Abstract
This chapter discusses current recommendations made by obstetrics and gynecology international committees including ACOG, RCOG, and FIGO.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Since PAS was first prescribed in the first half of the twentieth century, hysterectomy has been the sole management of this life-threatening disorder for several decades [1]. Uterus-preserving procedures have not been endorsed until relatively recently, perhaps in concordance with our developing understanding of risk factors and antenatal diagnosis, which has rendered planned delivery feasible for many cases. However, uterus-preserving procedures comprise a spectrum of expanding inconsistent techniques that are associated with variable success rates and complications [2,3,4]. These procedures are highly dependent on surgeon’s experience and dexterity, and evidence on their safety and efficacy is limited. In addition, some of these procedures may include manual removal of the placenta, which makes such procedures concerning since this may trigger extensive and life-threatening bleeding. Although uterus-preserving procedures have been increasingly appraised as a possible alternative particularly in women who are highly motivated to maintain their fertility, caesarean hysterectomy remains the standard procedure and is universally recommended by internationally recognized practice guidelines especially in severe cases [5].
Although evidence-based recommendations on management of PAS disorders have been consistently adopted by several international communities, this topic lacks high-quality prospective studies that would support many of these recommendations [4]. This may be due to the low incidence of PAS (0.2% of all pregnancies), which precludes conduction of large studies [6]. Furthermore, the serious nature of PAS disorders creates ethical restrictions to clinical assessment of some management approaches. In addition, many studies reflect a particular team-based practice on selected group of cases (case series) rather than a comprehensive and universal protocol to all women with PAS. Therefore, reproducibility of emerging results is usually doubtful. Unfortunately, external validation of any of the proposed techniques, on a larger cohort or in a different setting, is rarely done. These concerns disrupt robustness of evidence and broaden the gap between evidence-based guidance and actual practice since none of the these practice-based approaches could be satisfactorily studied to prove its safety and efficacy.
Evidence-Based Recommendations on Management of PAS
Antenatal Screening
With the rising trend of cesarean section rates worldwide, PAS is no longer considered a rare disorder. The Royal College of Obstetricians and Gynaecologists (RCOG) highlights the importance of identifying PAS risk factors during antenatal assessment [7]. Antenatal suspicion of PAS facilitates planned management, which yields substantially better outcomes compared to unrecognized cases diagnosed at the time of labor. Therefore, the Society of Obstetricians and Gynaecologists of Canada (SOGC) recommends routine screening of women with prior cesarean delivery or uterine surgery for PAS [8]. Screening can be made using ultrasound, which is ideally performed at the time of mid-trimester fetal anatomy scan [8]. As recommended by the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG), suspected cases of PAS should be planned as confirmed PAS and should be referred to a PAS specialized center [9].
Transfer of Care
Standard management of women with PAS should be initiated as early as suspicion is raised. The American College of Obstetricians and Gynecologists (ACOG) recommends immediate transfer of suspected patients to a tertiary center that has the facility to follow up and manage women with PAS disorders [6, 10]. Specifically, PAS referral centers should have sufficient and readily available blood products. Availability of autologous blood salvage devices is preferred. Autologous cell salvage is associated with lower need for allogenic blood transfusion, with no increased risk of complications [11,12,13]. Therefore, the International Federation of Gynecology and Obstetrics (FIGO) recommends the use of autologous cell salvage when available [14]. Indeed, autologous cell salvage may be compulsory if women decline or cannot receive blood products, e.g., Jehovah’s Witnesses [15, 16].
Furthermore, PAS specialized centers should support PAS-directed multidisciplinary care, which consists of an obstetrician or obstetric surgeon, a pelvic surgeon, an anesthesiologist, an intensivist, a neonatologist, a urologist, a hematologist, and an interventional radiologist [17]. Multidisciplinary structure, involved in decision-making and clinical care, promotes cumulative institutional experience in all aspects of PAS management, which eventually results in significant improvement of maternal outcomes and quality of care [18]. Specifically, this mounting experience yields lower risk of massive blood transfusion, intensive care admission, and reoperation [19]. Similar recommendations are made by the SOGC, which supports the role of specialized centers and multidisciplinary approach to optimize care of women with PAS [8]. SOGC defines the structure of these centers and emphasizes on the necessity of level II obstetric ultrasonography, level III maternity unit, level II neonatal intensive care unit, and adult intensive care unit. The role of centers of excellence and multidisciplinary care in reducing maternal morbidity is also recognized by FIGO [14, 17, 20,21,22]. In addition, FIGO strongly recommends that a surgeon specialized in complex pelvic surgery attends delivery [14]. A retrospective study of 98 women showed that attendance of a gynecologic oncologist was associated with less blood loss and lower need for blood transfusion [23]. Similarly, RCOG endorses the role of complex pelvic surgeons as a part of the managing team [7].
The managing team should hold a thorough discussion with the patient to explain her potential diagnosis. Women should be counseled on different management scenarios and potential complications associated with PAS including massive bleeding and potential need for blood transfusion, urinary tract injury, and hysterectomy and additional procedures that may be necessary to manage these complications. RCOG also recommends that anesthesia plan should be discussed antenatally and women should be counseled and consented on the possibility of conversion from spinal to general anesthesia [7].
Delivery Planning
Planned delivery is a crucial part of PAS management and is associated with better outcomes compared to emergency delivery [24, 25]. Delivery should be scheduled on a date that weighs the risk of preterm labor against risk of emergency delivery. According to ACOG, patient preference and maternal and fetal status should be also considered. Accordingly, “34 weeks” may be the optimal time to schedule delivery unless earlier delivery is otherwise indicated [26, 27]. Delivery window may be extended to 36 + 0 weeks. However, ACOG does not support expectant management beyond this point because it may increase risk of spontaneous bleeding and emergency delivery [26]. For similar reasons, SOGC recommends elective delivery between 34 and 36 weeks of gestation. Antenatal steroids should be offered within 1 week of planned delivery if it is scheduled at or before 34+6 weeks of gestation [8, 28]. FIGO also considers the balance between risks of bleeding and prematurity and recommends scheduled delivery, preferably between 34 and 35 weeks [20, 29,30,31]. However, RCOG extends the window of scheduled delivery between 35+0 and 36+6 weeks of gestation [7]. This recommendation is supported by retrospective data which did not show significant risks associated with expectant management of PAS beyond 36 weeks [32]. An emergency plan should be readily available if immediate delivery is necessary for bleeding or other urgent obstetric indications. SOGC recommends that women are counseled not to travel far away from specialized centers. They should be provided with a document declaring their diagnosis, managing center, and plan of care to facilitate their transfer in case of emergency [8].
As a part of planned delivery, operative room should be equipped with available blood products, and the blood bank should be notified and should anticipate and prepare for massive transfusion protocols. Devices and medications required for management of postpartum hemorrhage should be readily accessible. Management approach should be thoroughly discussed with the patient in advance, and she should be counseled on the necessity, complications, and outcomes of peripartum hysterectomy [10]. Women who are highly motivated to reserve future fertility should be aware of uterus-preserving options. ACOG recommends that decision should be individualized [10]. However, counseling should be prudently made since these options are not supported by high-quality evidence and they may be associated with significant risks. Either way, women should be consented for hysterectomy since uterus-preserving procedures are liable to failure or infeasibility due to intraoperative bleeding. It is important to emphasize that there are no randomized clinical trials or prospective well-controlled observational studies that compare planned hysterectomy to uterus-preserving procedures and current data is mostly derived from single-arm and small studies [33].
Although planned delivery in a specialized tertiary center is indicated in all suspected cases, unexpected intraoperative diagnosis of PAS is common, reaching more than 30% of all cases in some reports originating from developed countries [34]. In these situations, ACOG recommends proceeding with uterine closure and hysterectomy. Unfortunately, hysterectomy may not be feasible in all birth units, and under these circumstances, women should be hemodynamically stabilized with blood transfusion, tranexamic acid infusion, and abdominal packing if necessary, before the patient is transferred to a specialized center [10]. Similarly, if PAS is recognized prior to uterine incision, SOGC recommends that the abdomen should be closed, and the patient should be immediately transferred to a specialized center for definitive management [8, 35].
Unexpected intraoperative diagnosis of PAS may occur after vaginal delivery even in the absence of risk factors. If the placenta is retained with no uterine bleeding indicating placental separation, and no plane of placental separation can be felt by bimanual examination, PAS disorder should be suspected. According to SOGC guidelines, the acceptable approach comprises cutting of the umbilical cord and clamping it with an absorbable suture, administration of intravenous prophylactic antibiotics, and keeping an intravenous access with continuous oxytocin infusion. Oral intake is prevented for 12–24 hours should general anesthesia be needed for urgent surgical management. According to SOGC, placental tissue may be removed under ultrasound or hysteroscopic guidance if the patient remains stable with no active bleeding [8]. High-intensity focused ultrasound has been recently proposed in stable women if retained placental tissue is larger than 3 cm, yet not occupying more than half of the uterine cavity [36].
Preoperative Preparation
As a part of planned management, optimization of perioperative environment should be contemplated. Antenatal suspicion of PAS provides sufficient time to review medical records, request additional information, and carry out any necessary measures. SOGC recommends maternal serology testing, including hepatitis C, hepatitis B, and HIV viruses prior to delivery. Additionally, previous surgical reports, especially if associated with massive blood transfusion, should be obtained. A simple but crucial measurement is correction and follow-up of maternal hemoglobin prior to delivery since anemia may aggravate sequalae of blood loss both quantitatively and qualitatively [8]. Iron deficiency is the most common cause of anemia in pregnancy and can be corrected either orally or intravenously [37]. FIGO also proposes the use of erythropoietin, if clinically indicated, understanding that this treatment is associated with significantly higher cost [14].
Since PAS-indicated cesarean hysterectomy is associated with high incidence of urinary tract injuries (approximately one third of cases), utility of preoperative placement of ureteric stents has been investigated and was found to reduce the incidence of urinary tract injury to 6% [38]. Therefore, ureteric stents are endorsed by FIGO and RANZCOG particularly if bladder invasion is preoperatively suspected [9, 14]. Similarly, RCOG does not support the use of ureteric stents and cystoscopy unless the bladder is likely invaded [7, 39, 40]. Preoperative cystoscopy may be considered to assess bladder invasion [39]. A full bladder may facilitate bladder dissection from the lower segment, cystotomy, and cervical identification when total hysterectomy is performed [31]. Therefore, RCOG recommends bladder filling to identify bladder separation plane and cystotomy to excise affected area when bladder invasion is confirmed [7, 40, 41].
Massive bleeding and blood transfusion are the most common complications of PAS, and cross-matched blood products should be readily available for planned and emergency delivery. Obstetric hemorrhage in PAS patients requires greater compensation for the lost blood compared to other causes of postpartum hemorrhage. Therefore, RCOG recommends that standardized PAS-directed national or institutional protocols of postpartum hemorrhage and blood transfusion should be adopted and strictly followed [7, 42,43,44].
Intraoperative Management
-
I.
Anesthesia
As recommended by FIGO, the type of anesthesia should be determined by the anesthetist in collaboration with the multidisciplinary team especially when risk of massive intraoperative bleeding is significant [14]. However, if diagnosis of PAS is made intraoperatively, the probability of conversion of regional to general anesthesia is high [45,46,47,48]. General anesthesia is more suitable in emergency situations where anesthesia can be established quickly, and resuscitation of unstable women is facilitated. In general, regional anesthesia is preferable to general anesthesia whenever feasible since it is associated with lower incidence of anesthetic complications. Although some studies showed that regional anesthesia may reduce maternal morbidity caused by hemorrhage and blood transfusion in women with PAS [49, 50], a retrospective study of 50 cases with PAS did not support this conclusion [48]. In addition, regional anesthesia precludes the risk of neonatal respiratory depression caused by volatile drugs that cross the placenta. Fortunately, this risk may not be substantially significant [48].
-
II.
Positioning
Intraoperative placement of women with PAS in a modified lithotomy position is preferred. SOGC endorses this position should vaginal access be needed and to facilitate monitoring of vaginal bleeding intraoperatively [8].
-
III.
Perioperative Medications
Antibiotics and tranexamic acid should be administered intravenously at the time of skin incision [8, 51]. Oral or intravenous administration of tranexamic acid pre- or intraoperatively is also highly recommended by FIGO based on established results of a large double-blinded clinical trial. The study, that comprised 20,060 women, showed that use of tranexamic acid reduces postpartum hemorrhage-related deaths with no increased risks of thromboembolism [52]. Although the study was not specific to PAS, women with placenta previa or accreta were not excluded from the study, and they presented 9% of the study population.
-
IV.
Skin Incision
Classically, the pelvis should be accessed through a midline vertical skin incision. According to FIGO, midline skin incision should be opted for placentas that extend beyond the lower uterine segment toward the umbilicus and when cesarean hysterectomy is planned. However, transverse skin incision, either low or midline, may be appropriate depending on the highest level of anterior placental edge [53].
-
V.
Bladder Dissection
Since urinary tract injuries can significantly complicate surgery and disrupt visualization of the field, FIGO recommends assessment of bladder invasion and proper bladder dissection before the fetus is delivered [38, 54]. This should be completed and diagnosis of percreta is confirmed before cystotomy and excision of the invaded area of bladder are made [53]. In such cases, a posterior approach may be required to facilitate uterine devascularization and hysterectomy [55].
-
VI.
Uterine Incision
While assessing for extent of invasion, the uterus should be gently handled. Ultrasound can be used intraoperatively to guide uterine incision, which should be ideally a classical incision and should avoid cutting through the placenta. Intraoperative ultrasound has gained increasing popularity in localizing the placenta before uterine incision is made and is endorsed by SOGC and FIGO [8, 53]. Uterine incisions should be made above the upper placental margin including fundal hysterotomy which may be performed transversally to deliver the fetus if the placenta extends anteriorly [20, 21, 41, 56, 57]. Although the use of uterine staplers or Smith-Opitz clamps, as adopted in fetal surgery, may reduce intraoperative bleeding, availability and cost of these instruments limit the popularity of their application. SOGC recommends a one-layer closure of the uterus before proceeding with hysterectomy to reduce intraoperative blood loss [8].
-
VII.
Uterine Preservation
Although ACOG endorses cesarean hysterectomy as the standard management of women with PAS, uterine preservation may be considered on individual basis [6, 10]. ACOG restricts uterine preservation to PAS associated with focal invasion where the adherent area is sufficiently localized to permit manual or surgical removal of the placenta with closure of the defect [27]. Similarly, RCOG considers partial myometrial resection if minimal invasion is identified. However, a consent to preserve the uterus should be obtained [7]. En bloc removal of placental invasion, followed by uterine repair, may be considered with larger adherent areas [58]. Accordingly, feasibility of uterine preservation is mainly determined intraoperatively. Therefore, women should be clearly counseled that even if uterine preservation would be considered, hysterectomy may be eventually warranted.
Extirpative technique of uterine preservation refers to manual or forceful removal of the placenta to empty the uterus followed by bleeding control. Although the technique is old and well known in management of postpartum bleeding associated with incomplete separation of the placenta [15, 59,60,61,62,63,64], it is associated with substantial risk of intractable uterine bleeding in the presence of PAS, which would double the average blood loss in these cases [64]. Compared to “leaving placenta in situ,” extirpative technique is associated with higher incidence of blood transfusion, disseminated intravascular coagulopathy (DIC), hysterectomy, and infections [65]. Therefore, FIGO recommends avoidance of extirpative technique and advises against manual removal of the placenta if PAS is suspected and/or placental separation does not easily occur [53].
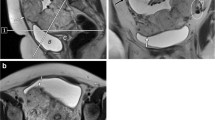
In concordance with ACOG, SOGC also considers uterine preservation if the placenta is separable with focal invasion that can be excised and repaired. In fact, excision of invaded myometrium may also reduce risk of recurrence in subsequent pregnancies [66]. Although FIGO realizes focal resection and reconstruction of the uterus as a possible method of uterine preservation [53, 58, 67, 68], it raises a valid concern on its reproducibility since the procedure could be highly dependent on surgeon’s skills [53]. SOGC also endorses a technique of perioperative localization of placenta wedge which may be guided by preoperative magnetic resonance imaging (MRI), pelvic devascularization, and placental nonseparation with resection of the invaded wedge. This procedure is known as “triple-P technique” [8, 69]. Although triple-P technique seems to reduce the incidence of hysterectomy, data may be too sparse to make a strong recommendation [69, 70]. FIGO also endorses the promising results of placental bed tamponade, which involves suturing of the inverted cervical lips to the lower uterine wall. The procedure was efficient as indicated by a few case series [71,72,73,74,75,76]. Nevertheless, larger studies may be warranted to establish robust recommendations. Both triple-P procedure and cervical tamponade were not considered by the RCOG due to limited evidence [7]. Uterine compression sutures have been proposed as a procedure to preserve the uterus in certain situations. They include either the same compression sutures used to manage atonic postpartum hemorrhage (e.g., B-Lynch sutures) or other sutures designed specifically to control bleeding from placental bed (e.g., multiple 8 compression sutures) [71, 77]. Although these procedures may be associated with reported cases of wound infection and intrauterine synechiae, overall, they seem safe and associated with reassuring long-term fertility outcomes [78,79,80]. However, most data originate from case series and small studies, and evidence is too limited to recommend their implementation [81]. A retrospective study of 148 women showed that the use of Bakri balloon for uterine preservation was comparable to local uterine wall resection and hysterectomy in rate of admission to intensive care unit, duration of hospital stay, operative time, and amount of transfused blood products [82]. However, larger well-designed studies are warranted to validate these conclusions. In fact, data on many uterus-preserving procedures are derived from case series and small studies and may be associated with inconsistent outcomes [83].
SOGC also acknowledges an alternative to hysterectomy if non-focal invasion is found. In this situation, there should be no trial to remove the placenta, which is left in place and the uterus is closed. Leaving “placenta in situ” is the first established uterus-preserving procedure. In this method, the cord is cut away from its placental origin and the uterus is closed [53]. Thereafter, patients expectantly managed awaiting tissue atrophy secondary to reduction in blood supply with subsequent resorption, separation, and expulsion of placental segments [84]. In a French retrospective multicenter study of 167 patients managed with this approach, success rate was 78% and the uterus took a median of 13.5 weeks (range 4–60) to spontaneously empty [85]. Although this approach is recognized by SOGC and RANZCOG, they are obvious about its drawbacks, which should be clearly shared with the patient before a preoperative decision is made. They include prolonged recovery course, relatively long follow-up, and persistent possibility of secondary hysterectomy (up to 40%), which may be indicated up to several months after delivery [3, 8, 9, 83]. Furthermore, leaving placenta in situ can lead to significant maternal morbidities. Pelvic infection, sepsis, hemorrhage, coagulopathy, and pulmonary embolism are among the reported complications of this approach [2, 15, 85, 86]. FIGO and RCOG state that administration of prophylactic antibiotics may be considered if the placenta is left in situ. Nevertheless, level of evidence is low [7, 27, 53]. Administration of methotrexate, as an adjuvant treatment to accelerate placental autolysis, was not shown to be considerably effective based on data from small studies and was associated with significant side effects such as pancytopenia and nephrotoxicity. In addition, methotrexate may increase risk of pelvic infection and sepsis due to its immunosuppressive effect [87,88,89,90,91]. Therefore, FIGO and RCOG recommend against the use of methotrexate if the placenta is left in situ [7, 53]. Postpartum removal of placental tissue using hysteroscopy and ultrasound guidance has been proposed to hasten placental resolution [92, 93]. However, these options are only supported by limited data, and risk of perforation of a postpartum uterus presents a major concern to their use [92]. High-intensity focused ultrasound, as a method to ablate placental tissue without perforation risk, has been recently proposed with initial promising results [94]. However, this method has only been investigated in women with residual placental tissue larger than 3 cm, but not occupying greater than 50% of the uterine cavity and has not been investigated in women who were managed specifically by leaving the whole placenta in situ [36].
-
VIII.
Cesarean Hysterectomy
If cesarean hysterectomy is planned, placental removal should not be attempted. Leaving the placenta in place while proceeding with hysterectomy is associated with less blood loss and lower incidence of blood transfusion [29, 32, 95, 96]. Although this practice is recommended by FIGO and RCOG, FIGO also considers a gentle trial to remove the placenta acceptable if spontaneous separation occurs or if placental invasion appears minimal [41]. In absence of spontaneous separation, FIGO advises that uterotonics should not be administered and that the operative team should proceed with immediate hysterectomy [14]. FIGO also recommends total hysterectomy over subtotal hysterectomy. Although subtotal hysterectomy is associated with shorter operative time, less blood loss and lower rate of blood transfusion, cervical involvement by placental invasion and risk of cancers that may rise from cervical stump make subtotal hysterectomy less preferred in modern practice [14]. Nevertheless, the Society of Maternal-Fetal Medicine (SMFM) survey showed balanced predilection among surgeons regarding their preferred hysterectomy technique (55% for total hysterectomy vs. 45% for subtotal hysterectomy) [97]. Other modifications to hysterectomy including posterior retrograde hysterectomy via pouch of Douglas [98], modified radical hysterectomy with the use of bipolar cautery device [20], linear cutting stable device for hysterotomy [99], and use of vessel-sealing devices [100] were also described.
In some cases, the placenta may extensively invade the surrounding pelvic organs, and thereby, immediate hysterectomy may become challenging to perform. Delayed hysterectomy may be scheduled from the 3rd to the 12th week after delivery [21, 101, 102]. The rationale of delayed surgery is to allow tissue resorption and reduction of vascularity before hysterectomy is performed. FIGO endorses the option of delayed hysterectomy if immediate hysterectomy is not feasible understanding that level of evidence, supporting this practice, is low [14]. Total blood loss associated with delayed surgery may be comparable to immediate hysterectomy [21, 101, 103]. However, delayed hysterectomy may be associated with risks of leaving placenta in situ. Thus, regular follow-up is mandatory and emergency hysterectomy should be planned, if necessary [14].
-
IX.
Pelvic Devascularization
In conjugation with primary intervention, pelvic devascularization is considered by many surgeons to reduce blood loss. Although internal iliac artery ligation is adopted by many PAS specialized centers, the procedure has not been proved to be effective [8]. This is probably because the rich collateral blood supply from external iliac arteries and the aorta compensates for internal iliac artery occlusion. Furthermore, internal iliac artery ligation may add to complexity of surgery and may be associated with longer operative time and risk of vascular complications [104]. Preoperative bilateral transfemoral placement of internal iliac artery balloons, which are inflated intraoperatively after delivering the fetus, was associated with similar outcomes [105, 106]. Thus, both techniques of occlusion are not routinely recommended by the SOGC [8]. Similarly, FIGO does not recommend routine radiologic or surgical devascularization [53]. In addition to their limited effectiveness, these procedures are associated with several complications including popliteal and external iliac arteries thrombosis [107, 108], rupture of iliac artery [109], and nerve injury due to ischemia.
Emerging evidence on temporary infrarenal aortic balloon occlusion supports its safety and efficacy. A meta-analysis of 11 clinical studies (776 patients) showed that the procedure was associated with significant reduction in blood loss (mean difference [MD], 1480 ml; 95% confidence interval [CI], –1806 to −1154 ml), operative time (MD, 29.23 min; 95% CI, –46.04 to −12.42), and volume of blood transfusion (MD, 1125 ml; 95% CI –1264 to −987). The procedure was also associated with shorter hospitalization and lowered hysterectomy rate when performed alone with uterus-preserving procedures (OR 0.30, 95% CI 0.19 to 0.48) [110]. Therefore, this approach is recommended by SOGC particularly when a difficult surgery is anticipated [8]. Similarly, SMFM endorses clamping and balloon occlusion of abdominal aorta as an effective method to decrease pelvic blood flow. However, risk of potential distal thrombosis or ischemia should be considered, and a vascular surgeon should be consulted if this option is considered [111, 112]. RCOG highlights the controversial role of interventional radiology, including internal iliac artery, uterine artery, and aortic occlusion due to lack of large well-designed studies [113,114,115,116,117,118,119,120,121,122]. Nevertheless, RCOG considers this option in women who decline blood transfusion along with cell salvage [7, 43]. Arterial embolization may be considered in women with postpartum hemorrhage particularly if they are hemodynamically stable and do not suffer severe bleeding [123].
Postoperative Care
Postoperative care of women with PAS is crucial since complications of high-volume blood loss, prolonged surgery, intraoperative hypotension, and organ system dysfunctions are not uncommon. SMFM recommends frequent monitoring of vital signs and urine output using an indwelling catheter. If there is anuria or persistent hematuria, urinary tract injuries should be considered among other causes. Bleeding from the vagina and the incision should be frequently assessed. Anemias and coagulopathies should be corrected. Women should be encouraged to ambulate early to reduce risk of thromboembolic events associated with pregnancy, surgery, massive blood loss, and blood transfusion [111].
In women who were managed by “leaving placenta in situ,” strict follow-up is indicated since residual villi may take up to 6 months to resolve [89]. There are no standardized protocols to follow up these patients. Nevertheless, follow-up should take place in a specialized center with suitable experience [53]. FIGO recommends weekly measurement of serum β-hCG to ensure reduction of placental tissue. Nevertheless, ultrasound remains the primary method of assessment of placental mass. Other imaging modalities, such as magnetic resonance imaging, are not required [124]. Besides, follow-up visits should include clinical assessment of vaginal bleeding and infection and investigations, such as vaginal culture, hemoglobin level, and leucocytic count, if indicated [85]. If postpartum course remains uncomplicated after 3 months, follow-up visits can be scheduled monthly [53].
Barriers to Evidence-Based Practice: Why Does Global Practice Not Strictly Follow Guidelines?
According to the World Health Organization (WHO), guidelines are a set of evidence-based recommendations that instruct clinicians on how to practice in a way that yields the best possible outcomes according to the highest quality of research [125, 126]. Although practice guidelines have played a major role in modern medicine, there are some inherent concerns that limit their reflection on clinical practice. For example, guidelines are associated with high dependency on homogenous controlled studies which may not be reflective of general population and actual practice circumstances. Also, guidelines tend to refer to committees’ opinion to resolve many inconclusive issues, which may be influenced by personal perspectives, institutional style of practice, served population, and availability of resources. Guidelines may limit the role of personal experience and appreciate study quality at the expense of unstudied population, which may differ significantly from the study cohort [127, 128]. Thus, these recommendations may offer a treatment of a specific disease rather than a particular patient [129,130,131]. In fact, the process of generation of practice guidelines may be influenced by the origin of the study, and in some situations, national guidelines may prioritize regional studies over international studies even if the later exhibit higher quality or larger cohorts [132]. Guidelines are limited by lack of high-quality data, which results in exclusion of several approaches, some of which may be efficient or deemed efficient based on unpublished institutional experience. Nevertheless, evidence-based guidelines remain the most widely acceptable method to practice standardized medicine in a controlled fashion. Otherwise, practice would be inconsistent, significantly impacted by providers’ varying experience, and medical malpractice will be challenging to define [29, 133].
Implementation of PAS guidelines may be challenged by several regional and clinical obstacles. Specifically, planned cesarean hysterectomy is defined as the standard management of PAS by all internationally recognizable practice guidelines. This is primarily due to safety concerns, which place a well-established surgery superior to less known and surgeon-dependent procedures. However, hysterectomy may have significant psychological sequalae in many women, including depression, even in the absence of preexisting psychiatric illness [134,135,136]. It is not uncommon that women experience negative thoughts regarding their physical and sexual well-being [137]. These sequalae are usually a reaction to their frustration of losing a special feminine organ and their inability to carry a pregnancy in the future. In some regions, the situation may be much exaggerated by cultural beliefs, lack of understanding and support, and restrictions to fertility options, particularly surrogacy. Under these circumstances, hysterectomy is strongly declined by many patients. Surgeons have had to establish their own experience in preserving the uterus to meet their patients’ interests, and with time, uterus-preserving procedures have become more prevalent than hysterectomy in these regions. Therefore, some institutes may be concerned that practice guidelines preclude their expertise and enforce recommendations that present others’ experiences. The varying intraoperative findings, endorsed by surgeons’ experience, may not be recognized as efficiently by guidelines, which are limited by available studies, which do not necessarily present all clinical data [44, 86].
On the contrary, some evidence-based recommendations are derived from studies, conducted in highly equipped institutes, and recruited highly compliant women. Although these studies may provide evidence of high quality, their results may be challenging to reproduce or concerning to adopt. For example, “leaving the placenta in situ” is an acceptable approach for uterine preservation by many international guidelines and is supported over many other approaches that are globally more prevalent, yet less studied. Nevertheless, “leaving the placenta in situ” is seldom performed as indicated by surveys that screen experts’ preference in management of PAS [97, 138, 139]. This may be attributed, in part, to complexity of follow-up and prolonged recovery course associated with this approach. In addition, many providers may be inconvenient with risks of serious complications, especially if patient compliance or institutional experience cannot be granted.
A survey of 36 experts in 2017, mainly based in Europe and Asia, showed that 61% perform primary cesarean hysterectomy as their first-line approach compared to 39% who opt for uterus-preserving procedures as a routine practice. Twenty eight percent of experts use partial myometrial resection and 17% use cervical tamponade. Atrial embolization is used by 50% of experts and 47% use intra-arterial balloons. In addition, 17 % of participants use methotrexate in their protocols [138]. This practice does not show substantial consistency with internationally recognized guidelines. Indeed, PAS practice is globally inconsistent, and data derived from different regions may vary. In a survey involving 508 of SMFM members, 14.9% report performing uterus-preserving procedures [139]. Nevertheless, data from the same region may not be consistent as well [97].
Validity of Established Practice: Why Does Established Practice Not Steer Guidelines?
As previously discussed, cesarean hysterectomy is considered the treatment of choice and the safest surgical approach in cases of PAS. However, international surveys revealed that many obstetricians consider uterus-preserving approaches their primary management of PAS even if not supported by evidence-based recommendations [138, 139]. Despite numerous studies that appraise a variety of uterus-preserving procedures, none of these procedures has been recognized as a standard management by current guidelines [140,141,142]. This fact highlights the gap between evidence-based guidelines and actual practice in many regions although clinical studies, used to create evidence, are anticipated to emerge from and appraise contemporary practice.
One of the main explanations of this gap is rarity of the condition, which makes it challenging for obstetricians to investigate their proposed approaches on a large population. A recent review of conservative managements of PAS reported that 54% and 89% of available studies recruited less than 20 patients and less than 50 patients, respectively [36]. These small studies may only show descriptive results and may not be eligible for more robust statistical analysis, which is required to yield definite conclusions such as regression analysis. Similarly, experimental approaches are almost always tested through single-arm studies with small sample sizes or case series [143, 144]. To a large extent, PAS is inherently deprived of randomized clinical trials, which provide a high level of evidence, due to difficult recruitment and ethical restrictions to experimental research in life-threatening conditions. Prospective studies are not commonly conducted, probably due to difficult requirement as well. Thus, poor quality of most published data limits their impact on evidence-based guidelines [145,146,147].
Case reports and case series are frequently reported particularly to assess novel approaches in management of PAS [71, 146,147,148,149,150,151,152,153]. Again, these studies permit limited statistical inference. Moreover, they typically review a few surgeon-selected cases who were managed by a particular approach rather than a controlled study of all eligible women with definite preoperative and intraoperative selection criteria that permit reproducibility of outcomes. This type of studies is highly subjected to publication bias since authors may document cases that went well rather than those who had major complications or even died, resulting in possible underreporting of complications of these procedures. Many of the published procedures are surgeon- or institution-based, meaning that they convey their established experience, which may not be easily reproduced if a novice team tries the same approach. Moreover, studying these procedures by a different team in a different institute is unlikely to receive ethical approval given the limited supportive data of their safety.
For similar reasons, systematic reviews on PAS studies are limited. Trials to review available data to build stronger conclusions are confronted with significant heterogeneity in study design and outcomes [36, 140, 142, 154]. Many of these studies are associated with significant concerns such as considering missing information as a non-occurred event [140]. Several novel procedures are proposed and appraised with only a few of them undergoing further validation by other investigators, resulting in numerous isolated techniques associated with limited data. Assessment of long-term outcomes, including fertility outcomes, of most studies is deficient due to lack of long-term follow-up [141]. Documentation of degree of placental invasion and size of myometrial invasion is also deficient in many studies. Thereby, systematic reviews cannot confidently ascertain that a procedure can be safely recommended to all women with PAS [140, 142].
With scarcity of PAS patients, the amount of wasted data from unpublished cases remains a frustrating concern. A recent systematic review reported that all recent studies that investigated uterine preservation were conducted in 17 countries only, and more than 50% of them were conducted in China [36]. This indicates that current data are not presentative of global practice and that there is significant leak of precious information since most institutes do not publish their data. The lack of PAS-focused clinical researchers in these institutes is the likely explanation.
These concerns highlight the importance of multicenter studies, which can solve recruitment issues and cohort size, and reach centers that do not participate in PAS research even if clinical researchers are not readily available in these centers. Large retrospective data can yield an acceptable level of evidence to guide further multicenter prospective studies or clinical trials without evoking significant ethical concerns. It remains an ongoing challenge that current recommendations do not provide definite preoperative and intraoperative criteria to determine eligibility for each management option. Thus, it is also important to evaluate a complete management protocol, rather than a procedure, where each management is considered based on certain criteria, in order to establish a safe platform for management of women with PAS.
Conclusion
Cesarean hysterectomy is the primary management in women with PAS. Uterus-preserving procedures should only be considered on individual basis and women should be carefully counseled on their possible risks. With the rising incidence of PAS cases, clinical researchers should actively collaborate to utilize expanding data in order to establish contemporary management plans. Future studies should consider the role of selective protocols rather than individual procedures, and multicenter studies should be more frequently conducted to overcome inherent limitations to PAS-related research.
References
Irving F. A study of placenta accreta. Surg Gynecol Obstet. 1937;64:178–200.
Clausen C, Lönn L, Langhoff-Roos J. Management of placenta percreta: a review of published cases. Acta Obstet Gynecol Scand. 2014;93(2):138–43.
Amsalem H, Kingdom JC, Farine D, Allen L, Yinon Y, D’Souza DL, et al. Planned caesarean hysterectomy versus “conserving” caesarean section in patients with placenta accreta. J Obstet Gynaecol Can. 2011;33(10):1005–10.
Jauniaux E, Collins SL, Jurkovic D, Burton GJ. Accreta placentation: a systematic review of prenatal ultrasound imaging and grading of villous invasiveness. Am J Obstet Gynecol. 2016;215(6):712–21.
Jauniaux E, Chantraine F, Silver R, Langhoff-Roos J, FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. Int J Gynaecol Obstet. 2018;140(3):265–73.
Accreta P. Committee Opinion No. 529. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120:207–11.
Jauniaux E, Alfirevic Z, Bhide A, Belfort M, Burton G, Collins S, et al. Placenta praevia and placenta accreta: diagnosis and management: green-top guideline No. 27a. BJOG. 2019;126(1):e1–e48.
Hobson SR, Kingdom JC, Murji A, Windrim RC, Carvalho JC, Singh SS, et al. No. 383-screening, diagnosis, and management of placenta accreta spectrum disorders. J Obstet Gynaecol Can. 2019;41(7):1035–49.
Royal Australian and New Zealand College of Obstetricians and Gynaecologists. placenta accreta. https://ranzcog.edu.au/statements-guidelines/obstetrics/placenta-accreta-(c-obs-20). Accessed on Jan 20th, 2021. 2015
Cahill AG, Beigi R, Heine RP, Silver RM, Wax JR. Placenta Accreta Spectrum. Am J Obstet Gynecol. 2018;219(6):B2–B16.
McDonnell N, Kennedy D, Long L, Gallagher-Swann M, Paech MJ. The development and implementation of an obstetric cell salvage service. Anaesth Intensive Care. 2010;38(3):492–9.
Elagamy A, Abdelaziz A, Ellaithy M. The use of cell salvage in women undergoing cesarean hysterectomy for abnormal placentation. Int J Obstet Anesth. 2013;22(4):289–93.
Lew E. Tagore SJSmj. Implementation of an obstetric cell salvage service in a tertiary women’s hospital. 2015;56(8):445.
Allen L, Jauniaux E, Hobson S, Papillon-Smith J, Belfort MA, Diagnosis FPA, et al. FIGO consensus guidelines on placenta accreta spectrum disorders: Nonconservative surgical management. Int J Gynaecol Obstet. 2018;140(3):281–90.
Chiang Y-C, Shih J-C, Lee C-N. Septic shock after conservative management for placenta accreta. Taiwan J Obstet Gynecol. 2006;45(1):64–6.
ACOG Practice Bulletin No. 95: anemia in pregnancy. Obstet Gynecol. 2008;112(1):201–7.
Eller AG, Bennett MA, Sharshiner M, Masheter C, Soisson AP, Dodson M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011;117(2 Pt 1):331–7.
Shamshirsaz AA, Fox KA, Erfani H, Clark SL, Salmanian B, Baker BW, et al. Multidisciplinary team learning in the management of the morbidly adherent placenta: outcome improvements over time. Am J Obstet Gynecol. 2017;216(6):612. e1–5.
Smulian JC, Pascual A-L, Hesham H, Qureshey E, Bijoy Thomas M, Depuy AM, et al. Invasive placental disease: the impact of a multi-disciplinary team approach to management. J Matern Fetal Neonatal Med. 2017;30(12):1423–7.
Shamshirsaz AA, Fox KA, Salmanian B, Diaz-Arrastia CR, Lee W, Baker BW, et al. Maternal morbidity in patients with morbidly adherent placenta treated with and without a standardized multidisciplinary approach. Am J Obstet Gynecol. 2015;212(2):218. e1–9.
Al-Khan A, Gupta V, Illsley NP, Mannion C, Koenig C, Bogomol A, et al. Maternal and fetal outcomes in placenta accreta after institution of team-managed care. Reprod Sci. 2014;21(6):761–71.
Smulian JC, Pascual A-L, Hesham H, Qureshey E, Bijoy Thomas M. Depuy AM, et al. Invasive placental disease: the impact of a multi-disciplinary team approach to management. 2017;30(12):1423–7.
Brennan DJ, Schulze B, Chetty N, Crandon A, Petersen SG, Gardener G, et al. Surgical management of abnormally invasive placenta: a retrospective cohort study demonstrating the benefits of a standardized operative approach. Acta Obstet Gynecol Scand. 2015;94(12):1380–6.
Chestnut DH, Dewan DM, Redick LF, Caton D, Spielman FJ. Anesthetic management for obstetric hysterectomy: a multi-institutional study. Anesthesiology. 1989;70(4):607–10.
Eller A, Porter T, Soisson P, Silver R. Optimal management strategies for placenta accreta. BJOG Int J Obstet Gynaecol. 2009;116(5):648–54.
Angstmann T, Gard G, Harrington T, Ward E, Thomson A, Giles W. Surgical management of placenta accreta: a cohort series and suggested approach. Am J Obstet Gynecol. 2010;202(1):38. e1–9.
Fox KA, Shamshirsaz AA, Carusi D, Secord AA, Lee P, Turan OM, et al. Conservative management of morbidly adherent placenta: expert review. Am J Obstet Gynecol. 2015;213(6):755–60.
Skoll A, Boutin A, Bujold E, Burrows J, Crane J, Geary M, et al. No. 364-antenatal corticosteroid therapy for improving neonatal outcomes. J Obstet Gynaecol Can. 2018;40(9):1219–39.
Eller A, Porter T, Soisson P, Silver RM. Optimal management strategies for placenta accreta. BJOG. 2009;116(5):648–54.
Warshak CR, Ramos GA, Eskander R, Benirschke K, Saenz CC, Kelly TF, et al. Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet Gynecol. 2010;115(1):65–9.
Seoud M, Nasr R, Berjawi G, Zaatari G, Seoud T, Shatila A, et al. Placenta accreta: Elective versus emergent delivery as a major predictor of blood loss. J Neonatal Perinatal Med. 2017;10(1):9–15.
Belfort MA. Indicated preterm birth for placenta accreta. Seminars in perinatology. Elsevier; 2011.
Jauniaux E, Hussein AM, Fox KA, Collins SL. New evidence-based diagnostic and management strategies for placenta accreta spectrum disorders. Best Pract Res Clin Obstet Gynaecol. 2019;61:75–88.
Rosenbloom JI, Hirshberg JS, Stout MJ, Cahill AG, Macones GA, Tuuli MG. Clinical Diagnosis of placenta Accreta and Clinicopathological outcomes. Am J Perinatol. 2019;36(2):124.
Aitken K, Cram J, Raymond E, Okun N, Allen L, Windrim R. “Mobile” medicine: a surprise encounter with placenta percreta. J Obstet Gynaecol Can. 2014;36(5):377.
Abd Elazeem HAS, Saad MM, Ahmed IA, Sayed EG, AlMahdy AM, Atef F, et al. High-intensity focused ultrasound in management of placenta accreta spectrum: a systematic review. Int J Gynaecol Obstet. 2020;151(3):325–32.
Breymann C, Milman N, Mezzacasa A, Bernard R, Dudenhausen J. Ferric carboxymaltose vs. oral iron in the treatment of pregnant women with iron deficiency anemia: an international, open-label, randomized controlled trial (FER-ASAP). J Perinat Med. 2017;45(4):443–53.
Tam Tam KB, Dozier J, Martin JN Jr. Approaches to reduce urinary tract injury during management of placenta accreta, increta, and percreta: a systematic review. J Matern Fetal Neonatal Med. 2012;25(4):329–34.
Norris BL, Everaerts W, Posma E, Murphy DG, Umstad MP, Costello AJ, et al. The urologist's role in multidisciplinary management of placenta percreta. BJU Int. 2016;117(6):961–5.
Wright JD, Silver RM, Bonanno C, Gaddipati S, Lu Y-S, Simpson LL, et al. Practice patterns and knowledge of obstetricians and gynecologists regarding placenta accreta. J Matern Fetal Neonatal Med. 2013;26(16):1602–9.
Matsubara S, Kuwata T, Usui R, Watanabe T, Izumi A, Ohkuchi A, et al. Important surgical measures and techniques at cesarean hysterectomy for placenta previa accreta. Acta Obstet Gynecol Scand. 2013;92(4):372–7.
Mavrides E, Allard S, Chandraharan E, Collins P, Green L, Hunt B, et al. Prevention and management of postpartum haemorrhage. Am J Obstet Gynecol. 2016;124(5):e106–e49.
Green L, Connolly C, Cooper T, Cho G, Allard S. Blood transfusion in obstetrics, guideline no. 47. JLRCoO, Gynaecologists. 2015;
Brookfield KF, Goodnough LT, Lyell DJ, Butwick AJ. Perioperative and transfusion outcomes in women undergoing cesarean hysterectomy for abnormal placentation. Transfusion. 2014;54(6):1530–6.
Taylor N, Russell R. Anaesthesia for abnormally invasive placenta: a single-institution case series. Int J Obstet Anesth. 2017;30:10–5.
Muñoz L, Mendoza G, Gomez M, Reyes L, Arevalo JJ. Anesthetic management of placenta accreta in a low-resource setting: a case series. Int J Obstet Anesth. 2015;24(4):329–34.
Kocaoglu N, Gunusen I, Karaman S, Ergenoglu AM, Firat V. Management of anesthesia for cesarean section in parturients with placenta previa with/without placenta accreta: a retrospective study. Ginekol Pol. 2012;83(2)
Nguyen-Lu N, Carvalho JCA, Windrim R, Allen L, Balki M. Mode of anesthesia and clinical outcomes of patients undergoing Cesarean delivery for invasive placentation: a retrospective cohort study of 50 consecutive cases. Can J Anaesth. 2016;63(11):1233–44.
Butwick A, Carvalho B, El-Sayed Y. Risk factors for obstetric morbidity in patients with uterine atony undergoing caesarean delivery. Br J Anaesth. 2014;113(4):661–8.
Hong J, Jee Y, Yoon H, Kim S. Comparison of general and epidural anesthesia in elective cesarean section for placenta previa totalis: maternal hemodynamics, blood loss and neonatal outcome. Int J Obstet Anesth. 2003;12(1):12–6.
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195–283.
Shakur H, Roberts I, Fawole B, Chaudhri R, El-Sheikh M, Akintan A, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105–16.
Sentilhes L, Kayem G, Chandraharan E, Palacios-Jaraquemada J, Jauniaux E, Diagnosis FPA, et al. FIGO consensus guidelines on placenta accreta spectrum disorders: conservative management. Int J Gynaecol Obstet. 2018;140(3):291–8.
Woldu SL, Ordonez MA, Devine PC, Wright JD. Urologic considerations of placenta accreta: a contemporary tertiary care institutional experience. Urol Int. 2014;93(1):74–9.
Belfort MA, Shamshirsaz AA, Fox KA. A technique to positively identify the vaginal fornices during complicated postpartum hysterectomy. Am J Obstet Gynecol. 2017;217(2):222. e1–3.
Camuzcuoglu A, Vural M, Hilali NG, Incebiyik A, Yuce HH, Kucuk A, et al. Surgical management of 58 patients with placenta praevia percreta. Wien Klin Wochenschr. 2016;128(9):360–6.
Walker MG, Pollard L, Talati C, Carvalho JC, Allen LM, Kachura J, et al. Obstetric and anaesthesia checklists for the management of morbidly adherent placenta. J Obstet Gynaecol Can. 2016;38(11):1015–23.
Jaraquemada JMP, Pesaresi M, Nassif JC, Hermosid S. Anterior placenta percreta: surgical approach, hemostasis and uterine repair. Acta Obstet Gynecol Scand. 2004;83(8):738–44.
American College of Obstetricians and Gynecologists. ACOG practice bulletin: clinical management guidelines for obstetrician-gynecologists number 76, October 2006: postpartum hemorrhage. Obstet Gynecol. 2006;108(4):1039–47.
Leduc D, Senikas V, Lalonde AB, Ballerman C, Biringer A, Delaney M, et al. Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. J Obstet Gynaecol Can. 2009;31(10):980–93.
Organization WH. WHO recommendations for the prevention and treatment of postpartum haemorrhage: World Health Organization; 2012.
Lalonde A, Motherhood FS. Prevention and treatment of postpartum hemorrhage in low-resource settings. Int J Gynaecol Obstet. 2012;117(2):108–18.
Sentilhes L, Vayssière C, Deneux-Tharaux C, Aya AG, Bayoumeu F, Bonnet M-P, et al. Postpartum hemorrhage: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF): in collaboration with the French Society of Anesthesiology and Intensive Care (SFAR). Eur J Obstet Gynecol Reprod Biol. 2016;198:12–21.
Fitzpatrick K, Sellers S, Spark P, Kurinczuk J, Brocklehurst P, Knight M, et al. The management and outcomes of placenta accreta, increta, and percreta in the UK: a population-based descriptive study. BJOG. 2014;121(1):62–71.
Kayem G, Anselem O, Schmitz T, Goffinet F, Davy C, Mignon A, et al. Conservative versus radical management in cases of placenta accreta: a historical study. J Gynecol Obstet Biol Reprod (Paris). 2007;36(7):680–7.
Palacios-Jaraquemada J. One-step conservative surgery for abnormal invasive placenta (Placenta Accreta–Increta–Percreta). IJRCOG. 2012:263–71.
Palacios-Jaraquemada JM. Diagnosis and management of placenta accreta. Best Pract Res Clin Obstet Gynaecol. 2008;22(6):1133–48.
Palacios-Jaraquemada JM. Placental adhesive disorders: Walter de Gruyter; 2012.
Chandraharan E, Rao S, Belli A-M, Arulkumaran S. The Triple-P procedure as a conservative surgical alternative to peripartum hysterectomy for placenta percreta. Int J Gynaecol Obstet. 2012;117(2):191–4.
Vinas MT, Belli A, Arulkumaran S, Chandraharan E. Prevention of postpartum hemorrhage and hysterectomy in patients with morbidly adherent placenta: a cohort study comparing outcomes before and after introduction of the Triple-P procedure. Ultrasound Obstet Gynecol. 2015;46(3):350–5.
Shazly SAE, Badee AY, Ali MK. The use of multiple 8 compression suturing as a novel procedure to preserve fertility in patients with placenta accreta: case series. Aust N Z J Obstet Gynaecol. 2012;52(4):395–9.
Huang G, Zhou R, Hu Y. A new suture technique for cesarean delivery complicated by hemorrhage in cases of placenta previa accreta. Int J Gynaecol Obstet. 2014;124(3):262–3.
Kaplanoglu M, Kaplanoglu D, Koyuncu O. A different approach to placenta previa accreta: intrauterine gauze compress combined B-Lynch uterine compression suture. Clin Exp Obstet Gynecol. 2015;42(1):53–6.
Li GT, Li XF, Li J, Liu YJ, Xu HM. Reflexed compression suture for the management of atonic postpartum hemorrhage with an abnormally adherent placenta. Gynecol Obstet Invest. 2015;80(4):228–33.
Li G-T, Li X-F, Wu B, Li GJ. Longitudinal parallel compression suture to control postopartum hemorrhage due to placenta previa and accrete. Gynecol Obstet Invest. 2016;55(2):193–7.
El Gelany SA, Abdelraheim AR, Mo’men MM, El-Rab MTG, Yousef AM, Ibrahim EM, et al. The cervix as a natural tamponade in postpartum hemorrhage caused by placenta previa and placenta previa accreta: a prospective study. BMC Pregnancy Childbirth. 2015;15(1):1–7.
Allam M, B-Lynch C. The B-Lynch and other uterine compression suture techniques. Int J Gynaecol Obstet. 2005;89(3):236–41.
Baskett TF. Uterine compression sutures for postpartum hemorrhage: efficacy, morbidity, and subsequent pregnancy. Obstet Gynecol. 2007;110(1):68–71.
Shahin AY, Farghaly TA, Mohamed SA, Shokry M, Abd-El-Aal DEM, Youssef MA. Bilateral uterine artery ligation plus B-lynch procedure for atonic postpartum hemorrhage with placenta accreta. Int J Gynecol Obstet. 2010;108(3):187–90.
Doumouchtsis S, Nikolopoulos K, Talaulikar V, Krishna A, Arulkumaran S. Menstrual and fertility outcomes following the surgical management of postpartum haemorrhage: a systematic review. BJOG Int J Obstet Gynaecol. 2014;121(4):382–8.
CON-PAS registry. Middle-East Obstetrics and Gynecology Graduate Education (MOGGE) Foundation. https://www.mogge-obgyn.com/con-pas-registry. Last accessed: April 6, 2021.
Durukan H, Durukan ÖB, Yazıcı FG. Placenta accreta spectrum disorder: a comparison between fertility-sparing techniques and hysterectomy. J Obstet Gynaecol. 2020:1–7.
Bisschop CNS, Schaap TP, Vogelvang TE, Scholten PC. Invasive placentation and uterus preserving treatment modalities: a systematic review. Arch Gynecol Obstet. 2011;284(2):491–502.
Sentilhes L, Goffinet F, Kayem G. Management of placenta accreta. Acta Obstet Gynecol Scand. 2013;92(10):1125–34.
Sentilhes L, Ambroselli C, Kayem G, Provansal M, Fernandez H, Perrotin F, et al. Maternal outcome after conservative treatment of placenta accreta. Obstet Gynecol. 2010;115(3):526–34.
Pather S, Strockyj S, Richards A, Campbell N, de Vries B, Ogle RJA, et al. Maternal outcome after conservative management of placenta percreta at caesarean section: a report of three cases and a review of the literature. Aust N Z J Obstet Gynaecol. 2014;54(1):84–7.
Widemann BC, Adamson PC. Understanding and managing methotrexate nephrotoxicity. Oncologist. 2006;11(6):694–703.
Lin K, Qin J, Xu K, Hu W, Lin J. Methotrexate management for placenta accreta: a prospective study. Arch Gynecol Obstet. 2015;291(6):1259–64.
Isaacs JD Jr, McGehee RP, Cowan BD. Life-threatening neutropenia following methotrexate treatment of ectopic pregnancy: a report of two cases. Obstet Gynecol. 1996;88(4):694–6.
Timmermans S, van Hof AC, Duvekot JJ. Conservative management of abnormally invasive placentation. Obstet Gynecol Surv. 2007;62(8):529–39.
Mussalli GM, Shah J, Berck DJ, Elimian A, Tejani N, Manning FA. Placenta accreta and methotrexate therapy: three case reports. J Perinatol. 2000;20(5):331–4.
Legendre G, Zoulovits FJ, Kinn J, Senthiles L, Fernandez H. Conservative management of placenta accreta: hysteroscopic resection of retained tissues. J Minim Invasive Gynecol. 2014;21(5):910–3.
Mazzon I, Favilli A, Grasso M, Horvath S, Gerli S. Is the cold loop hysteroscopic technique a myometrial sparing treatment for placenta accreta residuals in a puerperal uterus? J Matern Fetal Neonatal Med. 2016;29(10):1613–6.
Bai Y, Luo X, Li Q, Yin N, Fu X, Zhang H, et al. High-intensity focused ultrasound treatment of placenta accreta after vaginal delivery: a preliminary study. Ultrasound Obstet Gynecol. 2016;47(4):492–8.
Jauniaux E, Bhide A. Prenatal ultrasound diagnosis and outcome of placenta previa accreta after cesarean delivery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2017;217(1):27–36.
Hudon L, Belfort MA, Broome DR. Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv. 1999;54(11):156–64.
Esakoff TF, Handler SJ, Granados JM, Caughey AB. PAMUS: placenta accreta management across the United States. J Matern Fetal Neonatal Med. 2012;25(6):761–5.
Selman AE. Caesarean hysterectomy for placenta praevia/accreta using an approach via the pouch of Douglas. BJOG. 2016;123(5):815–9.
Belfort MA, Shamshiraz AA, Fox K. Minimizing blood loss at cesarean-hysterectomy for placenta previa percreta. Am J Obstet Gynecol. 2017;216(1):78. e1–2.
Rossetti D, Vitale SG, Bogani G, Rapisarda AMC, Gulino FA, Frigerio L. Usefulness of vessel-sealing devices for peripartum hysterectomy: a retrospective cohort study. Updates Surg. 2015;67(3):301–4.
Arendas K, Lortie KJ, Singh SS. Delayed laparoscopic management of placenta increta. J Obstet Gynaecol Can. 2012;34(2):186–9.
Smith DD, Perez-Delboy A, Burke WM, Tergas AI. Buttock necrosis after uterine artery embolization for delayed hysterectomy in placenta percreta. Case Rep Obstet Gynecol. 2016;2016:6921280.
Rupley DM, Tergas AI, Palmerola KL, Burke WM. Robotically assisted delayed total laparoscopic hysterectomy for placenta percreta. Gynecol Oncol Rep. 2016;17:53–5.
Hussein AM, Dakhly DMR, Raslan AN, Kamel A, Abdel Hafeez A, Moussa M, et al. The role of prophylactic internal iliac artery ligation in abnormally invasive placenta undergoing caesarean hysterectomy: a randomized control trial. J Matern Fetal Neonatal Med. (1476–4954 (Electronic)). 2019;32(20):3386–92.
Salim R, Chulski A, Romano S, Garmi G, Rudin M, Shalev E, et al. Precesarean prophylactic balloon catheters for suspected placenta accreta: a randomized controlled trial. Obstet Gynecol. 2015;126(5):1022–8.
Walker MG, Allen L, Windrim RC, Kachura J, Pollard L, Pantazi S, et al. Multidisciplinary management of invasive placenta previa. J Obstet Gynaecol Can. 2013;35(5):417–25.
Sewell MF, Rosenblum D, Ehrenberg H. Arterial embolus during common iliac balloon catheterization at cesarean hysterectomy. Obstet Gynecol. 2006;108(3):746–8.
Matsueda S, Hidaka N, Kondo Y, Fujiwara A, Fukushima K. Kato KJJoO, et al. External iliac artery thrombosis after common iliac artery balloon occlusion during cesarean hysterectomy for placenta accreta in cervico-isthmic pregnancy. 2015;41(11):1826–30.
Gagnon J, Boucher L, Kaufman I, Brown R, Moore A. Iliac artery rupture related to balloon insertion for placenta accreta causing maternal hemorrhage and neonatal compromise. Can J Anaesth. 2013;60(12):1212–7.
Chen L, Wang X, Wang H, Li Q, Shan N, Qi H, et al. Clinical evaluation of prophylactic abdominal aortic balloon occlusion in patients with placenta accreta: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):1–8.
Committee P. Society for Maternal–Fetal Medicine, Belfort MA. Placenta accreta. Am J Obstet Gynecol. 2010;203(5):430–9.
Shamshirsaz AA, Carusi D, Shainker SA, Einerson B, Khandelwal M, Erfani H, et al. Characteristics and outcomes of placenta accreta spectrum in twins versus singletons: a study from the pan American Society for Placenta Accreta Spectrum (PAS 2). Am J Obstet Gynecol. 2020;222(6):624–5.
Viñas MT, Chandraharan E, Moneta M, Belli A. The role of interventional radiology in reducing haemorrhage and hysterectomy following caesarean section for morbidly adherent placenta. Clin Radiol. 2014;69(8):e345–e51.
Bouvier A, Sentilhes L, Thouveny F, Bouet PE, Gillard P, Willoteaux S, et al. Planned caesarean in the interventional radiology cath lab to enable immediate uterine artery embolization for the conservative treatment of placenta accreta. Clin Radiol. 2012;67(11):1089–94.
Dilauro MD, Dason S, Athreya S. Prophylactic balloon occlusion of internal iliac arteries in women with placenta accreta: literature review and analysis. Clin Radiol. 2012;67(6):515–20.
Clausen C, Stensballe J, Albrechtsen CK, Hansen MA, Lönn L, Langhoff-Roos J. Balloon occlusion of the internal iliac arteries in the multidisciplinary management of placenta percreta. Acta Obstet Gynecol Scand. 2013;92(4):386–91.
D'Souza DL, Kingdom JC, Amsalem H, Beecroft JR, Windrim RC, Kachura JR. Conservative management of invasive placenta using combined prophylactic internal iliac artery balloon occlusion and immediate postoperative uterine artery embolization. Can Assoc Radiol J. 2015;66(2):179–84.
Chou MM, Kung HF, Hwang JI, Chen WC, Tseng JJ. Temporary prophylactic intravascular balloon occlusion of the common iliac arteries before cesarean hysterectomy for controlling operative blood loss in abnormal placentation. Taiwanese Journal of Obstetrics and Gynecology. 2015;54(5):493–8.
Duan XH, Wang YL, Han XW, Chen ZM, Chu QJ, Wang L, et al. Caesarean section combined with temporary aortic balloon occlusion followed by uterine artery embolisation for the management of placenta accreta. Clin Radiol. 2015;70(9):932–7.
Wei X, Zhang J, Chu Q, Du Y, Xing N, Xu X, et al. Prophylactic abdominal aorta balloon occlusion during caesarean section: a retrospective case series. Int J Obstet Anesth. 2016;27:3–8.
Wu Q, Liu Z, Zhao X, Liu C, Wang Y, Chu Q, et al. Outcome of pregnancies after balloon occlusion of the Infrarenal abdominal aorta during caesarean in 230 patients with placenta Praevia Accreta. Cardiovasc Intervent Radiol. 2016;39(11):1573–9.
Xie L, Wang Y, Luo F-Y, Man Y-C, Zhao X-L. Prophylactic use of an infrarenal abdominal aorta balloon catheter in pregnancies complicated by placenta accreta. J Obstet Gynaecol. 2017;37(5):557–61.
ACOG committee opinion. Placenta accreta. Number 266, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;77(1):77–8.
Soyer P, Sirol M, Fargeaudou Y, Bour L, Morel O, Dohan A, et al. Placental vascularity and resorption delay after conservative management of invasive placenta: MR imaging evaluation. Eur Radiol. 2013;23(1):262–71.
Organization WH. WHO handbook for guideline development: World Health Organization; 2014.
Green S, Pjehl J. Clinical practice guidelines: a guide to better practice, not a recipe for uniformity. Aust J Physiother. 2003;49(1):3–6.
Geleris P, Boudoulas H. Problems related to the application of guidelines in clinical practice: a critical analysis. Hell J Cardiol. 2011;52(2):97–102.
Wang Z, Norris SL, Bero L. Implementation plans included in World Health Organisation guidelines. Implement Sci. 2015;11(1):1–9.
Chong CC. Pros and cons of clinical practice based on guidelines. Hong Kong Med J. 2018;24:440–1.
Tinetti ME, Fried T. The end of the disease era. Am J Med. 2004;116(3):179–85.
Grol R, Dalhuijsen J, Thomas S, Rutten G, Mokkink H. Attributes of clinical guidelines that influence use of guidelines in general practice: observational study. BMJ. 1998;317(7162):858–61.
Shazly SA, Laughlin-Tommaso SK, Dowdy SC, Famuyide AO. Staging for low malignant potential ovarian tumors: a global perspective. Am J Obstet Gynecol. 2016;215(2):153–68. e2.
Fox J, Patkar V, Chronakis I, Begent R. From practice guidelines to clinical decision support: closing the loop. J R Soc Med. 2009;102(11):464–73.
Flory N, Bissonnette F, Binik YM. Psychosocial effects of hysterectomy: literature review. J Psychosom Res. 2005;59(3):117–29.
Naughton MJ, McBee WL. Health-related quality of life after hysterectomy. Clin Obstet Gynecol. 1997;40(4):947–57.
Kjerulff KH, Langenberg PW, Rhodes JC, Harvey LA, Guzinski GM, Stolley PD. Effectiveness of hysterectomy. Obstet Gynecol. 2000;95(3):319–26.
Marek K, Dimter A, Jawor M, Dudek D. Anxiety-depressive disorders in women after hysterectomy. Literature review. Psychiatria polska. 2001;35(5):763–9.
Cal M, Ayres-de-Campos D, Jauniaux E. International survey of practices used in the diagnosis and management of placenta accreta spectrum disorders. Int J Gynaecol Obstet. 2018;140(3):307–11.
Jolley JA, Nageotte MP, Wing DA, Shrivastava VK. Management of placenta accreta: a survey of maternal-fetal medicine practitioners. J Matern Fetal Neonatal Med. 2012;25(6):756–60.
Matsuzaki S, Yoshino K, Endo M, Kakigano A, Takiuchi T, Kimura T. Conservative management of placenta percreta. Int J Gynaecol Obstet. 2018;140(3):299–306.
Mei J, Wang Y, Zou B, Hou Y, Ma T, Chen M, et al. Systematic review of uterus-preserving treatment modalities for abnormally invasive placenta. J Obstet Gynaecol. 2015;35(8):777–82.
Steins Bisschop CN, Schaap TP, Vogelvang TE, Scholten PC. Invasive placentation and uterus preserving treatment modalities: a systematic review. Arch Gynecol Obstet. 2011;284(2):491–502.
Pinas-Carrillo A, Chandraharan E. Conservative surgical approach: the triple P procedure. Best Pract Res Clin Obstet Gynaecol. 2020;
Shmakov RG, Vinitskiy AA, Chuprinin VD, Yarotskaya EL, Sukhikh GT. Alternative approaches to surgical hemostasis in patients with morbidly adherent placenta undergoing fertility-sparing surgery. J Matern Fetal Neonatal Med. 2019;32(12):2042–8.
Kallianidis AF, Maraschini A, Danis J, Colmorn LB, Deneux-Tharaux C, Donati S, et al. Epidemiological analysis of peripartum hysterectomy across nine European countries. Acta Obstet Gynecol Scand. 2020;99(10):1364–73.
Palacios-Jaraquemada JM, Fiorillo A, Hamer J, Martinez M, Bruno C. Placenta accreta spectrum: a hysterectomy can be prevented in almost 80% of cases using a resective-reconstructive technique. J Matern Fetal Neonatal Med. 2020:1–8.
Lional KM, Tagore S, Wright AM. Uterine conservation in placenta accrete spectrum (PAS) disorders: a retrospective case series: is expectant management beneficial in reducing maternal morbidity? Eur J Obstet Gynecol Reprod Biol. 2020;254:212–7.
Pather SSS, Richards A, Campbell N, de Vries B, Ogle R. Maternal outcome after conservative management of placenta percreta at caesarean section: a report of three cases and a review of the literature. Aust N Z J Obstet Gynaecol. 2014;54:84–7.
Patabendige M, Sanjeewa JMP, Amarasekara AMAKG, Herath RP. Conservative Management of Placenta Percreta: three cases and a review of the literature regarding conservative Management of Placenta Accreta Spectrum (PAS) disorders. Case Rep Obstet Gynecol. 2020;2020:1–7.
Bai Y, Luo X, Li Q, Yin N, Fu X, Zhang H, Qi H. High-intensity focused ultrasound treatment of placenta accreta after vaginal delivery: a preliminary study. Ultrasound Obstet Gynecol. 2016;47(4):492–8.
Ye M, Yin Z, Xue M, Deng X. High-intensity focused ultrasound combined with hysteroscopic resection for the treatment of placenta accreta. BJOG. 2017;124:71–7.
Jiang X, Tang QL, Yang B, Ye F, Cai L, Wang X, Luo X, Bu H. High-intensity focused ultrasound combined procedures treatment of retained placenta accreta with marked vascularity after abortion or delivery. Int J Hyperth. 2019;36(1):421–7.
Liu Y, Zhang WW, He M, Gong C, Xie B, Wen X, Li D, Zhang L. Adverse effect analysis of high-intensity focused ultrasound in the treatment of benign uterine diseases. Int J Hyperth. 2018;35(1):56.
Palacios-Jaraquemada JM, D'Antonio F, Buca D, Fiorillo A, Larraza P. Systematic review on near miss cases of placenta accreta spectrum disorders: correlation with invasion topography, prenatal imaging, and surgical outcome. J Matern Fetal Neonatal Med. 2020;33(19):3377–84.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Shazly, S.A. et al. (2023). Evidence-Based Management of Placenta Accreta Spectrum. In: Shazly, S.A., Nassr, A.A. (eds) Placenta Accreta Spectrum. Springer, Cham. https://doi.org/10.1007/978-3-031-10347-6_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-10347-6_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-10346-9
Online ISBN: 978-3-031-10347-6
eBook Packages: MedicineMedicine (R0)