Abstract
The field of transplantation has provided tremendous progress to diabetic patients. One way to objectify this development is to determine the survival benefit of transplantation in the four diabetic recipient categories: simultaneous pancreas/kidney transplant (SPK), pancreas after kidney transplant (PAK), pancreas transplant alone (PTA), and kidney transplant alone (KTA). Over a 21-year time period, from January 1, 2000, to May 31, 2021, the International Pancreas Transplant Registry/United Network for Organ Sharing (IPTR/UNOS) collected information about listing and transplant outcome of diabetic patients. A total of 212,049 patient records were reviewed: 89,579 recipients who underwent pancreas and/or kidney transplantation and 122,470 patients who were placed on the waiting list and are still waiting or were removed from the waitlist due to deteriorating health or death. To determine the survival benefit of pancreas transplantation, patient survival on the waiting list versus after transplantation was defined as primary outcome. Over the 21-year time period, pancreas and/or kidney transplantation in all 4 diabetic recipient categories saved a total of 273,843 life-years. On average, 11.7 life-years per patient were saved in the SPK category, 6.4 life-years in the PTA category, 6.3 life-years in the PAK category, and 6.6 life-years in the KTA category. The survival benefit of pancreas and/or kidney transplant recipients was highly significant compared to diabetic patients still waiting for transplantation. The survival benefit was higher for patients with type 1 versus type 2 diabetes mellitus. The significant survival benefit of PTA recipients versus patients on the waiting list justifies the argument for pre-emptive pancreas transplantation, i.e., before the development of end-stage renal disease. Given the survival benefit as evidenced in 273,843 life-years saved, pancreas transplantation should be more widely applied, and pancreas donation encouraged.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pancreas transplantation
- Pancreas transplant alone (PTA)
- Pancreas after kidney transplant (PAK)
- Simultaneous pancreas/kidney transplant (SPK)
- Kidney transplant alone (KTA)
- Waiting list
- Survival benefit
- Mortality
- Life-years
- Life-years saved
Introduction
The first pancreas transplant was performed by William Kelly and Richard Lillehei at the University of Minnesota on December 17, 1966, but the field of pancreas transplantation was initially marred by high graft failure rates due to technical and immunological complications (see Chaps. 5 and 66). For that reason, until the early 1980s, less than 100 pancreas transplants per year were performed worldwide. With major improvements in surgical techniques and immunosuppressive therapy that number had increased to 1000 pancreas transplants per year in the early 1990s and to >2000 pancreas transplants per year after the turn of the millennium. By the end of 2020, more than 63,000 pancreas transplants had been performed worldwide with an average of 2300 transplants per year from 2010 to 2020. Despite this increase, the number of pancreas transplants has continued to substantially trail those of kidney and liver transplants. For that reason, survival benefit analyses of pancreas transplantation have also lagged those for kidney and liver transplantation [1,2,3,4]. In the past, only few studies have systematically analyzed the survival benefit of pancreas transplantation.
Life-Enhancing Versus Life-Saving Transplants
Survival benefit studies have resulted in a better understanding of life-enhancing versus life-saving transplants. Liver, heart, and lung transplants have always been considered life-saving procedures whereas kidney and pancreas transplantation were regarded as life-enhancing procedures.
In the case of kidney transplantation, the argument for merely a life-enhancing procedure was initially made because recipients are simply relieved of the requirement of dialysis. However, the survival advantage of kidney transplant recipients versus transplant candidates on dialysis was clearly shown by Port et al. in the early 1990s [1, 3, 5]. Although the overall mortality risk following kidney transplantation was initially increased, there was a long-term survival benefit for transplant recipients compared with similar patients on dialysis. In a study published two decades later [6, 7], it was shown that a kidney transplant is also a life-saving procedure: the number of life-years saved per kidney transplant recipient was akin to the number of life-years saved per liver transplant recipient. That same study also demonstrated a significant survival advantage for adult kidney transplant recipients of living-donor transplants compared with deceased-donor transplants [8, 9]: the median survival time was 18.5 years with a living donor versus 9.8 years with a deceased donor.
Akin to kidney transplantation, a pancreas transplant must also be considered a life-saving procedure.
For a long time, the perception has persisted that a pancreas transplant is simply an alternative to insulin replacement therapy, despite evidence in the literature to the contrary [9,10,11,12,13]. Unlike liver and heart transplants, pancreas transplants are usually not immediately life-saving procedures.
However, their life-saving nature becomes evident within several months posttransplant by decreasing the recipients’ risk of death from hypoglycemic unawareness, cardio-cerebrovascular events, and other secondary diabetic complications.
Methodological Survival Study Limitations
From a statistical point of view, comparative survival benefit analyses are complex due to an intrinsic selection bias for those candidates who undergo transplants. To overcome this bias, some studies have conducted sophisticated matching with propensity scores. However, a significant selection bias may remain and must be considered a limitation. The selection bias is also complicated by differences in listing criteria for candidates and recipient categories according to individual transplant centers and physicians. Another limitation of such studies is the bias introduced by the waiting time for patients who undergo transplants. These transplant candidates, by definition, had to survive their time on the waiting list. A third limitation is the variable entry completion by era, limiting the effectiveness of propensity score matching.
Another consideration is that the content of the database must be meticulously surveyed to avoid incorrect conclusions based on unscrutinized information. This occurred in a survival study in recipients of solitary pancreas transplants that supposedly showed that survival was significantly worse compared with the survival of waiting-list candidates receiving conventional therapy [14]. Using the same database but eliminating patients with multiple listings at different transplant centers or with false or incomplete information showed the exact opposite result [15] (see Chap. 22).
Lastly, direct group comparison between the four diabetic transplant categories (simultaneous pancreas/kidney transplant [SPK], pancreas transplant alone [PTA], pancreas after kidney transplant [PAK], kidney transplant alone [KTA]) is difficult because of preexisting conditions and choice of transplant category.
The Survival Benefit of Pancreas Transplantation in the Literature
Several single-center studies have shown a survival benefit for pancreas transplant recipients by comparing SPK with diabetic kidney transplant alone (KTA) recipients. A Dutch study by Smets et al. [12] not only found that the hazard ratio for mortality after the start of renal replacement therapy was significantly lower for SPK versus KTA recipients but also showed that the mortality ratio was lower for transplanted versus non-transplanted patients . A British study compared mortality between pancreas transplant recipients with a control group of patients on the waiting list. The authors noted a significantly higher waiting-list mortality of 30% compared with a mortality of 9% after transplantation. In addition, deaths on the waiting list compared with transplantation up to 1 year had a relative risk of 2.67, while those surviving >1 year had a relative risk of 5.89 of dying on the waiting list [16]. This finding is in line with an IPTR analysis that showed that the mortality risk of the transplant procedure itself is higher only within the first few months of the first transplant year (SPK, 59 days posttransplant; PAK, 80 days posttransplant; PTA, 230 days posttransplant) and then significantly decreases below the waitlist mortality for the remainder of the first posttransplant year [15].
The hitherto most comprehensive study of survival benefit after all types of solid organ transplants in the United States and covering a 25-year time period found a significant survival advantage for all types of pancreas transplants irrespective of the recipient category [6]. The strongest survival advantage was noted for SPK recipients (4.7 life-years per recipient). A PTA conferred a median survival time of 13.6 years (compared with 8 years in patients on the waiting list). The survival benefit became more pronounced with long-term follow-up. The authors also noted that there was an earlier controversy (see above) about the survival benefit of solitary pancreas transplants in studies with five years of follow-up [14, 15]. In Rana et al.’s study, the follow-up time was up to 20 years; their findings unequivocally confirmed the survival benefits of solitary pancreas transplants in the PTA and PAK categories over waitlisted patients [6].
Survival Benefit According to International Pancreas Transplant Registry/United Network for Organ Sharing (IPTR/UNOS)
A new IPTR analysis (see Chap. 66) determined the survival benefit for pancreas and/or kidney transplants based on the IPTR/UNOS database and the Social Security Administration Death Master File for the time period from January 1, 2000, to May 31, 2021. During that time period, 212,049 diabetic patients were listed for a primary deceased-donor transplant. In total, 184,927 patients were listed for a KTA, 21,244 for an SPK, 3512 for a PAK, and 2366 for a PTA. The distributions of the different diabetes categories are significantly different and are shown in Table 67.1. While diabetic patients listed for a KTA transplant are more likely to have type 2 diabetes mellitus, patients listed in the solitary pancreas categories (PTA and PAK) are more likely to be type 1 as are patients listed for an SPK transplant.
Overall, 89,579 diabetic patients underwent a pancreas and/or kidney transplant and 122,470 patients were still on the waiting list, were taken off the list, or had died while waiting. There were 69,041 KTA, 16,088 SPK, 2667 PAK, and 1783 PTA recipients. Adjustments were made for multiple listings, incomplete information, and classifications. The primary outcome was patient survival while on the waiting list or after transplant adjusted for potential confounders.
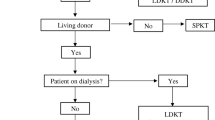
The overall waitlist mortality for all listed diabetic patients regardless of their transplant status is shown in Fig. 67.1; it was highest for SPK and KTA candidates. The median waitlist survival for all diabetic patients (type 1 and 2 diabetes) was 5.0 years for SPK, 5.8 years for KTA, 8.6 years for PAK, and 11.6 years for PTA candidates. By diabetes type, the median survival for patients listed with type 1 (versus type 2) diabetes mellitus was 4.9 (5.2) years for KTA, 5.0 (5.4) years for SPK, 8.6 (8.2) years for PAK, and 12.0 (−) years for PTA candidates. Listings for PTA candidates with type 2 are very rare and the number of candidates is too low for analysis. The waitlist mortality of KTA and SPK listings was higher for patients with type 1 compared to patients with type 2 diabetes mellitus. Only in PAK listings was the mortality in type 2 candidates higher than in type 1 candidates.
A multivariable model for mortality risk assessment showed in all four categories a significant decrease in the mortality risk after transplantation compared to remaining on the waitlist. The highest risk reduction was achieved in the SPK category: it reduced the relative mortality risk by 94%. In the KTA category the relative mortality risk was reduced by 86%; in the PAK category, by 78%; and in the PTA category, by 70%. The relative mortality risk was 25% lower in type 2 versus type 1 diabetic patients. Being on dialysis increased the relative waitlist mortality in the SPK category by 38% and by 21% in the KTA category. In all four categories, the relative mortality risk significantly increased with increasing age at listing.
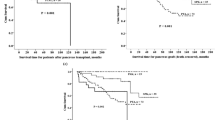
To assess life-year saved, the patients who remained on the waitlist were used as control to assess the effect of the transplant. All computations were performed from the time of listing. To compute the life-years saved, the area under the survival curve for patients who remained on the waitlist is subtracted from the area under the survival curve for the patients who received a deceased-donor transplant. Figure 67.2 shows the significant life-saving impact of a KTA compared to remaining on the waitlist. The median survival on the waitlist was 4.1 years compared to 11.6 years after receiving a KTA. Figure 67.3 shows the results in the SPK category. The median waitlist survival of 2.7 years compares to 17.0 years for patients who received the transplant. Figures 67.4 and 67.5 show the results for solitary pancreas transplants. The median survival on the waitlist is significantly higher than in the SPK category (6.7 years in the PAK and 11.4 years in the PTA categories). In contrast, for transplanted patients, the median survival time in the PAK category was 14.3 years and 18.3 years in the PTA category.
According to this IPTR analysis, primary deceased-donor pancreas and/or kidney transplants in diabetic patients saved a total of 273,843 life-years: on average, 6.6 life-years per patient were saved by KTA, 11.7 per patient by SPK, 6.3 per patient years by PAK, and 6.4 per patient by PTA transplants (Table 67.2). When the survival benefit only for patients with type 1 diabetes mellitus was computed, the average life-years saved for PAK remained the same but increased slightly for PTA (6.6 years) and SPK (11.9 years) transplants. For KTA transplants in patients with type 1 diabetes mellitus, the life-years saved per person increased to 8.2 years, which was still lower compared to SPK recipients (Table 67.3).
In addition, the gain in life-years has also had an impact on employment and societal re-integration: significantly more PTA and PAK versus SPK recipients worked for income after than before transplantation [17].
Conclusions
The life-saving nature and survival benefit of a kidney and/or pancreas transplant in all four diabetic recipient categories have repeatedly been demonstrated in registry and single-center studies. These findings go along with a significant increase in life expectancy after pancreas and/or kidney transplantation. Although the transplant procedures themselves are associated with a certain mortality risk, that risk exceeds the mortality risk on the waiting list only for the first few weeks or months after transplantation. The highest impact on outcome was found in the SPK category in which almost twice as many life-years were saved as in the KTA category. In general, dialysis status is a very influential risk factor for mortality: pre-emptive transplants before the development of end-stage renal disease increase life expectancy significantly. For that reason, the gain in survival time was less pronounced in the PAK category due to the previously restored kidney function, which resulted in a lower waitlist mortality than in the SPK and KTA categories. Patients in the PTA category represent the healthiest population due to the lack of advanced secondary diabetic complications; hence, the surgical risk of the procedure itself has a higher impact on possible transplant mortality although the overall risk of death is minimal. Nevertheless, on average 6.4 life-years per patient were saved through a PTA transplant. Notably, transplant recipients with type 1 diabetes have a higher gain in life-years than recipients with type 2 diabetes; young transplant recipients (<30 years) have a lower gain than older recipients due to a significantly higher graft loss rate for immunological reasons.
Lastly, a combined 273,843 life-years saved over a 21-year time period resulted in approximately 13,000 life-years saved per year or adding another 7 years (on average) annually to almost 2000 diabetic pancreas and/or kidney recipients. The average number of life-years saved per patient (11.7 for SPK, 6.4 for PTA, 6.3 for PAK, and 6.6 for KTA recipients) contributes substantially to the fact that pancreas and/or kidney transplantation clearly prolongs and saves the lives of diabetic patients.
References
Port FK, et al. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA. 1993;270(11):1339–43.
Merion RM, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005;294(21):2726–33.
Ojo AO, et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J Am Soc Nephrol. 2001;12(3):589–97.
Merion RM, et al. The survival benefit of liver transplantation. Am J Transplant. 2005;5(2):307–13.
Schnitzler MA, et al. The life-years saved by a deceased organ donor. Am J Transplant. 2005;5(9):2289–96.
Rana A, et al. Survival benefit of solid-organ transplant in the United States. JAMA Surg. 2015;150(3):252–9.
Meier-Kriesche HU, et al. Survival improvement among patients with end-stage renal disease: trends over time for transplant recipients and wait-listed patients. J Am Soc Nephrol. 2001;12(6):1293–6.
Terasaki PI, et al. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995;333(6):333–6.
Ojo AO, et al. The impact of simultaneous pancreas-kidney transplantation on long-term patient survival. Transplantation. 2001;71(1):82–90.
White SA, Shaw JA, Sutherland DE. Pancreas transplantation. Lancet. 2009;373(9677):1808–17.
Rayhill SC, et al. Simultaneous pancreas-kidney transplantation and living related donor renal transplantation in patients with diabetes: is there a difference in survival? Ann Surg. 2000;231(3):417–23.
Smets YF, et al. Effect of simultaneous pancreas-kidney transplantation on mortality of patients with type-1 diabetes mellitus and end-stage renal failure. Lancet. 1999;353(9168):1915–9.
Esmeijer K, et al. Superior long-term survival for simultaneous pancreas-kidney transplantation as renal replacement therapy: 30-year follow-up of a Nationwide cohort. Diabetes Care. 2020;43(2):321–8.
Venstrom JM, et al. Survival after pancreas transplantation in patients with diabetes and preserved kidney function. JAMA. 2003;290(21):2817–23.
Gruessner RW, Sutherland DE, Gruessner AC. Mortality assessment for pancreas transplants. Am J Transplant. 2004;4(12):2018–26.
van Dellen D, et al. Mortality in diabetes: pancreas transplantation is associated with significant survival benefit. Nephrol Dial Transplant. 2013;28(5):1315–22.
Gruessner S, et al. Employment pattern after pancreas transplantation - facts and risk factors - a registry analysis. Rev Diabet Stud. 2017; 14(1).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gruessner, R.W.G., Gruessner, A.C. (2023). Survival Benefit of Pancreas Transplantation. In: Gruessner, R.W.G., Gruessner, A.C. (eds) Transplantation of the Pancreas. Springer, Cham. https://doi.org/10.1007/978-3-031-20999-4_67
Download citation
DOI: https://doi.org/10.1007/978-3-031-20999-4_67
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20998-7
Online ISBN: 978-3-031-20999-4
eBook Packages: MedicineMedicine (R0)