Abstract
Biologics and targeted therapies are increasingly being used for many autoimmune and malignant diseases Rosman Z et al. Biologic therapy for autoimmune diseases: an update. BMC medicine 2013;11:88; IQVIA institute. Biologics Market Dynamics: Setting the Stage for Biosimilars. 2020; Available at:https://www.ftc.gov/system/files/documents/public_events/1568297/aitken_-_biologics_market_dynamics_setting_the_stage_for_biosimilars_slides.pdf. Accessed May/24, 2021; Patented Medicine Prices Review Board (PMPRB). Biologics in Canada. Part 1: Market Trends, 2018. 2020; Available at: https://www.canada.ca/content/dam/pmprb-cepmb/documents/reports-andstudies/chartbooks/biologics-part1-market-trends.pdf. They have been shown to be safe and effective medications for these indications, but due to their mechanism of action, they alter immune function (Fernández-Ruiz M et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: an infectious diseases perspective (Introduction). Clinical Microbiology and Infection. 24:S2-S9). This may increase a patient’s susceptibility to infections—some of which are vaccine preventable diseases. It is therefore important to vaccinate these patients for as many preventable illnesses as possible. This chapter summarizes the available data on vaccine safety and efficacy in patients on biologic and targeted therapies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Summary Table

Evidence Summary by Medication Class
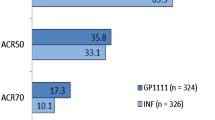
TNF-Alpha Inhibitors and Abatacept
Hepatitis B (HBV) Vaccine
Patients on TNF inhibitors may have a lower response rate to HBV vaccine that is not significantly improved by using high dose vaccine. The general trend of declining response with age is seen in these patients as well.
HBV vaccine is more than 90% effective in healthy young adults and 95% effective in infants, children, and adolescents after three doses. However, after age 40 only 90% respond with protective titers with a further decline to 75% by age 60. It is recommended that patients on renal replacement therapy receive high dose HBV vaccine. This recommendation may be applicable to other immunocompromised patients, but specific groups are not mentioned [1].
In a study looking at high dose (HD) vs. standard dose (SD) HBV vaccine with patients on TNF inhibition, no significant difference was found (61.1% in HD, 49.3% in SD) [2].
In a retrospective chart review using healthy hospital employees as controls, 60.8% of chronic inflammatory disease patients responded to HBV vaccine vs. 94.3% of healthy controls. 33–80% of patients on anti-TNF therapy had protective titers, depending on which TNF inhibitor was prescribed (infliximab and certolizumab had the lowest seroconversion rate). Increasing age and longer time on biologics tended to cause decreased response rates [3]. In a subset of patients (N = 4) receiving anti-TNF therapy, all 4 responded to HBV vaccine with only mild side effects. One patient had a disease flare unrelated to the vaccine [4]. In another cohort study, response rates to HBV vaccine varied by biologic prescribed but ranged from 67% to 100% (lowest were abatacept and adalimumab). Older patients were more likely to be nonresponders [5].
Among children receiving HBV vaccine on TNF inhibition—lower titers were observed; however, overall seroprotective titer rate was similar. There may be a faster decline in titers, but 74% of children responded to boosters. No safety concerns were noted [6].
Pneumococcal Vaccine
There is some conflicting evidence, but patients on abatacept may have decreased response to pneumococcal vaccination with preserved response in patients on TNF-inhibitors. Patients on TNF inhibition, but not abatacept, responded to boosting PCV-13 with PPSV-23.
In a study of patients with inflammatory rheumatic diseases, fewer patients on abatacept responded to PCV13 and PPSV23 than controls or patients on cDMARDs. Antibody increase was seen post PCV-13, but not PPSV-23 in the abatacept group. Antibody functionality (as measured by opsonophagocytosis) was also reduced [7]. In contrast, in a systematic review and meta-analysis more patients on TNF inhibitors seroconverted post PPSV-23 suggesting some benefit of boosting PCV-13 response with PPSV-23. In the same meta-analysis, older patients, longer disease history, and higher disease activity score correlated with nonresponse [8].
In a study of 88 rheumatoid arthritis (RA) patients, 17 receiving abatacept, response to PCV-13 was lower in the abatacept group compared to controls. For one strain, response was better than the methotrexate only group [9]. In another study of 149 RA patients—50 on combination therapy with methrotrexate and TNF-i and 62 on TNF-i alone—compared to healthy controls, all groups had similar response rates to PPSV-23. Interestingly, the methotrexate group had the lowest response rate, although this was not statistically significant [10]. An additional study of 22 RA patients receiving etanercept (with or without methotrexate) compared with 24 osteoarthritis controls showed greater than twofold increases in IgG titers in both groups after PCV-13 vaccination. The control group had higher titers than the etanercept group [11]. In 96 IBD patients, response and antibody titer to PPSV-23 was lower in infliximab and combination therapy groups (infliximab + cDMARD). Disease activity was not found to correlate in multivariate analysis. Vaccine was well tolerated with only two mild reactions noted and no disease flare post vaccine [12].
Influenza Vaccine
Influenza vaccine is safe and well tolerated with some conflicting evidence on efficacy (most studies showing no difference in seroresponders). Antibody titers may be improved by high dose vaccine; they may not last as long as in immunocompetent patients. Vaccination reduces the number of influenza-related adverse events.
In a study of patients with chronic inflammatory diseases, there were no differences between TNF-I, abatacept, tocilizumab, and anakinra groups with lower response rates in the rituximab group. No healthy control or disease control groups were analyzed [13]. In another study looking at TNF-i, TNF-i plus other immunosuppression, or healthy controls there was no difference in number of patients with seroprotective titers post influenza vaccination. However, seroconversion rate (measured as >fourfold rise in titer) was lower in the TNF and combination therapy groups. Vaccine was safe and well tolerated with four mild adverse reactions and no disease flares [14]. Similar results were found in a systematic review of RA patients on TNF inhibition compared to healthy controls [15] and other studies [16, 17], although response on abatacept was lower in one (N = 20) [16]. Conversely, two studies found decreased seroprotection rates in patients on TNF-i compared to healthy controls, especially with influenza B [18, 19] and an additional study with decreased rates against H1 Influenza compared to healthy controls but not methotrexate [20]. No serious adverse events or disease flares were reported.
In a study of 40 patients on TNF inhibition comparing high dose versus standard dose vaccine, high dose vaccine was associated with higher seroprotection and seroconversion rates [21].
Lokota et al. studied the effects of using a pandemic influenza vaccine post trivalent vaccine with another booster a few weeks later. Again, seroprotective rates were similar in TNF-i, tocilizumab, and healthy controls but titers waned more quickly in the immunosuppressant group. The booster dose did not significantly change the number of patients with seroprotective titers or increase longevity of antibody response [22].
In a study looking at the long-term effects of adalimumab, a sub-group of vaccinated vs. unvaccinated patients was analyzed for influenza-related adverse events. These occurred in 14% of unvaccinated patients compared to 5% of vaccinated patients [23].
Live Vaccines
Live vaccines are likely safe up to 14 days prior to biologic start. Although there are limited data, MMR and varicella vaccine may be safely administered on therapy. There are case reports of vaccine strain-related yellow fever infections, although revaccination may be tolerated. BCG vaccination can lead to vaccine strain disease.
In a review of children on biologic medications, overall data suggests VZV vaccine has maintained efficacy with mild reactions (no reaction to mild self-limiting vesicular rash noted). No flares were noted. Similarly, there were no safety concerns with the MMR vaccine. Seroprotective rates were similar to non-immunocompromised vaccine recipients, with a trend to lower antibody titers [6, 24].
There are two studies published on the use of live vaccines (Measles, mumps, rubella, varicella, and rotavirus vaccines) prior to infliximab (14–90 days prior) for Kawasaki’s disease. No serious vaccine-related adverse events were reported; however, patients received vaccine prior to biologic start and most received only one dose of infliximab [25, 26].
A few case reports of yellow fever following yellow fever vaccination in patients on TNF inhibition or adalimumab. One patient recovered without need for hospitalization and only noted prolonged fatigue. Seroprotective antibodies persisted for at least 10 months (no further measurements reported) [27]. Another developed fever and increased liver enzymes with no other complications and development of protective antibodies [28], and a third had no illness reported with protective antibodies measured 2 years post vaccine [29].
The preceding three cases were reported from areas not endemic for yellow fever. There are two reports from Brazil—one with 31 patients with rheumatic illness including three on infliximab. There were only mild adverse events noted, with titers lower than in healthy controls [30]. The other report included 17 patients on infliximab and methotrexate revaccinated during the outbreak (preceding vaccine was 10–22 years prior) with only two patients having no detectable titers prior to vaccine. All but one patient responded to vaccine with a trend to lower titers in the immunosuppressed group. No safety concerns were noted [31].
A Crohn’s patient on infliximab inadvertently injected with BCG vaccine developed an abscess at the injection site requiring drainage and systemic therapy for 6 months [32]. Another patient on infliximab given BCG vaccine had no symptoms up to 9 months later [33].
IL-1 Inhibitors
Data found only for canakinumab. No difference in vaccine response or increase in adverse events even in cases of live vaccines (N = 3), except unusual severe inflammatory reaction noted with pneumococcal vaccines in patients with CAPS.
In a study of 51 healthy volunteers (25 given canakinumab and 26 controls), there was no difference in response to influenza or meningococcal vaccine. No serious adverse events were noted [34].
Analysis of vaccine response in 68 cryopyrin associated periodic syndrome (CAPS) patients from a registry being treated with canakinumab. Fifty-five patients received influenza vaccine (107 vaccines administered) with 7 mild reactions. Twelve patients received tetanus and diphtheria vaccine with mild reactions noted. Eleven patients received 21 other vaccines (6 HBV, 5 HAV, 3 typhoid, 2 tick borne encephalitis, 1 polio, 1 MMR, 1 HPV, 1 Lyme disease, and 1 cholera) with 21 non-severe reactions noted. Eighteen patients received 19 pneumococcal vaccines (2 PCV-13, 15 PPSV-23, 2 unknown) with 5 serious adverse reactions to PPSV-23, 3 of these requiring hospitalization (1 non-resolving fever, 2 headache and nausea (1 possible meningitis)) [35].
Two more reports of CAPS patients (one in age 5 and younger and the other in pediatric and adult patients) reported good vaccine seroconversions rates with no adverse events, including in the patients receiving pneumococcal vaccines. One live vaccine (MMR) was administered [36, 37]. There is an additional case report of live vaccines administered while on canakinumab—measles, mumps, rubella, and varicella with no adverse effects and documented seroconversion [38].
In a report of 7 patients with CAPS (6 receiving canakinumab), 2 had systemic reactions, including one meningitis, post pneumococcal vaccination (1 PPSV and 1 PCV13), and 5 had severe local reactions. The authors hypothesize that this could be due to stimulation of TLR-2 and TLR-4, as this reaction was not seen with other vaccines in the same patients [39].
IL-6
Small numbers for each individual vaccine , but most studies show little impact on post vaccine titers. Data is from tocilizumab patients only.
HBV Vaccine
Within a larger cohort of patients on various immunosuppressive agents given HBV vaccine—7/9 (78%) of patients on tocilizumab responded with protective titers [5].
Pneumococcal Vaccine
Sixteen patients treated with tocilizumab within 88 RA patient cohort receiving PCV-13 showed the same number of seroresponders as control. Absolute titers were lower in the tocilizumab group [9]. Ninety one patients receiving tocilizumab plus methotrexate showed numerically lower response rates than methotrexate alone for PPSV-23 (60% vs. 70.8%), but this did not reach significance [40]. In other studies, all 21 patients receiving tocilizumab responded to PPSV-23 [41], and there was no difference in response rates between tocilizumab and RA control patients [42].
Influenza
Six studies for influenza vaccine included patients on tocilizumab. Two studies showed equal seroprotective rates compared to control for influenza A [22, 43]; however, titers waned more quickly compared to control [22]. Seroresponse rate was slightly decreased for Influenza B in one study [43]. One study (N = 5 patients on tocilizumab) showed decreased response compared to other immunosuppressants (methotrexate and TNF-inhibitors) [16]. Three other studies (one in JIA patients, two in RA patients) showed no difference in response on tocilizumab compared to age matched controls (JIA) or other DMARDs (RA patients) [41, 44, 45].
There were no serious adverse events or disease flares noted in the above studies, but there is one case report in a JIA patient with disease flares post both doses of influenza vaccine [46].
Tetanus
Tetanus vaccine seroconversion was similar between both groups (42% for combination and 39.1% in methotrexate alone) [40].
Live Vaccines
In two studies on juvenile idiopathic arthritis patients (only three patients total on tocilizumab), no safety issues or vaccine strain disease was noted. Varicella antibodies titers were low 11 and 27 months post vaccine [47, 48].
IL-12/23
Few studies involved patients on Ustekinumab but the response rates were similar to controls except for hepatitis B vaccine.
Twenty-five patients on Ustekinumab among 109 patients with inflammatory disease were vaccinated against hepatitis B. There was a 72% response rate in the Ustekinumab group. Overall, there was no improvement in response rate with a higher dose [2].
Sixty psoriasis patients on Ustekinumab were compared to 50 patients not on systemic therapy after PPSV-23 and tetanus vaccines. There was no difference in vaccine response [49].
Twenty-seven patients with Crohn’s disease (15 Ustekinumab, 12 adalimumab) and 20 healthy controls were vaccinated with the seasonal influenza vaccine. No difference in titers between ustekinumab patients and healthy controls, and post vaccine T-cell responses were also similar [50].
IL-17
Only a few studies are available, but the evidence suggests no impact on vaccine response rates. No data available for live vaccines.
Three studies compared influenza vaccine in patients receiving secukinumab (two in psoriasis patients and one in healthy volunteers). No differences in post vaccine titer or response and no serious adverse events or disease flares were recorded [51,52,53].
The study with healthy volunteers also looked at the group C meningococcal vaccine response. Again, responses between the secukinumab and control groups were similar [51].
One study with ixekizumab looked at responses to PPSV-23 and tetanus vaccine in healthy volunteers. No differences in response rates were noted. All adverse events were mild—mostly headache, injection site erythema, and fatigue [54].
Eculizumab
Patients on eculizumab are at extremely high risk of invasive meningococcal disease. These patients should receive both the quadrivalent and MenB vaccines prior to therapy initiation. Given the breakthrough infections, sub-optimal vaccine response, and non-vaccine strains causing critical (and occasionally fatal) disease, consideration should be given to antimicrobial prophylaxis.
Current recommendations include immunization against meningococcal disease using both quadrivalent (MenACYW) and MenB vaccine [120,121,57]. Booster vaccines are recommended while patients continue on eculizumab, as rates of disease as well as mortality are higher compared to the general population. Preferably, vaccination series should be completed at least 2 weeks prior to the first dose of eculizumab, but if treatment is urgent, antimicrobial prophylaxis should be provided for at least 2 weeks [58].
Studies looking at titers post vaccination show a general trend of lower titers and response rates. Nine patients with cold agglutinin disease were vaccinated for MenACYW and response rates were 25%, 37.5%, 75%, and 62.5% to group A, C, Y, and W respectively. Patients with prior B cell therapy (like rituximab) were less likely to respond. No cases of meningococcal disease were reported [59]. In another study of 23 patients with PNH, overall response rates were 78%, 87%, 48%, and 70% for groups A, C, Y, and W respectively [60]. In a subset of pediatric patients with splenic or complement deficiencies, the eight patients on eculizumab had lower response rates compared to the other children [61]. In 25 patients receiving eculizumab for aHUS, only 20% showed a full response after the first dose of quadrivalent meningococcal vaccine, a further 36% responded after the second dose. Incomplete response was seen in 52% after the first dose and 29% of the revaccinated patients [62].
Response to the menB vaccine is likely also reduced. In a study of 15 patients with aHUS (5 on eculizimab at time of vaccination), response rates were only 50%. Titers were measured when patients were off eculizumab as human complement is needed to judge response (which is blocked by eculizumab) [63]. In 43 patients with PNH, IgG, and IgG binding post MenB vaccine was similar to healthy controls. However, no whole blood killing was noted. Therefore despite adequate titers, there may be an impaired response when exposed [64].
Meningococcemia has been noted even in immunized patients [62,63,67] and occasionally despite prophylactic antimicrobials [68, 69]. Fatal sepsis from non-vaccine strains has also been reported [70].
VEGF Inhibitors (Bevacizumab, Aflibercept)
Very little data, therefore no comment can be made for efficacy compared to other oncology patients. No serious adverse events reported for the 3 bevacizumab patients.
Ninety-five oncology patients treated with various chemotherapy agents, including 3 on bevacizumab, were given seasonal influenza, pandemic influenza, and PPSV 23 vaccine. Response rates were divided into rituximab and non-rituximab patients with no further breakdown. In the 83 patients not on rituximab, 62% and 87% responded after dose 1 and 2 of the pandemic influenza vaccine. Response rate for the seasonal influenza was 70% for H1N1, 58% for H3N2, and 43% for the PPSV-23 vaccine. No serious adverse events were reported [71].
VEGF-R Inhibitors (Sorafenib, Sunitinib, Axitinib, Pazopanib, Regorafenib, Vandetanib, Cabozantinib, Ramucirumab)
Influenza vaccine appears to have the same response in patients on sorafenib and sunitinib as healthy control in a very small number of patients. No serious adverse events were mentioned in the study.
In the previously mentioned study, one patient was on sunitinib. Since no breakdown of the non-rituximab patients was reported, no comment on efficacy can be made. No serious adverse events were reported [71].
Sixteen sunitinib and six sorafenib patients were compared to 11 healthy control and seven patients with metastatic RCC without systemic therapy. There was no difference in titers measured post vaccination between groups, but the patients on sorafenib had lower interferon gamma production and lymphocyte proliferation. Adverse event rates were not mentioned [72].
ErbB2/HER2 Inhibitors (Trastuzumab, Pertuzumab)
In a small number of patients on trastuzumab only, influenza vaccine had the same response rate as healthy controls and was well tolerated.
Influenza vaccine was given to 37 patients on trastuzumab vs. 20 healthy controls and titers were checked post immunization. Patients on any other immunosuppressive therapy, metastatic cancer, and dual HER2 blockade patients were excluded. Similar seroconversion and seroprotective rates between groups for the H1N1 and influenza B strains after adjusting for baseline titer differences, five patients had mild adverse events that resolved within 48 h (local pain, arthalgias, myalgias, chills), and one skin and skin structure infection unrelated to vaccine site. No influenza like illness was reported in either group during the follow-up period [73].
ErbB Receptor Tyrosine Kinases (Erlotinib, Gefitinib, Afatinib, Osimertinib, Lapatinib, Neratinib)
Very little data, but only a few mild reactions in a small number of erlotinib patients receiving influenza vaccine.
Fourteen patients with NSCLC on erlotinib received seasonal influenza vaccine (11 vaccines) and pandemic H1N1 vaccine (seven vaccines). No data on immunogenicity, but only two mild reactions were observed (pain at injection site and rash). No patients developed influenza [74].
BCR-ABL Tyrosine Kinase Inhibitors (Imatinib, Dasatinib, Nilotinib, Bosutinib, Ponatinib)
With the limited data available, influenza vaccine appears to be safe. Seroprotective rates are similar to other patients on chemotherapy, but rates are lower than reports from other biologics or immunocompetent patients. A few live virus vaccines were administered to CML patients with some efficacy and no adverse events.
Four patients with CML (age 12–15) on imatinib were vaccinated against measles and varicella. Fifty percent had stable seroconversion, one did not seroconvert for varicella, and one lost immunity and so was re-immunized. No adverse vaccine events were reported, and imatinib was held for only one patient for 1 week pre- and 2 weeks post-vaccine. All patients had stable disease (ratio BCR-ABL1/ABL1 = 1% or lower with lymphocyte counts >1500 cells/μL) at the time of vaccination [75].
In a study on response to Influenza vaccine, 33% of patients on tyrosine kinase inhibitors responded with protective titers against all three strains compared to 27% of patients on other chemotherapies. No serious adverse events were reported, two patients had injection site pain and fever. Two influenza infections occurred in this patient population, but not in patients with protective titers [76].
Burton Tyrosine Kinase Inhibitors (Ibrutinib, Acalabrutinib)
Data only for ibrutinib. Small numbers, but data suggests decreased vaccine response for influenza, PCV-13, and hepatitis B vaccine.
Two studies looked at the response to influenza vaccine in patients on ibrutinib (almost all CLL, 1 Waldenstrom’s macroglobulinemia). Influenza response was lower in the ibrutinib group (N = 14) compared to healthy controls. Five infections were reported in the ibrutinib group, only one was confirmed as influenza B [77]. Another study with 19 patients showed that 74% of patients had seroprotective titers post immunization, although only five patients had increasing antibody levels enough to seroconvert. Seven patients developed ILI—one confirmed influenza B, the others were mild and not lab-confirmed [78]. No mention of vaccine-related side effects in either study.
In a subgroup analysis of CLL patients treated with ibrutinib (N = 34), only one patient had an immune response to PCV13 based on IgG measurements. Side effects were seen in four patients and were mild. Another study compared patients with CLL on ibrutinib to controls—none of the patients in the ibrutinib group responded to PCV-13, whereas all four of the control patients did. All the ibrutinib patients were also on rituximab, so that may have confounded the findings [79].
A total of 315 lymphoma patients were vaccinated with hepatitis B vaccine—118 in the low dose group, 118 in the high dose group, and 79 in the high dose, high frequency group. Response rates were 68.8%, 81.4%, and 82.3% respectively. Only 47.4% of the ibrutinib patients responded to vaccine [80].
PI3K Inhibitors Idelalisib, Buparlisib, Rigosertib, Duvelisib
One study with PCV-13 in ten patients suggests decreased ability to respond to vaccines.
In a subgroup analysis of CLL patients treated with idelalisib (N = 10), none had a response to PCV13 as measured by IgG response. Vaccine-related adverse events were mild [81].
Janus Kinase Inhibitors (Ruxolitinib, Tofacitinib, Baricitinib)
Vaccine response may be blunted for patients on Janus kinase inhibitors, especially when used with methotrexate. Live vaccines administered prior to biologic start are safe.
Pneumococcal Vaccine
Response to PCV13 was tested in 60 patients on tofacitinib for psoriasis. More than 80% of patients responded adequately, with no difference found in the subgroup of lymphopenic patients. 37.7% of patients reported adverse events, but all were mild reactions [82]. In another study comparing patients on tofacitinib to placebo, fewer patients in the tofacitinib group responded to PPSV-23 (45.1% vs. 68.4%). In the subset of patients only on tofacitinib (without methotrexate) compared to no DMARD, the response was still slightly lower (62.2% vs. 76.7%) [83].
In the same study, the investigators compared vaccine response when tofacitinib was interrupted vs. continued. The response was 75% in the continuous vs. 84.6% in the interrupted group. Again, response rates were higher if the patients were not on concomitant methotrexate (89.2% vs. 91.7%) [83].
One hundred and six rheumatoid arthritis patients on baracitinib (89% also on methotrexate) were vaccinated with PCV-13. Sixty-eight percent of patients had a response that was maintained for at least 3 months. Older age was inversely correlated with response. Adverse effects were all mild [84].
Influenza
Winthrop et al. also compared the reaction to influenza vaccine alongside PPSV-23. The response was 56.9% vs. 62.2% in the tofacitinib and placebo groups, with a higher response seen in the subset of patients not on methotrexate (64.4% vs. 67.4%). The proportion of patients with seroprotective titers was higher in the placebo group (91.8% vs. 76.5%).
Response to influenza in the interrupted arm was 63.7% compared to 66.3%, with seroprotective titers of 75% in the interrupted arm compared to 82.4% [83].
Tetanus
Two studies compared the response to tetanus vaccine—one with tofacitinib and one with baricitinib. Eighty-eight percent of tofacitinib patients had an adequate response and 74% of baricitinib patients. No control group was included. Adverse events were all mild [82, 84].
Live Zoster Vaccine
Two studies compared safety and efficacy of live zoster vaccine (LZV) either 2 or 4 weeks prior to tofacitinib start. In the first, a post hoc analysis of a randomized control trial, 3 (1.4%) patients in the vaccinated arm had herpes zoster compared to 15 (1.6%) in the unvaccinated arm. This was not statistically significant. Only one infection was multidermatomal but none were serious. The vaccine was well tolerated with no vesicular lesions within 42 days of vaccine [85].
The other study looked at 112 patients—55 on tofacitinib and 57 on placebo. Both groups were given LZV 2 weeks prior to tofacitinib start. Judging response by mean fold rise in IgG titers, both groups were similar at week 2, 6, and 14. Seven nonserious adverse events were reported in the tofacitinib group and five in placebo group. An additional three serious events occurred in the tofacitinib group—bronchitis, cholangitis, and primary varicella (in a patient later found to have no primary immunity) [86].
mTOR Inhibitors (Everolimus, Temsirolimus)
In a study of pandemic strain influenza vaccine (2009), seroprotection and seroconversion rates were similar to other solid organ transplant recipients but titers were lower. Four patients were infected with influenza, but none had protective antibodies even post infection. No safety concerns were noted (rejection or vaccine adverse events) [87].
Anti-CD20 (Rituximab, 90Y-Ibritumomab Tiuxetan, Ofatumumab, Ocrelizumab, Veltuzumab, 131I-Tositumomab, Obinutuzumab, Ocaratuzumab, Ublituximab)
Overall results show dramatic decrease in vaccine response lasting months beyond last dose. No increase in adverse events for inactivated vaccines.
Pneumococcal Vaccine
Sixty-eight ocrelizumab patients in the VELOCE study (relapsing multiple sclerosis) were vaccinated with PPSV-23 and PCV-13 (as a booster to PPSV-23). Positive response to PPSV-23 was 71.6% compared to 100% in the control group. PCV-13 did not boost response to PPSV-23 for ocrelizumab patients [88]. Reduction in response to PPSV-23 was also seen in a study of rheumatoid arthritis patients on Rituximab (57% vs. 82%) [89]. Other studies in different diseases also show reduction or no response in response to both PPSV-23 and PCV-13 while on rituximab [7,8,9, 81, 90].
Similar results are found in pediatric lupus patients given PCV-13—among the nine patients on rituximab, only one responded and reached protective titers. Another patient remotely exposed to rituximab (>2 years ago) with hypogammaglobulinemia had a fourfold increase in titers but did not reach protective levels. All control pediatric patients responded to the vaccine [91].
Influenza
Decreased influenza response was noted across many studies and patient populations, with a trend to increasing response with more time between vaccine and rituximab dose. No serious adverse events noted in studies and no disease flares [13, 15, 16, 22, 71, 89,90,91,95].
Hepatitis B Vaccine
Significantly fewer patients on rituximab responded to Hepatitis B vaccine. Response rates varied from 25% to 69.5%. Vaccine was well tolerated with only mild adverse effects noted and no disease flares [4, 5, 80, 96].
Tetanus
Decreased tetanus response was compared to control with ocrelizumab (23.9% vs. 54.5%) [88]. Response to vaccine on rituximab was similar to patients on methotrexate (39.1% vs. 42.3%) [89].
Varicella
Case report of a patient on ocrelizumab vaccinated with varicella vaccine with seroconversion to positive IgG (VZV IgG). After receiving ocrelizumab, titers of VZV IgG declined to nonprotective levels. Repeat vaccination was attempted, but with no response (given 7 months post ocrelizumab dose).
Hematological malignancy patients on anti-CD20 were given a four-dose regimen of the inactivated herpes zoster vaccine. There was a fourfold rise in titer from baseline suggestive of immunogenicity. Most reactions were mild and, while 18 serious adverse events were noted, only one was thought to be vaccine-related (seizures). Five patients reported a vesicular rash [97].
Alemtuzumab
Small amount of data, but vaccine response likely to be reduced especially if within 6 months of alemtuzumab infusion.
Twenty-four multiple sclerosis patients on alemtuzumab (median time since last infusion 18 months) were given multiple vaccines to measure antibody response. Twenty-two patients received diphtheria and tetanus vaccine, 21 received inactivated polio vaccine, 23-valent polysaccharide pneumococcal vaccine (PPSV-23), Haemophilus vaccine, and meningococcal C vaccine. All vaccinated patients had positive IgG to diphtheria and tetanus prior to vaccine, therefore no comment on vaccine effect can be made. Polio seroprotective rate improved from 95% to 100% for type 1 poliovirus, and from 77% to 95% for type 3 poliovirus. Response in patients receiving PPSV-23 exceeded literature controls. Seropositivity for Haemophilus increased from 13% to 74% and from 91% to 100% for meningococcal C vaccine. Overall trend towards decreased vaccine response if within 6 months of alemtuzumab infusion [89, 98].
In 61 islet cell transplant patients, lower seroconversion and seroprotection rates were seen for 2010–2011 influenza vaccine compared to published rates for healthy controls. There was a trend towards lower response if patients received alemtuzumab for induction therapy, regardless of time from transplant. There was a significantly lower response rate in patients who were less than 1 year from their transplant [99].
Anti CD-38 (Daratumumab, Isatuxumab)
Very limited data on a small number of patients with confounding immune system abnormalities. No further decrease in response to pneumococcal vaccine compared to other patients with the same chronic illness. One case report suggesting recombinant zoster vaccine is ineffective.
In a series of multiple myeloma patients (17 on daratumumab, 10 on other immunomodulators) vaccinated against pneumococcal disease, response rates to PCV-13 and PPSV-23 were comparable between the two groups [100].
One case report of a 65-year-old with prior stem cell transplant on daratumumab with a vesicular rash, hypoxic respiratory failure, and subsequent retinitis secondary to VZV. She was vaccinated with recombinant zoster vaccine 6 months prior to presentation and 2 months prior to daratumumab. Virus was sequenced and found to be wild-type, suggesting the vaccine is not effective in all patients [101].
CTLA-4 Inhibitors (Ipilimumab, Tremelimumab)
No increased adverse events noted post influenza vaccine with a lower rate of influenza compared to institutional average.
A retrospective review was done over three influenza seasons (2014–2017) in patients receiving Influenza vaccine within 65 days of immune checkpoint inhibitor. Most patients received PD-1 inhibitors only, but 81 patients received combination therapy with ipilimumab. Only four patients received monotherapy with ipilimumab. 20% of patients experienced immune-related adverse events (IRAEs); the majority were Grade 2–3 in severity. Patients receiving combination therapy had a higher likelihood of having an IRAE and it being more severe. There were no large local reactions or severe post vaccine events. These rates are not higher than published literature for the medications alone, leading the authors to conclude that vaccination did not lead to increased IRAEs. The rate of influenza in these vaccinated patients over 3 years was 3.5% compared to the institutional incidence of 10.7% [102].
PD-1 and PD-1 Ligand Inhibitors (Nivolumab, Pembrolizumab, Atezolizumab)
Data mostly on Influenza vaccine—high baseline immune-related adverse events, but these were not worse with vaccine administration in all but one study.
Influenza Vaccine
The retrospective review mentioned above included patients mostly on PD-1 inhibitors. As noted earlier, no increased IRAEs were noted in the influenza-vaccinated patients compared to the published literature. The rate of influenza in these vaccinated patients over 3 years was 3.5% compared to the institutional incidence of 10.7% [102]. In two cohort studies, the incidence of IRAEs was not higher in the vaccinated group. There was also no increased risk if the vaccine was given in between doses [103, 104].
One study with 23 patients compared to 11 healthy controls found a slightly lower seropositivity rate in treated patients (not significant). IRAEs occurred in 52.2% of patients with 26.1% of patients having grade 3–4 reactions, including 3 neurological reactions (2 encephalitis and 1 peripheral neuropathy). This rate was higher than the published literature for PD-1 inhibitors [105]. Additionally, there was one report on a patient with Guillain-Barre syndrome (GBS) with symptoms starting 3 weeks post influenza vaccine. Unfortunately, the patient worsened and passed away. The differential for his symptoms included vaccine-related GBS, but also worsening melanoma with brain metastases and nivolumab-associated neurological IRAE [106].
Recombinant Zoster Vaccine
A patient receiving pembrolizumab developed oral and skin lesions suggestive of Stevens-Johnson syndrome 7 days post vaccination with recombinant zoster vaccine. The patient improved on steroids but was not given the second dose of vaccine [107].
LFA-3 Inhibitor (Alefacept)
Data from one study in patients with psoriasis shows polysaccharide pneumococcal vaccine is safe with no loss in efficacy (when compared to patients on other immunomodulators).
Forty-two patients with psoriasis were given PPSV-23 in the middle of 12 weekly doses of Alefacept. Serial antibody titers showed 86% and 78% of patients had a twofold rise at 3 and 6 months, and 57% and 47% of patients had a fourfold rise. This is compared to a baseline rate of 34.5% response for patients on methotrexate and anti-TNF agents. Adverse events were generally mild [108].
Alpha 4-Integrin and LFA-1 Inhibitors (Natalizumab, Vedolizumab, Efalizumab)
Influenza Vaccine
Likely lower response in patients on natalizumab; no difference in one study done for patients on vedolizumab.
Seventeen patients on Natalizumab had no significant difference in Influenza A and B antibody titers post vaccine compared to ten healthy controls. There was a trend towards lower titers in the natalizumab group, but overall small numbers and the groups were not well matched [109]. In another study with 113 patients on immunomodulators (17 on natalizumab and 36 on interferon) compared to 216 healthy controls, response to 2009 H1N1 influenza vaccine was lower in the natalizumab group compared to the interferon or health control groups [89]. A similar trend was found in two other studies comparing 14 patients on natalizumab to patients on interferon [110] and 12 patients on natalizumab compared to 53 controls [111]. In contrast, a study of patient 19 patients on vedolizumab receiving standard dose influenza vaccine showed no difference in seroprotection or seroconversion rates compared to healthy controls [21].
Other Vaccines
Small numbers, but trend suggestive of preserved response to tetanus vaccine and hepatitis B vaccine.
Sixty patients (30 natalizumab, 30 control) were evaluated for their response to tetanus vaccine and keyhole limpet hemocyanin (KLH, a neoantigen). No significant differences were observed between natalizumab and control groups, although the number of patients that responded was slightly lower in the natalizumab group [112]. Similar results were seen in a study with 41 patients on efalizumab compared to 22 controls receiving tetanus vaccine. Antibody titers were slightly lower in the efalizumab group, but seroprotection rates were equivalent [113].
Hepatitis B and oral cholera vaccine responses were assessed in 127 healthy volunteers (64 vedolizumab and 63 placebo). Response to hepatitis B vaccine was preserved, but response to oral cholera vaccine was lower in the vedolizumab group. Adverse events were similar in both groups [114].
Live Vaccines
No disease flare or vaccine illness noted post yellow fever vaccine, but one case report of likely vaccine strain measles.
Twenty-three multiple sclerosis patients on natalizumab received yellow fever vaccine with no adverse events and no flares post vaccine. All patients were from Switzerland and received vaccine for travel reasons. Therefore, they would be unlikely to have prior immunity or exposure [115].
One case report of a patient on natalizumab developing non-severe measles 7 days post vaccine. No typing was done, but the diagnosis was confirmed by PCR. However, the report is from Switzerland with no known community measles contact, making it more likely that this is vaccine strain disease [116].
Sphingosine 1-Phosphate Receptor Inhibitor (Fingolimod, Siponimod)
Data suggests lowered vaccine response, and possible loss of protective antibodies from prior vaccines.
A review of multiple sclerosis patients on immunomodulators had conflicting evidence regarding patients on fingolimod receiving Influenza vaccine—two studies showing no difference in efficacy (with lower absolute antibody titers) and two studies showing lowered seroprotection (smaller numbers) [89]. A study of Siponimod in healthy persons receiving influenza vaccine and polysaccharide pneumococcal vaccine showed decreased response to Influenza B in the continued therapy and interrupted therapy groups. All groups responded well to the pneumococcal vaccine [117].
Two patients on fingolimod vaccinated against tick-borne encephalitis had the lowest antibody increase compared to 18 other multiple sclerosis patients. It is unknown if they developed protective (but low) titers [118]. Out 23 patients vaccinated for varicella zoster virus (VZV) prior to therapy, 7 lost detectable antibody. Out of three patients that stopped fingolimod due to side effects, two recovered varicella antibody and one developed chickenpox 1 year post fingolimod [119]. There is also one case report of a patient on fingolimod developing VZV encephalitis despite history of chickenpox and prior vaccination. This patient was also previously treated with natalizumab [120].
Proteosome Inhibitors (Bortezomib, Carfilzomib, Ixazomib)
No data on efficacy, but MMR vaccine may be tolerated while on proteosome inhibitors. One study showing clinical benefit with pneumococcal vaccine.
Thirteen multiple myeloma patients post stem cell transplant on bortezomib were vaccinated for the measles, mumps, and rubella (MMR) vaccine 25 months post transplant. Three patients had mild adverse events, but there was no vaccine strain disease, no fevers, no hospitalizations, and no deaths. No titers were done to look at efficacy [121]. In a study looking at conjugate pneumococcal vaccine efficacy, 18 vaccinated multiple myeloma patients (11 on bortezomib and 2 on ixazomib) were compared to 18 unvaccinated multiple myeloma patients (9 on bortezomib and 5 on ixazomib). The rate of pneumonia over 1 year was 16.7% in the vaccinated group and 50% in the unvaccinated group, suggesting that pneumococcal vaccine is effective at preventing clinical disease. No adverse vaccine events were documented in the study. The dosing of vaccine was unusual (three doses given 1 month apart) [122].
References
Hamborsky J, Kroger A, Wolfe S, editors. Centers for Disease Control and Prevention. Epidemiology and prevention of vaccine-preventable diseases. 13th ed. Washington, DC: Public Health Foundation; 2015.
Haykir Solay A, Eser F. High dose hepatitis B vaccine is not effective in patients using immunomodulatory drugs: a pilot study. Hum Vaccin Immunother. 2019;15(5):1177–82.
Okay G, Biberci Keskin E, Akkoyunlu Y, Bolukcu S, Betul Uslu A, Meric Koc M. Evaluation of hepatitis B vaccine efficacy and factors affecting vaccine nonresponse in patients receiving anti-tumor necrosis factor agents. Eur J Gastroenterol Hepatol. 2020;33(8):1091–6.
Intongkam S, Samakarnthai P, Pakchotanon R, Narongroeknawin P, Assavatanabodee P, Chaiamnuay S. Efficacy and safety of hepatitis B vaccination in rheumatoid arthritis patients receiving disease-modifying antirheumatic drugs and/or biologics therapy. J Clin Rheumatol. 2018;25(8):329–34.
Richi P, Alonso O, Martin MD, Gonzalez-Hombrado L, Navio T, Salido M, et al. Evaluation of the immune response to hepatitis B vaccine in patients on biological therapy: results of the RIER cohort study. Clin Rheumatol. 2020;39(9):2751–6.
Tse HN, Borrow R, Arkwright PD. Immune response and safety of viral vaccines in children with autoimmune diseases on immune modulatory drug therapy. Expert Rev Vaccines. 2021;19(12):1115–27.
Nived P, Jonsson G, Settergren B, Einarsson J, Olofsson T, Jorgensen CS, et al. Prime-boost vaccination strategy enhances immunogenicity compared to single pneumococcal conjugate vaccination in patients receiving conventional DMARDs, to some extent in abatacept but not in rituximab-treated patients. Arthritis Res Ther. 2020;22(1):36.
van Aalst M, Langedijk AC, Spijker R, de Bree GJ, Grobusch MP, Goorhuis A. The effect of immunosuppressive agents on immunogenicity of pneumococcal vaccination: a systematic review and meta-analysis. Vaccine. 2018;36(39):5832–45.
Crnkic Kapetanovic M, Saxne T, Jonsson G, Truedsson L, Geborek P. Rituximab and abatacept but not tocilizumab impair antibody response to pneumococcal conjugate vaccine in patients with rheumatoid arthritis. Arthritis Res Ther. 2013;15(5):R171.
Kapetanovic MC, Saxne T, Sjoholm A, Truedsson L, Jonsson G, Geborek P. Influence of methotrexate, TNF blockers and prednisolone on antibody responses to pneumococcal polysaccharide vaccine in patients with rheumatoid arthritis. Rheumatology (Oxford). 2006;45(1):106–11.
Rakoczi E, Perge B, Vegh E, Csomor P, Pusztai A, Szamosi S, et al. Evaluation of the immunogenicity of the 13-valent conjugated pneumococcal vaccine in rheumatoid arthritis patients treated with etanercept. Jt Bone Spine. 2016;83(6):675–9.
Fiorino G, Peyrin-Biroulet L, Naccarato P, Szabo H, Sociale OR, Vetrano S, et al. Effects of immunosuppression on immune response to pneumococcal vaccine in inflammatory bowel disease: a prospective study. Inflamm Bowel Dis. 2012;18(6):1042–7.
Richi P, Martin MD, Navio MT, Gonzalez-Hombrado L, Salido M, Llorente J, et al. Antibody responses to influenza vaccine in patients on biological therapy: results of RIER cohort study. Med Clin (Barc). 2019;153(10):380–6.
Andrisani G, Frasca D, Romero M, Armuzzi A, Felice C, Marzo M, et al. Immune response to influenza A/H1N1 vaccine in inflammatory bowel disease patients treated with anti TNF-alpha agents: effects of combined therapy with immunosuppressants. J Crohns Colitis. 2013;7(4):301–7.
Huang Y, Wang H, Tam WWS. Is rheumatoid arthritis associated with reduced immunogenicity of the influenza vaccination? A systematic review and meta-analysis. Curr Med Res Opin. 2017;33(10):1901–8.
Adler S, Krivine A, Weix J, Rozenberg F, Launay O, Huesler J, et al. Protective effect of A/H1N1 vaccination in immune-mediated disease—a prospectively controlled vaccination study. Rheumatology (Oxford). 2012;51(4):695–700.
Elkayam O, Bashkin A, Mandelboim M, Litinsky I, Comaheshter D, Levartovsky D, et al. The effect of infliximab and timing of vaccination on the humoral response to influenza vaccination in patients with rheumatoid arthritis and ankylosing spondylitis. Semin Arthritis Rheum. 2010;39(6):442–7.
Salemi S, Picchianti-Diamanti A, Germano V, Donatelli I, Di Martino A, Facchini M, et al. Influenza vaccine administration in rheumatoid arthritis patients under treatment with TNFalpha blockers: safety and immunogenicity. Clin Immunol. 2010;134(2):113–20.
Mamula P, Markowitz JE, Piccoli DA, Klimov A, Cohen L, Baldassano RN. Immune response to influenza vaccine in pediatric patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5(7):851–6.
Fomin I, Caspi D, Levy V, Varsano N, Shalev Y, Paran D, et al. Vaccination against influenza in rheumatoid arthritis: the effect of disease modifying drugs, including TNF alpha blockers. Ann Rheum Dis. 2006;65(2):191–4.
Caldera F, Hillman L, Saha S, Wald A, Grimes I, Zhang Y, et al. Immunogenicity of high dose influenza vaccine for patients with inflammatory bowel disease on anti-TNF monotherapy: a randomized clinical trial. Inflamm Bowel Dis. 2020;26(4):593–602.
Lakota K, Perdan-Pirkmajer K, Sodin-Semrl S, Cucnik S, Subelj V, Prosenc K, et al. The immunogenicity of seasonal and pandemic influenza vaccination in autoimmune inflammatory rheumatic patients-a 6-month follow-up prospective study. Clin Rheumatol. 2019;38(5):1277–92.
Burmester GR, Landewe R, Genovese MC, Friedman AW, Pfeifer ND, Varothai NA, et al. Adalimumab long-term safety: infections, vaccination response and pregnancy outcomes in patients with rheumatoid arthritis. Ann Rheum Dis. 2017;76(2):414–7.
Borte S, Liebert UG, Borte M, Sack U. Efficacy of measles, mumps and rubella revaccination in children with juvenile idiopathic arthritis treated with methotrexate and etanercept. Rheumatology (Oxford). 2009;48(2):144–8.
Miura M, Kobayashi T, Igarashi T, Hamada H, Iwata N, Sasaki Y, et al. Real-world safety and effectiveness of infliximab in pediatric patients with acute Kawasaki disease: a postmarketing surveillance in Japan (SAKURA study). Pediatr Infect Dis J. 2020;39(1):41–7.
Lee AM, Burns JC, Tremoulet AH. Safety of infliximab following live virus vaccination in Kawasaki disease patients. Pediatr Infect Dis J. 2017;36(4):435–7.
Ekenberg C, Friis-Moller N, Ulstrup T, Aalykke C. Inadvertent yellow fever vaccination of a patient with Crohn’s disease treated with infliximab and methotrexate. BMJ Case Rep. 2016;2016.
Ruddel J, Schleenvoigt BT, Schuler E, Schmidt C, Pletz MW, Stallmach A. Yellow fever vaccination during treatment with infliximab in a patient with ulcerative colitis: a case report. Z Gastroenterol. 2016;54(9):1081–4.
Nash ER, Brand M, Chalkias S. Yellow fever vaccination of a primary vaccinee during adalimumab therapy. J Travel Med. 2015;22(4):279–81.
Oliveira ACV, Mota LMH, Santos-Neto LL, Simoes M, Martins-Filho OA, Tauil PL. Seroconversion in patients with rheumatic diseases treated with immunomodulators or immunosuppressants, who were inadvertently revaccinated against yellow fever. Arthritis Rheumatol. 2015;67(2):582–3.
Scheinberg M, Guedes-Barbosa LS, Mangueira C, Rosseto EA, Mota L, Oliveira AC, et al. Yellow fever revaccination during infliximab therapy. Arthritis Care Res (Hoboken). 2010;62(6):896–8.
Aegerter JP, Christin L, Guyot J, Zellweger J. Bacille Calmette-Guerin injection instead of purified protein derivative injection in an infliximab treated patient. Int J Tuberc Lung Dis. 2016;20(7):990–1.
Toussirot E, Wendling D. Bacillus Calmette-Guerin vaccination in a patient treated with infliximab. J Rheumatol. 2005;32(12):2500–1.
Chioato A, Noseda E, Felix SD, Stevens M, Del Giudice G, Fitoussi S, et al. Influenza and meningococcal vaccinations are effective in healthy subjects treated with the interleukin-1 beta-blocking antibody canakinumab: results of an open-label, parallel group, randomized, single-center study. Clin Vaccine Immunol. 2010;17(12):1952–7.
Jaeger VK, Hoffman HM, van der Poll T, Tilson H, Seibert J, Speziale A, et al. Safety of vaccinations in patients with cryopyrin-associated periodic syndromes: a prospective registry based study. Rheumatology (Oxford). 2017;56(9):1484–91.
Brogan PA, Hofer M, Kuemmerle-Deschner JB, Kone-Paut I, Roesler J, Kallinich T, et al. Rapid and sustained long-term efficacy and safety of canakinumab in patients with cryopyrin-associated periodic syndrome ages five years and younger. Arthritis Rheumatol. 2019;71(11):1955–63.
Kuemmerle-Deschner JB, Hachulla E, Cartwright R, Hawkins PN, Tran TA, Bader-Meunier B, et al. Two-year results from an open-label, multicentre, phase III study evaluating the safety and efficacy of canakinumab in patients with cryopyrin-associated periodic syndrome across different severity phenotypes. Ann Rheum Dis. 2011;70(12):2095–102.
Watanabe M, Nishikomori R, Fujimaki Y, Heike T, Ohara A, Saji T. Live-attenuated vaccines in a cryopyrin-associated periodic syndrome patient receiving canakinumab treatment during infancy. Report No.: 5.
Walker UA, Hoffman HM, Williams R, Kuemmerle-Deschner J, Hawkins PN. Brief report: severe inflammation following vaccination against Streptococcus pneumoniae in patients with cryopyrin-associated periodic syndromes. Arthritis Rheumatol. 2016;68(2):516–20.
Bingham CO, Rizzo W, Kivitz A, Hassanali A, Upmanyu R, Klearman M. Humoral immune response to vaccines in patients with rheumatoid arthritis treated with tocilizumab: results of a randomised controlled trial (VISARA). Ann Rheum Dis. 2015;74(5):818–22.
Tsuru T, Terao K, Murakami M, Matsutani T, Suzaki M, Amamoto T, et al. Immune response to influenza vaccine and pneumococcal polysaccharide vaccine under IL-6 signal inhibition therapy with tocilizumab. Mod Rheumatol. 2014;24(3):511–6.
Mori S, Ueki Y, Akeda Y, Hirakata N, Oribe M, Shiohira Y, et al. Pneumococcal polysaccharide vaccination in rheumatoid arthritis patients receiving tocilizumab therapy. Ann Rheum Dis. 2013;72(8):1362–6.
Mori S, Ueki Y, Hirakata N, Oribe M, Hidaka T, Oishi K. Impact of tocilizumab therapy on antibody response to influenza vaccine in patients with rheumatoid arthritis. Ann Rheum Dis. 2012;71(12):2006–10.
Shinoki T, Hara R, Kaneko U, Miyamae T, Imagawa T, Mori M, et al. Safety and response to influenza vaccine in patients with systemic-onset juvenile idiopathic arthritis receiving tocilizumab. Mod Rheumatol. 2012;22(6):871–6.
Kapetanovic MC, Kristensen L, Saxne T, Aktas T, Morner A, Geborek P. Impact of anti-rheumatic treatment on immunogenicity of pandemic H1N1 influenza vaccine in patients with arthritis. Arthritis Res Ther. 2014;16(1):R2.
Shimizu M, Ueno K, Yachie A. Relapse of systemic juvenile idiopathic arthritis after influenza vaccination in a patient receiving tocilizumab. Clin Vaccine Immunol. 2012;19(10):1700–2.
Uziel Y, Moshe V, Onozo B, Kulcsar A, Trobert-Sipos D, Akikusa JD, et al. Live attenuated MMR/V booster vaccines in children with rheumatic diseases on immunosuppressive therapy are safe: Multicenter, retrospective data collection. Vaccine. 2020;38(9):2198–201.
Toplak N, Avcin T. Long-term safety and efficacy of varicella vaccination in children with juvenile idiopathic arthritis treated with biologic therapy. Vaccine. 2015;33(33):4056–9.
Brodmerkel C, Wadman E, Langley RG, Papp KA, Bourcier M, Poulin Y, et al. Immune response to pneumococcus and tetanus toxoid in patients with moderate-to-severe psoriasis following long-term ustekinumab use. J Drugs Dermatol. 2013;12(10):1122–9.
Doornekamp L, Goetgebuer RL, Schmitz KS, Goeijenbier M, van der Woude CJ, Fouchier R, et al. High immunogenicity to influenza vaccination in Crohn’s disease patients treated with ustekinumab. Vaccines (Basel). 2020;8(3):455.
Chioato A, Noseda E, Stevens M, Gaitatzis N, Kleinschmidt A, Picaud H. Treatment with the interleukin-17A-blocking antibody secukinumab does not interfere with the efficacy of influenza and meningococcal vaccinations in healthy subjects: results of an open-label, parallel-group, randomized single-center study. Clin Vaccine Immunol. 2012;19(10):1597–602.
Richi P, Martin MD, de Ory F, Gutierrez-Larraya R, Casas I, Jimenez-Diaz AM, et al. Secukinumab does not impair the immunogenic response to the influenza vaccine in patients. RMD Open. 2019;5(2):e001018.
Furer V, Zisman D, Kaufman I, Arad U, Berman M, Sarbagil-Maman H, et al. Immunogenicity and safety of vaccination against seasonal influenza vaccine in patients with psoriatic arthritis treated with secukinumab. Vaccine. 2020;38(4):847–51.
Gomez EV, Bishop JL, Jackson K, Muram TM, Phillips D. Response to tetanus and pneumococcal vaccination following administration of ixekizumab in healthy participants. BioDrugs. 2017;31(6):545–54.
Immunisation of individuals with underlying medical conditions: the green book, chapter 7 - GOV.UK (2020) https://www.gov.uk/government/publications/immunisation-of-individuals-with-underlying-medical-conditions-thegreen-book-chapter-7 (accessed August 29, 2022).
Manage Meningococcal Disease Risk in Patients Taking Eculizumab | CDC n.d. https://www.cdc.gov/meningococcal/clinical/eculizumab.html (accessed August 29, 2022).
Meningococcal vaccine: Canadian Immunization Guide - Canada.ca n.d. https://www.canada.ca/en/publichealth/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-13-meningococcal-vaccine.html#p4c12a5c1 (accessed August 29, 2022).
Pittock SJ, Weitz I, Howard JF, Sabatella G, Mehta S, Franklin J. Response to: eculizumab package insert recommendations for meningococcal vaccinations: call for clarity and a targeted approach for use of the drug in neuromyelitis optica spectrum disorder. CNS Spectr. 2020;26(3):195–6.
Alashkar F, Vance C, Herich-Terhurne D, Turki AT, Schmitz C, Bommer M, et al. Serologic response to meningococcal vaccination in patients with cold agglutinin disease (CAD) in the novel era of complement inhibition. Vaccine. 2019;37(44):6682–7.
Alashkar F, Vance C, Herich-Terhurne D, Preising N, Duhrsen U, Roth A. Serologic response to meningococcal vaccination in patients with paroxysmal nocturnal hemoglobinuria (PNH) chronically treated with the terminal complement inhibitor eculizumab. Ann Hematol. 2017;96(4):589–96.
Martinon-Torres F, Bernatowska E, Shcherbina A, Esposito S, Szenborn L, Marti MC, et al. Meningococcal B vaccine immunogenicity in children with defects in complement and splenic function. Pediatrics. 2018;142(3):09.
Gackler A, Kaulfus M, Rohn H, Vogel U, Claus H, Feldkamp T, et al. Failure of first meningococcal vaccination in patients with atypical haemolytic uraemic syndrome treated with eculizumab. Nephrol Dial Transplant. 2020;35(2):298–303.
Mulling N, Rohn H, Vogel U, Claus H, Wilde B, Eisenberger U, et al. Low efficacy of vaccination against serogroup B meningococci in patients with atypical hemolytic uremic syndrome. Biosci Rep. 2020;40(3):BSR20200177.
Langereis JD, van den Broek B, Franssen S, Joosten I, Blijlevens NMA, de Jonge MI, et al. Eculizumab impairs Neisseria meningitidis serogroup B killing in whole blood despite 4CMenB vaccination of PNH patients. Blood Adv. 2020;4(15):3615–20.
Reher D, Fuhrmann V, Kluge S, Nierhaus A. A rare case of septic shock due to Neisseria meningitidis serogroup B infection despite prior vaccination in a young adult with paroxysmal nocturnal haemoglobinuria receiving eculizumab. Vaccine. 2018;36(19):2507–9.
Lebel E, Trahtemberg U, Block C, Zelig O, Elinav H. Post-eculizumab meningococcaemia in vaccinated patients. Clin Microbiol Infect. 2018;24(1):89–90.
Struijk GH, Bouts AHM, Rijkers GT, Kuin EAC, ten Berge IJM, Bemelman FJ. Meningococcal sepsis complicating eculizumab treatment despite prior vaccination. Am J Transplant. 2013;13(3):819–20.
Polat M, Yuksel S, Sahin NU. Fatal meningococcemia due to Neisseria meningitidis serogroup Y in a vaccinated child receiving eculizumab. Hum Vaccin Immunother. 2018;14(11):2802.
Parikh SR, Lucidarme J, Bingham C, Warwicker P, Goodship T, Borrow R, et al. Meningococcal B vaccine failure with a penicillin-resistant strain in a young adult on long-term eculizumab. Pediatrics. 2017;140(3):e20162452.
Nolfi-Donegan D, Konar M, Vianzon V, MacNeil J, Cooper J, Lurie P, et al. Fatal nongroupable Neisseria meningitidis disease in vaccinated patient receiving eculizumab. Emerg Infect Dis. 2018;24(8):08.
Berglund A, Willen L, Grodeberg L, Skattum L, Hagberg H, Pauksens K. The response to vaccination against influenza A(H1N1) 2009, seasonal influenza and Streptococcus pneumoniae in adult outpatients with ongoing treatment for cancer with and without rituximab. Acta Oncol. 2014;53(9):1212–20.
Mulder SF, Jacobs JFM, Olde Nordkamp MAM, Galama JMD, Desar IME, Torensma R, et al. Cancer patients treated with sunitinib or sorafenib have sufficient antibody and cellular immune responses to warrant influenza vaccination. Clin Cancer Res. 2011;17(13):4541–9.
Joona TB, Digkas E, Wennstig A, Nystrom K, Nearchou A, Nilsson C, et al. Influenza vaccination in breast cancer patients during subcutaneous trastuzumab in adjuvant setting. Breast Cancer Res Treat. 2020;184(1):45–52.
Spitaleri G, Delmonte A, Toffalorio F, De Pas TM, Gregorc V. Safety of concomitant administration of seasonal and/or H1N1 flu vaccination in patients receiving erlotinib for advanced non-small cell lung cancer. J Thorac Oncol. 2010;5(5):752–4.
Bettoni da Cunha-Riehm C, Hildebrand V, Nathrath M, Metzler M, Suttorp M. Vaccination with live attenuated vaccines in four children with chronic myeloid leukemia while on imatinib treatment. Front Immunol. 2020;11:628.
Sanada Y, Yakushijin K, Nomura T, Chayahara N, Toyoda M, Minami Y, et al. A prospective study on the efficacy of two-dose influenza vaccinations in cancer patients receiving chemotherapy. Jpn J Clin Oncol. 2016;46(5):448–52.
Douglas AP, Trubiano JA, Barr I, Leung V, Slavin MA, Tam CS. Ibrutinib may impair serological responses to influenza vaccination. Haematologica. 2017;102(10):e397–9.
Sun C, Gao J, Couzens L, Tian X, Farooqui MZ, Eichelberger MC, et al. Seasonal influenza vaccination in patients with chronic lymphocytic leukemia treated with ibrutinib. JAMA Oncol. 2016;2(12):1656–7.
Andrick B, Alwhaibi A, DeRemer DL, Quershi S, Khan R, Bryan LJ, et al. Lack of adequate pneumococcal vaccination response in chronic lymphocytic leukaemia patients receiving ibrutinib. Br J Haematol. 2018;182(5):712–4.
Zhuang W, Wang Y. Analysis of the immunity effects after enhanced hepatitis B vaccination on patients with lymphoma. Leuk Lymphoma. 2020;61(2):357–63.
Mauro FR, Giannarelli D, Galluzzo CM, Vitale C, Visentin A, Riemma C, et al. Response to the conjugate pneumococcal vaccine (PCV13) in patients with chronic lymphocytic leukemia (CLL). Leukemia. 2020;35:737–46.
Winthrop KL, Korman N, Abramovits W, Rottinghaus ST, Tan H, Gardner A, et al. T-cell-mediated immune response to pneumococcal conjugate vaccine (PCV-13) and tetanus toxoid vaccine in patients with moderate-to-severe psoriasis during tofacitinib treatment. J Am Acad Dermatol. 2018;78(6):1149–55.e1.
Winthrop KL, Silverfield J, Racewicz A, Neal J, Lee EB, Hrycaj P, et al. The effect of tofacitinib on pneumococcal and influenza vaccine responses in rheumatoid arthritis. Ann Rheum Dis. 2016;75(4):687–95.
Winthrop KL, Bingham CO, Komocsar WJ, Bradley J, Issa M, Klar R, et al. Evaluation of pneumococcal and tetanus vaccine responses in patients with rheumatoid arthritis receiving baricitinib: results from a long-term extension trial substudy. Arthritis Res Ther. 2019;21(1):102.
Calabrese LH, Abud-Mendoza C, Lindsey SM, Lee S, Tatulych S, Takiya L, et al. Live zoster vaccine in patients with rheumatoid arthritis treated with tofacitinib with or without methotrexate, or adalimumab with methotrexate: a post hoc analysis of data from a phase IIIb/IV randomized study. Arthritis Care Res (Hoboken). 2020;72(3):353–9.
Winthrop KL, Wouters AG, Choy EH, Soma K, Hodge JA, Nduaka CI, et al. The safety and immunogenicity of live zoster vaccination in patients with rheumatoid arthritis before starting tofacitinib: a randomized phase II trial. Arthritis Rheumatol. 2017;69(10):1969–77.
Cordero E, Perez-Ordonez A, Aydillo TA, Torre-Cisneros J, Gavalda J, Lara R, et al. Therapy with m-TOR inhibitors decreases the response to the pandemic influenza A H1N1 vaccine in solid organ transplant recipients. Am J Transplant. 2011;11(10):2205–13.
Bar-Or A, Calkwood JC, Chognot C, Evershed J, Fox EJ, Herman A, et al. Effect of ocrelizumab on vaccine responses in patients with multiple sclerosis: the VELOCE study. Neurology. 2020;95(14):e1999–2008.
Ciotti JR, Valtcheva MV, Cross AH. Effects of MS disease-modifying therapies on responses to vaccinations: a review. Mult Scler Relat Disord. 2020;45:102439.
Nived P, Nagel J, Saxne T, Geborek P, Jonsson G, Skattum L, et al. Immune response to pneumococcal conjugate vaccine in patients with systemic vasculitis receiving standard of care therapy. Vaccine. 2017;35(29):3639–46.
Gorelik M, Elizalde A, Wong Williams K, Gonzalez E, Cole JL. Immunogenicity of sequential 13-valent conjugated and 23-valent unconjugated pneumococcal vaccines in a population of children with lupus. Lupus. 2018;27(14):2228–35.
Oren S, Mandelboim M, Braun-Moscovici Y, Paran D, Ablin J, Litinsky I, et al. Vaccination against influenza in patients with rheumatoid arthritis: the effect of rituximab on the humoral response. Ann Rheum Dis. 2008;67(7):937–41.
van Assen S, Holvast A, Benne CA, Posthumus MD, van Leeuwen MA, Voskuyl AE, et al. Humoral responses after influenza vaccination are severely reduced in patients with rheumatoid arthritis treated with rituximab. Arthritis Rheum. 2010;62(1):75–81.
Bedognetti D, Zoppoli G, Massucco C, Zanardi E, Zupo S, Bruzzone A, et al. Impaired response to influenza vaccine associated with persistent memory B cell depletion in non-Hodgkin’s lymphoma patients treated with rituximab-containing regimens. J Immunol. 2011;186(10):6044–55.
Ide Y, Imamura Y, Ohfuji S, Fukushima W, Ide S, Tsutsumi C, et al. Immunogenicity of a monovalent influenza A(H1N1)pdm09 vaccine in patients with hematological malignancies. Hum Vaccin Immunother. 2014;10(8):2387–94.
Intongkam S, Samakarnthai P, Pakchotanon R, Narongroeknawin P, Assavatanabodee P, Chaiamnuay S. Efficacy and safety of hepatitis B vaccination in rheumatoid arthritis patients receiving disease-modifying antirheumatic drugs and/or biologics therapy. J Clin Rheumatol. 2019;25(8):329–34.
Parrino J, McNeil SA, Lawrence SJ, Kimby E, Pagnoni MF, Stek JE, et al. Safety and immunogenicity of inactivated varicella-zoster virus vaccine in adults with hematologic malignancies receiving treatment with anti-CD20 monoclonal antibodies. Vaccine. 2017;35(14):1764–9.
McCarthy CL, Tuohy O, Compston DAS, Kumararatne DS, Coles AJ, Jones JL. Immune competence after alemtuzumab treatment of multiple sclerosis. Neurology. 2013;81(10):872–6.
Silva M, Humar A, Shapiro AMJ, Senior P, Hoschler K, Baluch A, et al. Humoral immune response following seasonal influenza vaccine in islet transplant recipients. Cell Transplant. 2013;22(3):469–76.
Frerichs KA, Bosman PWC, van Velzen JF, Fraaij PLA, Koopmans MPG, Rimmelzwaan GF, et al. Effect of daratumumab on normal plasma cells, polyclonal immunoglobulin levels, and vaccination responses in extensively pre-treated multiple myeloma patients. Haematologica. 2020;105(6):e302–6.
Chen RI, Deaner JD, Srivastava SK, Lowder CY. Acute retinal necrosis following recombinant subunit varicella-zoster virus vaccine. United States: 2020. Report No.: 20.
Chong CR, Park VJ, Cohen B, Postow MA, Wolchok JD, Kamboj M. Safety of inactivated influenza vaccine in cancer patients receiving immune checkpoint inhibitors. Clin Infect Dis. 2020;70(2):193–9.
Failing JJ, Ho TP, Yadav S, Majithia N, Riaz IB, Shin JY, et al. Safety of influenza vaccine in patients with cancer receiving pembrolizumab. JCO Oncol Pract. 2020;16(7):e573–80.
Wijn DH, Groeneveld GH, Vollaard AM, Muller M, Wallinga J, Gelderblom H, et al. Influenza vaccination in patients with lung cancer receiving anti-programmed death receptor 1 immunotherapy does not induce immune-related adverse events. Eur J Cancer. 2018;104:182–7.
Läubli H, Balmelli C, Kaufmann L, Stanczak M, Syedbasha M, Vogt D, et al. Influenza vaccination of cancer patients during PD-1 blockade induces serological protection but may raise the risk for immune-related adverse events. J Immunother Cancer. 2018;6(1):40.
Yuen C, Kamson D, Soliven B, Kramer C, Goldenberg F, Rezania K. Severe relapse of vaccine-induced Guillain-Barre syndrome after treatment with nivolumab. J Clin Neuromuscul Dis. 2019;20(4):194–9.
Riano I, Cristancho C, Treadwell T. Stevens-Johnson syndrome-like reaction after exposure to pembrolizumab and recombinant zoster vaccine in a patient with metastatic lung cancer. J Investig Med High Impact Case Rep. 2020;(8):2324709620914796.
Lynde C, Krell J, Korman N, Mathes B. Vaccine Study Investigators. Immune response to pneumococcal polysaccharide vaccine in adults with chronic plaque psoriasis treated with alefacept. J Am Acad Dermatol. 2011;65(4):799–806.
Vagberg M, Kumlin U, Svenningsson A. Humoral immune response to influenza vaccine in natalizumab-treated MS patients. Neurol Res. 2012;34(7):730–3.
Metze C, Winkelmann A, Loebermann M, Hecker M, Schweiger B, Reisinger EC, et al. Immunogenicity and predictors of response to a single dose trivalent seasonal influenza vaccine in multiple sclerosis patients receiving disease-modifying therapies. CNS Neurosci Ther. 2019;25(2):245–54.
Olberg HK, Eide GE, Cox RJ, Jul-Larsen A, Lartey SL, Vedeler CA, et al. Antibody response to seasonal influenza vaccination in patients with multiple sclerosis receiving immunomodulatory therapy. Eur J Neurol. 2018;25(3):527–34.
Kaufman M, Pardo G, Rossman H, Sweetser MT, Forrestal F, Duda P. Natalizumab treatment shows no clinically meaningful effects on immunization responses in patients with relapsing-remitting multiple sclerosis. J Neurol Sci. 2014;341(1):22–7.
Krueger JG, Ochs HD, Patel P, Gilkerson E, Guttman-Yassky E, Dummer W. Effect of therapeutic integrin (CD11a) blockade with efalizumab on immune responses to model antigens in humans: results of a randomized, single blind study. J Invest Dermatol. 2008;128(11):2615–24.
Wyant T, Leach T, Sankoh S, Wang Y, Paolino J, Pasetti MF, et al. Vedolizumab affects antibody responses to immunisation selectively in the gastrointestinal tract: randomised controlled trial results. Gut. 2015;64(1):77–83.
Huttner A, Eperon G, Lascano AM, Roth S, Schwob J, Siegrist C, et al. Risk of MS relapse after yellow fever vaccination: a self-controlled case series. Neurol Neuroimmunol Neuroinflamm. 2020;7(4):07.
Miauton A, Tan R, Pantazou V, Du Pasquier R, Genton B. Vaccine-associated measles in a patient treated with natalizumab: a case report. BMC Infect Dis. 2020;20(1):753.
Ufer M, Shakeri-Nejad K, Gardin A, Su Z, Paule I, Marbury TC, et al. Impact of siponimod on vaccination response in a randomized, placebo-controlled study. Neurol Neuroimmunol Neuroinflamm. 2017;4(6):e398.
Winkelmann A, Metze C, Frimmel S, Reisinger EC, Zettl UK, Loebermann M. Tick-borne encephalitis vaccination in multiple sclerosis: a prospective, multicenter study. Neurol Neuroimmunol Neuroinflamm. 2020;7(2):01.
Signoriello E, Bonavita S, Sinisi L, Russo CV, Maniscalco GT, Casertano S, et al. Is antibody titer useful to verify the immunization after VZV vaccine in MS patients treated with fingolimod? A case series. Netherlands: 2020. Report No.: 40.
Issa NP, Hentati A. VZV encephalitis that developed in an immunized patient during fingolimod therapy. Neurology. 2015;84(1):99–100.
Pandit A, Leblebjian H, Hammond SP, Laubach JP, Richardson PG, Baden LR, et al. Safety of live-attenuated measles-mumps-rubella and herpes zoster vaccination in multiple myeloma patients on maintenance lenalidomide or bortezomib after autologous hematopoietic cell transplantation. Bone Marrow Transplant. 2018;53(7):942–5.
Stoma I, Karpov I, Iskrov I, Lendina I, Uss A. Clinical efficacy of pneumococcal vaccination in multiple myeloma patients on novel agents: results of a prospective clinical study. Vaccine. 2020;38(30):4713–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sonpar, A. (2022). Safety and Efficacy of Vaccines in Patients on Targeted and Biologic Therapies. In: Cervera, C., Aguado, J.M. (eds) Infectious Complications in Biologic and Targeted Therapies. Springer, Cham. https://doi.org/10.1007/978-3-031-11363-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-11363-5_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-11362-8
Online ISBN: 978-3-031-11363-5
eBook Packages: MedicineMedicine (R0)