Abstract
Since its origins, medicine has been more linked to the cure of diseases than to their prevention. This is due to multiple factors, training of health professionals aimed at curing diseases, lack of quality data, processing capacity, poor multidisciplinary approach, etc. However, this paradigm is changing, focusing on maintaining the health of individuals to avoid diseases, improving social welfare. To achieve this, the new approach proposes that medicine must be Preventive, Participatory, Predictive, and Personalized (P4 Medicine). In this chapter, we will analyze how artificial intelligence can convincingly contribute to the construction of P4 Medicine, through the processing of key data such as DNA, electronic medical records and environmental variables to which people have been exposed. Here we can find complex data such as Computed Tomography images, electroencephalograms, free text in electronic medical records, pharmacological data, etc. These data have grown exponentially and efforts to improve their quality are already paying off. However, it is no longer possible for a health professional to analyze them to provide a better diagnosis or carry out preventive work on diseases, requiring the formation of multidisciplinary teams to find new solutions to ancient problems, such as healthcare, where data processing, knowledge extraction and its subsequent parameterization in support systems for medical decision-making are vital to save lives. In this sense, artificial intelligence, together with new methods for processing complex data and computational resources to process massive data, will be key to improving the humanity health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1.1 Introduction
Artificial Intelligence (AI) is perhaps the greatest technological revolution of the 21st century. Its beginnings can be placed in the late 50s, when the famous English mathematician Alan Turing began to wonder what conditions are needed to consider a machine as intelligent. His ideas were reflected in his seminal article “Computing Machinery and Intelligence” [1]. However, the main concept was coined in 1956 by John McCarthy in the Dartmouth Summer Research Project on Artificial Intelligence [2], defining AI as “the science and engineering of making intelligent machines, especially intelligent computer programs”. Currently, practically no technological development escapes the use or influence of AI. We can find it in everyday situations such as the coffee machine that prepares us a cappuccino or sophisticated ones such as those that allow us to calculate the most optimal path so that an emergency vehicle (ambulance, fire truck, etc.) finds the optimal route to save lives or even very complex ones like a robot performing a complex surgery on a patient with a critical heart condition. In that sense, the IA has two main branches: virtual and physical. The first one is related with the informatics approaches where the algorithms are used for creating complex computer systems. The second one is close to robotics, where the algorithms are used to give the correct movement to the physic parts of a devices to perform an specific task.
But, what is intelligence? A very simple question with a no simple answer. In fact, we don’t have a general agreement on the definition of intelligence, but some good approaches have been presented during the last century, such as the capacity to give good answers from the point of view of truth or facts [3], the ability to continue an abstract thinking [4], the combination of abilities necessaries to survive in a particular culture [5], the ability to solve problems, to create products valued based on cultural settings [6] and from Random House Unabridged Dictionary (2006), the “capacity for learning, reasoning, understanding, and similar forms of mental activity; aptitude in grasping truths, relationships, facts, meanings, etc.”. It seems the learning capacity is an important issue when we try to explain what intelligence is.
Can a machine be intelligent as a human being? For now and hopefully for the future, the answer is no. But a very good approach is to give the machines the capacity of learning from data originated in a source, for example environmental data for a good prediction about future conditions. In that sense, if during the learning process the machine gets enough capacity to predict future scenarios, and making good predictions for taking correct decisions, we will be in front of an intelligent machine. But the reasoning and understanding capacities are not present in that machine.
For creating an intelligent machine, the learning process is essential because it is where the machine can identify patterns from the data and define rules on how to use them to make its best prediction regarding a future situation. However, data is not always required to make a machine perform tasks as an intelligent being would. Who has not ever played chess with the computer? Normally chess programming is based on rules of piece movements, being unnecessary data regarding the moves of other players. But these rules intrinsically contain a series of patterns that the programmer has programmed into algorithms. Clearly, the algorithm that represents the cybernetic player can be improved by finding new patterns that the programmer never imagined. This is where once again the massive processing of data from other players’ plays becomes extremely relevant. Indeed, the algorithm that represents the cybernetic player can be continuously improved until it reaches the point where it learns from patterns of so many plays that it practically covers a large part of the universe of possibilities that a human player would have, making the machine beat the man, which has already happened, but it has not been a process of reasoning, but rather of processing capacity.
There is no doubt that the applications developed and to be developed based on AI are beyond any prediction that we can make at the moment. However, it is practically an assumed fact that the world we know is undergoing dizzying changes where AI in many cases has taken a leading role. This is how in healthcare and in medicine in general, the next step in its development cannot be taken without the support of AI.
Since immemorial time, medicine has been focused on the cure of diseases and ailments of all kinds of patients [7], who have in common that symptoms have first manifested before decisions can be made, which in many cases may arrive late. However, the focus is changing, where the maintenance of healthy begins to to be relevant. Indeed, medicine is moving from a reactive to a proactive discipline being participatory, predictive, personalized and preventive P4 medicine [8]. The foregoing will be possible to the extent that we can obtain information and knowledge of the data related to the health of patients, in particular their DNA, electronic medical records and the environment in which they have lived, among other data. This is a huge challenge, starting with the maintenance and consolidation of data that ensures secure access for study purposes and of course to help patients with their ailments. Followed by the data storage and processing capacity for the extraction of patterns that help all health personnel in tasks such as diagnosis, treatment, medication, etc. And finally, to provide adequate help to both the patient and the health personnel to achieve the primary objective that goes beyond the cure of the disease, we refer to the maintenance of good health in the population. Given this scenario, artificial intelligence is playing a key role in massive data processing that allows the creation of countless applications, which cover practically all branches of medicine, such as radiology, nephrology, nutrition, psychiatry, neurology, etc. [9].
This chapter is organized as follow. Section 1.2 introduces the process about how the machines learn. In Sect. 1.3, the possible applications of artificial intelligence in medicine is shown. A short review about papers related with P4 medicine is developed in Sect. 1.4. And finally, as chapter’s summary, some reflections on the current and future potential of the application of artificial intelligence in medicine are shown.
1.2 How Do Machines Learn?
How do we human beings learn? through examples which are reflected in our neural network that then allow us to analyze sounds, images, movements, structures, tastes, etc. In this sense, the automatic learning of a machine is very similar, that is, many examples are needed so that the machine can extract patterns from the data that then allows it to extrapolate a future decision. When they receive data that did not belong to the set of examples as input and for which you are looking for an output, it will give you the best prediction based on what it had learnt before [10].
According to [11] an algorithm is capable to learn when given a task, training experience, and a performance measure, so its achievement on the task improves with experience. Based on experiences learned, the algorithms can take decisions, make predictions, classify objects, predict cancer in a patient, give directions to the robots, recognize the human voice, and a huge set the possible uses and applications. In this context, the data play a central role in achieving a correct training of the algorithms. In other words, if the data are not clean and consolidated, the training of the algorithm will be affected and its learning capacity will be reduced, which will affect all the uses described above, making it impossible to create applications.
Machine learning is the concept that groups the set of algorithms that are capable of learning from the data. It was defined by Arthur L. Samuel as a “field of study that gives computers the ability to learn without being explicitly programmed” [12]. Depending of type of data and the algorithm to use, the learning process can be classified in supervised, unsupervised, reinforcement [13], and deep learning [14].
In supervised learning, a set of training data is created where the input and output vector are known. Then the algorithm learns the associations between inputs and outputs to create a mathematical model, which is validated and tested with real data before it can be used. A different situation happens in unsupervised learning where the algorithm learns the associations in the training data but the output is unknown, identifying undiscovered patterns. In reinforcement learning the algorithm learns a behaviour through trial-and-error to maximize a defined reward. Finally, deep learning allow to process big amount of raw data to extract patterns for detection or classification of issues.
1.2.1 Machine Learning Process
Giving a collection of data we are trying to extract patterns and rules about how to use them. The basic assumption is that the data was not created randomly, i.e., there are intrinsic relationships among them, for example regularities, which can then be detected and represented as patterns that allow a machine learning algorithm to be trained. In other words, if the data are dirty, their dispersion is high or there are no possible relationships among them, then there will be no machine learning algorithm able to create an analysis, predict, classify, or model the phenomenon under study. In that sense, statistical techniques are used to analyze the quality of the data and make prospects of its possible uses in a training process of a machine learning algorithm [15].
Figure 1.1 shows a conceptual diagram about the machine learning algorithms, where the deep learning one is part of the artificial neural network family. Depending on the kind of data to be processed and the phenomenon under study to be modeled, is the machine learning algorithms to use.
Machine learning algorithms, concepts and classes, based on [14]
Figure 1.2 shows the general learning process for machine learning algorithms focused in supervised learning. From a set of row data, the target data, i.e. the data to be considered to analyze the phenomenon under study, are selected. Next, a feature vector transformation process is developed. The feature vectors set is divided in three parts: training, validation, and testing. The training data are used to train the model by applying a selected machine learning algorithm. Then the model is validated to check if there are problems of overfitting/underfitting. And finally, testing is applied to get some effectiveness measure such as accuracy. After the whole process, the model is put into production, being useful for taking decisions.
1.2.2 Machine Learning in Medicine
Considering the current amount of data related to people’s health, and that its future growth will be exponential, it is no longer possible by using traditional methods of extracting information and knowledge, fundamentally manual, can obtain any benefit from these data [16]. In this way that machine learning algorithms have become the new way of processing large volumes of data, in many cases complex and multivariable, and in particular medical data [17].
Machine learning algorithms and a subset of them, like deep learning, allow to create a computational model to process medical data for getting novel patterns from raw data, for instance, digitized X-ray images of a human chest to detect if the patient has pneumonia or COVID-19 [18]. The learning model is trained by using a set of learning techniques, in this case an object detection technique to predict if a new chest X-ray image is classify as normal, pneumonia, or COVID-19.
Medical data are available in an enormous variety of types and sources, which include diseases, public health data, prognosis, diagnosis, images, time series, etc., and everything indicates that its growth will continue to be exponential, as more and better sensor devices are added to medical exams [19]. Almost by construction, medical data are complex to analyze, even when there are very few records to analyze a disease, the mere fact that these records have high dimentionality makes them a challenge in machine learning. Additionally, in many cases it is not entirely clear what methods have been used to ensure the quality of medical data, which directly influences the predictive quality of the model to be trained [20].
There is no doubt that the applications of machine learning, and deep learning in particular, in medicine are enormous and will continue to expand in the incoming years. In [17] presents a study on the use of machine learning in medical research in recent years. From there it follows that the most used algorithms have been Random Forrest, Decision Tree, Support Vector Machine, Naïve Bayes, Artificial Neural Networks, and clustering techniques. Especial attention with Deep Learning algorithms, used in an important set of papers, in particular Convolutional neural network (CNN) for medical imagine processing [21].
1.3 Artificial Intelligence in Medicine
During the last decade, Artificial Intelligence research has grown exponentially in projects related to medicine. Indeed only in 2016, AI projects related to medicine attracted much more investment than AI projects related to other sectors of the global economy [22, 23]. What factors explain this heightened growth and interest?, among the reasons we can find is the great capacity of AI to improve the efficiency and effectiveness of healthcare delivery. AI in medicine aims to optimize clinical decision-making by using data related with health to provide information and patterns for improving the healthcare of the individuals.
Then, what AI algorithms can do for the future of medicine? It is an inescapable fact that in the developed world, the amount of data related to each person’s health is growing by leaps and bounds. Also that the reality of the quality and consolidation of these data in many countries is doubtful. However, steps are being taken in the right direction to achieve the digitalization of computer systems related to electronic medical data, continuous improvement in data quality, interoperability of systems, and security protocols that guarantee that the access, processing, and use of the data will be carried out in accordance with the law [24]. In this context, there is only one question: what do we do with medical data? This is where AI plays a central role. With the avalanche of data that health information systems are producing day by day, the number of exams that patients must perform, DNA analyzes that are less expensive every day, and the data provided by the patients themselves through applications for Smartphones or other devices, the possibility of a human being able to analyze all this is simply impossible, which is why advanced mechanisms are required in data processing and in the presentation of information and patterns for making relevant clinical decisions.
Consider the following situation. A person suffers from a severe headache and tells a friend about his ailment. Immediately the friend takes out a medicine that he carries in his backpack that a doctor diagnosed him with years ago and that has always helped him with his headaches. Immediately afterwards, he gives a pill to his friend so that he can make the strong pain that he is suffering disappear. Several questions immediately arise: (1) if they are different persons, why give them the same drug? (2) does the friend know the person’s medical history?; (3) The dose delivered is correct?; (4) Will there be any contraindications? And we could continue asking questions, but the fact is that the advisable thing would be that if they are different persons, the treatment at least would not have to be the same. This is the essence of precision medicine that is the basis of the medicine of the future. Precision medicine, sometimes called personalized medicine is defined by the National Institute of Health (NIH) precision medicine as “refers to a new treatment and prevention method based on understanding of individual gene, environment and life-style” [25]. And to achieve this, information and knowledge extracted from quality data per individual are required, considering their medical history, DNA, environment, and lifestyle.
Figure 1.3 shows the integration of several data sources related with the patients, and the respective data processing by using artificial intelligence tools, machine learning algorithms and deep learning algorithms. The outcome aims to provide information, patterns, knowledge, etc, to improve the decision-making for different users, such as healthcare professionals and patients.
In Fig. 1.3, the collection of data presented is only a part of the data that are related to the life and healthcare of people. Among these data we also find those from online social networks [26] and those provided by people through smartphone applications related to healthcare [27]. Clearly, the more quality data that can be collected from an individual, the better the diagnosis to cure a disease or the advice to maintain their health, making the patient central in their healthcare. However, such amount of data cannot be processed directly by human beings, so a large data processing capacity is needed together with advanced algorithms for the extraction of information, patterns, and knowledge. The final result points to multiple users, starting with the patient, being able to make correct use of this new knowledge, which is key in healthcare.
There is no doubt that AI is causing a great positive revolution in terms of people’s healthcare. However, not everything is a rose garden. As it is sensitive personal data, its processing must be carried out under strict security measures and ethical considerations [28]. Indeed, what would happen when analyzing the DNA data of an individual, it is detected that she/he has a high probability of developing diabetes in the future, will this be a prevalence? will health insurance cover this disease? will the individual suffer some kind of discrimination? We must not forget that the use of AI in healthcare is to help people in an ethical and responsible manner [29], taking care that their personal data is not used for purposes other than to support health maintenance or cure the disease that affects an individual. In no way can they be used for other purposes that violate the fundamental human rights [30].
1.4 AI Applications in Medicine
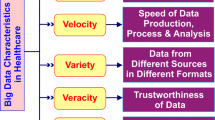
As mentioned above, the development of high-throughput, data-intensive research assays, and technologies in medicine has created a need for researchers to develop strategies to analyze, integrate, and interpret the massive amounts of data they generate. Traditional approaches do not allow working with ’big data’, which presents the opportunity to improve people’s health, so the use of AI techniques suggest that they could be particularly appropriate. In addition, the results of the application of medical exams reveal a great heterogeneity in the pathophysiological factors and processes that contribute to a disease, suggesting that there is a need to adapt or ’customize’ the medicines to the nuanced characteristics and, often, unique to individual patients [31].
P4 Medicine represents the foundations of a model of clinical medicine, which offers the opportunity to modify the healthcare paradigm: the participation of the individual is essential to put into practice the other three aspects of P4 Medicine with each patient [32].
In Fig. 1.4 a summary about the P4 Medicine is shown. The future of health services focuses on giving people a complete picture of the many factors that affect their health. Personalized medicine proposes the integration of numerous biological data points, including molecular, cellular, and phenotypic longitudinal measurements, as well as individual genome sequences, to better define the health or well-being of each person, predict transitions to disease and guide medical interventions [33,34,35]. The implementation of the P4 from the clinical point of view will create predictive and personalized models that represent the well-being of each patient or of a disease, which will allow the design of new pharmacological tests that take into account the heterogeneity of responses to therapies and disease stratification [36].
Summary scheme of the definitions and components of the 4Ps of medicine: predictive, preventive, personalized, and participatory. Own elaboration based on [37]
1.4.1 Predictive Medicine
Predictive medicine is a branch of medicine that aims to identify patients at risk of developing a disease, allowing for early prevention or treatment of that disease. Single or more commonly multiple assays are used to identify markers of future disease disposition [38].
The goal of predictive medicine is to obtain and catalog the characteristics of individual patients, analyze that data to predict an individual patient’s risk for an outcome of interest, predict which treatment in which individual will be most effective, and then intervene before the event occurs. However, previously limited to the realm of genetics, genetics-based risk prediction has been of limited benefit because whole genome sequencing is still relatively expensive, and most diseases affecting today’s population depend on different variables [39]. These are not only influenced by genetics but also by demographic, psychosocial data, eating habits, stress levels, etc. Therefore, the need arises to collect and organize different types of data to perform a more complete analysis of people.
In recent years, machine learning algorithms such as deep learning that can account for complex interactions among features is shown to be promising in predictive modeling in healthcare [40]. Artificial intelligence can help doctors make better clinical decisions. Algorithms can unlock clinically relevant information hidden in the vast volume of healthcare data guided by clinically relevant questions asked by healthcare professionals. In clinical trials of most medical studies, specific hypotheses or questions are clearly defined, and algorithms are trained to predict certain outcomes, given that a set of features and insights can be developed through prediction [41].
Artificial intelligence is used in many different health conditions and healthcare applications, for example, to assess the readmission of patients to hospitals [42], to detect patients who will suffer adverse effects when taking medications [43], in chronic diseases such as diabetes [44] and hypertension [45]; just to name a few. Table 1.1 presents some research that has applied artificial intelligence in predictive medicine.
1.4.2 Participatory Medicine
Participatory medicine focuses on the patient, in order to empower people to make more informed decisions related to their health, where the individual/patient is at the center of any related health care initiative [61]. In recent times, the role of patients in managing their own health has been changing [62]. People have gone from being mere observers to more active, committed and empowered actors in the decision-making process shared with the health team [63, 64]. For example, vaccination is strictly participatory since the individual is responsible for administering it, including that of children. This issue has become highly relevant due to the pandemic, and the multiple recently developed COVID-19 vaccines, given their differences in composition, timing of administration, effectiveness, and potential adverse events [65].
AI applied to participatory health involves individuals and their representatives, who would be the main beneficiaries of this technology [66, 67]. People can collect, record, and track indicators to quantify their health, providing insights into their overall health status [68], giving AI the opportunity to further understand their health.Continuing with the example in the pandemic context, thanks to AI, surveillance, monitoring of close contacts, compliance with quarantines, and the reduction of workload for health teams have been facilitated. Along with this, mobile technology has been harnessed to collect data on the symptoms reported by individuals combined with other data from different sources to obtain information on the disease and the spread of infection, contributing to knowledge about the prevalence and transmission of asymptomatic COVID-19 [69]. Images from security cameras, facial recognition, bank card records, and GPS data from vehicles and mobile phones have also been used to closely monitor possible contacts between infected people. In this way, data on the location and movements of people were collected to alert neighbors/patients to new cases.
AI applications within participatory health have been evaluated in the context of a wide variety of health conditions, health promotion activities, and healthcare settings through: social media, mobile apps, chatbots, health records, questionnaires, and open collaborative health studies [64, 67]. Each allows for the generation, production, or collection of various types of data, reflecting various facets of health, including psychological, physical, social, physiological, or cognitive indicators.
Tables 1.2 and 1.3 present the tools that have been used to apply AI in participatory medicine: papers that work with social networks and research where different devices and applications are used.
1.4.3 Personalized Medicine
Personalized medicine is the tailoring of therapies to defined subsets of patients based on their likelihood to respond to therapy or their risk of adverse events [85]. It uses an individual’s genetic profile to guide decisions about disease prevention, diagnosis, and treatment. Knowing a patient’s genetic profile can help clinicians select the appropriate drug or treatment and administer it at the appropriate dose or regimen [86].
Personalized medicine has the potential to tailor therapy with the best response and the largest safety margin to ensure better patient care. By enabling every patient to receive early diagnosis, risk assessment and optimal treatment, it promises to improve care while lowering costs [87].
The focus of personalized medicine is on identifying which approaches will be effective for which patients based on genetic, environmental, and lifestyle factors. If information is collected from different sources for the same individual, a specific profile of the subject can be established, in which the sensitivity to certain risk factors can be accurately determined, and with this, appropriate measures can be taken to reduce the risk of developing the disease. Furthermore, risk assessment can benefit from precision medicine by generating estimates that lead to evidence-based recommendations for different outcomes [88], including historical data [89]. In addition, precision medicine’s focus on the individual will lead to accumulating evidence of multiple exposures and thus characterizing the body’s short- and long-term response to changes that occur, exposures to environmental factors, and occupational agents [88].
The use of Artificial Intelligence techniques applied to personalized medicine can contribute to the detection or prediction of diseases, achievement of accurate diagnosis, and optimal treatment. Some examples are based on personalized diagnosis and treatment based on Cardiac Imaging [90], applications of artificial intelligence in early detection of cancer [91] (such as automatic classification of cancer based on images [92] and on genes [33]), computer-aided detection and computer-aided diagnosis of colorectal polyps [93], and automatic health-record heart failure with preserved ejection fraction patient phenotyping [33]. Finally, it is highlighted that in recent times, the pandemic prompted the execution of research in personalized medicine applied in the timely diagnosis of COVID-19, in order to be able to deal with the disease, from containing the spread of the virus to the correct treatment of patients [34].
Table 1.4 presents some studies that focus on the use of artificial intelligence to support personalized medicine.
1.4.4 Preventive Medicine
Due to rising health care costs, early disease prevention has never been more important than it is today. Given the above, the concept of preventive medicine is strengthened, which is based on Medical practices that are designed to avert and avoid disease[108].
Digital health announces that thanks to technological progress embodied in applications, wearable technology, remote monitoring, telemedicine, and communication tools, among other diagnostic devices; the quality of patient care will be optimized, as well as a more timely response to any situation. This occurs because these tools make data available, which are extracted and used for the detection, prediction, and support for diagnosis/decision making of anomalies [109].
AI-driven health interventions fall into four categories relevant to global health researchers: (1) diagnosis, (2) patient morbidity or mortality risk assessment, (3) disease outbreak prediction and surveillance, and (4) health policy and planning [110]. Through the use of AI, huge amounts of data derived from different sources can be interpreted to facilitate diagnosis and increase the ability to execute early initiatives and prevent diseases to reduce the burden on both the patient and caregivers. Then executing successful interventions depends on the knowledge of the causes of the disease, the transmission dynamics, the identification of risk factors and groups, the methods of early detection and treatment, the implementation of these methods and the continuous evaluation and development of the methods. prevention methods and treatment. The identification of the determinants of a disease at the population level is a prerequisite, to prevent its appearance in a single individual, providing the basis for targeted and specific treatment [109].
The application of AI in disease prevention has been carried out in the evaluation of breast cancer risk [111], heart disease diagnosis [112], early prognosis in patients with liver disorders [113], prediction of admissions, complications and mortality in ICUs [114], and the prognosis of severity and outcome of cerebrovascular accidents [115], among others.
Table 1.5 shows a summary of some research that applies Machine Learning and Deep Learning algorithms in the field of preventive medicine.
1.5 Summary
People’s healthcare is changing, going from being a task focused on curing diseases to one based on preserving health, through various methods that anticipate possible illnesses, treatments to maintain indicators of internal biology of the human body within certain margins and of course, considering that people are the center of any initiative regarding healthcare. Hence, the adequate collection of quality data related to people’s lives and health is very important. For several years, enormous efforts have been made to improve the processes of capturing and storing data related to health, its subsequent maintenance, transmission, and exploitation. However, despite all these efforts, in many places there is still no unified electronic medical record, which is essential to apply the concepts behind 4P medicine. But it is a matter of time before the situation gradually improves. For now, efforts have been focused on using the data related to people’s health in the best possible way to create various applications and systems that are aimed at gradually improving population’s health. Considering this scenario and the inescapable fact that health-related data only grows in complexity and size, it is essential to have automated tools for its processing to extract information and knowledge to support decision-making in the field of healthcare. This is where artificial intelligence plays an essential role, enabling massive data processing, process automation, timely delivery of information and knowledge and, of course, support for diagnosis. We are at the gates of a new medicine, much more participatory, predictive, preventive and personalized, where the joint work between health personnel and artificial intelligence is bearing increasingly significant fruits. But remember, with all this tremendous technological power comes great responsibility. The processing of data related to people’s health must be carried out in a safe, responsible and, above all, ethical manner, taking care to safeguard the human rights of individuals above all else. Only in this way can the benefits of AI be accessed in the field of healthcare.
References
Turing, A. Computing machinery and intelligence. Mind (1950)
McCarthy, J., Minsky, M.L., Rochester, N., Shannon, C.E.: A proposal for the Dartmouth summer research project on artificial intelligence, 31 Aug 1955. AI Mag. 27(4), 12–12 (2006)
Thorndike, E.I.: Intelligence and its measurement: a symposium–i. J. Educ. Psychol. 12(3), 124 (1921)
Terman, L.M.: Intelligence and its measurement: a symposium–ii. J. Educ. Psychol. 12(3), 127 (1921)
Anastasi, A.: What counselors should know about the use and interpretation of psychological tests. J. Counsel. Dev. 70(5), 610–615 (1992)
Gardner, H.: Frames of mind: theory of multiple intelligences. Fontana Press (1993)
Subbarayappa, B.V.: The roots of ancient medicine: an historical outline. J. Biosci. Bangalore 26(2), 135–143 (2001)
Hood, L., Friend, S.H.: Predictive, personalized, preventive, participatory (p4) cancer medicine. Nat. Rev. Clin. Oncol. 8(3), 184–187 (2011)
Koteluk, O., Wartecki, A., Mazurek, S., Kołodziejczak, I., Mackiewicz, A.: How do machines learn? artificial intelligence as a new era in medicine. J. Person. Med. 11(1), 32 (2021)
Thrun, S., Pratt, L. Learning to Learn. Springer (2012)
Mitchell, T.: Learning to Learn. McGraw-Hill (1997)
Samuel, A.L.: Machine learning. Technol. Rev. 62(1), 42–45 (1959)
Ray, S.: A quick review of machine learning algorithms. In 2019 International Conference on Machine Learning, Big Data, Cloud and Parallel Computing (COMITCon), pp. 35–39. IEEE (2019)
Janiesch, C., Zschech, P., Heinrich, K.: Machine learning and deep learning. Electron. Markets 31(3), 685–695 (2021)
Gudivada, V., Apon, A., Ding, J.: Data quality considerations for big data and machine learning: going beyond data cleaning and transformations. Int. J. Adv. Softw. 10(1), 1–20 (2017)
Awaysheh, A., Wilcke, J., Elvinger, F., Rees, L., Fan, W., Zimmerman, K.I.: Review of medical decision support and machine-learning methods. Veterinary Pathol. 56(4), 512–525 (2019)
Garg, A., Mago, V.: Role of machine learning in medical research: a survey. Comput. Sci. Rev. 40, 100370 (2021)
Das, S., Roy, S.D., Malakar, S., Velásquez, J.D., Sarkar, R.: Bi-level prediction model for screening covid-19 patients using chest X-ray images. Big Data Res. 25, 100233 (2021)
Tao, X., Velásquez, J.D.: Multi-source information fusion for smart health with artificial intelligence. Inf. Fusion 83–84, 93–95 (2022)
Lee, C.H., Yoon, H.-J.: Medical big data: promise and challenges. Kidney Res. Clin. Practice 36(1), 3 (2017)
Garain, A., Basu, A., Giampaolo, F., Velasquez, J.D., Sarkar, R.: Detection of covid-19 from CT scan images: a spiking neural network-based approach. Neural Comput. Appl. 33(19), 12591–12604 (2021)
Buch, V.H., Ahmed, I., Maruthappu, M.: Artificial intelligence in medicine: current trends and future possibilities. Bri. J. General Practice 68(668), 143–144 (2018)
CB Insights Research: Healthcare remains the hottest AIcategory for deals (2017)
Chan, K.S., Fowles, J.B., Weiner, J.P.: Electronic health records and the reliability and validity of quality measures: a review of the literature. Med. Care Res. Rev. 67(5), 503–527 (2010)
Wang, Z.-G., Zhang, L., Zhao, W.-J.: Definition and application of precision medicine. Chin. J. Traumatol. 19(05), 249–250 (2016)
Flavia Guinazu, M., Cortes, V., Ibanez, C.F., Velasquez, J.D.: Employing online social networks in precision-medicine approach using information fusion predictive model to improve substance use surveillance: a lesson from twitter and marijuana consumption. Inf. Fusion 55, 150–163 (2020)
González, F., Vera, F., González, F., Velásquez, J.D.: Kefuri: a novel technological tool for increasing organ donation in Chile. In: 2020 IEEE/WIC/ACM International Joint Conference on Web Intelligence and Intelligent Agent Technology (WI-IAT), pp. 470–475. IEEE (2020)
Knoppers, B.M., Thorogood, A.M.: Ethics and big data in health. Curr. Opin. Syst. Biol4, 53–57 (2017)
Morley, J., Machado, C.C.V., Burr, C., Cowls, J., Joshi, I., Taddeo, M., Floridi, L.: The ethics of AI in health care: a mapping review. Soc. Sci. Med. 260, 113172 (2020)
Mann, J.M., Gostin, L.O., Gruskin, S., Brennan, T., Lazzarini, Z., Fineberg, H.V.: Health and human rights. In: Health and Human Rights in a Changing World, pp. 16–31. Routledge (2013)
Douali, N., Jaulent, M.-C.: Genomic and personalized medicine decision support system. In: 2012 IEEE International Conference on Complex Systems (ICCS), pp. 1–4 (2012)
Hood, L., Flores, M.: A personal view on systems medicine and the emergence of proactive p4 medicine: predictive, preventive, personalized and participatory. New Biotechnol. 29(6), 613–624 (2012)
Gifari, M.W., Samodro, P., Kurniawan, D.W.: Artificial intelligence toward personalized medicine. Pharmaceut. Sci. Res. 8(2), 1 (2021)
Lin B., Wu, S.: Digital transformation in personalized medicine with artificial intelligence and the internet of medical things. Omics: J. Integr. Biol. 26(2), 77–81 (2022)
Zellweger, M.J., Tsirkin, A., Vasilchenko, V., Failer, M., Dressel, A., Kleber, M.E., Ruff, P., März, W.: A new non-invasive diagnostic tool in coronary artery disease: artificial intelligence as an essential element of predictive, preventive, and personalized medicine. EPMA J. 9(3), 235–247 (2018)
Flores, M., Glusman, G., Brogaard, K., Price, N.D., Hood, L.: P4 medicine: how systems medicine will transform the healthcare sector and society. Pers. Med. 10(6), 565–576 (2013)
Doherty, T.M., Di Pasquale,A., Michel, J.-P., Del Giudice, G.: Precision medicine and vaccination of older adults: from reactive to proactive (a mini-review). Gerontology 66(3), 238–248
Taylor, C.A., Draney, M.T., Ku, J.P., Parker, D., Steele, B.N., Wang, K., Zarins, C.K.: Predictive medicine: computational techniques in therapeutic decision-making. Comput. Aided Surgery: Off. J. Int. Soc. Comput. Aided Surgery (ISCAS) 4(5), 231–247 (1999)
Jen, M.Y., Shahrokhi, M., Varacallo, M.: Predictive medicine. In: StatPearls. StatPearls Publishing, Treasure Island (FL) (2022)
Deo, R.C.: Machine learning in medicine. Circulation 132(20), 1920–1930 (2015)
Yang, Christopher C.: Explainable artificial intelligence for predictive modeling in healthcare. J. Healthcare Inform. Res. 6(2), 228–239 (2022)
Xue, Y., Klabjan, D., Luo, Y.: Predicting ICU readmission using grouped physiological and medication trends. Artif. Intell. Med. 95, 27–37 (2019)
Yang, H., Yang, C.C.: Using health-consumer-contributed data to detect adverse drug reactions by association mining with temporal analysis. ACM Trans. Intell. Syst. Technol. 6(4), 1–55 (2015)
Krieg, S.J., Robertson, D.H., Pradhan, M.P., Chawla, N.V.: Higher-order networks of diabetes comorbidities: disease trajectories that matter. In: 2020 IEEE International Conference on Healthcare Informatics (ICHI), pp. 1–11 (2020)
Martinez-Ríos, E., Montesinos, L., Alfaro-Ponce, M., Pecchia, L.: A review of machine learning in hypertension detection and blood pressure estimation based on clinical and physiological data. Biomed. Signal Process. Control 68, 102813 (2021)
Goh, K.H., Wang, L., Kwang Yeow, A.Y., Poh, H., Li, K., Lin Yeow, J.J., Heng Tan, GY.: Artificial intelligence in sepsis early prediction and diagnosis using unstructured data in healthcare. Nature Commun. 12(1), 1–10 (2021)
D’Haese, P.-F., Finomore, V., Lesnik, D., Kornhauser, L., Schaefer, T., Konrad, P.E., Hodder, S., Marsh, C., Rezai, A.R.: Prediction of viral symptoms using wearable technology and artificial intelligence: a pilot study in healthcare workers. PLOS ONE 16(10), e0257997 (2021) (Public Library of Science)
Elujide, I., Fashoto, S.G., Fashoto, B., Mbunge, E., Folorunso, S.O., Olamijuwon, J.O.: Application of deep and machine learning techniques for multi-label classification performance on psychotic disorder diseases. Inf. Med. Unlocked 23, 100545 (2021)
Noor, S.T., Asad, S.T., Khan, M.M., Gaba, G.S., Al-Amri, J.F., Masud, M.: Predicting the risk of depression based on ECG using RNN. Comput. Intell. Neurosci. (2021)
Vijayalaxmi, A., Sridevi, S., Sridhar, N., Ambesange, S.: Multi-disease prediction with artificial intelligence from core health parameters measured through non-invasive technique. In: 2020 4th International Conference on Intelligent Computing and Control Systems (ICICCS), pp. 1252–1258. IEEE (2020)
Lauritsen, S.M., Kristensen, M., Olsen,M.V., Larsen, M.S., Lauritsen, K.M., Jørgensen, M.J., Lange, J., Thiesson, B.: Explainable artificial intelligence model to predict acute critical illness from electronic health records. Nat. Commun. 11(1), 3852 (2020) (Nature Publishing Group)
Jiang, X., Coffee, M., Bari, A., Wang, J., Jiang, X., Huang, J., Shi, J., Dai, J., Cai, J., Zhang, T., Zhengxing, W., He, G., Huang, Y.: Towards an artificial intelligence framework for data-driven prediction of coronavirus clinical severity. Comput. Mater. Continua 62, 537–551 (2020)
Kanegae, H., Suzuki, K., Fukatani, K., Ito, T., Harada, N., Kario, K.: Highly precise risk prediction model for new-onset hypertension using artificial intelligence techniques. J. Clin. Hypertension 22(3), 445–450 (2020)
Rebane, J., Karlsson, I., Papapetrou, P.: An investigation of interpretable deep learning for adverse drug event prediction. In: 2019 IEEE 32nd International Symposium on Computer-Based Medical Systems (CBMS), pp. 337–342. IEEE (2019)
Kalmady, S.V., Greiner, R., Agrawal, R., Shivakumar, V., Narayanaswamy, J.C., Brown, M.R.G., Greenshaw, A.J., Dursun, S.M., Venkatasubramanian, G.: Towards artificial intelligence in mental health by improving schizophrenia prediction with multiple brain parcellation ensemble-learning. NPJ Schizophrenia 5(1), 1–11 (2019)
Schmidt-Erfurth, U., Waldstein, S.M., Klimscha, S., Sadeghipour, A., Hu, X., Gerendas, B.S., Osborne, A., Bogunović, H.: Prediction of individual disease conversion in early amd using artificial intelligence. Invest. Ophthalmol. Vis. Sc. 59(8), 3199–3208 (2018)
Choi, E., Bahadori, M.T., Schuetz, A., Stewart, W.F., Sun, J.: Doctor AI: Predicting clinical events via recurrent neural networks. In: Machine Learning for Healthcare Conference, pp. 301–318. PMLR (2016)
Esteban, C., Staeck, O., Baier, S., Yang, Y., Tresp, V.: Predicting clinical events by combining static and dynamic information using recurrent neural networks. In: 2016 IEEE International Conference on Healthcare Informatics (ICHI), pp. 93–101. IEEE (2016)
Francis, N.K., Luther, A., Salib, E., Allanby, L., Messenger, D., Allison, A.S., Smart, N.J., Ockrim, J.B.: The use of artificial neural networks to predict delayed discharge and readmission in enhanced recovery following laparoscopic colorectal cancer surgery. Tech. Coloproctol. 19(7), 419–428 (2015)
Ng, E.Y.-K., Fok, S.C., Peh, Y.C., Ng, F.C., Sim, L.S.J.: Computerized detection of breast cancer with artificial intelligence and thermograms. J. Med. Eng. Technol. 26(4), 152–157 (2002)
Swan, M.: Health 2050: The realization of personalized medicine through crowdsourcing, the quantified self, and the participatory biocitizen. J. Pers. Med. 2(3), 93–118 (2012)
DeBronkart, D.: From patient centred to people powered: autonomy on the rise. BMJ 350 (2015)
Millenson, M.L.: When “patient centred” is no longer enough: the challenge of collaborative health: an essay by Michael L Millenson. BMJ 358 (2017)
Coughlin, S., Roberts, D., O’Neill, K., Brooks, P.: Looking to tomorrow’s healthcare today: a participatory health perspective. Internal Med. J. 48(1), 92–96 (2018)
Gonzalez-Hernandez, G., Sarker, A., O’Connor, K., Savova, G.: Capturing the patient’s perspective: a review of advances in natural language processing of health-related text. Yearbook Med. inform. 26(01), 214–227 (2017)
Wright, M.T., Springett, J., Kongats, K.: What is participatory health research? In Participatory Health Research, pp. 3–15. Springer (2018)
Denecke, K., Gabarron, E., Grainger, R., Th Konstantinidis, S., Lau, A., Rivera-Romero, O., Miron-Shatz, T., Merolli, M.: Artificial intelligence for participatory health: applications, impact, and future implications. Yearbook Med. Inform. 28(01), 165–173 (2019)
Almalki, M., Gray, K., Sanchez, K.M.: The use of self-quantification systems for personal health information: big data management activities and prospects. Health Inf. Sci. Syst. 3(1), 1–11 (2015)
Staccini, P., Fernandez-Luque, L., et al.: Secondary use of recorded or self-expressed personal data: consumer health informatics and education in the era of social media and health apps. Yearbook Med. Inform. 26(01), 172–177 (2017)
Adikari, A., Nawaratne, R., De Silva, D., Ranasinghe, S., Alahakoon, O., Alahakoon, D., et al.: Emotions of covid-19: content analysis of self-reported information using artificial intelligence. J. Med. Internet Res. 23(4), e27341 (2021)
Amin, S., Irfan Uddin, M., Hassan, S., Khan, A., Nasser, N., Alharbi, A., Alyami, H.: Recurrent neural networks with TF-IDF embedding technique for detection and classification in tweets of dengue disease. IEEE Access 8, 131522–131533 (2020)
Mann, P., Paes, A., Matsushima, E.H.: See and read: detecting depression symptoms in higher education students using multimodal social media data. In: Proceedings of the International AAAI Conference on Web and Social Media, vol. 14, pp. 440–451 (2020)
Wang, T., Brede, M., Ianni, A., Mentzakis, E.: Social interactions in online eating disorder communities: A network perspective. PloS One 13(7), e0200800 (2018)
Nguyen, T., Larsen, M.E., O’Dea, B., Phung, D., Venkatesh, S., Christensen, H.: Estimation of the prevalence of adverse drug reactions from social media. In. J. Med. Informa. 102, 130–137 (2017)
Adams, D.Z., Gruss, R., Abrahams, A.S.: Automated discovery of safety and efficacy concerns for joint & muscle pain relief treatments from online reviews. Int. J. Med. Inform. 100, 108–120 2017
Yang, F.C., Lee, A.J.T., Kuo, S.-C.: Mining health social media with sentiment analysis. J. Med. Syst. 40(11), 1–8 (2016)
Rastegar-Mojarad, M., Ye, Z., Wall, D., Murali, N., Lin, S., et al.: Collecting and analyzing patient experiences of health care from social media. JMIR Res. Protocols 4(3), e3433 (2015)
Lin, Y.J., Chuang, C.-W., Yen, C.-Y., Huang, S.-H., Huang, P.-W., Chen, J.-Y., Lee, S.-Y.: Artificial intelligence of things wearable system for cardiac disease detection. In: 2019 IEEE International Conference on Artificial Intelligence Circuits and Systems (AICAS), pp. 67–70 (2019)
Mathew, R.B., Varghese, S., Joy, S.E. Alex, S.S.: Chatbot for disease prediction and treatment recommendation using machine learning. In: 2019 3rd International Conference on Trends in Electronics and Informatics (ICOEI), pp. 851–856 (2019)
Sullivan B.: Pilot trial of the first conversational agent for smoking cessation (QuitBot). In: Clinical Research Trial Listing (Smoking Cessation) (NCT03585231)
Wall, D.P.: Superpower glass project: a mobile at-home intervention for children with autism. Clinical Trial Registration NCT03569176, clinicaltrials.gov, July 2018. Submitted: 14 June 2018
Stein, N., Brooks, K., et al.: A fully automated conversational artificial intelligence for weight loss: longitudinal observational study among overweight and obese adults. JMIR Diabetes 2(2), e8590 (2017)
Fitzpatrick, K.K., Darcy, A., Vierhile, M.: Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Mental Health 4(2), e7785
Boston Medical Center: Conversational agents to improve quality of life in palliative care. Clinical Trial Registration NCT02750865, clinicaltrials.gov, December 2021. submitted: March 30, 2016
Bates, S.: Progress towards personalized medicine. Drug Discovery Today 15(3–4), 115–120 (2010)
Schork, N.J.: Personalized medicine: time for one-person trials. Nature 520(7549):609–611 (2015)
Vogenberg, F.R.,, Barash, C.I., Pursel, M.: Personalized medicine. Pharm. Therapeut. 35(10):560–576 (2010)
Bollati, V., Ferrari, L., Leso, V., Iavicoli, I.: Personalised medicine: implication and perspectives in the field of occupational health. La Medicina del Lavoro 111(6), 425 (2020)
Orlando, L.A., Ryanne Wu, R., Myers, R.A., Neuner, J., McCarty, C., Haller, I.V., Harry, M., Fulda, K.G., Dimmock, D., Rakhra-Burris, T., et al.: At the intersection of precision medicine and population health: an implementation-effectiveness study of family health history based systematic risk assessment in primary care. BMC Health Services Res. 20(1), 1–10 (2020)
Dilsizian, S.E., Siegel, E.L.: Artificial intelligence in medicine and cardiac imaging: harnessing big data and advanced computing to provide personalized medical diagnosis and treatment. Curr. Cardiol. Rep. 16(1), 1–8 (2014)
Ullah, M., Akbar, A., Yannarelli, G.G.: Applications of artificial intelligence in early detection of cancer, clinical diagnosis and personalized medicine (2020)
Sollini, M., Bartoli, F., Marciano, A., Zanca, R., Slart, R.H.J.A., Erba, P. A.: Artificial intelligence and hybrid imaging: the best match for personalized medicine in oncology. Eur. J. Hybrid Imaging 4(1), 1–22 (2020)
Alagappan, M., Glissen Brown, J.R., Mori, Y., Berzin, T.M.: Artificial intelligence in gastrointestinal endoscopy: the future is almost here. World J. Gastrointest. Endosc. 10(10), 239 (2018)
Patel, D., Kher, V., Desai, B., Lei, X., Cen, S., Nanda, N., Gholamrezanezhad, A., Duddalwar, V., Varghese, B., Oberai, A.A.: Machine learning based predictors for covid-19 disease severity. Sci. Rep. 11(1), 1–7 (2021)
Murugan, R., Goel, T.: E-diconet: extreme learning machine based classifier for diagnosis of covid-19 using deep convolutional network. J. Ambient Intell. Hum. Comput. 12(9), 8887–8898 (2021)
Bibi, N., Sikandar, M., Ud Din, I., Almogren, A., Ali, S.: IoMT-based automated detection and classification of leukemia using deep learning. J. Healthcare Eng. (2020)
Nanmaran, R., Srimathi, S., Yamuna, G., Thanigaivel, S., Vickram, A.S., Priya, A.K., Karthick, A., Karpagam, J., Mohanavel, V., Muhibbullah, M.: Investigating the role of image fusion in brain tumor classification models based on machine learning algorithm for personalized medicine. Comput. Math. Methods Med. (2022)
McKinney, S.M., Sieniek, M., Godbole, V., Godwin, J., Antropova, N., Ashrafian, H., Back, T., Chesus, M., Corrado, G.S., Darzi, A., et al.: International evaluation of an AI system for breast cancer screening. Nature 577(7788), 89–94 (2020)
Franzmeier, N., Koutsouleris, N., Benzinger, T., Goate, A., Karch, C.M., Fagan, A.M., McDade, E., Duering, M., Dichgans, M., Levin, J., et al.: Predicting sporadic Alzheimer’s disease progression via inherited Alzheimer’s disease-informed machine-learning. Alzheimer’s Dementia 16(3), 501–511 (2020)
Zhou, T., Thung, K.-H., Zhu, X., Shen, D.: Effective feature learning and fusion of multimodality data using stage-wise deep neural network for dementia diagnosis. Hum. Brain Map. 40(3), 1001–1016 (2019)
Long, E., Lin, H., Liu, Z., Xiaohang, W., Wang, L., Jiang, J., An, Y., Lin, Z., Li, X., Chen, J., et al.: An artificial intelligence platform for the multihospital collaborative management of congenital cataracts. Nat. Biomed. Eng. 1(2), 1–8 (2017)
Tan, W.K., Hassanpour, S., Heagerty, P.J., Rundell, S.D., Suri, P., Huhdanpaa, H.T., James, K., Carrell, D.S., Langlotz, C.P., Organ, N.L., et al.: Comparison of natural language processing rules-based and machine-learning systems to identify lumbar spine imaging findings related to low back pain. Acad. Radiol. 25(11), 1422–1432
Frunza, O., Inkpen, D., Tran, T.: A machine learning approach for identifying disease-treatment relations in short texts. IEEE Tran. Knowl. Data Eng. 23(6), 801–814 (2011)
Khan, I.Y., Zope, P., Suralkar, S.R.: Importance of artificial neural network in medical diagnosis disease like acute nephritis disease and heart disease. Int. J. Eng. Sci. Innovat. Technol. 2, 210–217 (2013)
Kumar, K., Abhishek, B.: Artificial Neural Networks for Diagnosis of Kidney Stones Disease, vol. 10. GRIN Verlag Germany (2012)
Yang, C., An, B., Yin, S.: Heart-disease diagnosis via support vector machine-based approaches. In: 2018 IEEE International Conference on Systems, Man, and Cybernetics (SMC), pp. 3153–3158 (2018)
Orunesu, E., Bagnasco, M., Salmaso, C., Altrinetti, V., Bernasconi, D., Del Monte, P., Pesce, G., Marugo, M., Mela, G.S.: Use of an artificial neural network to predict graves’ disease outcome within 2 years of drug withdrawal. Eur. J. Clin. Invest. 34(3), 210–217 (2004)
Clarke, E.A.: What is preventive medicine? Can. Fam.Phys. 20(11), 65 (1974)
Chang, A.: The role of artificial intelligence in digital health. In: Digital Health Entrepreneurship, pp. 71–81. Springer (2020)
Schwalbe, N., Wahl, B.: Artificial intelligence and the future of global health. Lancet 395(10236), 1579–1586 (2020)
Gastounioti, A., Desai, S., Ahluwalia, V.S., Conant, E.F., Kontos, D.: Artificial intelligence in mammographic phenotyping of breast cancer risk: a narrative review. Breast Cancer Res. 24(1), 1–12 (2022)
Johnson, K.W., Soto J.T., Glicksberg, B.S., Shameer, K., Miotto, R., Ali, M., Ashley, E., Dudley, J.T.: Artificial intelligence in cardiology. J. Am. Col. Cardiol. 71(23), 2668–2679 (2018)
Ahn, J.C., Connell, A., Simonetto, D., Hughes, C., Shah, V.H.: Application of artificial intelligence for the diagnosis and treatment of liver diseases. Hepatology 73(6), 2546–2563 (2021)
Greco, M., Caruso, P.F., Cecconi, M.: Artificial intelligence in the intensive care unit. Seminars Respirat. Crit. Care Med. 42(1) (2021) (Thieme Medical Publishers, Inc.)
Damen, J.A.A.G., Hooft, L., Schuit, E., Debray, T.P.A., Collins, G.S., Tzoulaki, I., Lassale, C.M., Siontis, G.C.M., Chiocchia, V., Roberts, C.: et al.: Prediction models for cardiovascular disease risk in the general population: systematic review (2016)
Ravaut, M., Sadeghi, H., Leung, K.K., Volkovs, M., Kornas, K., Harish, V., Watson, T., Lewis, G.F., Weisman, A., Poutanen, T., et al.: Predicting adverse outcomes due to diabetes complications with machine learning using administrative health data. NPJ Digit. Med. 4(1), 1–12 (2021)
Nejra, K., Lejla, K., Nermana, K., Amina, K., Božana, L., Amina, L., Almir, B.: Application of artificial intelligence techniques to predict effects of cigarette smoking on hematological parameters and attributable diseases. In: International Conference on Medical and Biological Engineering, pp. 313–318. Springer (2021)
Mora-Jiménez, I., Tarancón-Rey, J., Álvarez-Rodríguez, J., Soguero-Ruiz, C.: Artificial intelligence to get insights of multi-drug resistance risk factors during the first 48 hours from ICU admission. Antibiotics 10(3), 239 (2021)
Yang, N.I., Yeh, C.-H., Tsai, T.-H., Chou, Y.-J., Hsu, P.W.-C., Li, C.-H., Chan, Y.-H., Kuo, L.-T., Mao, C.-T., Shyu, Y.-C., et al.: Artificial intelligence-assisted identification of genetic factors predisposing high-risk individuals to asymptomatic heart failure. Cells 10(9), 2430 (2021)
Lu, Y., Stathopoulou, T., Vasiloglou, M.F., Pinault, L.F., Kiley, C., Spanakis, E.K., Mougiakakou, S.: goFOODTM: an artificial intelligence system for dietary assessment. Sensors 20(15), 4283 (2020)
Regalia, G., Onorati, F., Lai, M., Caborni, C., Picard, R.W.: Multimodal Wristworn devices for seizure detection and advancing research: focus on the Empatica wristbands. Epilepsy Res. 153, 79–82 (2019)
Christiansen, M.P., Garg, S.K., Brazg, R., Bode, B.W., Bailey, T.S., Slover, R.H., Sullivan, A., Huang, S., Shin, J., Lee, S.W., et al.: Accuracy of a fourth-generation subcutaneous continuous glucose sensor. Diabetes Technol. Therapeut. 19(8), 446–456 (2017)
Liu, Q., Cui, X., Chou, Y.-C., Abbod, M.F., Lin, J., Shieh, J.-S.: Ensemble artificial neural networks applied to predict the key risk factors of hip bone fracture for elders. Biomed. Signal Process. Control, 21, 146–156 (2015)
Irena Spasić, Pete Burnap, Mark Greenwood, and Michael Arribas-Ayllon. A naïve bayes approach to classifying topics in suicide notes. Biomedical informatics insights, 5:BII–S8945, 2012
Jang, K.J., Balakrishnan, G., Syed, Z., Verma, N.: Scalable customization of atrial fibrillation detection in cardiac monitoring devices: Increasing detection accuracy through personalized monitoring in large patient populations. In: 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, pp. 2184–2187. IEEE (2011)
Zhang, Y., Szolovits, P.: Patient-specific learning in real time for adaptive monitoring in critical care. J. Biomed. Inform. 41(3), 452–460 (2008)
Acknowledgements
The authors gratefully acknowledge financial support from ANID PIA/APOYO AFB180003. This work was supported by projects ANID (National Research and Development Agency of Chile) Doctorado Nacional #2116137
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ruiz, R.B., Velásquez, J.D. (2023). Artificial Intelligence for the Future of Medicine. In: Lim, C.P., Vaidya, A., Chen, YW., Jain, V., Jain, L.C. (eds) Artificial Intelligence and Machine Learning for Healthcare. Intelligent Systems Reference Library, vol 229. Springer, Cham. https://doi.org/10.1007/978-3-031-11170-9_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-11170-9_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-11169-3
Online ISBN: 978-3-031-11170-9
eBook Packages: EngineeringEngineering (R0)