Abstract
A 24-year-old male, presented with epilepsy, was treated with upfront (primary); Linac-based stereotactic radiosurgery (SRS) for left, frontal, parenchymal AVM. The target volume of 3.1 cc received a marginal dose of 25.6 Gy normalized to 80% isodose line. Serial post-SRS follow-up MRIs showed progressive reduction in the size of AVM nidus, coupled with perinidal high signal in T2 and FLAIR studies, denoting vasogenic edema. At 24 months post-SRS, MRI showed non-visualized AVM nidus and appearance of small focal ring-enhancing lesion at the site of prior AVM nidus, in T1 Gadolinium-enhanced study, denoting radiation necrosis. At 30 months post-SRS, conventional cerebral angiography documented complete obliteration of the AVM nidus. At 57 months post-SRS, MRI showed a large cystic lesion with a slightly enhancing rim at the site of prior AVM nidus, in T1 Gadolinium-enhanced study, denoting radiation-induced parenchymal changes with cyst formation. At last follow-up (81 months post-SRS), MRI showed regression in the size of the radiation-induced cyst and persistent surrounding vasogenic edema. Successful, uncomplicated SRS treatment was paralleled with control of seizures without anticonvulsant medications at the patient’s last clinical follow-up 96 months post-SRS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Arteriovenous malformation
- Cerebral AVM
- Parenchymal AVM
- Seizures
- Stereotactic radiosurgery
- Linear accelerator
- Linac-based radiosurgery
- Primary SRS
- Cerebral angiography
- Nidus obliteration
- Radiation necrosis
- Radiosurgery cyst formation
-
Demographics: Male; 24 years
-
Initial Presentation: Epilepsy for 7 months before radiosurgery treatment
-
Diagnosis: Cerebral parenchymal AVM
-
Pre-radiosurgery Treatment: None
-
Pre-radiosurgery Presentation: Epilepsy (generalized tonic-clonic seizures)
-
Radiosurgery Treatment:
Upfront (primary); Linac-based SRS for left, frontal, parenchymal AVM
-
Radiosurgery Dosimetry:
-
Target volume: 3.1 cc
-
Marginal dose: 25.6 Gy
-
Marginal isodose: 80%
-
Maximum dose: 33.0 Gy
-
Minimum dose: 24.6 Gy
-
Average dose: 31.7 Gy
-
Number of isocenters: 1
-
-
Follow-Up Period: 96 months post-SRS
-
Clinical Outcome:
-
6 months post-SRS: Persistent seizures with medications
-
24 months post-SRS: Infrequent seizures with medications
-
36 months post-SRS: Controlled seizures with medications
-
96 months post-SRS: Sustainable control of seizures with medications
-
-
Complications: None
-
Radiological Outcome:
-
6 months post-SRS (MRI): Slight decrease in size of AVM nidus
-
12 months post-SRS (MRI):
-
Marked decrease in size of AVM nidus
-
Appearance of perinidal high signal in T2 and FLAIR studies, denoting vasogenic edema
-
-
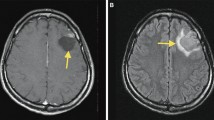
24 months post-SRS (MRI):
-
Non-visualized AVM nidus
-
Appearance of small focal ring enhancing lesion at the site of prior AVM nidus, in T1 Gadolinium-enhanced study, denoting radiation necrosis
-
Increased high signal, in T2 and FLAIR studies, surrounding the ring enhancing lesion at the site of prior AVM nidus
-
-
30 months post-SRS (conventional angiography): Complete obliteration of AVM nidus
-
57 months post-SRS (MRI):
-
Appearance of large cystic lesion with slightly enhancing rim at the site of prior AVM nidus, in T1 Gadolinium-enhanced study, denoting radiation-induced parenchymal changes with cyst formation
-
Markedly increased high signal in T2 and FLAIR studies around the radiation-induced large cyst
-
-
81 months post-SRS (MRI):
-
Regression in size of the heterogeneously enhancing cystic lesion at the site of prior AVM nidus, in T1 Gadolinium-enhanced study
-
Persistent increased high signal in T2 and FLAIR studies around the residual small enhancing radiation-induced cyst
-
-
-
Post-radiosurgery Treatment: Continued anti-convulsant medications











Further Reading
Abdelaziz OS. Stereotactic radiosurgery for angiographically visible, intracranial, parenchymal arteriovenous malformations: a review. Neurosurg Q. 2000;10(1):42–52. https://www.researchgate.net/publication/286618593.
Al Hinai Q, Tampieri D, Souhami L, et al. Cyst formation following radiosurgery for AVMs: report of 3 cases. Can J Neurol Sci. 2011;38:734–40.
Daou BJ, Palmateer G, Wilkinson DA, et al. Radiation-induced imaging changes and cerebral edema following stereotactic radiosurgery for brain AVMs. Am J Neuroradiol. 2021;42:82. https://doi.org/10.3174/ajnr.A6880.
Ding D, Stark RM, Kano H, et al. Radiosurgery for cerebral arteriovenous malformations in a randomized trial of unruptured brain arteriovenous malformations (ARUBA)-eligible patients: a Multicenter study. Stroke. 2016;47:342–9.
Schäuble B, Cascino GD, Pollock BE, et al. Seizure outcomes after stereotactic radiosurgery for cerebral arteriovenous malformations. Neurology. 2004;63(4):683–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Abdelaziz, O.S., De Salles, A.A.F. (2023). Cerebral Parenchymal Arteriovenous Malformation (AVM). In: NeuroRadiosurgery: Case Review Atlas. Springer, Cham. https://doi.org/10.1007/978-3-031-16199-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-16199-5_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-16198-8
Online ISBN: 978-3-031-16199-5
eBook Packages: MedicineMedicine (R0)