are well-described by their main characteristics: the calibration and the discrimination ability [31]. Discrimination defines the probability that a test will correctly discriminate between two alternatives. In the case of SISS, it helps to identify the patient who eventually will die correctly. A SISS with excellent discrimination may have some role at the patient level when counseling the family or triggering a revision over the therapeutic ceiling. Calibration is the degree to which the predicted probability generated by a model agrees with the actual event rate observed in a population, i.e., the ability of a model to correctly stratify groups of patients accordingly to their observed incidence of death. This characteristic is helpful when comparing two different populations, for example, if higher mortality is just the effect of a more critical population. SISSs are affected by several flaws intrinsic to the way they are built. Internal validity can be severely affected by the clinician withholding or withdrawing a treatment accordingly to the SISS. This leads to the classical scenario of the self-fulfilling prophecy that creates artificial overconfidence in a model specificity and negative predictive value [32]. The external validity can be even more challenging as the outcome can be a function of the resources and expertise available to treat the patient (e.g., a high-volume academic center vs. a rural ICU) or the implementation of an effective treatment in a previously untreatable disease.
NWS are used to classify patients according to the demand of assistance and program the number of nurses a unit needs. Cullen et al. [33] in 1974 described the Therapeutic Intervention Scoring System (TISS), a 57-items score to describe the nurse workload. Every item is a typical nurse activity in ICU, and the score is the sum of those activities done in 24 h. This score is the archetype of the NWS and correlated with costs, need for nurse units, and mortality because patients with a higher severity show a higher need for assistance. The idea is to quantify the time spent by the nurse in personal activities through the record of specific activities. The negative side is that to score 57 or 76 items is time-consuming, so a simplified version, the TISS-28, with only 28-items, was developed in 1996 [34]. The Nine Equivalents of Nursing Manpower Score is a furthermost simplification of the TISS-28 [35], considering only nine items comprehensive of the 28 items of the TISS-28. 40–50 NEMS points are the maximum “amount of work” a nurse can deliver, and six of those items are directly related to the organ failure a patient can suffer in ICU. This substantial overlap between nursing workload and the number and severities of organ failures (a proxy of the severity of the patient) is the basis for the definition of Level of Care (LoC). LoC is defined as the relationship between the severity of the illness of the patient and the nurse-to-patient ratio [36]. LoC can be high, intermediate, and low (see Table 13.2), and the number of patients a nurse can attend is related to their LoC [37].
3 What Is an ICU?
The WFSICCM definition [1] of ICU is: “An intensive care unit is an organized system for the provision of care to critically ill patients that provides intensive and specialized medical and nursing care, an enhanced capacity for monitoring, and multiple modalities of physiologic organ support to sustain life during a period of acute organ system insufficiency. Although an ICU is based in a defined geographic area of a hospital, its activities often extend beyond the walls of the physical space to include the emergency department, hospital ward, and follow-up clinic.” According to human, technological, and organizational resources, this dense statement defines ICUs with a lesser role for technological ones. ICU is a matter of workflow rather than the place where it happens or the devices used. Several national societies pose the benchmarks for ICUs. Since 2001, the Society of Critical Care Medicine (SCCM) has classified ICUs focusing on the concept of “model,” who delivers the care, and “level,” how invasive and complex care can be [6]. Those definitions reflected different, regionalized, local stories that brought to the creation of ICUs and mirrored locally available resources.
3.1 ICUs Models
ICU model defines who is in charge of the critically ill patient and has the privileges to admit and discharge patients from ICU [6].
In the open model, every physician can admit to ICU, and those patients are under his direct care. Those physicians have compelling responsibilities in the hospital (i.e., operating rooms, outpatient clinic, or general ward) and did not receive specific training in critical care medicine. The intensivist, if available, is consulted only at the discretion of the admitting physician.
In the transitional model, the patient is admitted under the care of a nonintensivist physician, but intensivist consultation is mandatory, at least once during the ICU stay.
In the closed ICU model, only the intensivist has the privileges to admit and discharge patients. All the patients admitted to the ICU are under the direct care of an intensivist.
These models can be subclassified as high-intensity staffing if an intensivist is 24 h available and low-intensity staffing if the intensivist is not always available [38].
The classification of ICUs has a historical origin. In 1991, the SCCM published the data from a survey upon ICU organization and staffing [39, 40]. Those data comprised 40% of all ICUs from the United States. They showed a wide variety of management and organizational structure, with just 22% of units fulfilling the criteria for a closed one. Since then, compelling evidence suggested increased patient outcome [41] (reduced mortality [38], length of hospital/ICU stay [38], adherence to guidelines, and best medical practice [42]) when mainly intensivists staffed ICUs. In 2001 SCCM favored the model of an ICU with extensive, if not exclusive, presence of intensivists to reduce mortality, length of stay, and costs and increase the overall quality of work [6]. Subsequent evidence pointed out that “an intensivist-led, high-intensity team is an integral part of effective care delivery in the ICU and can lead to improved outcomes” [43] as several studies showed to fail an improvement in outcomes of a strictly closed with 24/7 onsite intensivist coverage.
One of the main drives for those studies was to overcome the shortages of intensivists and reduce costs. In 2011, the European Society of Critical Care (ESICM) rolled out the essential requirement for ICUs regarding structural and organizational aspects, coming to a different solution [3]. ESICM stated that ICUs should be staffed only by intensivists with a recognized and certified intensive care curriculum. All the other physicians participating in the care of critically ill patients should be considered a consultant. However, how an ICU is physician-staffed is often a matter of available resources. In a low-resource setting, it is more likely that the ICU will have physician and nurse staffing from different backgrounds.
Moreover, the recent COVID-19 pandemic with the tremendous surge of critically ill respiratory patients forced to stretch medical and nurse expertise. Several institutions promoted remote consultation by intensivists and highly protocolized bundles of care taken over by nonintensivist [44]; others stretched resources as much as possible, and physicians and nurses with non-ICU backgrounds were implemented [45] to run ICUs. Despite the lack of solid evidence, this stepping back from the model of high-intensity staffing might have led to less-than-optimal results, as suggested by a striking difference in mortality favoring patients transferred to ICUs not overwhelmed by the inflow of patients from those treated locally with the available resources [46].
3.2 ICUs Levels
ICU level refers to the ability to provide specialized care to critically ill patients with increasing complexity of monitoring and treatment. Definitions are usually at the nation or regional level and consider the resources available on the territory and peculiarities such as underpopulated areas, remote areas, or large academic centers. Several scientific societies [1, 3, 6, 43], national societies, and governmental regulatory authorities [4, 8] defined the ICUs level, pointing out: how they should be staffed, what type of monitoring and organ support must be available, what type, and for how long they should be able to treat critically ill patients, what is their role in the community they sit. Every intensivist should be aware of the specific requirement in the area where he works.
The usual classification is in three levels, from the most basic level I to the most advanced Level III.
A level I ICU sits in a small, not specialistic, hospital. It should be able to provide essential monitoring and basic cardiovascular and ventilatory support for a short period. The unit must have a protocol for transferring and referring more complex patients to secondary or tertiary ICUs. Medical staffing can be challenging as few certified intensivists are usually willing to work full-time in small centers. However, at least the medical director should be a certified intensivist [3, 4, 8]. Ideally, the level I ICU is in an underpopulated area or is a small clinic in an urban center dealing mainly with postsurgical patients or critically ill patients with basic needs. As a rule, they treat patients who need a short period of stabilization or patients for whom the treatment in the community they live out outweighs the advantages of a transfer in a center capable of more advanced monitoring and treatment options [8]. To maintain sufficient clinical skills, the minimal number of mechanically ventilated patients is not established, but one hundred can be considered a reasonable number [4].
A level II ICU provides a high standard of general ICU care for a prolonged period of time [1, 3, 4, 8]. It should be capable of delivering care to a patient requiring complex multisystem life support like mechanical ventilation, continuous renal replacement therapy, invasive cardiovascular monitoring, and essential invasive cardiovascular support. A level II ICU is a designated area in a medium-large hospital that treats definitively the critically ill patients referred to that hospital. Transfer of patients happens when there is no appropriate specialty within the hospital. The ICU should have a protocol in place to refer for admission and consultation patients to tertiary centers capable of neurosurgery, cardiothoracic surgery, transplant, burn, and advanced pediatric care. Despite the shortage of intensivists, a Level II ICU should be staffed only by certified intensivists [3]. A caseload of at least 200 mechanically ventilated patients per annum is advisable to maintain a high level of clinical expertise and provide adequate clinical exposure and education to staff [4].
A level III ICU is a tertiary referral unit for intensive care patients and should provide complex multisystem life support for an indefinite time [3, 4, 6, 8]. A level III ICU should sit in a tertiary referral hospital center, have academic and research commitment, and give specialized and definitive care to subspecialty patients (i.e., neuro-trauma, cardiovascular, pediatric, transplant, ECMO, and burns patients). Physicians with privileges to work there should be certified intensivists and, possibly, formally trained in the subspecialty they practice. It is difficult to identify a minimal caseload of complex patients per annum to maintain enough clinical exposure. If 400 mechanically ventilated patients can be enough to retain enough high-level skills in complex patients [4], this number can be less critical when a tertiary center is dedicated to specific pathologies (e.g., liver transplant unit, neuro-trauma, cardiothoracic unit) or to specific treatment (e.g., ECMO center, bone marrow transplant unit).
3.3 ICU Workforce
3.3.1 Physicians
Physician staffing of ICUs is driven by local legislation, the availability of physicians trained in Intensive Care, recommendation by the national or international societies of CCM, and the ICU level. As a general rule, the majority of societies recommend that the higher the level of the ICU, the higher the share of intensive care-trained physicians [1, 4, 6, 8]. However, ESICM [3] suggests that only intensive care-certified physicians should practice in ICU, if possible.
The training and core curriculum of an intensivist is highly variable at the national level. The SCCM rolled out the first list of competencies an intensivist should have in 1992 [7]. Since that benchmarking paper, the core curriculum has become a competency-based one in several countries. In 2003, Competency-Based Training in Intensive Care medicinE (CoBaTrICE) was founded to create the first unified European curriculum in CCM. The main focus was to standardize the competencies an intensivist should have at an international level in the EU area and provide a reliable and unified assessment through the institution of a mandatory exit exam, the European Diploma of Intensive Care (EDIC). However, the training program is still very variable between countries [47]. CCM is considered: a primary specialty with direct access after undergraduate training in some countries (i.e., Sweden and Switzerland), in other, is a multidisciplinary ‘supra-specialty’ with access from several primary specialties to a standard national core curriculum for CCM (e.g., USA, Germany, Ireland), in other is just a piece of another specialty (e.g., Denmark, Germany) or a dual joint certification, usually anesthesia and CCM (e.g., France, Italy). A formal national system for quality assurance of CCM training exists in the majority of the European countries, as well as some form of mandatory exit evaluation. Despite the presence of a well-recognized international standard, all EU countries are different, and the mandatory examination can range from an informal evaluation (e.g., Turkey) to a national exam (e.g., France) or a mandatory pass of the EDAIC (e.g., Denmark, Ireland).
A few papers investigate the optimal number of patients a single physician can manage (patient-to-intensivist ratio, PIR). Gershengorn et al. [48] evaluated the possible relationship between the PIR and mortality and found a U-shaped curve with a nadir of mortality for a PIR between 7 and 8. The authors argue that a PIR lower than seven probably does not assure enough exposure to the intensivist to keep him proficient in treating complex patients. On the contrary, a PIR higher than eight just overwhelms the intensivist and increases mortality.
3.3.2 Nurses
Nurse staffing should be provided by nurses with specific training in CCM and emergency medicine, giving rise to the critical care nurse (CCN) [1, 3, 4, 8, 43, 49] The prominent role of CCN in emergency medicine and critical care has been recognized since the first experiences in Pittsburg in the ’60s. As Safar stated [50], “we discovered nursing in this area required special skills not ordinarily available in the average hospital nurse.” Hence, they provided advanced training to them in mechanical ventilation and hemodynamic monitoring. Nurse education evolved from a secondary level to a tertiary level almost everywhere in the world [51, 52]. The peculiarity of the work in an ICU requires a post-tertiary (e.g., master or Ph.D.) education or, at least, some informal training in ICU while working under supervision. A recent survey in the EU [53] showed that 70% of European countries have a formal post-tertiary program to educate CCN and that 54% of the European Countries surveyed recognized CCNs as specialized and highly skilled health care professional workers. Despite acknowledging the importance of the CCNs, the training programs were highly variable, ranging from a 240-h course to a 2-years theoretical and practical course. The survey pointed out the lack of standardization between and inside countries regarding how teaching was provided, the students assessed, and the qualification awarded. The education of CCN cannot be overemphasized as, probably, even limited education programs on specific issues, like mechanical ventilation, may reduce strong outcomes as mortality, length of stay in ICU, or ventilator acquired pneumonia [54].
National and international societies defined the number of nurses and the share with a post-tertiary education an ICU should have [1, 3, 4, 8, 55]. The LoC drives the planning of nurses’ unit need because different levels need a different nurse-to-patient ratio. A patient with a high LoC needs a nurse-to-patient ratio of 1:1 or 1:2. At the same time, the 1:3 or 1:4 nurse-to-patient ratio can suffice for those with a lower or intermediate LoC [36].
3.3.3 Allied Health Care Professionals
Other professional figures have flanked physicians and nurses since the first experiences of ICU. Several national and international guidelines define the work in ICU as a “teamwork” [3, 4, 6, 8]. Intensivists and CCN have as a primary task to coordinate other healthcare workers in multidisciplinary or interdisciplinary care, in which team members work in parallel but maintain strict disciplinary boundaries. In 2018, Donovan et al. [56], on behalf of the SCCM, defined interprofessional care as “the care provided by a team of healthcare professionals with overlapping expertise and an appreciation for the unique contribution of other team members, working as partners in achieving a common goal.” This vision goes beyond the classical teamwork to embrace a different definition of the team as “a cohesive group with shared team identity, clarity, interdependence, integration, and shared responsibility” [57]. This definition emphasizes the team over its members or the sum of them. A team-based approach demonstrated an impact on major outcomes: adherence to bungles and guidelines, reduction of cost and mortality, better end-of-life decisions, ICU rounds, and handover [56].
An ICU team can be formed by: intensivist, nonintensivist physicians, CCN, advanced practice providers (APP), clinical pharmacists, respiratory care practitioners, rehabilitation specialists, dietitians, social workers, case managers, and spiritual care providers [1, 3, 4, 6, 8, 56]. Few of those professional characters have demonstrated an impact on the outcome of the patients.
APP such as nurse practitioners and physician assistants are used with more frequency as a shortcoming to the lack of intensivists. Several studies showed no differences in strong outcomes like mortality or length of hospital stay when comparing units staffed with APPs or physicians in training [56, 58, 59]. However, the evidence was weak due to their academic single-center population, retrospective design, and failure to control for intensivist staffing models. However, those studies showed longer ICU length of stay and nonhome discharge.
Clinical pharmacists have had a longer presence in ICU teams and are common in several countries [3, 4, 8]. In 2000, SCCM defined in a position paper [60] how a critical care pharmacy service should be organized and the requirements for a clinical pharmacist to work in the ICU. Several studies reviewed the impact of clinical pharmacists on ICU outcome [61], in particular: increased adherence to specific interdisciplinary bundles, reduction of adverse events, and costs.
Respiratory care Practitioners have a central role in intubated but also for non-intubated patients. Their presence contributes specifically to the optimal provision of spontaneous breathing trials, early mobility, implementation of PAD guidelines, and ABCDEF bundles [56].
Rehabilitation therapists have a fundamental role in improving and speeding up functional and cognitive impairment in critical care patients. Their work has been demonstrated to be safe, feasible, and to have a positive effect in the following areas: decreased ICU and hospital lengths of stay, shorter duration of delirium, better functional outcomes at hospital discharge, and more ventilator-free days, reduced delirium incidence, assessment and management of dysphagia, facilitation of communication, and management of patients with tracheotomies and adherence to the ABCDEF bundle.
3.4 ICU Service: Operational Requirement
Quality healthcare is defined as care that is “safe, effective, efficient, equitable, timely and patient-centered” [62]. National and International guidelines [1, 3, 4, 8, 63] pose benchmarking standard of logistics, equipment, design, and technological need of an ICU as well as other operational requirements related to the development of human resources and organization. Material requirements are related to the level and model of the ICU and, most importantly, to the resources available, i.e., the availability of monitoring or expensive invasive procedure (like ECMO or continuous renal replacement therapy) is different between high, middle, and low-income countries. We will briefly overview the operational requirements related to work organization and human resources. Whereas they are still related to the available recourses, there is a cultural background that health care providers and managers should adopt and adapt to their local environment. This cultural background is founded on the concept of clinical audit, i.e., a means to find out if the healthcare provided is in line with the best standards. This is achieved by identifying how the service is performing and where improvement could be made. Quality Improvement is the ultimate step. It is the “combined and unceasing efforts of everyone –to make changes that will lead to better patient outcome (health), better system performance (care) and better professional development (learning)” [64]. Several guidelines [1, 3, 4, 8] address this goal and define some tools an ICU should have to reach it, and in some cases, they are mandatory to accredit an ICU. The most cited are: a continuous medical education system with staff nurses and physicians that have a protected time to meet the educational demands of the unit and protected time for the unit itself to continue education; mandatory participation in a national or international audit system with revision of cases, treatment, ICU performances and comparison of results with other units; a morbidity and mortality program; structured handover and clinical rounds; the participation in research and development activities; a dedicated interprofessional group for the implementation of multidisciplinary bundles; a post-ICU clinic in order to continue test long- and middle-term patients’ outcome [65].
4 General Principle of Management
Table 13.3 reports the general principle of monitoring and respiratory management in trauma and EGS patients.
4.1 Monitoring
The ICU provides a place for monitoring and care of patients with potentially severe physiologic instability, such as EGS patients. The critical endpoint is oxygen supply to tissues according to their metabolic needs. Therefore, both oxygenation and perfusion must be monitored in the implementation of any resuscitation strategy [66].
Despite this high acuity of ICU patients described in the TRIPP study, ‘monitoring’ was the reason for ICU admission for 16.6% of nontrauma surgical patients [25].
Trauma and EGS patients are prone to hemodynamic instability. Several complications may occur, so they must be monitored with various modalities, invasive and noninvasive, to detect any deterioration promptly.
4.1.1 Hemodynamic Monitoring
The importance of hemodynamic monitoring was highlighted in 2020 by the American Association for the Surgery of Trauma (AAST).
The AAST underlines a delicate balance between hypovolemia/hypoperfusion and volume overload, which is equally associated with complications [67].
Current practice in EGS patients involves the assimilation of multiple endpoints of resuscitation into an overall assessment. Resuscitative endpoints should be tracked in real-time, and, as they approach a normal range, resuscitation is titrated not to overshoot euvolemia [67].
Heart rate, blood pressure, and urine output are basic vital signs that should be monitored in all trauma and nontrauma EGS patients. However, they can easily miss low cardiac output (CO) states and are of limited value in the surgical ICU [68] or trauma settings [69]. Evidence of persistent hypoperfusion could be found in 80% of critically traumatized patients, despite the normalization of their vital signs [70]. Hence, different markers of low CO states have been evaluated: shock index, biomarkers like serum lactate or the oxygen saturation in superior vena cava, invasive or minimally invasive CO monitoring, and functional hemodynamic monitoring like echocardiography. Focused echocardiography may allow rapid, noninvasive, point-of-care assessment of hemodynamic status, providing valuable information on the etiology of shock and assessing response to therapeutic interventions [71, 72]. Hemodynamic monitoring is addressed in other chapters of this book.
4.1.2 Respiratory Monitoring
Pulse oximetry, airway patency, and respiratory rate should be monitored in all surgical patients. Patients with hypothermia, hypotension, hypovolemia, or peripheral vascular disease, or receiving vasoconstrictive medications may have inaccurate pulse oximetry readings.
Some patients will arrive in ICU already extubated; nevertheless, they still need respiratory monitoring since postoperative pulmonary complications (PPCs) can occur. Postoperative pain and immobility may lead to decreased cough, clearance of secretions, and an inability to recruit alveoli. Monitoring pain score is essential since appropriate pain control and early mobilization are critical in preventing pulmonary complications [73].
All patients under mechanical ventilation benefit from capnography measurement because the presence of ETCO2 implies adequate ventilation and perfusion; an acute decrease in ETCO2 is a life-threatening emergency, representing a sudden decrease in one or both of these parameters. Frequent causes in the postoperative setting include a pulmonary embolus, low cardiac output state, or disconnection from the ventilator.
Outside the ICU, continuous monitoring of oximetry and capnography may allow the detection of pathophysiologic abnormalities earlier in postoperative patients, but the evidence for improved clinical outcomes remains weak [74].
Other respiratory monitoring techniques can include arterial blood gas analysis and imaging studies, such as chest x-ray or lung ultrasounds. In ventilated patients, monitoring respiratory mechanics may be relevant as well.
4.1.3 Neurologic Monitoring
A focused neurologic examination should follow every acute care surgical procedure. After anesthesia, patients should return to their preoperative level of consciousness and exhibit no lateralizing signs. In the immediate postoperative period, depressed mental status with nonfocal findings most commonly represents persistent anesthetic drug effects or under-resuscitation. If there is no improvement after the appropriate time, imaging may be required.
Besides clinical examination, additional monitoring may be required in trauma or emergency surgical patients (ICP, EEG, SjvO2, PtbO2, and TCD) [75,76,77,78,79].
4.2 Organ Function Support
Hemodynamic support (i.e., fluid therapy and vasoactive drugs) and coagulation support are addressed in other chapters. We will focus on respiratory support in the general trauma and surgical patients and special populations as the patients with an open abdomen treatment or a severe traumatic brain injury.
4.2.1 Respiratory Support
Postoperative pulmonary complications (PPC)—such as atelectasis, pneumonia, respiratory insufficiency- are frequent causes of morbidity and mortality after EGS [80, 81].
According to current literature, patients undergoing major abdominal EGS are the surgical patients with the highest risk of developing PCCs [82, 83].
Emergency surgery confers a two-to-six-fold increase in the risk of PPCs compared to elective surgery [84]. In the ALPINE study, 48% of patients undergoing emergency laparotomy developed a PPC, with respiratory failure being the most common one [85]. The development of PPCs after EGS has been associated with prolonged hospital stay and increased death rate [86]. Advanced age, abnormal BMI (<21 kg/m [6] or >30 kg/m [6]), upper or upper/lower incision, and multiple procedures have been associated with increased risk for PPCs [86].
Incidence of acute respiratory distress syndrome (ARDS) after trauma has been reported in 12–25% of injured patients [87]. While studies differ on the mortality attributable to ARDS in trauma patients, with some reporting no increase in mortality in patients experiencing ALI [88], injured patients with ARDS and MOF have mortality rates as high as 50–80% [89].
Multivariable predictors of ARDS after trauma include subject age, Acute Physiology and Chronic Health Evaluation II Score, injury severity score, the presence of blunt traumatic injury, pulmonary contusion, massive transfusion, and flail chest injury (area under the receiver operator characteristic curve 0.79) [90].
4.2.2 Ventilation
4.2.2.1 Emergency General Surgery
There has been increasing evidence that a lung-protective ventilation (LPV) strategy is associated with reduced postoperative pulmonary complications (PPCs), mainly derived from studies on elective abdominal surgery [91]. According to the ALPINE study [85], a recent prospective multicentre observational study, only 4.9% of patients undergoing emergency laparotomy were ventilated using the LPV strategy. In contrast, most patients received a median tidal volume of 8 mL/kg ideal body weight (IBW), a PEEP of 5 cm H2O, and a median peak inspiratory pressure (PIP) of 20 cm H2O. The study revealed that almost half of these patients developed a PPC and that PIP, increased FiO2, and age were significantly associated with it [85].
There is a lack of evidence regarding the best ventilator settings in the specific setting of emergency surgery. However, optimizing mechanical ventilation with protective ventilation is essential to minimize VILI in patients at risk of ARDS undergoing surgical procedures.
Moreover, evidence supports the benefit of lung-protective ventilation strategies in high-risk surgical patients, including EGS patients.
Patients undergoing EGS may present with ARDS or develop this syndrome postoperatively.
The incidence of ARDS in the postoperative period is relatively low, but the impact of ARDS on patient outcomes is significant. The postoperative development of ARDS is associated with prolonged hospitalization, longer duration of mechanical ventilation, increased intensive care unit length of stay, high morbidity, and mortality [91]. EGS patients with postoperative ARDS should be managed according to the ARDSnet guidelines [92].
Despite prone positioning being a major intervention in severe ARDS [92], clinicians remain uncertain whether ARDS patients in the postoperative period of abdominal surgery should be turned prone because of the risk of abdominal complications. Recently, the SAPRONADONF trial demonstrated that the prone position of ARDS patients after abdominal surgery was not associated with an increased rate of surgical complication with clear benefit in terms of oxygenation [93].
Postoperative strategies to decrease the risk of respiratory complications include: head-up or sitting position, encouragement of deep breathing exercises, early mobilization, intensive physiotherapy, incentive spirometry, airway toilette, careful fluid management, and adequate opioid-sparing analgesia. However, high-quality evidence for these strategies is lacking.
Noninvasive positive pressure ventilation (NIMV) or Continuous Positive Airway Pressure (CPAP) can be used to treat early mild ARDS. However, their role as prophylactic measures is unclear in patients with previously healthy lungs at risk of ARDS [94].
Early recognition of underlying respiratory infections and pneumonia should include identifying the causative pathogens, early empiric antibiotic therapy, and subsequent de-escalation to directed therapy in patients with sepsis.
4.2.2.2 Intra-abdominal Hypertension
EGS patients present several recognized risk factors for intra-abdominal hypertension (IAH), especially in patients with a BMI > 30 kg/m2, admitted to the ICU after emergency abdominal surgery or with a diagnosis of pancreatitis [95].
There is an association between IAH and respiratory failure due to the effects of IAH on respiratory mechanics (decrease in lung volumes, respiratory system, but especially chest wall system compliance and increase in airway pressures) and gas exchange (increased dead-space ventilation, intrapulmonary shunt, and lung edema) [96].
The presence of IAH may add to the development of VILI. Optimal ventilator management of patients with ARDS and IAH should include the following:
-
Intra-abdominal, oesophageal pressure, and hemodynamic monitoring;
-
Lung protective ventilation;
-
Deep sedation with or without neuromuscular paralysis in severe ARDS.
-
Open abdomen in selected patients with severe abdominal compartment syndrome [97].
Abdominal-thoracic pressure transmission is around 50% [98]. While keeping driving pressures within safe limits, higher plateau pressures than normally considered might be acceptable [99]. Regli et al. [97] suggest the following correction: corrected target plateau pressure = target plateau pressure − 7 + IAP (mmHg) * 0.7.
Higher positive end-expiratory pressure (PEEP) levels are often required to avoid alveolar collapse, but the optimal PEEP in these patients is still unknown. Some authors suggest setting a PEEP (in cm H2O) equals IAP value (in mmHg) or using esophageal pressure in the most challenging case of IAH and concomitant ARDS [100].
During recruitment maneuvers, higher opening pressures may be required while closely monitoring oxygenation and the hemodynamic response.
Adjunctive therapies to consider are neuro-muscular blocking agents that can reduce IAP and improve oxygenation, negative fluid balance, ascites drainage, and laparostoma [101].
Prone positioning cannot be routinely recommended for IAH patients. However, it may reduce IAP and improve oxygenation in patients with IAH and ARDS if a free-hanging abdomen is assured and no IAP increase is documented [102].
4.2.2.3 Open Abdomen
Patients with an open abdomen (OA) after trauma and nontrauma EGS are usually subjected to prolonged mechanical ventilation, likely due to the need for repeated revision of the laparostoma. Although most patients with an OA have underlying conditions that mandate intubation and mechanical ventilation, the presence of OA does not require intubation per se. Several papers showed that by maintaining negative subdiaphragmatic pressures (a factor that prevents rapid loss of volume during expiration), respiratory musculature can compensate for the loss of the abdominal wall integrity [103].
There are no guidelines or weaning protocols to guide respiratory management, particularly the feasibility of extubating patients with an OA. Taveras et al. demonstrated the feasibility of early extubation in trauma, and EGS patients managed with an OA, possibly decreasing VAP rates with minimal risk of extubation failure [104].
However, patients with OA have a significant risk of developing ARDS early in their ICU course. A lung-protective approach is recommended, and extubation of such patients should be done cautiously.
4.2.2.4 Trauma
The incidence of ARDS in severely injured trauma patients is still significant, with figures approaching 10–30% and intubation rates ranging from 25 to 75% in the specific context of chest trauma [90]. Trauma-related ARDS is a relatively infrequent ARDS risk factor (only 5% of ARDS), and it is associated with lowered mortality rates compared to other causes of ARDS [105]. Nevertheless, the development of ARDS after severe trauma has been associated with significant increases in morbidity and mortality beyond baseline severity of illness [106].
Prevention of lung injury before the onset of ARDS should be considered a cornerstone in managing patients with chest trauma. Optimal pain control and early application of positive end-expiratory pressure (PEEP) can improve the outcome of trauma patients at risk of respiratory deterioration [107, 108].
Factors predisposing multiple trauma patients to respiratory failure are not fully understood. Several scoring systems have been developed to identify patients at risk for pulmonary complications, such as the Lung Organ Failure Score [109] or the Watkins predictive model [90]. While these scores seem to have limited value in the early identification of ARDS, the Thoracic Trauma Severity score [110] seems to be preferable since it predicts both early and delayed ARDS in almost half of the trauma patients with lung contusion [111].
ARDS after trauma may differ from other forms of ARDS. Two distinct patterns have been described: early-onset (days 1–2) ARDS that is associated with higher severity of chest trauma, more severe hypotension, and increased red blood cell transfusion requirement, and late-onset (days 4–5) ARDS where pneumonia, sepsis, and multiorgan dysfunction are the main culprits.
In the setting of trauma, ARDS may occur because of different mechanisms:
-
1.
Direct thoracic injury;
-
2.
Secondary mechanisms induced by trauma, such as fat embolism, transfusion-related lung injury, activation of local and systemic inflammatory mechanisms, or sepsis;
-
3.
Mechanical ventilation: ventilator-induced lung injury (VILI) and ventilator-associated pneumonia (VAP) [112].
Many thoracic injuries can lead to respiratory impairment because they compromise gas exchange, chest-wall mechanic, or both [112]. Pulmonary contusions are well known to evolve towards respiratory failure, usually after a free interval of 24–48 h. A pulmonary contusion surface of 20% of the overall parenchyma was documented as a robust predictive threshold for ARDS (positive predictive values 80%) [113].
Despite current progress in ARDS management, only a limited body of high-quality evidence is available on the best strategy in the specific setting of chest trauma-related ARDS. Two ventilatory strategies are frequently adopted in this context: lung-protective ventilation (LPV) and open-lung ventilation (OLV).
LPV forms the basis of respiratory support, and most experts strongly recommend its use [112].
The ARDSNet protocol includes tidal volumes (VT) of 6–8 mL/kg of PBW, standardized PEEP/FiO2 ratios based on oxygenation, and avoidance of elevation of plateau pressure beyond 30 cm H2O [114].
Trauma is one of the recognized risk factors for ARDS. LPV strategies have never been studied explicitly in chest trauma with associated ARDS, especially in the flail chest. Trauma patients represent only 8–13% of the cohorts of the principal ARDS trials [114,115,116,117,118,119]. Although reducing mortality by using LPV strategies in patients at risk for ARDS has been well documented, LPV is not always applied in trauma patients, especially regarding VT [120]. Interestingly, Plurad et al. [121] demonstrated that the restrictive transfusion policies and ventilation strategies that potentially limit elevations in early peak inspiratory pressures are associated with the decreased incidence of late posttraumatic ARDS observed in the last decades.
OLV seems a reasonable strategy, and it has been more extensively studied in trauma. However, high PEEP may be associated with hemodynamic compromise and significant stress and strain to the heterogeneous lung parenchyma of the trauma patient [116]. Moreover, the OLV strategy is not applicable in the case of air leaks (tracheobronchial rupture, bronchopleural fistula).
In the delicate and heterogeneous trauma setting, it seems necessary to determine the optimal ventilation strategy according to lesional status and phase of treatment.
After the PROSEVA trial demonstrated a mortality benefit using prone positioning in ARDS [122], the 2017 ATS/ESICM/SCCM international consensus guidelines for ARDS management made a strong recommendation for prone positioning in severe ARDS [92].
Of note, exclusion criteria of the PROSEVA trial pertinent to the trauma population included ICP >30, unstable fractures of the spine, femur, or pelvis, burn >20% TSBA, facial trauma, and recent sternotomy or anterior chest tube presence with active air leak [122]. Nevertheless, there is increasing evidence that prone positioning can be used safely with similar oxygenation benefits in trauma and EGS patients [93, 99].
Alternative methods of mechanical ventilation have been studied in ARDS related to chest trauma, such as airway pressure release ventilation (APRV), high-frequency oscillatory ventilation (HFOV), high-frequency percussive ventilation (HFPV), high-frequency jet ventilation (HFJV), or independent lung ventilation.
APRV is a pressure-limited, time-cycled mode of ventilation where a CPAP is applied, with intermittent releases to allow for convective CO2 removal. APRV allows unrestricted spontaneous breathing in any phase of the mechanical ventilation, and APVR showed significant benefit on oxygenation [123] in a cohort of trauma patients, but many issues remain unanswered. Andrews et al. [124] showed a reduction in mortality using early APRV. At the same time, Maung et al. [125] found that APRV increased the duration of mechanical ventilation when compared to conventional ventilation in trauma patients with respiratory failure.
HFOV, a mode characterized by the high-frequency application of minimal tidal volumes, may have some physiological benefit in cases of chest trauma. However, its use is not recommended due to the higher mortality rate observed with HFO in ARDS not related to trauma [117].
HFPV seems an acceptable temporary ventilation strategy in specific cases, such as refractory pulmonary contusions or broncho-pleural disruption.
HFJV may have a role only as a temporary and rescue strategy in the setting of traumatic tracheobronchial rupture during the initial management while waiting for emergent surgical repair.
Independent lung ventilation (ILV) is a complex strategy suitable in rare refractory cases of unilateral chest trauma. The asymmetry in lung pathology, resulting in different compliances between the two lungs, provides the rationale for ILV. ILV has been proposed to ventilate the diseased lung while avoiding hyperinflation in the normal lung, thus improving the ventilation/perfusion matching in each lung [126].
Despite the fear of the hemorrhagic risk, ECMO has to be considered a rescue strategy since it may improve survival [127]. Heparin-free ECMO is a safe and valid option in patients with a high risk of bleeding [128].
Traumatic brain injury (TBI) represents a challenging situation since the ventilatory management goals for lung and brain injury may conflict. Respiratory failure develops in up to one-third of patients suffering from a severe head injury, and it fulfills ARDS criteria in 8% of patients with head abbreviated injury score (AIS) of 4 or greater [129].
In isolated brain injury, a degree of vulnerability is still present in the lung tissue secondary to the proinflammatory state, and high tidal volumes [130] ventilation aggravates it.
High levels of PEEP can increase intrathoracic pressure with a detrimental effect on cerebral venous drainage and cerebral perfusion. However, in case of decreased lung compliance, the transmission of intrathoracic pressure to the cranium is reduced, with a minor effect on cerebral perfusion. Therefore, in the case of ARDS and TBI, PEEP can be safely applied, provided the volume status and mean arterial pressure are maintained.
There is a general lack of good quality clinical studies upon the best strategies to ventilate TBI patients. In 2020, a large consensus conference from the ESICM [131] failed to reach a consensus on several topics and came out with expert-determined recommendations. As a general rule, patients without an Intracranial Pressure Elevation should receive a protective lung strategy. In case TBI and acute lung injury are present together with increased intracranial pressure, the control of PaCO2 takes the priority, even if higher tidal volumes, which can lead to pulmonary injury, are required.
Dos and Don’ts
Do
-
Do admit to ICU only patients with potentially severe physiologic instability, such as EGS patients.
-
Do optimize resource and personnel especially in high volume admission flux.
Don’t
-
Do not overwhelm the HUB ICU; whenever possible use the step down.
-
Do not forget to organize the HUB- SPOKE step down protocols.
Take-Home Message
-
An Intensive Care Unit (ICU) is an organized system that provides specialized medical and nursing care for comprehensive management of patients having, or at risk of developing, acute, life-threatening organ dysfunction.
-
ICU model (open, transitional, or closed) defines who is in charge of the critically ill patient and, as a general rule, the higher the level of the ICU, the higher the share of intensive care trained physicians should be.
-
ICU level refers to the ability to provide specialized care to critically ill patients with increasing complexity of monitoring and treatment.
-
ICU provides a place for monitoring and care of patients with potentially severe physiologic instability, such as EGS patients.
-
There is limited high-quality evidence on the best strategy in the setting of respiratory failure occurring after EGS and trauma. The ventilation strategy should be adapted to lesional status and phase of treatment.
Multiple-Choice Questions
-
1.
One of the following characteristics is not in the definition of critical care medicine:
-
A.
It is focused on the treatment of patients requiring mechanical ventilation; (Correct Answer)
-
B.
The main focus of CCM is restoring normal, or close to normal, physiology;
-
C.
It is a multidisciplinary and interprofessional specialty dedicated to the comprehensive management of patients having, or at risk of developing, acute, life-threatening organ dysfunction;
-
D.
CCM is driven by a multidisciplinary and multispecialty approach to critically ill patients.
-
A.
-
2.
What is\are the main characteristics of a Severity of Illness Scoring System:
-
A.
Calibration ability;
-
B.
Discrimination ability;
-
C.
All the previous; (Correct Answer)
-
D.
None of them.
-
A.
-
3.
A level II ICU should transfer a patient who needs:
-
A.
Mechanical ventilation for a prolonged period;
-
B.
Continuous renal replacement therapy for acute renal failure;
-
C.
Invasive monitoring of Cardiac Output by a pulmonary artery catheter;
-
D.
Invasive monitoring of the Intracranial Pressure. (Correct Answer)
-
A.
-
4.
In the ICU multidisciplinary team can be present:
-
A.
Respiratory therapist;
-
B.
Advanced Care Providers;
-
C.
Clinical Pharmacist;
-
D.
All the above. (Correct Answer)
-
A.
-
5.
What is an “open model” ICU:
-
A.
It is an ICU where every physician with privileges, even without intensive care training, can admit to ICU, and those patients are under his direct care; (Correct Answer)
-
B.
It is an ICU where relatives can visit the patients whenever they want;
-
C.
It is an ICU where only intensivists have privileges to admit and discharge patients in ICU;
-
D.
It is an ICU where the patient is admitted under the care of a nonintensivist, but intensivist consultation is mandatory.
-
A.
-
6.
Which one of the following is the correct statement regarding monitoring of EGS patients?
-
A.
Heart rate, blood pressure, and urine output can always identify low CO states;
-
B.
Pulse oximetry and respiratory rate monitoring is not required in surgical patients;
-
C.
There is a delicate balance between hypovolemia and volume overload, which are both equally associated with complication; (Correct Answer)
-
D.
Focused echocardiography cannot be implemented in EGS setting.
-
A.
-
7.
Ventilator setting after EGS (choose the correct statement):
-
A.
Can be easily protocolized according to current high-level evidence in literature
-
B.
Is critical to minimize VILI in patients at risk of ARDS undergoing surgical procedures; (Correct Answer)
-
C.
Always follows the LPV strategy according to recent surveys
-
D.
Should never be managed according to the ARDSnet guidelines.
-
A.
-
8.
Postoperative strategies to decrease the risk of respiratory complications do not include:
-
A.
Head-up or sitting position and early mobilization
-
B.
Intensive physiotherapy and incentive spirometry
-
C.
Generous fluid administration; (Correct Answer)
-
D.
Adequate opioid-sparing analgesia.
-
A.
-
9.
EGS patients with intra-abdominal hypertension (choose the correct statement):
-
A.
Are not at risk of respiratory failure
-
B.
May require higher PEEP levels, even though optimal PEEP is still unknown; (Correct Answer)
-
C.
Should never undergo prone positioning
-
D.
Should not receive lung protective ventilation.
-
A.
-
10.
ARDS after trauma (choose the correct statement):
-
A.
May occur because of different mechanisms, only early (1–2 days) after trauma
-
B.
Is not related to the extent of pulmonary contusion
-
C.
May require prone positioning, which can be used safely; (Correct Answer)
-
D.
Cannot benefit from lung protective ventilation.
-
A.
-
11.
Respiratory failure in TBI patients (choose the correct statement):
-
A.
Is a rare complication in this setting
-
B.
Can be easily managed like other forms of respiratory failure
-
C.
Cannot benefit from PEEP
-
D.
Is a challenging a situation since the ventilatory management goals for lung and brain injury may conflict. (Correct Answer)
-
A.
References
Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, Fowler RA, Meyfroidt G, Nakagawa S, Pelosi P, Vincent J-L, Vollman K, Zimmerman J. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270–6.
Guidelines for intensive care unit admission, discharge, and triage. Task force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med. 1999;27:633–638.
Valentin A, Ferdinande P, ESICM Working Group on Quality Improvement. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. 2011;37:1575–87.
CICM—professional documents. https://www.cicm.org.au/Resources/Professional-Documents#Policies. Accessed 16 Jan 2021.
Ristagno G, Weil MH. History of critical care medicine: the past, the present and the future. In: Gullo A, Lumb PD, Besso J, Williams GF, eds. Intensive and critical care medicine: WFSICCM World Federation of Societies of Intensive and Critical Care Medicine. Milano: Springer Milan, 2009:3–17. https://doi.org/10.1007/978-88-470-1436-7_1. Accessed 22 Sept 2021.
Brilli RJ, Spevetz A, Branson RD, Campbell GM, Cohen H, Dasta JF, Harvey MA, Kelley MA, Kelly KM, Rudis MI, St Andre AC, Stone JR, Teres D, Weled BJ, American College of Critical Care Medicine Task Force on Models of Critical Care Delivery. The American College of Critical Care Medicine Guidelines for the Definition of an Intensivist and the Practice of Critical Care Medicine. Critical care delivery in the intensive care unit: defining clinical roles and the best practice model. Crit Care Med. 2001;29:2007–19.
Guidelines for the definition of an intensivist and the practice of critical care medicine. Guidelines Committee; Society of Critical Care Medicine. Crit Care Med. 1992;20:540–542.
Guidelines for the provision of intensive care services V2 | The Faculty of Intensive Care Medicine. https://www.ficm.ac.uk/standards-research-revalidation/guidelines-provision-intensive-care-services-v2. Accessed 16 Jan 2021.
Ghaffar S, Pearse RM, Gillies MA. ICU admission after surgery: who benefits? Curr Opin Crit Care. 2017;23:424–9.
Rohrig SAH, Lance MD, Faisal Malmstrom M. Surgical intensive care—current and future challenges? Qatar Med J. 2019;2019:3.
Lyu HG, Najjar P, Havens JM. Past, present, and future of emergency general surgery in the USA. Acute Med Surg. 2018;5:119–22.
Weissman C, Klein N. The importance of differentiating between elective and emergency postoperative critical care patients. J Crit Care. 2008;23:308–16.
Giannoudi M, Harwood P. Damage control resuscitation: lessons learned. Eur J Trauma Emerg Surg. 2016;42:273–82.
Ozdemir BA, Sinha S, Karthikesalingam A, Poloniecki JD, Pearse RM, Grocott MPW, Thompson MM, Holt PJE. Mortality of emergency general surgical patients and associations with hospital structures and processes. Br J Anaesth. 2016;116:54–62.
Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, Vallet B, Vincent J-L, Hoeft A, Rhodes A, European Surgical Outcomes Study (EuSOS) group for the Trials groups of the European Society of Intensive Care Medicine and the European Society of Anaesthesiology. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012;380:1059–65.
Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, Reznor G, Salim A. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015;78:306–11.
Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–30.
Cihoric M, Toft Tengberg L, Bay-Nielsen M, Bang Foss N. Prediction of outcome after emergency high-risk intra-abdominal surgery using the surgical Apgar score. Anesth Analg. 2016;123:1516–21.
Parmar KL, Law J, Carter B, Hewitt J, Boyle JM, Casey P, Maitra I, Farrell IS, Pearce L, Moug SJ, ELF Study Group. Frailty in older patients undergoing emergency laparotomy: results from the UK observational emergency laparotomy and frailty (ELF) study. Ann Surg. 2021;273:709–18.
Hajibandeh S, Hajibandeh S, Antoniou GA, Antoniou SA. Meta-analysis of mortality risk in octogenarians undergoing emergency general surgery operations. Surgery. 2021;169:1407–16.
Green G, Shaikh I, Fernandes R, Wegstapel H. Emergency laparotomy in octogenarians: a 5-year study of morbidity and mortality. World J Gastrointest Surg. 2013;5:216–21.
McCunn M, Dutton RP, Dagal A, Varon AJ, Kaslow O, Kucik CJ, Hagberg CA, McIsaac JH, Pittet J-F, Dunbar PJ, Grissom T, Vavilala MS. Trauma, critical care, and emergency care anesthesiology: a new paradigm for the “acute care” anesthesiologist? Anesth Analg. 2015;121:1668–73.
Privette AR, Evans AE, Moyer JC, Nelson MF, Knudson MM, Mackersie RC, Callcut RA, Cohen MJ. Beyond emergency surgery: redefining acute care surgery. J Surg Res. 2015;196:166–71.
Lissauer ME, Galvagno SM, Rock P, Narayan M, Shah P, Spencer H, Hong C, Diaz JJ. Increased ICU resource needs for an academic emergency general surgery service*. Crit Care Med. 2014;42:910–7.
Michetti CP, Fakhry SM, Brasel K, Martin ND, Teicher EJ, Newcomb A, TRIPP Study Group. Trauma ICU prevalence project: the diversity of surgical critical care. Trauma Surg Acute Care Open. 2019;4:e000288.
Butcher N, Balogh ZJ. AIS>2 in at least two body regions: a potential new anatomical definition of polytrauma. Injury. 2012;43:196–9.
Shere-Wolfe RF, Galvagno SM, Grissom TE. Critical care considerations in the management of the trauma patient following initial resuscitation. Scand J Trauma Resusc Emerg Med. 2012;20:68.
Harris T, Davenport R, Mak M, Brohi K. The evolving science of trauma resuscitation. Emerg Med Clin North Am. 2018;36:85–106.
Kirkpatrick AW, Ball CG, D’Amours SK, Zygun D. Acute resuscitation of the unstable adult trauma patient: bedside diagnosis and therapy. Can J Surg. 2008;51:57–69.
Lemeshow S, Le Gall JR. Modeling the severity of illness of ICU patients. A systems update. JAMA. 1994;272:1049–55.
Alba AC, Agoritsas T, Walsh M, Hanna S, Iorio A, Devereaux PJ, McGinn T, Guyatt G. Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA. 2017;318:1377–84.
McCracken DJ, Lovasik BP, McCracken CE, Frerich JM, McDougal ME, Ratcliff JJ, Barrow DL, Pradilla G. The intracerebral hemorrhage score: a self-fulfilling prophecy? Neurosurgery. 2019;84:741–8.
Cullen DJ, Civetta JM, Briggs BA, Ferrara LC. Therapeutic intervention scoring system: a method for quantitative comparison of patient care. Crit Care Med. 1974;2:57–60. http://pubmed.ncbi.nlm.nih.gov/4832281/. Accessed 1 Sept 2021.
Miranda DR, de Rijk A, Schaufeli W. Simplified Therapeutic Intervention Scoring System: the TISS-28 items—results from a multicenter study. Crit Care Med. 1996;24:64–73.
Reis Miranda D, Moreno R, Iapichino G. Nine equivalents of nursing manpower use score (NEMS). Intensive Care Med. 1997;23:760–5.
Miranda DR, Langrehr D. National and Regional Organisation. In: Miranda DR, Williams A, Loirat PH, editors. Management of intensive care: guidelines for better use of resources. Developments in critical care medicine and anesthesiology. Dordrecht: Springer Netherlands; 1990. p. 83–102. https://doi.org/10.1007/978-94-009-2043-9_4. Accessed 1 Sept 2021.
Iapichino G, Radrizzani D, Bertolini G, Ferla L, Pasetti G, Pezzi A, Porta F, Miranda DR. Daily classification of the level of care. A method to describe clinical course of illness, use of resources and quality of intensive care assistance. Intensive Care Med. 2001;27:131–6.
Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–62.
Groeger JS, Guntupalli KK, Strosberg M, Halpern N, Raphaely RC, Cerra F, Kaye W. Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization. Crit Care Med. 1993;21:279–91.
Groeger JS, Strosberg MA, Halpern NA, Raphaely RC, Kaye WE, Guntupalli KK, Bertram DL, Greenbaum DM, Clemmer TP, Gallagher TJ. Descriptive analysis of critical care units in the United States. Crit Care Med. 1992;20:846–63.
Wilcox ME, Chong CAKY, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, Fan E. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. 2013;41:2253–74.
Hanson CW, Deutschman CS, Anderson HL, Reilly PM, Behringer EC, Schwab CW, Price J. Effects of an organized critical care service on outcomes and resource utilization: a cohort study. Crit Care Med. 1999;27:270–4.
Weled BJ, Adzhigirey LA, Hodgman TM, Brilli RJ, Spevetz A, Kline AM, Montgomery VL, Puri N, Tisherman SA, Vespa PM, Pronovost PJ, Rainey TG, Patterson AJ, Wheeler DS, Task Force on Models for Critical Care. Critical care delivery: the importance of process of care and ICU structure to improved outcomes: an update from the American College of Critical Care Medicine Task Force on Models of Critical Care. Crit Care Med. 2015;43:1520–5.
Harris GH, Baldisseri MR, Reynolds BR, Orsino AS, Sackrowitz R, Bishop JM. Design for implementation of a system-level ICU pandemic surge staffing plan. Crit Care Explor. 2020;2:e0136.
Zangrillo A, Gattinoni L. Learning from mistakes during the pandemic: the Lombardy lesson. Intensive Care Med. 2020;46(8):1622–3.
Guillon A, Laurent E, Godillon L, Kimmoun A, Grammatico-Guillon L. Inter-regional transfers for pandemic surges were associated with reduced mortality rates. Intensive Care Med. 2021;47(7):798–800.
CoBaTrICE Collaboration. The educational environment for training in intensive care medicine: structures, processes, outcomes and challenges in the European region. Intensive Care Med. 2009;35:1575–83.
Gershengorn HB, Harrison DA, Garland A, Wilcox ME, Rowan KM, Wunsch H. Association of intensive care unit patient-to-intensivist ratios with hospital mortality. JAMA Intern Med. 2017;177:388–96.
McKinley S, Elliott D. Twenty-five years of critical care nursing scholarship in Australia. Aust Crit Care. 2013;26:7–11.
Safar P, Dekornfeld TJ, Pearson JW, Redding JS. The intensive care unit. A three year experience at Baltimore city hospitals. Anaesthesia. 1961;16:275–84.
Kerlin MP, Costa DK, Kahn JM. The Society of Critical Care Medicine at 50 years: ICU organization and management. Crit Care Med. 2021;49:391–405.
Xu Y, Xu Z, Zhang J. The nursing education system in the People’s Republic of China: evolution, structure and reform. Int Nurs Rev. 2000;47:207–17.
Endacott R, Jones C, Bloomer MJ, Boulanger C, Ben Nun M, Lliopoulou KK, Egerod I, Blot S. The state of critical care nursing education in Europe: an international survey. Intensive Care Med. 2015;41:2237–40.
Guilhermino MC, Inder KJ, Sundin D. Education on invasive mechanical ventilation involving intensive care nurses: a systematic review. Nurs Crit Care. 2018;23:245–55.
Perioperative and intensive care management of the surgical patient—ClinicalKey. https://www-clinicalkey-com.ospbg.clas.cineca.it/#!/content/book/3-s2.0-B9780702072475000050?indexOverride=GLOBAL. Accessed 7 Jan 2021.
Donovan AL, Aldrich JM, Gross AK, Barchas DM, Thornton KC, Schell-Chaple HM, Gropper MA, Lipshutz AKM, University of California, San Francisco Critical Care Innovations Group. Interprofessional care and teamwork in the ICU. Crit Care Med. 2018;46:980–90.
Reeves S, Lewin S, Espin S, Zwarenstein M. Interprofessional teamwork for health and social care. Hoboken: Wiley; 2011.
Scherzer R, Dennis MP, Swan BA, Kavuru MS, Oxman DA. A comparison of usage and outcomes between nurse practitioner and resident-staffed medical ICUs. Crit Care Med. 2017;45:e132–7.
Kawar E, DiGiovine B. MICU care delivered by PAs versus residents: do PAs measure up? JAAPA. 2011;24:36–41.
Rudis MI, Brandl KM. Position paper on critical care pharmacy services. Society of Critical Care Medicine and American College of Clinical Pharmacy Task Force on Critical Care Pharmacy Services. Crit Care Med. 2000;28:3746–50.
Erstad BL, Haas CE, O’Keeffe T, Hokula CA, Parrinello K, Theodorou AA. Interdisciplinary patient care in the intensive care unit: focus on the pharmacist. Pharmacotherapy. 2011;31:128–37.
Baker A. Crossing the quality chasm: a new health system for the 21st century. BMJ. 2001;323:1192.
Papali A, Adhikari NKJ, Diaz JV, Dondorp AM, Dünser MW, Jacob ST, Phua J, Romain M, Schultz MJ. Infrastructure and organization of adult intensive care units in resource-limited settings. In: Dondorp AM, Dünser MW, Schultz MJ, editors. Sepsis management in resource-limited settings. Cham: Springer; 2019. http://www.ncbi.nlm.nih.gov/books/NBK553820/. Accessed 13 July 2021.
Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007;16:2–3.
Modrykamien AM. The ICU follow-up clinic: a new paradigm for intensivists. Respir Care. 2012;57:764–72.
Kipnis E, Ramsingh D, Bhargava M, Dincer E, Cannesson M, Broccard A, Vallet B, Bendjelid K, Thibault R. Monitoring in the intensive care. Crit Care Res Pract. 2012;2012:473507.
Martin ND, Codner P, Greene W, Brasel K, Michetti C, AAST Critical Care Committee. Contemporary hemodynamic monitoring, fluid responsiveness, volume optimization, and endpoints of resuscitation: an AAST Critical Care Committee Clinical Consensus. Trauma Surg Acute Care Open. 2020;5:e000411.
Celoria G, Steingrub JS, Vickers-Lahti M, Teres D, Stein KL, Fink M, Friedmann P. Clinical assessment of hemodynamic values in two surgical intensive care units. Effects on therapy. Arch Surg. 1990;125:1036–9.
Convertino VA, Ryan KL, Rickards CA, Salinas J, McManus JG, Cooke WH, Holcomb JB. Physiological and medical monitoring for en route care of combat casualties. J Trauma. 2008;64:S342–53.
Abou-Khalil B, Scalea TM, Trooskin SZ, Henry SM, Hitchcock R. Hemodynamic responses to shock in young trauma patients: need for invasive monitoring. Crit Care Med. 1994;22:633–9.
Nagre AS. Focus-assessed transthoracic echocardiography: implications in perioperative and intensive care. Ann Card Anaesth. 2019;22:302–8.
Cowie BS. Focused transthoracic echocardiography in the perioperative period. Anaesth Intensive Care. 2010;38:823–36.
Britt LD, Trunkey DD, Feliciano DV. Acute care surgery. Principles and practice. In: Acute care surgery. Principles and practice. Vol. The perioperative management of the acute care surgical patient. Springer; 2007. p. 67–83.
Lamberti JP. Respiratory monitoring in general care units. Respir Care. 2020;65:870–81.
Kochanek PM, Carney N, Adelson PD, Ashwal S, Bell MJ, Bratton S, Carson S, Chesnut RM, Ghajar J, Goldstein B, Grant GA, Kissoon N, Peterson K, Selden NR, Tasker RC, Tong KA, Vavilala MS, Wainwright MS, Warden CR, American Academy of Pediatrics-Section on Neurological Surgery, American Association of Neurological Surgeons/Congress of Neurological Surgeons, Child Neurology Society, European Society of Pediatric and Neonatal Intensive Care, Neurocritical Care Society, Pediatric Neurocritical Care Research Group, Society of Critical Care Medicine, Paediatric Intensive Care Society UK, Society for Neuroscience in Anesthesiology and Critical Care, World Federation of Pediatric Intensive and Critical Care Societies. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents—second edition. Pediatr Crit Care Med. 2012;13 Suppl 1:S1–S82.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GWJ, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, Rubiano AM, Shutter L, Tasker RC, Vavilala MS, Wilberger J, Wright DW, Ghajar J. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Hawryluk GWJ, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, Arrastia RD, Diringer M, Figaji A, Gao G, Geocadin R, Ghajar J, Harris O, Hoffer A, Hutchinson P, Joseph M, Kitagawa R, Manley G, Mayer S, Menon DK, Meyfroidt G, Michael DB, Oddo M, Okonkwo D, Patel M, Robertson C, Rosenfeld JV, Rubiano AM, Sahuquillo J, Servadei F, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019;45:1783–94. https://springerlink.bibliotecabuap.elogim.com/epdf/10.1007/s00134-019-05805-9. Accessed 1 Sept 2020.
Chesnut RM, Temkin N, Videtta W, Petroni G, Lujan S, Pridgeon J, Dikmen S, Chaddock K, Barber J, Machamer J, Guadagnoli N, Hendrickson P, Aguilera S, Alanis V, Bello Quezada ME, Bautista Coronel E, Bustamante LA, Cacciatori AC, Carricondo CJ, Carvajal F, Davila R, Dominguez M, Figueroa Melgarejo JA, Fillipi MM, Godoy DA, Gomez DC, Lacerda Gallardo AJ, Guerra Garcia JA, la Fuente Zerain G, Lavadenz Cuientas LA, et al. Consensus-Based Management Protocol (CREVICE Protocol) for the treatment of severe traumatic brain injury based on imaging and clinical examination for use when intracranial pressure monitoring is not employed. J Neurotrauma. 2020;37:1291–9.
Chesnut R, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, Arrastia RD, Diringer M, Figaji A, Gao G, Geocadin R, Ghajar J, Harris O, Hoffer A, Hutchinson P, Joseph M, Kitagawa R, Manley G, Mayer S, Menon DK, Meyfroidt G, Michael DB, Oddo M, Okonkwo D, Patel M, Robertson C, Rosenfeld JV, Rubiano AM, Sahuquillo J, Servadei F, et al. A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2020;46:919–29.
Tengberg LT, Cihoric M, Foss NB, Bay-Nielsen M, Gögenur I, Henriksen R, Jensen TK, Tolstrup M-B, Nielsen LBJ. Complications after emergency laparotomy beyond the immediate postoperative period—a retrospective, observational cohort study of 1139 patients. Anaesthesia. 2017;72:309–16.
McCoy CC, Englum BR, Keenan JE, Vaslef SN, Shapiro ML, Scarborough JE. Impact of specific postoperative complications on the outcomes of emergency general surgery patients. J Trauma Acute Care Surg. 2015;78:912–8; discussion 918–919.
Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, Lee J-W, Henderson WG, Moss A, Mehdiratta N, Colwell MM, Bartels K, Kolodzie K, Giquel J, Vidal Melo MF. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the Perioperative Research Network Investigators. JAMA Surg. 2017;152:157–66.
Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, Sabaté S, Mazo V, Briones Z, Sanchis J, ARISCAT Group. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113:1338–50.
Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118:317–34.
Watson X, Chereshneva M, Odor PM, Chis Ster I, Pan-London Perioperative Audit and Research Network (PLAN), Cecconi M. Adoption of lung protective ventilation IN patients undergoing emergency laparotomy: the ALPINE study. A prospective multicentre observational study. Br J Anaesth 2018;121:909–917.
Serejo LGG, da Silva-Júnior FP, Bastos JPC, de Bruin GS, Mota RMS, de Bruin PFC. Risk factors for pulmonary complications after emergency abdominal surgery. Respir Med. 2007;101:808–13.
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–93.
Treggiari MM, Hudson LD, Martin DP, Weiss NS, Caldwell E, Rubenfeld G. Effect of acute lung injury and acute respiratory distress syndrome on outcome in critically ill trauma patients. Crit Care Med. 2004;32:327–31.
Holland MC, Mackersie RC, Morabito D, Campbell AR, Kivett VA, Patel R, Erickson VR, Pittet J-F. The development of acute lung injury is associated with worse neurologic outcome in patients with severe traumatic brain injury. J Trauma. 2003;55:106–11.
Watkins TR, Nathens AB, Cooke CR, Psaty BM, Maier RV, Cuschieri J, Rubenfeld GD. Acute respiratory distress syndrome after trauma: development and validation of a predictive model. Crit Care Med. 2012;40:2295–303.
Serpa Neto A, Hemmes SNT, Barbas CSV, Beiderlinden M, Biehl M, Binnekade JM, Canet J, Fernandez-Bustamante A, Futier E, Gajic O, Hedenstierna G, Hollmann MW, Jaber S, Kozian A, Licker M, Lin W-Q, Maslow AD, Memtsoudis SG, Reis Miranda D, Moine P, Ng T, Paparella D, Putensen C, Ranieri M, Scavonetto F, Schilling T, Schmid W, Selmo G, Severgnini P, Sprung J, et al. Protective versus conventional ventilation for surgery: a systematic review and individual patient data meta-analysis. Anesthesiology. 2015;123:66–78.
Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, Adhikari NKJ, Amato MBP, Branson R, Brower RG, Ferguson ND, Gajic O, Gattinoni L, Hess D, Mancebo J, Meade MO, McAuley DF, Pesenti A, Ranieri VM, Rubenfeld GD, Rubin E, Seckel M, Slutsky AS, Talmor D, Thompson BT, Wunsch H, Uleryk E, Brozek J, Brochard LJ, American Thoracic Society, European Society of Intensive Care Medicine, and Society of Critical Care Medicine. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–63.
Gaudry S, Tuffet S, Lukaszewicz A-C, Laplace C, Zucman N, Pocard M, Costaglioli B, Msika S, Duranteau J, Payen D, Dreyfuss D, Hajage D, Ricard J-D. Prone positioning in acute respiratory distress syndrome after abdominal surgery: a multicenter retrospective study: SAPRONADONF (Study of Ards and PRONe position After abDOmiNal surgery in France). Ann Intensive Care. 2017;7:21.
Ireland CJ, Chapman TM, Mathew SF, Herbison GP, Zacharias M. Continuous positive airway pressure (CPAP) during the postoperative period for prevention of postoperative morbidity and mortality following major abdominal surgery. Cochrane Database Syst Rev. 2014;2014:CD008930.
Smit M, Koopman B, Dieperink W, Hulscher JBF, Hofker HS, van Meurs M, Zijlstra JG. Intra-abdominal hypertension and abdominal compartment syndrome in patients admitted to the ICU. Ann Intensive Care. 2020;10:130.
Ranieri VM, Brienza N, Santostasi S, Puntillo F, Mascia L, Vitale N, Giuliani R, Memeo V, Bruno F, Fiore T, Brienza A, Slutsky AS. Impairment of lung and chest wall mechanics in patients with acute respiratory distress syndrome: role of abdominal distension. Am J Respir Crit Care Med. 1997;156:1082–91.
Regli A, Pelosi P, Malbrain MLNG. Ventilation in patients with intra-abdominal hypertension: what every critical care physician needs to know. Ann Intensive Care. 2019;9:52.
De Keulenaer BL, De Waele JJ, Powell B, Malbrain MLNG. What is normal intra-abdominal pressure and how is it affected by positioning, body mass and positive end-expiratory pressure? Intensive Care Med. 2009;35:969–76.
Voggenreiter G, Aufmkolk M, Stiletto RJ, Baacke MG, Waydhas C, Ose C, Bock E, Gotzen L, Obertacke U, Nast-Kolb D. Prone positioning improves oxygenation in post-traumatic lung injury—a prospective randomized trial. J Trauma. 2005;59:333–41; discussion 341–343.
Tonetti T, Cavalli I, Ranieri VM, Mascia L. Respiratory consequences of intra-abdominal hypertension. Minerva Anestesiol. 2020;86:877–83.
De Keulenaer B, Regli A, De Laet I, Roberts D, Malbrain MLNG. What’s new in medical management strategies for raised intra-abdominal pressure: evacuating intra-abdominal contents, improving abdominal wall compliance, pharmacotherapy, and continuous negative extra-abdominal pressure. Anaesthesiol Intensive Ther. 2015;47:54–62.
Kirkpatrick AW, Pelosi P, De Waele JJ, Malbrain ML, Ball CG, Meade MO, Stelfox HT, Laupland KB. Clinical review: intra-abdominal hypertension: does it influence the physiology of prone ventilation? Crit Care. 2010;14:232.
Mondal P, Abu-Hasan M, Saha A, Pitts T, Rose M, Bolser DC, Davenport PW. Effect of laparotomy on respiratory muscle activation pattern. Physiol Rep. 2016;4:e12668.
Taveras LR, Imran JB, Cunningham HB, Madni TD, Taarea R, Tompeck A, Clark AT, Provenzale N, Adeyemi FM, Minshall CT, Eastman AL, Cripps MW. Trauma and emergency general surgery patients should be extubated with an open abdomen. J Trauma Acute Care Surg. 2018;85:1043–7.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, Ranieri M, Rubenfeld G, Thompson BT, Wrigge H, Slutsky AS, Pesenti A, LUNG SAFE Investigators, ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Shah CV, Localio AR, Lanken PN, Kahn JM, Bellamy S, Gallop R, Finkel B, Gracias VH, Fuchs BD, Christie JD. The impact of development of acute lung injury on hospital mortality in critically ill trauma patients. Crit Care Med. 2008;36:2309–15.
Chiumello D, Coppola S, Froio S, Gregoretti C, Consonni D. Noninvasive ventilation in chest trauma: systematic review and meta-analysis. Intensive Care Med. 2013;39:1171–80.
Bouzat P, Raux M, David JS, Tazarourte K, Galinski M, Desmettre T, Garrigue D, Ducros L, Michelet P, Expert’s Group, Freysz M, Savary D, Rayeh-Pelardy F, Laplace C, Duponq R, Monnin Bares V, D’Journo XB, Boddaert G, Boutonnet M, Pierre S, Léone M, Honnart D, Biais M, Vardon F. Chest trauma: first 48 hours management. Anaesth Crit Care Pain Med. 2017;36:135–45.
Wutzler S, Wafaisade A, Maegele M, Laurer H, Geiger EV, Walcher F, Barker J, Lefering R, Marzi I, Trauma Registry of DGU. Lung Organ Failure Score (LOFS): probability of severe pulmonary organ failure after multiple injuries including chest trauma. Injury. 2012;43:1507–12.
Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504.
Daurat A, Millet I, Roustan J-P, Maury C, Taourel P, Jaber S, Capdevila X, Charbit J. Thoracic Trauma Severity score on admission allows to determine the risk of delayed ARDS in trauma patients with pulmonary contusion. Injury. 2016;47:147–53.
Ramin S, Charbit J, Jaber S, Capdevila X. Acute respiratory distress syndrome after chest trauma: epidemiology, specific physiopathology and ventilation strategies. Anaesth Crit Care Pain Med. 2019;38:265–76.
Miller PR, Croce MA, Bee TK, Qaisi WG, Smith CP, Collins GL, Fabian TC. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51:223–8; discussion 229–230.
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8.
Mercat A, Richard J-CM, Vielle B, Jaber S, Osman D, Diehl J-L, Lefrant J-Y, Prat G, Richecoeur J, Nieszkowska A, Gervais C, Baudot J, Bouadma L, Brochard L, Expiratory Pressure (Express) Study Group. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:646–55.
Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, Davies AR, Hand LE, Zhou Q, Thabane L, Austin P, Lapinsky S, Baxter A, Russell J, Skrobik Y, Ronco JJ, Stewart TE, Lung Open Ventilation Study Investigators. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:637–45.
Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P, Zhou Q, Matte A, Walter SD, Lamontagne F, Granton JT, Arabi YM, Arroliga AC, Stewart TE, Slutsky AS, Meade MO, OSCILLATE Trial Investigators, Canadian Critical Care Trials Group. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med. 2013;368:795–805.
Papazian L, Forel J-M, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal J-M, Perez D, Seghboyan J-M, Constantin J-M, Courant P, Lefrant J-Y, Guérin C, Prat G, Morange S, Roch A, ACURASYS Study Investigators. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–16.
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36.
Zochios V, Chandan JS, Dunne É, Sherwin J, Torlinski T. Adherence to least injurious tidal volume ventilation in thoracic trauma: a tertiary trauma centre retrospective cohort analysis. J Intensive Care Soc. 2019;20:NP10–3.
Plurad D, Martin M, Green D, Salim A, Inaba K, Belzberg H, Demetriades D, Rhee P. The decreasing incidence of late posttraumatic acute respiratory distress syndrome: the potential role of lung protective ventilation and conservative transfusion practice. J Trauma. 2007;63:1–7; discussion 8.
Guérin C, Reignier J, Richard J-C, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, Clavel M, Chatellier D, Jaber S, Rosselli S, Mancebo J, Sirodot M, Hilbert G, Bengler C, Richecoeur J, Gainnier M, Bayle F, Bourdin G, Leray V, Girard R, Baboi L, Ayzac L, PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–68. https://doi.org/10.1056/NEJMoa1214103. Epub 2013 May 20. PMID: 23688302.
Dart BW, Maxwell RA, Richart CM, Brooks DK, Ciraulo DL, Barker DE, Burns RP. Preliminary experience with airway pressure release ventilation in a trauma/surgical intensive care unit. J Trauma. 2005;59:71–6.
Andrews PL, Shiber JR, Jaruga-Killeen E, Roy S, Sadowitz B, O’Toole RV, Gatto LA, Nieman GF, Scalea T, Habashi NM. Early application of airway pressure release ventilation may reduce mortality in high-risk trauma patients: a systematic review of observational trauma ARDS literature. J Trauma Acute Care Surg. 2013;75:635–41.
Maung AA, Schuster KM, Kaplan LJ, Ditillo MF, Piper GL, Maerz LL, Lui FY, Johnson DC, Davis KA. Compared to conventional ventilation, airway pressure release ventilation may increase ventilator days in trauma patients. J Trauma Acute Care Surg. 2012;73:507–10.
Cinnella G, Dambrosio M, Brienza N, Giuliani R, Bruno F, Fiore T, Brienza A. Independent lung ventilation in patients with unilateral pulmonary contusion. Monitoring with compliance and EtCO(2). Intensive Care Med. 2001;27:1860–7.
Guirand DM, Okoye OT, Schmidt BS, Mansfield NJ, Aden JK, Martin RS, Cestero RF, Hines MH, Pranikoff T, Inaba K, Cannon JW. Venovenous extracorporeal life support improves survival in adult trauma patients with acute hypoxemic respiratory failure: a multicenter retrospective cohort study. J Trauma Acute Care Surg. 2014;76:1275–81.
Robba C, Ortu A, Bilotta F, Lombardo A, Sekhon MS, Gallo F, Matta BF. Extracorporeal membrane oxygenation for adult respiratory distress syndrome in trauma patients: a case series and systematic literature review. J Trauma Acute Care Surg. 2017;82:165–73.
Bakowitz M, Bruns B, McCunn M. Acute lung injury and the acute respiratory distress syndrome in the injured patient. Scand J Trauma Resusc Emerg Med. 2012;20:54.
Mascia L, Zavala E, Bosma K, Pasero D, Decaroli D, Andrews P, Isnardi D, Davi A, Arguis MJ, Berardino M, Ducati A, Brain IT Group. High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med. 2007;35:1815–20.
Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, Chieregato A, Cinotti R, Duranteau J, Einav S, Ercole A, Ferguson N, Guerin C, Siempos II, Kurtz P, Juffermans NP, Mancebo J, Mascia L, McCredie V, Nin N, Oddo M, Pelosi P, Rabinstein AA, Neto AS, Seder DB, Skrifvars MB, Suarez JI, Taccone FS, van der Jagt M, Citerio G, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020;46:2397–410.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Di Matteo, M., Corbella, D. (2023). Critical Care Medicine. In: Coccolini, F., Catena, F. (eds) Textbook of Emergency General Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-22599-4_13
Download citation
DOI: https://doi.org/10.1007/978-3-031-22599-4_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-22598-7
Online ISBN: 978-3-031-22599-4
eBook Packages: MedicineMedicine (R0)