Abstract
Hearing loss is the most frequent symptom caused by vestibular schwannomas [1]. Aside from the rare tumor that presents itself for a hearing-preservation surgery, the majority of tumors will likely result in deafness of the affected ear regardless of the intervention modality. The natural history of hearing in observed tumors also predicts eventual decline [2]. Hearing loss attributed to vestibular schwannomas remains the primary driver for poor quality of life in this patient population [3, 4].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Hearing loss is the most frequent symptom caused by vestibular schwannomas [1]. Aside from the rare tumor that presents itself for a hearing-preservation surgery, the majority of tumors will likely result in deafness of the affected ear regardless of the intervention modality. The natural history of hearing in observed tumors also predicts eventual decline [2]. Hearing loss attributed to vestibular schwannomas remains a primary driver for poor quality of life in this patient population [3, 4].
The auditory system is designed for hearing from two ears (binaural hearing). When bilateral input is lost, patients suffer from poor sound localization and speech discrimination in noise. The following text will review the audiologic disadvantages of single-sided deafness and the evolution of hearing rehabilitation following vestibular schwannoma surgery.
Unilateral Hearing Loss
The auditory system is designed for binaural input. When one ear suffers from hearing loss, it manifests as difficulty with sound localization and speech recognition, particularly in the presence of background noise. The clinical impact of unilateral hearing loss is dependent on the patient’s daily listening environment. For instance, children in a noisy classroom often have a background signal-to-noise ratio (SNR) of 2–9 dB. Children with severe-to-profound unilateral hearing loss in that environment have a 22–35% of chance of repeating a grade and a 12–41% chance of requiring additional educational support [5,6,7]. Unilateral hearing loss in children is an independent risk factor for poor language comprehension and oral expression scores [8]. Adults with unilateral hearing loss are also subject to the negative psychological and social consequences of this handicap. Recurring adult themes include anxiety about potential hearing loss in the contralateral ear, strong negative emotions including embarrassment and frustration, and negative coping strategies such as withdrawal from social engagements [9]. In a survey of 51 patients who had undergone cerebellopontine angle surgery, the postoperative decreased quality of life strongly correlated with their unilateral profound hearing loss [10].
The audiologic benefits of binaural hearing are based on the principles of binaural summation, binaural squelch, and the head shadow effect. Together these phenomena allow the brain to detect subtle interaural time and intensity differences that facilitate sound localization and improved hearing in noise. Binaural summation occurs when sound is captured from each ear independently and integrated along the auditory pathway. This integration process results in an internal amplification of 4–6 dB [11].
Binaural squelch refers to a patient’s ability to listen only to the sound of interest when additional sound sources are present. For instance, honing in during a conversation amidst a loud background environment such as a cocktail party, thus named the cocktail party effect. Binaural squelch also occurs as sound is transmitted along the subcortical and cortical auditory pathways. The threshold benefit of binaural squelch is modest, with only a 1–2 dB increase, but the ability to understand speech at a lower SNR (i.e., loud environment) is significant [12, 13].
Sound travels as an energy wave through space. In the binaural condition, the energy waves arrive at each ear with a slightly different time and intensity. The interaural time difference (ITD) and interaural level difference (ILD) are critical for sound localization. High-frequency sounds, which have wavelengths that are shorter than the circumference of the skull, are subject to further modification secondary to head interference. The interference accentuates the ILD and creates a head shadow effect. For high frequencies, the head shadow effect can result in a 15–20 dB ILD, while lower frequencies have only a 5 dB ILD. Together, binaural summation, binaural squelch, and the head shadow effect enable patients to localize sound and improve speech comprehension in noise. Without binaural input these elements are lost, thus creating the difficulties seen among patients who suffer from unilateral hearing loss.
Hearing Rehabilitation
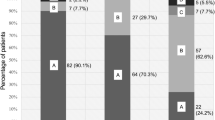
Hearing rehabilitation options are dependent on the status of a patient’s external ear, cochlea, and cochlear nerve. Some tumors may present with characteristics favorable for a hearing preservation surgical approach. These factors include tumors that originate from the superior vestibular nerve, the presence of cerebrospinal fluid between the lateral tumor edge and the cochlea (i.e., fundal cap), and small tumor size [14,15,16]. In patients with hearing preserved after surgery, amplification of the operative ear depends solely on the amount of residual hearing that remains after the procedure. The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) and the Gardner-Robertson (GR) hearing classification systems both designate serviceable hearing as greater than 50% on speech discrimination testing and less than 50 dB pure tone average (Table 12.1) [17, 18]. Good hearing (AAO-HNS Class A) may not require additional amplification, while compromised but preserved hearing (AAO-HNS Classes B and C) will likely benefit from a traditional hearing aid. Patients with a speech discrimination less than 50% (AAO-HNS Class D) have a less predictable response to amplification in the affected ear. Some patients may be bothered by poor clarity from the amplification, while others may appreciate improved sound localization from the bilateral input. If some degree of hearing persists, then at least a hearing aid trial should be considered before moving to the single-sided deafness rehabilitation options.
In traditional cerebellopontine angle surgery where hearing is not preserved, the external ear and cochlea remain intact but the cochlear nerve is damaged secondary to the tumor or tumor resection. This creates a unilateral, profound sensorineural hearing loss with no ability to rehabilitate using a traditional hearing aid or cochlear implant (CI). Therefore, the mainstays of auditory rehabilitation in this patient population have focused on bringing sound from the deafened ear over to the healthy ear.
Contralateral Routing of Signal
The concept of bringing noise from a deafened ear to the better ear via modified hearing aids connected with a “sound tube” was first suggested in 1960 [19]. In 1964, Harry Teder, while working at Telex, created a patent that coined the term contralateral routing of sound (CROS), and by 1965 Harford and Barry introduced the first CROS hearing aid [20]. This device consisted of a microphone attached to eyeglasses on the hearing impaired side. The microphone detected sound from the deafened side and transmitted it via a wire that ran across the eyeglass frame into a hearing aid placed in the better hearing ear. The classic CROS scenario implies normal hearing in the contralateral ear. Harford and Barry also developed a Bi-CROS system in which sound presented on the side of the better hearing ear could also be amplified if that ear had hearing loss. This basic construct of a microphone on the deafened ear connected via a wire to a hearing aid on the better hearing ear, with or without the eyeglasses, remained in place until 2004. While this version of the CROS was a useful option for patients with monaural hearing, the wire attachment was bulky, and patients disliked the blocked feeling, termed occlusal effect, of having a hearing aid placed in the ear canal of a normal hearing ear [21].
In 2004, Siemens developed the first wireless CROS device, called the e2e Wireless®, which has since become the industry standard and has improved patient satisfaction [22]. Directional microphones and improved processing strategies have also improved performance [23]. However, the wireless adaptation does not eliminate the occlusal effect or the perceived cosmetic aspect of wearing bilateral hearing devices. Additionally, insurance coverage in the United States for hearing aids, including the CROS system, is sporadic, and the out-of-pocket expense can be a barrier to access. Still, the noninvasive nature of the device makes it a logical first step for patients entertaining the idea of hearing rehabilitation following lateral skull base surgery.
The first goal of a CROS device is to enhance the SNR, thus improving speech clarity in background noise. The SNR is particularly problematic when the primary speech signal and background noise are spatially separated. If the speaker is talking into the deafened ear with a CROS device in place, the device has the potential to increase clarity of the spoken word by creating an artificial head shadow effect and lowering the speech reception threshold of the spoken word [24, 25]. Conversely, if the ambient noise is presented to the deafened side with a CROS device, there is potential for degradation of speech intelligibility secondary to enhancement of the background noise [25,26,27].
The second goal of a CROS device is to provide sound awareness on the deafened side. Because CROS aids do not restore the ITD, ILD, and natural head shadow effect, they will not enable the precise localization that is seen with binaural hearing. However, CROS users should have an improved ability to tell from which side of the body sound originates. In a sample of 21 patients with unilateral hearing loss, only 10% could correctly identify which side of their body a sound originated from prior to using a CROS aid. After 4 weeks of use, that sound awareness improved to over 40% [25]. Older CROS aids focused on transmission of high-frequency sound (above 1000 Hz) that is associated with the head shadow effect. Modern CROS processors can transmit the full bandwidth of sound, and this has potential for further improvement in sound awareness on the deafened side but still lacks the ability to precisely localize a noise [27].
Osseointegrated Hearing Implants
The skull’s density enables an alternative method for stimulation of the contralateral ear. Bone conduction has an interaural attenuation of 5 dB or less. Therefore, rather than transmitting sound via air like a traditional hearing aid, osseoconductive devices vibrate the skull, which carries the sound through the densely packed bone and into the inner ear. Osseoconductive hearing devices were proposed as early as Roman antiquity. In the eighteenth and nineteenth centuries, crude devices made of wood, metal, or glass were constructed but ultimately failed due to poor sound attenuation through the scalp or discomfort when they were applied to teeth [28].
Pioneering work from Brånemark in Sweden around 1965 revolutionized bone anchored devices. Working with titanium dental implants, his group discovered that osteocytes in direct contact with titanium adhere via a process called osseointegration. This discovery led to titanium’s wide utilization in dental and craniofacial reconstructions [29, 30]. Then in 1977, Brånemark’s partner, Anders Tjellström, recognized the potential for osseointegrated titanium to conduct sound, paving the way for modern osseoconductive device systems. Tjellström was the first to place a percutaneous abutment attached to a titanium implant in the mastoid bone [31]. A modified hearing aid that vibrates rather than produces sound waves in the air could then be attached to the abutment and propagate sound energy via the skull and into a healthy cochlea. Tjellström’s initial patients all had chronic ear disease that prohibited traditional hearing aid placement. After 5 years, the benefit persisted and patient satisfaction remained high, which led to an entire field of osseointegrated hearing devices [32]. The bone anchored hearing aid (BAHA®) device became commercially available in 1987, and it was approved for conductive hearing loss by the U.S. Food and Drug Administration (FDA) in 1996. The initial American experience in forty patients with chronic ear disease mirrored the positive results reported by Tjellström [33]. As of 2010, more than 80,000 osseointegrated devices have been implanted worldwide. In 2002, the FDA approved the BAHA for the indication of single-sided deafness (SSD), and since then Ponto® has also become commercially available.
Osseointegrated devices do require surgical implantation. The surgical steps have evolved considerably. The titanium implant is placed into the mastoid bone approximately 5.5 cm behind the external auditory canal. Initially, the titanium implant was placed at a separate stage to facilitate osseointegration without any load-bearing forces. This technique is still sometimes used in young children or temporal bones that have received radiation, but in general both the titanium implant and its percutaneous abutment can be implanted in a single procedure [34]. The soft-tissue work has also evolved. Initially, no soft tissue reduction was performed, but some patients experienced adverse skin reactions. In an effort to reduce skin reaction, surgeons began thinning the subcutaneous tissue around the abutment. The original soft tissue reduction technique described by the Nijmegen group called for a linear incision, wide soft tissue reduction, and then the implant placed in the middle of the incision [35, 36]. Additional modifications, such as a semicircular skin incision with the implant punched through the base of the pedicle (U-graft technique) or use of a dermatome, were also suggested [37]. Recently, a minimally invasive Ponto surgery (MIPS) technique has been described that forgoes any skin incision and allows placement of the implant through a 5-mm hole created with a skin punch [38]. In general, the surgical techniques have trended toward a single-stage procedure with less need for soft reduction and more emphasis placed on proper skin handling with minimal cauterization. The osseointegration process takes time, and initial protocols suggested waiting 3 months to ensure proper healing before activation with the vibrating hearing aid. Evidence suggests that earlier activation is safe, with most centers loading the implant 6–8 weeks after implantation. Some data also suggest earlier loading may be feasible [39].
Major surgical complications following implantation of an osseointegrated device are rare. Potential injury to the dura or a dural venous sinus is mitigated by drilling the osseous well in a stepwise fashion and confirming that healthy bone is present at the depth of the well prior to implant placement. Two cases of intracerebral abscess following implantation have been reported [40, 41]. Failure of osseointegration is a relatively rare event and can be precipitated by trauma, infection, prior radiation, or improper technique that results in osteocyte death secondary to overheating. The rate of implant extrusion is 3–4% [42,43,44].
Soft tissue adverse events are unfortunately more common with most reports suggesting a rate between 8.7% and 13%, but some studies suggest the rate is 30% or higher [42, 44]. The skin reactions can be classified according to the Holgers grading system (Table 12.2) [45]. The majority of skin reactions are mild (Holgers grade 1 or 2) and can be treated with topical steroids or topical antibiotics. The presence of granulation tissue (Holgers grade 3) can be addressed with silver nitrate cauterization or the addition of oral antibiotics. More serious infections (Holgers grade 4) may require removal of the abutment or resection of overgrown skin. The rate of revision surgery is from 7% to 12% and is typically due to skin overgrowth (Fig. 12.1) [42, 44].
Percutaneous osseointegrated device examples. All cases depict a right ear. (a) Healthy appearance of a percutaneous abutment (Holger Grade 0). (b) Erythema and moisture around the abutment indicative of a soft tissue infection (Holger Grade 2). (c) Robust granulation tissue around the abutment (Holger Grade 3). (d) Wound breakdown and granulation tissue following application of silver nitrate (Holger Grade 3)
In an effort to limit the adverse events associated with a percutaneous implant, two modifications have been introduced. The first variation is a transcutaneous magnet that employs the same titanium implant placed during a traditional osseointegrated implant; but rather than attaching a percutaneous abutment, there is a subcutaneous magnet attached to the implant. The magnet is then coupled to a device that rests on the skin. The device vibrates, and that vibration is transmitted to the subcutaneous magnet and then to the titanium implant. This type of transcutaneous model has the benefit of no abutment protruding through the skin. Despite this, the large magnets needed to couple with the external vibrating bone conduction hearing aid can still produce skin related complications [46]. Furthermore, the sound energy has to pass through the soft tissue of the scalp (i.e., transcutaneous), which causes approximately 10 dB of sound attenuation.
The second variation is a direct-drive bone conduction system. As of 2020, there are two FDA-approved direct-drive bone conduction systems, specifically MED-EL’s Bonebridge® and Cochlear Corporation’s Osia®. Their utility in unilateral hearing loss is still being studied but should mirror the previously described pros/cons [47]. There are some differences in how these devices function. For instance, the Bonebridge® involves drilling a well in the mastoid cavity to house a floating-mass transducer (FMT). The FMT attaches to the cortical mastoid bone via two titanium screws. An external processor with two microphones connects to the internal receiver via a magnet. Sound received by the external processor is sent to the internal receiver, which drives the FMT to vibrate skull [48]. This design has the advantage of requiring a smaller magnet, and it eliminates soft tissue attenuation. The surgical steps are slightly more complex secondary to the larger space needed to hold the FMT, and its utilization following lateral skull base surgery has not been widely reported. Rather than using a FMT, the Cochlear Corporation’s Osia® implant uses a titanium screw identical to the implant used with their BAHA® system. Attached to a titanium screw is a piezoelectric driver that rests under the skin and drives the bone conduction. Both the direct-drive bone conduction system and the transcutaneous magnet system should be used with caution if future magnetic resonance imaging (MRI) is necessary to monitor cerebellopontine angle or intracranial pathology. Both devices have a large metallic artifact secondary to the size of the FMT and internal magnet [49].
Other nonsurgical forms of osseoconductive hearing aids exist but have shown varied commercial success. Bone conduction hearing aids, attached with a headband or a soft elastic band, are available. One more innovative device is the SoundBite®. This system had a behind-the-ear microphone that sent a wireless signal to a transducer that was attached to a molar as a dental appliance. The transducer vibrated the tooth to take advantage of the tooth’s inherent osseointegration. Despite early studies showing high patient satisfaction and a global hearing benefit, the start-up company that developed the product filed for bankruptcy in 2015 [50]. Another nonsurgical alternative osseoconductive hearing aid is the TransEar®. This system also has a behind-the-ear microphone, but it is attached via a wire to a custom-fit ear mold that houses an oscillator. The oscillator vibrates the osseous external auditory canal, sending a transcranial signal to the better hearing ear. The TransEar also has had limited commercial success due to patient discomfort from the oscillator and poor hearing results [51].
The potential benefits of an osseointegrated device for unilateral hearing loss following vestibular schwannoma surgery are the same as the CROS hearing aid, specifically improved hearing in noise and sound awareness on the deafened side. Like CROS hearing aids, osseointegrated devices will not restore sound localization because it does not create binaural hearing. An additional benefit of osseointegrated devices compared to CROS is the lack of occlusal effect on the better hearing ear as well as the lack of needing to wear bilateral hearing aids. These benefits must be weighed against the need for a surgery and the possible skin-related complications [24].
The modest hearing benefits of osseointegrated devices for unilateral hearing loss have been documented both subjectively and objectively. In a survey of 139 patients following translabyrinthine resection of a vestibular schwannoma, patients that chose to be implanted with an osseointegrated device had a 17.4% improvement on the Background Noise subscale of the Abbreviated Profile of Hearing Aid Benefit (APHAB) questionnaire. Additionally, they reported an 11.6% improvement on the Ease of Communication subscale and a 13.2% improvement on the Reverberation subscale [52]. A systematic review analyzing 14 studies with 296 unilateral hearing loss patients demonstrated overall improvement with speech discrimination in noise and improved quality of life [53].
When choosing between osseointegrated device and CROS, individual interpretation of the previously discussed advantages and disadvantages must be considered. Trials of the CROS device and a bone conduction hearing aid are recommended so that patients can make an informed decision with appropriate expectations [54]. New techniques of simulating the bone conduction system with real ear measures have the potential to improve fitting parameters and patient satisfaction [55,56,57].
From an audiologic standpoint, many studies have tried to compare the results of osseointegrated devices and CROS. However, these studies are underpowered, lack randomization, and introduce selection bias as all osseointegrated device patients chose to undergo surgical intervention to address their hearing loss. In 2006, Baguley and colleagues performed a meta-analysis on four prospective studies with 47 patients comparing CROS versus BAHA [58,59,60,61]. In this analysis, the BAHA significantly outperformed CROS on all APHAB subscales (Ease of Communication, Reverberation, Background Noise, and Aversiveness of Sounds) [62]. Studies that are more recent have failed to replicate the superiority of osseointegrated devices, citing similar audiometric advantages with both systems [63,64,65]. In general, when patients are presented with all options following vestibular schwannoma surgery, only 30–50% will ultimately choose to be implanted with an osseointegrated device [52, 54, 63].
The limitations of either an osseointegrated device or a CROS are its inability to restore the ITD and ILD, which results in poor sound localization and limited ability to improve hearing in noise. Individuals with a unilateral hearing loss will function best if they can control their environment to limit the SNR or place the important sound source close to their better hearing ear. An osseointegrated device or a CROS may even be detrimental if it amplifies unfavorable background noise rather than the speaker of interest. In those listening environments, the patient may benefit from temporary removal of the device to prevent a masking phenomenon of the better hearing ear.
Auditory Brainstem Implants
A small subset of patients will present with bilateral profound sensorineural hearing loss accompanied by damaged cochleae or cochlear nerves that prohibit hearing rehabilitation with CROS, BAHA, or cochlear implantation. This clinical scenario most commonly occurs in the setting of neurofibromatosis type 2 (NF2) but may also be applicable for sporadic vestibular schwannomas in an only hearing ear. The auditory brainstem implant (ABI) was developed as a means of bypassing the cochlea and cochlear nerve to directly stimulate the auditory pathway at the cochlear nucleus.
The first ABI was placed by Drs. William House and William Hitselberger in 1979 for a patient with NF2 who lost all hearing following vestibular schwannoma removal in her only hearing ear [66]. Twenty years after placement, this rudimentary paired ball electrode device continued to provide the patient with improved lip-reading ability and environmental sound detection. Since this first case, more than 1000 ABIs have been implanted worldwide, and many device modifications have attempted to improve cochlear nucleus stimulation.
In 2000, Cochlear Corporation first received FDA approval to implant patients 12 years and older with NF2 using the Nucleus 24 ABI® device. (MED-EL also makes an ABI device, but it is not FDA-approved.) Both manufacturers have adapted their CI software platforms for the electrical stimulation required for their ABI products. The latest version of Cochlear Corporation’s ABI is the Nucleus ABI54®. This device that includes an external component consisting of a behind-the-ear microphone, speech processor, and transmitter coil sends a digital signal to a receiver-stimulator implanted beneath the scalp. The signal is then transmitted to the ABI electrode paddle, which has 21 individual platinum disks that contact the cochlear nucleus. The paddle is covered by a polyethylene terephthalate (PET) mesh that promotes fibrous ingrowth and long-term device fixation along the dorsolateral brainstem (Fig. 12.2) [67].
Cochlear Corporation’s auditory brainstem implant system. (a) The behind-the-ear component contains two microphones and a speech processor attached to an external transmitter coil. (b) The internal receiver-stimulator gets the signal from the external transmitter coil and sends it down the electrode array. (c) The electrode array ends in a paddle containing 21 platinum disk contacts. The back side of the paddle is coated with a PET mesh to prevent future movement
Placement of the ABI targets the cochlear nucleus complex, which lies at the dorsal pontomedullary junction located along the lateral recess at the floor of the fourth ventricle. The cochlear nucleus is not visible on the surface of the brainstem, so its location must be approximated by nearby landmarks. Access to this area is usually achieved during vestibular schwannoma resection, classically through a translabyrinthine approach. The vestibulocochlear nerve, glossopharyngeal nerve, and choroid plexus serve as important landmarks for ABI placement. In large tumors, the brainstem anatomy and vestibulocochlear nerve may be distorted. By tracing the glossopharyngeal nerve superiorly to the choroid plexus, the lateral aperture of the lateral recess (foramen of Luschka) is identified. With gentle posterior and superior retraction of the choroid plexus, the lateral recess can be opened to allow placement of the ABI paddle in proximity of the cochlear nucleus (Fig. 12.3) [68]. During this dissection, it is important to be aware of cardiac and cranial nerve monitoring (VII, VIII, IX, X, XI) because surgical dissection or stimulation can result in bradycardia or hemodynamic instability.
Intraoperative photos of a right-sided auditory brainstem implant (ABI). The fourth ventricle connects to the cerebellopontine cistern via the lateral recess. The lateral aperture of the lateral recess is termed the foramen of Luschka (FL). (a) The choroid plexus (ChP) is a key landmark for identification of the lateral recess. (b) With the choroid plexus retracted, the opening of the FL becomes apparent. (c) The ABI is placed into the lateral recess so that its platinum contacts face the dorsolateral surface of the pontomedullary junction. The vestibulocochlear nerve (VIII) and facial nerve (VII) are labeled
The ABI is placed on the surface of the cochlear nucleus complex, which is a structure with several distinct subunits that carry different auditory processing functions. The main subunits are the dorsal and ventral cochlear nuclei. In brief, the ventral cochlear nucleus serves as the primary relay center for afferent auditory input and maintains the tonotopic organization started in the cochlea—this is the primary ABI target. The dorsal cochlear nucleus receives afferent input but also efferent input that facilitates complex auditory processing. In an attempt to better access the different cochlear nucleus subunits, a penetrating auditory brainstem implant (PABI) was designed. This design had penetrating microelectrodes emanating from the traditional ABI surface paddle. Ultimately, the PABI design failed to improve cochlear nucleus stimulation. Results showed no improvement in speech perception, with less than 25% of the penetrating electrodes producing auditory sensation compared with 60% of the surface electrodes [69].
Like the PABI, the auditory midbrain implant (AMI) was another experimental device hoping to overcome some of the challenges associated with cochlear nucleus stimulation. The target for the AMI is further rostral along the auditory pathway at the inferior colliculus. The implant is a penetrating electrode array placed in the midbrain. The device continues to undergo modifications, but to date it remains an experimental option for NF2 patients [70].
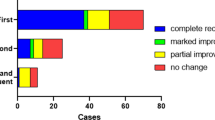
With more than 1000 patients implanted with ABIs, primarily for hearing loss due to NF2, the expected auditory outcomes include environmental sound awareness and assistance with lip-reading. Only a small subset of patients will obtain open-set word understanding. Some factors responsible for the outcome variability include tumor growth that distorts the brainstem anatomy, ABI electrode positioning, imprecise cochlear nucleus stimulation, and surgical trauma [71]. A 2014 consensus statement evaluated 84 NF2 patients with ABIs to identify several factors associated with improved outcomes. Overall, 26 of 84 (31%) patients achieved open-set sentence scores greater than 30%. The surgical factors thought to portend a good outcome included the use of a semi-sitting surgical position and early cutting of the vestibulocochlear nerve near the brainstem to minimize transfer of electrocautery excitotoxicity to the cochlear nucleus during tumor dissection. In addition, patient factors like duration of preoperative deafness correlated with performance. Among excellent performers, the ability to identify eleven distinct pitches predicted a greater than 80% open-set speech recognition without background noise [72]. Another cohort of 23 NF2 patients with ABI showed that 19 (83%) continued to use their device after implantation while 8 of 23 (35%) patients achieved speech perception and only 4 (17%) patients could use the telephone [71].
In general, ABI placement does not increase the risk of complications during vestibular schwannoma surgery. Potential complications include cerebrospinal fluid (CSF) leak, meningitis, cranial neuropathy, hydrocephalus, stroke, and even death while device-specific complications include device failure, extrusion, migration, and nonauditory stimulation. In a review of 61 patients undergoing ABI, Otto and colleagues identified two patients with CSF leaks (3.3%) and one with meningitis (1.6%). Electrode migration occurred in one (1.6%) patient and failure to produce useful auditory sensation occurred in six (9.8%) patients demonstrating the importance of accurate device position. No serious consequences of nonauditory stimulation occurred, but 24% of tested electrodes could not be used due to these stimuli. The deactivated electrodes generally were located at either the proximal or distal end of the electrode paddle; nonauditory sensations included tingling, altered vision, and dizziness [73]. The risk of CSF leak does require particular diligence during closure because the ABI can serve as a wick for CSF into the mastoid or soft tissue.
Given the low complication rate and preference to avoid additional surgery, many centers use the concept of a “sleeper” ABI when planning auditory rehabilitation for NF2 patients. These situations are unique in that patients have bilateral vestibular schwannomas and eventual bilateral deafness is expected. Therefore, an ABI can be placed during the first tumor removal despite still having useful hearing in the contralateral ear. Then, if hearing in the contralateral ear is lost or surgical intervention requires sacrifice of that cochlear nerve, the previously placed ABI can be activated. ABI placement at the time of large tumor removal or with brainstem compression can be technically difficult, so the “sleeper” approach also creates an extra opportunity for accurate ABI placement.
Cochlear Implantation
Surgical priorities for vestibular schwannoma microsurgery continue to evolve as the operative morbidity declines. Early surgical techniques focused on lowering the disconcertingly high mortality rate. The next iteration of advances reduced major perioperative morbidities such as facial nerve paralysis and CSF leaks. Finally, optimization of hearing preservation outcomes based on various patient and tumor factors yields fairly predictive surgical outcomes. Despite these innovations, hearing can be lost even when cochlear nerve integrity remains intact, presumably from vascular insult to the cochlea or trauma to the cochlear nerve.
In the early 1990s, studies by Cueva and colleagues, Kartush and colleagues, and Vrabec colleagues demonstrated that, after labyrinthectomy or vestibular schwannoma microsurgery, a preserved cochlear nerve could transmit an auditory signal despite complete loss of hearing [74,75,76]. These studies performed transtympanic promontory stimulation to identify positive auditory responses as well as distinct auditory pitch perception. Positive responses could be achieved at 9 months after initial surgery and were comparable to responses achieved by CI candidates. These findings were supported by temporal bone studies of patients after labyrinthectomy that revealed spiral ganglion cell survival years after surgery [77]. If spiral ganglion cells can survive and the cochlear nerve integrity is maintained, then the possibility of cochlear implantation exists.
As early as 1992, several case reports showed the feasibility of a staged cochlear implantation after labyrinthectomy or removal of a vestibular schwannoma, with an intact cochlear nerve [78,79,80,81,82]. These studies confirmed that the auditory pathway could transmit an electrical signal despite postoperative hearing loss and that cochlear ossification did not always occur, thus allowing CI placement. In 1995, Arriaga and colleagues reported the first cases of a simultaneous CI performed during translabyrinthine vestibular schwannoma removal. This patient’s tumor was in his only hearing ear [83]. Intraoperative promontory stimulation was not performed. At 10 months, the patient was still using the CI with enhanced lip-reading ability. Some authors advocate simultaneous CI and tumor removal in an effort to minimize delays in auditory rehabilitation, reduce the number of surgical procedures, and avoid potential cochlear obstruction if ossification occurs [84].
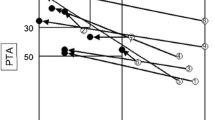
Recently, several case series have demonstrated that either staged or simultaneous cochlear implantation is safe and feasible for hearing rehabilitation as long as the cochlea is patent and the cochlear nerve is intact. Many patients can achieve improved sound awareness and open-set speech, but the results are more variable than traditional CI candidates [85,86,87]. A recent prospective study evaluated simultaneous cochlear implantation and translabyrinthine tumor resection for sporadic vestibular schwannomas. All seven patients had preservation of the cochlear nerve and five of seven (71%) had auditory precepts with CI activation. In regard to the five patients, at 1 month their sound localization improved from 78° ± 13°, with the CI off to 41° ± 9° with the CI on. This improvement in sound localization is a distinct benefit over the hearing rehabilitation with CROS or BAHA. Additionally, the five patients in this study also demonstrated modest improvement in speech understanding and tinnitus reduction [88].
If the cochlear nerve is preserved and a CI is placed, one potential concern is the sustainability of the benefits, particularly in patients with NF2 who are susceptible to distorted brainstem anatomy, tumor recurrence, or new tumor growth. Neff and colleagues reported on six patients with NF2 who had undergone tumor resection with CI placement and had long-term follow-up with a mean of 7.9 years (range: 5–13 years). In all but one patient, the benefit from CI was maintained, and five of six (83%) patients were still able to use a telephone with their CI devices [89]. Although continued long-term follow-up is needed, no case reports have been published in which a CI had to be removed due to tumor re-growth. Additionally, tumor surveillance by MRI is improved by newly expanded FDA guidelines, allowing 1.5–3 T strength MRI depending on the CI device manufacturer. CI magnets do produce artifact that may distort surveillance of the cerebellopontine angle. Placement of the internal receiver-stimulator in a more superior position and use of reformatted coronal and sagittal views can help mitigate this distortion. In a retrospective review of 34 ears undergoing a 1.5 T MRI scan with a CI in place secured by a firm head wrap, the authors found the ipsilateral cerebellopontine angle could be visualized without difficulty in 94% of cases. However, there was a 15% risk of magnet movement even with the use of a head wrap [90]. Clearly, caution must be used in device selection when considering postoperative tumor surveillance.
In conclusion, management of vestibular schwannomas has made great strides in patient safety and decreased morbidity. Still, the loss of hearing is an inevitable fate for many patients with a vestibular schwannoma and has a significant impact on patients’ quality of life. The most common hearing rehabilitation options, CROS and BAHA, can improve sound awareness and speech in noise but fail to restore the audiologic benefits of binaural hearing. If the cochlea is accessible and the cochlear nerve is intact, then CI has the potential to restore binaural function. If no cochlear nerves are viable, then an ABI can provide sound detection to improve lip-reading abilities and, in rare cases, even open-set speech.
References
Matthies C, Samii M. Management of 1000 vestibular schwannomas (acoustic neuromas): clinical presentation. Neurosurgery. 1993;40:1–10.
Stangerup SE, Thomsen J, Tos M, Cayé-Thomasen P. Long-term hearing preservation in vestibular schwannoma. Otol Neurotol. 2010;31:271–5.
Wiegand D, Fickel V. Acoustic neuroma, the patient’s perspective: subjective assessment of symptoms, diagnosis, therapy, and outcome in 541 patients. Laryngoscope. 1989;99:179–87.
Tos T, Cayé-Thomasen P, Stangerup S, et al. Patients’ fears, expectations and satisfactions in relation to management of vestibular schwannoma: a comparison of surgery and observation. Acta Otolaryngol. 2003;123:600–5.
Bess F, Tharpe A. Unilateral hearing impairment in children. Pediatrics. 1984;74:2016–216.
Keller W, Bundy R. Effects of unilateral hearing loss upon educational achievement. Child Care Health Dev. 1980;6:93–100.
Oyler R, Oyler A, Matkin N. Unilateral hearing loss: demographics and educational impact. Lang Speech Hear Serv Sch. 1988;19:201–10.
Lieu JEC, Tye-Murray N, Karzon RK, Piccirillo JF. Unilateral hearing loss is associated with worse speech-language scores in children. Pediatrics. 2010;125:e1348–55.
Lucas L, Katiri R, Kitterick PT. The psychological and social consequences of single-sided deafness in adulthood. Int J Audiol. 2018;57:21–30.
Subramaniam K, Eikelboom RH, Eager KM, Atlas MD. Unilateral profound hearing loss and the effect on quality of life after cerebellopontine angle surgery. Otolaryngol Head Neck Surg. 2005;133:339–46.
Mencher GT, Davis A. Bilateral or unilateral amplification: is there a difference? A brief tutorial. Int J Audiol. 2006;45:S3–11.
Snik A, Agterberg M, Bosman A. How to quantify binaural hearing in patients with unilateral hearing using hearing implants. Audiol Neurotol. 2015;20:44–7.
Killion M. SNR loss: “I can hear what people say, but I can’t understand them”. Hear Rev. 1997;4:8–14.
Shelton C, Brackmann DE, House WF, Hitselberger WE. Acoustic tumor surgery. Prognostic factors in hearing conservation. Arch Otolaryngol Head Neck Surg. 1989;115:1213–6.
Dubrulle F, Ernst O, Vincent C, Vaneecloo F, Lejeune J, Lemaitre L. Cochlear fossa enhancement at MR evaluation of vestibular schwannoma: correlation with success at hearing-preservation surgery. Radiology. 2000;215:458–62.
Kutz JW, Scoresby T, Isaacson B, et al. Hearing preservation using the middle fossa approach for the treatment of vestibular schwannoma. Neurosurgery. 2012;70:334–40.
Committee on hearing and equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma): American Academy of Otolaryngology—Head and Neck Surgery Foundation, INC. Otolaryngol Head Neck Surg. 1995;113:179–80.
Gardner G, Roberston J. Hearing preservation in unilateral acoustic neuroma surgery. Ann Otol Rhinol Laryngol. 1988;97:55–66.
Fowler E. Bilateral hearing aids for monaural total deafness. Arch Otolaryngol. 1960;72:41–2.
Harford E, Barry J. A rehabilitative approach to the problem of unilateral hearing impairment; the contralateral routing of signals (CROS). J Speech Hear Dis. 1965;30:121–38.
Aufricht H. A follow-up study of the CROS hearing aid. J Speech Hear Dis. 1972;37:113–7.
Herbig R, Barthel R, Branda E. A history of e2e wireless technology. Hear Rev. 2014;21:34–7.
Valente M, Oeding K. Evaluation of a BICROS System with a directional microphone in the receiver and transmitter. J Am Acad Audiol. 2015;26:856–71.
Bishop CE, Eby TL. The current status of audiologic rehabilitation for profound unilateral sensorineural hearing loss. Laryngoscope. 2010;120:552–6.
Ryu NG, Moon IJ, Byun H, et al. Clinical effectiveness of wireless CROS (contralateral routing of offside signals) hearing aids. Eur Arch Oto-Rhino-Laryngol. 2015;272:2213–9.
Lotterman S, Kasten R. Examination of the CROS type hearing aid. J Speech Hear Res. 1971;14:416–20.
Lin LM, Bowditch S, Anderson MJ, May B, Cox KM, Niparko JK. Amplification in the rehabilitation of unilateral deafness: speech in noise and directional hearing effects with bone-anchored hearing and contralateral routing of signal amplification. Otol Neurotol. 2006;27:172–82.
Mudry A, Tjellström A. Historical background of bone conduction hearing devices and bone conduction hearing aids. Adv Otorhinolaryngol. 2011;71:1–9.
Brånemark P, Adell R, Breine U, Hansson B, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. Experimental studies. Scand J Plast Reconstr Surg. 1969;3:81–100.
Albrektsson T, Brånemark P, Hansson H, Lindström J. Osseointegrated titanium implants. Requirements for ensuring long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70.
Tjellström A, Lindström J, Hallen O, Albrektsson T, Brånemark P. Osseointegrated titanium implant in the temporal bone. A clinical study on bone-anchored hearing aids. Am J Otol. 1981;2:304–10.
Tjellström A, Rosenhall J, Lindström O, Hallen T, Albrektsson T, Brånemark P. Five-year experience with skin-penetrating bone-anchored implants in the temporal bone. Acta Otolaryngol. 1983;95:568–75.
Lustig LR, Arts H, Brackmann DE, et al. Hearing rehabilitation using the BAHA bone-anchored hearing aid: results in 40 patients. Otol Neurotol. 2001;22:328–34.
Tjellström A, Granstrom G. One stage procedure to establish osseointegration. A zero to five years follow-up report. J Laryngol Otol. 1995;109:593–8.
Myalnus E, Cremers C. A one-stage surgical procedure for placement of percutaneous implants for the bone-anchored hearing aid. J Laryngol Otol. 1994;108:1031–5.
De Wolf MJF, Hol MKS, Huygen PLM, Mylanus EAM, Cremers CWRJ. Clinical outcome of the simplified surgical technique for BAHA implantation. Otol Neurotol. 2008;29:1100–8.
Stalfors J, Tjellström A. Skin reactions after BAHA surgery: a comparison between the U-graft technique and the BAHA dermatome. Otol Neurotol. 2008;29:1109–14.
Calon TGA, van Hoof M, van den Berge H, et al. Minimally Invasive Ponto Surgery compared to the linear incision technique without soft tissue reduction for bone conduction hearing implants: study protocol for a randomized controlled trial. Trials. 2016;17:1–11.
McLarnon CM, Johnson I, Davison T, et al. Evidence for early loading of osseointegrated implants for bone conduction at 4 weeks. Otol Neurotol. 2012;33:1578–82.
Scholz M, Eufinger H, Anders A, et al. Intracerebral abscess after abutment change of a bone anchored hearing aid (BAHA). Otol Neurotol. 2003;24:896–9.
Tjellström A, Niparko JK. Intracerebral abscess after BAHA abutment change. Otol Neurotol. 2005;26:552–3.
House JW, Kutz JW Jr. Bone-anchored hearing aids: incidence and management of postoperative complications. Otol Neurotol. 2007;28:213–7.
Shirazi MA, Marzo SJ, Leonetti JP. Perioperative complications with the bone-anchored hearing aid. Otolaryngol Head Neck Surg. 2006;134:236–9.
Hobson JC, Roper AJ, Andrew R, Rothera MP, Hill P, Green KM. Complications of bone-anchored hearing aid implantation. J Laryngol Otol. 2010;124:132–6.
Holgers K, Tjellström A, Bjursten L, Erlandsson B. Soft tissue reactions around percutaneous implants: a clinical study of soft tissue conditions around skin-penetrating titanium implants for bone-anchored hearing aids. Am J Otol. 1988;9:56–9.
Dimitriadis PA, Farr MR, Allam A, Ray J. Three year experience with the cochlear BAHA attract implant: a systematic review of the literature. BMC Ear Nose Throat Disord. 2016;16:1–8.
Laske RD, Röösli C, Pfiffner F, Veraguth D, Huber AM. Functional results and subjective benefit of a transcutaneous bone conduction device in patients with single-sided deafness. Otol Neurotol. 2015;36:1151–6.
Sprinzl G, Lenarz T, Ernst A, et al. First European multicenter results with a new transcutaneous bone conduction hearing implant system: short-term safety and efficacy. Otol Neurotol. 2013;34:1076–83.
Steinmetz C, Mader I, Arndt S, Aschendorff A, Laszig R, Hassepass F. MRI artefacts after Bonebridge implantation. Eur Arch Oto-Rhino-Laryngol. 2014;271:2079–82.
Gurgel RK, Shelton C. The SoundBite hearing system: patient-assessed safety and benefit study. Laryngoscope. 2013;123:2807–12.
Battista RA, Mullins K, Wiet RM, Sabin A, Kim J, Rauch V. Sound localization in unilateral deafness with the Baha or TransEar device. JAMA Otolaryngol Head Neck Surg. 2013;139:64–70.
House JW, Kutz JW, Chung J, Fisher LM. Bone-anchored hearing aid subjective benefit for unilateral deafness. Laryngoscope. 2010;120:601–7.
Kim G, Ju HM, Lee SH, Kim HS, Kwon JA, Seo YJ. Efficacy of bone-anchored hearing aids in single-sided deafness: a systematic review. Otol Neurotol. 2017;38:473–83.
Siau D, Dhillon B, Andrews R, Green KMJ. Bone-anchored hearing aids and unilateral sensorineural hearing loss: why do patients reject them? J Laryngol Otol. 2015;129:321–5.
Laitakari K, Löppönen H, Salmivalli A, Sorri M. Objective real ear measurements of bone-conduction hearing aid performance. Scand Audiol. 1995;24:53–6. http://www.ncbi.nlm.nih.gov/pubmed/7761800. Accessed 5 Jun 2018.
Håkansson B, Carlsson P. Skull simulator for direct bone conduction hearing devices. Scand Audiol. 1989;18:91–8. http://www.ncbi.nlm.nih.gov/pubmed/2756338. Accessed 5 Jun 2018.
Valente M, Oeding K, Brockmeyer A, Smith S, Kallogjeri D. Differences in word and phoneme in quiet, sentence recognition in noise and subjective outcomes between manufacturer first fit and bone-anchored device programmed to DSL I/O. J Am Acad Audiol. 2018;29:706–21.
Wazen J, Spitzer J, Ghossaini S, et al. Transcranial contralateral cochlear stimulation in unilateral deafness. Otolaryngol Head Neck Surg. 2003;129:248–54.
Hol M, Bosman A, Snik A, Mylanus E, Cremers C. Bone-anchored hearing in unilateral inner ear deafness: a study of 20 patients. Audiol Neurotol. 2004;9:274–81.
Bosman A, Hol M, Snik A, Mylanus E, Cremers C. Bone-anchored hearing aids in unilateral inner ear deafness. Acta Otolaryngol. 2003;123:258–60.
Niparko JK, Cox KM, Lustig LR. Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otol Neurotol. 2003;24:73–8.
Baguley DM, Bird J, Humphriss RL, Prevost AT. The evidence base for the application of contralateral bone anchored hearing aids in acquired unilateral sensorineural hearing loss in adults. Clin Otolaryngol. 2006;31:6–14.
Hol MKS, Kunst SJW, Snik AFM, Cremers CWRJ. Pilot study on the effectiveness of the conventional CROS, the transcranial CROS and the BAHA transcranial CROS in adults with unilateral inner ear deafness. Eur Arch Oto-Rhino-Laryngol. 2010;267:889–96.
Snapp HA, Holt FD, Liu X, Rajguru SM. Comparison of speech-in-noise and localization benefits in unilateral hearing loss subjects using contralateral routing of signal hearing AIDS or bone-anchored implants. Otol Neurotol. 2017;38:11–8.
Finbow J, Bance M, Aiken S, Gulliver M, Verge J, Caissie R. A comparison between wireless CROS and bone-anchored hearing devices for single-sided deafness: a pilot study. Otol Neurotol. 2015;36:819–25.
House WF, Hitselberger WE. Twenty-year report of the first auditory brain stem nucleus implant. Ann Otol Rhinol Laryngol. 2001;110:103–4.
Shannon RV, Fayad J, Moore J, et al. Auditory brainstem implant: II. Postsurgical issues and performance. Otolaryngol Head Neck Surg. 1993;108:634–42.
Abe H, Rhoton AL. Microsurgical anatomy of the cochlear nuclei. Neurosurgery. 2006;58:728–39.
Otto SR, Shannon RV, Wilkinson EP, et al. Audiologic outcomes with the penetrating electrode auditory brainstem implant. Otol Neurotol. 2008;29:1147–54.
Lim HH, Lenarz T. Auditory midbrain implant: research and development towards a second clinical trial. Hear Res. 2015;322:212–23.
Sanna M, Di Lella F, Guida M, Merkus P. Auditory brainstem implants in NF2 patients. Otol Neurotol. 2012;33:154–64.
Behr R, Colletti V, Matthies C, et al. New outcomes with auditory brainstem implants in NF2 patients. Otol Neurotol. 2014;35:1844–51.
Otto SR, Brackmann DE, Hitselberger WE, Shannon RV, Kuchta J. Multichannel auditory brainstem implant: update on performance in 61 patients. J Neurosurg. 2002;96:1063–71.
Kartush JM, Linstrom CJ, Graham MD, Kulick KC, Bouchard KR. Promontory stimulation following labyrinthectomy: implications for cochlear implantation. Laryngoscope. 1990;100:5–9.
Cueva RA, Thedinger BA, Harris JP, Glasscock ME. Electrical promontory stimulation in patients with intact cochlear nerve and anacusis following acoustic neuroma surgery. Laryngoscope. 1992;102:1220–4.
Vrabec JT, Lambert PR, Arts HA, Ruth RA. Promontory stimulation following translabyrinthine excision of acoustic neuroma with preservation of the cochlear nerve. Am J Otol. 1995;16:643–7. http://www.ncbi.nlm.nih.gov/pubmed/8588670. Accessed 23 May 2018.
Chen DA, Linthicum FH, Rizer FM. Cochlear histopathology in the labyrinthectomized ear: implications for cochlear implantation. Laryngoscope. 1988;98:1170–2. http://www.ncbi.nlm.nih.gov/pubmed/3185070. Accessed 23 May 2018.
Hoffman RA, Kohan D, Cohen NL. Cochlear implants in the management of bilateral acoustic neuromas. Am J Otol. 1992;13:525–8. http://www.ncbi.nlm.nih.gov/pubmed/1449178. Accessed 23 May 2018.
Pensak ML, Tew JM, Keith RW, Vanloveren HR. Management of the acoustic neuroma in an only hearing ear. Skull Base Surg. 1991;1:93–6. http://www.ncbi.nlm.nih.gov/pubmed/17170828. Accessed 23 May 2018.
Tono T, Ushisako Y, Morimitsu T. Cochlear implantation in an intralabyrinthine acoustic neuroma patient after resection of an intracanalicular tumor. Adv Otorhinolaryngol. 1997;52:155–7. http://www.ncbi.nlm.nih.gov/pubmed/9042475. Accessed 23 May 2018.
Zwolan TA, Shepard NT, Niparko JK. Labyrinthectomy with cochlear implantation. Am J Otol. 1993;14:220–3. http://www.ncbi.nlm.nih.gov/pubmed/8372917. Accessed 23 May 2018.
Hulka GF, Bernard EJ, Pillsbury HC. Cochlear implantation in a patient after removal of an acoustic neuroma. The implications of magnetic resonance imaging with gadolinium on patient management. Arch Otolaryngol Head Neck Surg. 1995;121:465–8.
Arriaga MA, Marks S. Simultaneous cochlear implantation and acoustic neuroma resection: imaging considerations, technique, and functional outcome. Otolaryngol Head Neck Surg. 1995;112:325–8.
Roehm PC, Clair JM-S, Jethanamest D, et al. Auditory rehabilitation of patients with neurofibromatosis Type 2 by using cochlear implants. J Neurosurg. 2011;115:827–34.
Carlson ML, Breen JT, Driscoll CL, et al. Cochlear implantation in patients with neurofibromatosis type 2: variables affecting auditory performance. Otol Neurotol. 2012;33(5):853–62.
Lloyd SK, Glynn FJ, Rutherford SA, et al. Ipsilateral cochlear implantation after cochlear nerve preserving vestibular schwannoma surgery in patients with neurofibromatosis type 2. Otol Neurotol. 2014;35(1):43–51.
Lassaletta L, Aristegui M, Medina M, et al. Ipsilateral cochlear implantation in patients with sporadic vestibular schwannoma in the only or best hearing ear and in patients with NF2. Eur Arch Oto-Rhino-Laryngol. 2016;273(1):27–35.
Rooth MA, Dillon MT, Brown KD. Prospective evaluation of patients undergoing translabyrinthine excision of vestibular schwannoma with concurrent cochlear implantation. Otol Neurotol. 2017;38:1512–6.
Neff BA, Wiet RM, Lasak JM, et al. Cochlear implantation in the neurofibromatosis type 2 patient: long-term follow-up. Laryngoscope. 2007;117(6):1069–72.
Carlson ML, Neff BA, Link MJ, et al. Magnetic resonance imaging with cochlear implant magnet in place. Otol Neurotol. 2015;36(6):965–71.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wick, C.C., Durakovic, N., Herzog, J.A., Buchman, C.A. (2022). Hearing Rehabilitation Following Acoustic Neuroma Surgery. In: Bambakidis, N.C., Megerian, C.A., Spetzler, R.F. (eds) Surgery of the Cerebellopontine Angle. Springer, Cham. https://doi.org/10.1007/978-3-031-12507-2_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-12507-2_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-12506-5
Online ISBN: 978-3-031-12507-2
eBook Packages: MedicineMedicine (R0)