Abstract
Percutaneous transluminal angioplasty (PTA) is the standard endovascular treatment for peripheral artery disease. To reduce acute procedural complications and optimize long-term clinical response, vessel preparation has become more common to modify plaque and increase luminal gain prior to PTA. Innovative methods for vessel preparation are specifically needed for long, complex lesions that may involve more time, additional equipment, and increased risk for long-term complications. The FLEX Vessel Prep™ (FLEX VP) System is a novel device designed to modify plaque, improve vessel compliance, and facilitate drug delivery by creating longitudinal, controlled-depth, circumferential micro-incisions along the entire length of a lesion using a retrograde pullback approach. FLEX VP is currently indicated for use with PTA catheters to facilitate dilation of stenoses in the femoral and popliteal arteries. This chapter describes FLEX VP’s mechanism of action and summarizes current clinical results in patients with peripheral arterial disease. The FLEX VP System provides safe plaque modification and vessel preparation via consistent, controlled-depth, circumferential micro-incisions in complex, mixed morphology lesions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Longitudinal incisions
- Micro-incisions
- Controlled-depth
- FLEX Vessel Prep
- Vessel preparation
- Plaque modification
- Femoral artery
- Popliteal artery
- Angioplasty
- Peripheral artery disease
Peripheral artery disease (PAD) involving the lower extremities is an increasingly prevalent problem. It is estimated that worldwide more than >200 million people have PAD [1]. The standard practice for endovascular treatment of peripheral artery disease is percutaneous transluminal angioplasty (PTA), including plain balloon (POBA) and drug-coated balloons (DCB). The safety and efficacy of PTA compared to surgical revascularizations have been established [2]. PTA is intended to increase luminal gain in the obstructed vessel. Although PTA and DCB are primary therapies, there is risk of uncontrolled dissections, including those that are flow-limiting. Severe dissections can require bailout stenting and have subsequent negative effects on long-term clinical outcomes, including restenosis and the need for future reinterventions [3]. The FLEX Vessel Prep (FLEX VP) System (VentureMed Group, Minneapolis, MN) is a proprietary technology that enables for controlled and predictable plaque modification in long, complex lesions of varying morphology. The FLEX VP System is designed to create longitudinal, controlled-depth, circumferential micro-incisions along the entire length of a lesion that reduce the number and severity of dissections and other complications often seen with other vessel preparation devices. These controlled-depth micro-incisions help reduce the circumferential tension along the entire length of stenoses, improving vessel compliance that enables enhanced luminal gain at lower balloon inflation pressures.
The Clinical Benefit of Reducing Dissections
PTA remains the primary intervention to treat peripheral arterial stenoses [4]. Balloon dilatation can result in uncontrolled dissections that separate the intima from the media of a vessel wall and/or cause injury to the adventitia [5, 6]. The acute vessel damage may range from a superficial plaque disruption to deep, flow-limiting dissections. Dissections are a clinical concern as dissection-induced damage to smooth muscle tissue increases the risk of stenosis due to induction of an inflammatory response, leukocyte recruitment, platelet activation, thrombosis, and neointimal hyperplasia [7,8,9,10,11,12].
Dissections have been reported across a wide range of superficial femoral artery (SFA) and popliteal angioplasties (7–84%) [13,14,15,16,17,18]. However, the reported occurrence and severity of dissection may be underestimated as data from clinical studies that utilize independent core lab review tend to report significantly higher extent and severity of dissections as compared to the dissection data reported from non-adjudicated clinical studies [19]. It has also been noted that intravascular imaging methods such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT) allow for more precise identification of arterial dissections, as compared to conventional angiography, with a comparative analysis demonstrating that IVUS identified four to six times more dissections than angiography [20]. High-grade dissections post balloon angioplasty correlate with reduced patency and increased target lesion revascularization (TLR) [14, 20]. Mild-to-moderate-grade dissections also may be associated with lower patency and higher TLR rates (National Heart, Lung, and Blood Institute [NHLBI] Classification of Dissection) [4]. PTA-induced dissections have been identified as a contributing factor in acute procedure complications, such as bailout stenting, long-term clinical outcomes such as reduced patency, acute occlusions, thrombus formation, in-stent restenosis, and an increased need for future target lesion revascularization (TLR) [4, 14, 16, 20,21,22,23,24]. Minimizing dissection rate and severity are key to successful endovascular procedures.
Plaque morphology and lesion length play a key role in the severity of dissections after angioplasty. It is widely accepted that calcification is a more challenging lesion morphology to treat and often results in higher rates of severe dissections [16, 25,26,27,28]. In a study involving IVUS in coronary and peripheral arteries to assess dissections and calcium burden of the lesion, it was noted that 87% of dissections showed calcium deposits on the same side of the vessel wall as the dissection [25]. Unfortunately, our understanding of calcification’s contribution to dissection rates during endovascular procedures is limited because severely calcified lesions that are associated with higher rates of dissections are routinely excluded as part of trial criteria [4, 28]. In addition, lesion length was found as independent predictor of severe dissection rate [14, 21].
Often dissections are treated with adjunctive therapies, such as stenting, to maximize luminal gain and improve flow dynamics. Another commonly used technique to treat dissections is prolonged balloon inflation. Contributing factors such as the location, depth, and magnitude of dissections determine the treatment algorithm. Minor dissections (Type A or B) may not require further treatment, while more severe (Types C through F) dissections may require a bailout stent. A retrospective analysis of the incidence of post-PTA dissections found an occurrence of 84% [14]. Lesions with Type C–F dissections had a 34% TLR at 6 months, as compared to a 14% TLR for Type A and B dissections or patients with zero dissections identified in the same study [14].
The THUNDER study evaluated the safety and efficacy of a paclitaxel-coated balloon and reported that lesions with Type A and B dissections had statistically similar rates of TLR at 6 months as lesions with Types C through E (33% and 44%, respectively). At 24 months, the TLR rates increased to 43% for Type A and B dissections and to 78% for Type C through E dissections [17]. The prevalence of dissections identified via angiography has been reported to be between 50 and 85% following balloon angioplasty in the SFA [14]. POBA complication rates have been reported to be as high as 30%, including high rates of uncontrolled dissections with higher rates observed in longer lesions with likelihood that angiographically identified dissections are under-reported [20, 29,30,31,32].
Current Methods for Vessel Preparation
Although PTA remains the most common endovascular intervention, the dissections that occur remain uncontrolled and have the potential to impact the patient’s long-term outcomes. Advances in vessel preparation prior to PTA show promise in reducing the risk of severe dissections and long-term adverse consequences. Numerous technologies have been developed to modify the plaque prior to endovascular treatments in order to improve therapeutic response and reduce procedural complications. Additionally, vessel preparation and plaque modification may potentially facilitate the delivery of anti-restenotic drugs across the arterial wall [33, 34]. Current technologies include specialty angioplasty balloons, atherectomy, and intravascular lithotripsy.
Specialty Angioplasty Balloons
Specialty angioplasty balloons include additional features that modify plaque by focal force, static cutting, or scoring. These balloon-based scoring devices utilize the combination of external wires or atherotomes and balloon dilatation to attempt to create controlled dissections by exerting focal force to the lesion [32]. However, limitations of these devices include fixed scoring elements, application of symmetrical focal force even when lesions are asymmetrical, potential requirement for overlapping dilatations, and risk for injury to healthy tissue due to dilatation of more normal vessel segments. A pivotal trial for evaluating intervention of a specialty scoring balloon in 245 patients with SFA/PA lesions reported dissection and stent rates of 26% and 32%, respectively [35].
Atherectomy
Atherectomy is intended to provide lumen gain by removing (debulking) the plaque through cutting, shaving, grinding, or vaporizing. The four current types of atherectomy technologies are directional, rotational, orbital, and laser. Atherectomy has reported advantages in shorter lesions, severely calcified lesions, and longer non-occlusive lesions [36, 37]. However, limitations to atherectomy include the inability to control depth of plaque removal, risk of vessel perforations during debulking, damage to the media and adventitia, and risk of embolization [38,39,40]. Dissection rates related to atherectomy range from 2 to 17% [41,42,43]. In addition to clinical risks, atherectomy may both increase procedure times and require the use of additional procedural resources related to training, capital equipment, extra time with fluoroscopy, additional ancillary products like filter devices, and inventory of multiple size single-use devices [36].
Intravascular Lithotripsy (IVL)
IVL is intended to achieve plaque modification in calcified lesions by using sonic pressure waves to create microfractures or microfissures [22, 44]. IVL relies on energy absorption by calcium and thus may have suboptimal impact on lesions with mixed morphology and/or light calcification. Furthermore, the current device is limited to 300 pulses with longer lesions requiring overlapping treatments for complete coverage. Based on its design, IVL may be best suited for shorter, severely calcified lesions with circumferential calcium deposition [45].
Creating Longitudinal Micro-Incisions to Modify Plaque with Fewer Complications
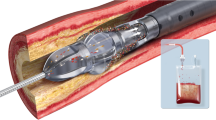
The FLEX VP System is a novel approach to vessel preparation and plaque modification that uses proprietary non-balloon technology to create multiple, longitudinal, controlled-depth micro-incisions across the entire lesion length (Fig. 8.1). These circumferential controlled-depth micro-incisions are an integral part of the design that reduce the number and severity of dissections and other complications (Fig. 8.2). The FLEX VP System is indicated for use with PTA catheters to facilitate dilation of stenoses in the femoral and popliteal arteries and treatment of obstructive lesions of native or synthetic arteriovenous dialysis fistulae. The device is also indicated for the treatment of in-stent restenosis (ISR) of balloon-expandable and self-expanding stents in the peripheral vasculature. The FLEX VP is designed for mixed morphology lesions with a range of characteristics (e.g., long, calcified).
The FLEX VP is an over-the-wire sheathed catheter with a three-strut treatment element at the distal tip. It is compatible with a 6-French sheath and 0.014 in or 0.018 in guidewire and is available in two working lengths (40 cm or 120 cm). The proximal portion of each treatment element strut includes a 0.010 in height microsurgical blade. Once the device is advanced past the lesion, the treatment element (TE) is deployed and expanded, and the catheter is drawn back, allowing the microsurgical blades on the proximal end of each TE strut to independently engage in the lesion and create three parallel, circumferential continuous micro-incisions, with a consistent depth, along the entire length of the lesion. After the first pass, the TE is re-sheathed and advanced again through the lesion, rotated approximately 30 degrees before the treatment element is re-deployed and the retrograde pullback described above is repeated. This process is repeated based on the patient’s disease characteristics. For example, a procedure with 4 passes of the device prepares the artery by performing 12 longitudinal micro-incisions in the lesions (as illustrated in Fig. 8.2 center and right panels). Additional features that benefit the clinician and adoption into current clinical practice include a braided shaft that is engineered to facilitate tracking the pullback performance; an atraumatic tip, with a 2 mm crossing profile that provides trackability and a low risk of perforation; a radiopaque marker band that facilitates placement of the FLEX VP System to treat any length lesion; and a single size that applies to most complex, mixed morphology lesions by self-sizing to the lumen diameter.
Clinical Data in Peripheral Arterial Disease
Clinical data has reported consistent outcome with FLEX VP treatment across long complex lesions [20, 46]. In over 700 peripheral arterial disease patients, average luminal gain following FLEX VP alone was 20–30% with average balloon opening pressure <5 atm and provisional stent rate of <20% in lesions with average length ranging from 136 to 245 mm (see Table 8.1 for study summary details).
Collectively, these data indicate that FLEX VP is effective in a broad range of PAD lesion lengths across real-world plaque morphologies, improves vessel compliance, is associated with reduced rate/grade/severity of dissections, and creates luminal gain without perforations or embolization.
Mechanism of Action
The longitudinal micro-incisions created by FLEX VP are key to the technology’s mechanism of action in several ways. First, the treatment element struts are designed to independently “flex” (adaptively expand and compress) to the contour of the vessel wall morphology (Fig. 8.3). This is in contrast with other vessel preparation or plaque modification technologies that utilize concentric expansion of angioplasty balloons to apply focal force to the vessel wall. The independent, dynamic action of the protective struts of the FLEX VP System enables precise, controlled-depth micro-incisions that self-size to the lesion during the retrograde pullback. The FLEX VP is also indicated for ISR which can be difficult to treat due to the limitations of other vessel prep devices inside a stent (Fig. 8.4).
Minimizing disruption to the elastic lamina during vessel prep reduces the damage to the media and adventitia and associated risk of an inflammatory response leading to lower rates of restenosis [7,8,9,10,11,12]. FLEX VP evaluated in cadaveric tissue demonstrates minimal disruption to the elastic lamina while offering continuous engagement along the treated lesion (Figs. 8.5 and 8.6).
Histology (hematoxylin and eosin stain; H&E) in a tibial cadaveric lesion with an asymmetrical neointima with partial luminal occlusion (left) and a calcified cadaveric SFA lesion (right) post-FLEX VP. Arrows indicate micro-incisions created by FLEX VP used to treat cadaveric popliteal stenosis. Micro-incision depth is equivalent to the blade height (0.25 mm)
Next, the circumferential placement and controlled depth of the micro-incisions improve vessel compliance and enable even lumen gain and controlled expansion of the artery during PTA or DCB. Figure 8.7 provides an optical coherence tomography (OCT) cross-sectional image of pre- and post-different vessel preparation technologies tested in an ISR porcine lesion. Vessel prep technology tested included scoring PTA, direction atherectomy, and FLEX VP. Note the lack of circumferential engagement in alternative technologies as compared to FLEX VP, which demonstrates a consistent circumferential engagement (Fig. 8.8).
FLEX VP Micro-Incisions May Facilitate Drug Delivery
In addition to improving vessel compliance, FLEX VP micro-incisions potentially facilitate the diffusion of anti-restenotic drugs to the target lesions from drug-coated or drug-eluting technologies. SEM evaluation in human cadaver studies confirms the deposition of both sirolimus and paclitaxel anti-restenotic drugs into FLEX VP micro-incisions (Fig. 8.8).
A retrospective clinical study evaluating 12-month outcomes of patients with de novo SFA/PA lesions treated with FLEX VP prior to a DCB reported freedom from TLR rates (>93%) that were comparable to freedom from TLR rates reported for DCBs with published superior performance characteristics [49, 50]. Thus, these encouraging early patency results suggest that vessel preparation with circumferential, controlled-depth, continuous micro-incisions may facilitate DCB drug delivery [33, 34]. Results from this retrospective observational study are currently being investigated in the BELONG prospective study (NCT03721939).
Future Directions
In conclusion, the FLEX VP System provides safe plaque modification and vessel preparation via consistent circumferential controlled-depth micro-incisions in complex, mixed morphology PAD lesions. FLEX VP is currently indicated for use with PTA catheters to facilitate dilation of stenoses in the femoral and popliteal arteries and treatment of obstructive lesions of native or synthetic arteriovenous dialysis fistulae. In addition, FLEX VP is indicated for ISR treatment of balloon-expandable and self-expanding stents in the peripheral vasculature. Future directions include seeking expanded indications to include below-the-knee lesions. Other new indications being evaluated include venous, iliac, and coronary applications.
References
Shu J, Santulli G. Update on peripheral artery disease: epidemiology and evidence-based facts. Atherosclerosis. 2018;275:379–81.
Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366(9501):1925–34.
Shammas NW, Coiner D, Shammas G, Jerin M. Predictors of provisional stenting in patients undergoing lower extremity arterial interventions. Int J Angiol. 2011;20(2):95–100.
Armstrong EJ, Shishehbor MH. Commentary: contemporary outcomes of endovascular interventions for peripheral artery disease: the LIBERTY to determine optimal treatment strategies. J Endovasc Ther. 2019;26(2):155–7.
Castaneda-Zuniga WR, Formanek A, Tadavarthy M, Vlodaver Z, Edwards JE, Zollikofer C, et al. The mechanism of balloon angioplasty. Radiology. 1980;135(3):565–71.
van der Lugt A, Gussenhoven EJ, Mali WP, Reekers JA, Seelen JL, Tielbeek AV, et al. Effect of balloon angioplasty in femoropopliteal arteries assessed by intravascular ultrasound. Eur J Vasc Endovasc Surg. 1997;13(6):549–56.
Welt FG, Rogers C. Inflammation and restenosis in the stent era. Arterioscler Thromb Vasc Biol. 2002;22(11):1769–76.
Mongiardo A, Curcio A, Spaccarotella C, Parise S, Indolfi C. Molecular mechanisms of restenosis after percutaneous peripheral angioplasty and approach to endovascular therapy. Curr Drug Targets Cardiovasc Haematol Disord. 2004;4(3):275–87.
Ohtani K, Egashira K, Ihara Y, Nakano K, Funakoshi K, Zhao G, et al. Angiotensin II type 1 receptor blockade attenuates in-stent restenosis by inhibiting inflammation and progenitor cells. Hypertension. 2006;48(4):664–70.
Araujo PV, Ribeiro MS, Dalio MB, Rocha LA, Viaro F, Dellalibera Joviliano R, et al. Interleukins and inflammatory markers in in-stent restenosis after femoral percutaneous transluminal angioplasty. Ann Vasc Surg. 2015;29(4):731–7.
Nakazawa KR, Wengerter SP, Power JR, Lookstein RA, Tadros RO, Ting W, et al. Preoperative inflammatory status as a predictor of primary patency after femoropopliteal stent implantation. J Vasc Surg. 2017;66(1):151–9.
Guimaraes TS, da Rocha LA, Becari C, Piccinato CE, Joviliano RD, Ribeiro MS, et al. The role of interleukins and inflammatory markers in the early restenosis of covered stents in the femoropopliteal arterial segment. Ann Vasc Surg. 2018;50:88–95.
Fanelli F, Cannavale A, Boatta E, Corona M, Lucatelli P, Wlderk A, et al. Lower limb multilevel treatment with drug-eluting balloons: 6-month results from the DEBELLUM randomized trial. J Endovasc Ther. 2012;19(5):571–80.
Fujihara M, Takahara M, Sasaki S, Nanto K, Utsunomiya M, Iida O, et al. Angiographic dissection patterns and patency outcomes after balloon angioplasty for superficial femoral artery disease. J Endovasc Ther. 2017;24(3):367–75.
Rosenfield K, Jaff MR, White CJ, Rocha-Singh K, Mena-Hurtado C, Metzger DC, et al. Trial of a paclitaxel-coated balloon for femoropopliteal artery disease. N Engl J Med. 2015;373(2):145–53.
Tepe G, Beschorner U, Ruether C, Fischer I, Pfaffinger P, Noory E, et al. Drug-eluting balloon therapy for femoropopliteal occlusive disease: predictors of outcome with a special emphasis on calcium. J Endovasc Ther. 2015;22(5):727–33.
Tepe G, Zeller T, Schnorr B, Claussen CD, Beschorner U, Brechtel K, et al. High-grade, non-flow-limiting dissections do not negatively impact long-term outcome after paclitaxel-coated balloon angioplasty: an additional analysis from the THUNDER study. J Endovasc Ther. 2013;20(6):792–800.
Werk M, Albrecht T, Meyer DR, Ahmed MN, Behne A, Dietz U, et al. Paclitaxel-coated balloons reduce restenosis after femoro-popliteal angioplasty: evidence from the randomized PACIFIER trial. Circ Cardiovasc Interv. 2012;5(6):831–40.
Bosiers M, Scheinert D, Hendriks JM, Wissgott C, Peeters P, Zeller T, et al. Results from the tack optimized balloon angioplasty (TOBA) study demonstrate the benefits of minimal metal implants for dissection repair after angioplasty. J Vasc Surg. 2016;64(1):109–16.
Shammas NW, Torey JT, Shammas WJ, Jones-Miller S, Shammas GA. Intravascular ultrasound assessment and correlation with angiographic findings demonstrating femoropopliteal arterial dissections post atherectomy: results from the iDissection study. J Invasive Cardiol. 2018;30(7):240–4.
Kobayashi N, Hirano K, Yamawaki M, Araki M, Sakai T, Sakamoto Y, et al. Simple classification and clinical outcomes of angiographic dissection after balloon angioplasty for femoropopliteal disease. J Vasc Surg. 2018;67(4):1151–8.
Kokkinidis DG, Jeon-Slaughter H, Khalili H, Brilakis ES, Shammas NW, Banerjee S, et al. Adjunctive stent use during endovascular intervention to the femoropopliteal artery with drug coated balloons: insights from the XLPAD registry. Vasc Med. 2018;23(4):358–64.
Laird JA, Schneider PA, Jaff MR, Brodmann M, Zeller T, Metzger DC, et al. Long-term clinical effectiveness of a drug-coated balloon for the treatment of femoropopliteal lesions. Circ Cardiovasc Interv. 2019;12(6):e007702.
Tan M, Urasawa K, Koshida R, Haraguchi T, Kitani S, Igarashi Y, et al. Comparison of angiographic dissection patterns caused by long vs short balloons during balloon angioplasty of chronic femoropopliteal occlusions. J Endovasc Ther. 2018;25(2):192–200.
Fitzgerald PJ, Ports TA, Yock PG. Contribution of localized calcium deposits to dissection after angioplasty. An observational study using intravascular ultrasound. Circulation. 1992;86(1):64–70.
Kaladji A, Vent PA, Danvin A, Chaillou P, Costargent A, Guyomarch B, et al. Impact of vascular calcifications on long femoropopliteal stenting outcomes. Ann Vasc Surg. 2018;47:170–8.
Mattesini A, Di Mario C. Calcium: a predictor of interventional treatment failure across all fields of cardiovascular medicine. Int J Cardiol. 2017;231:97–8.
Rocha-Singh KJ, Zeller T, Jaff MR. Peripheral arterial calcification: prevalence, mechanism, detection, and clinical implications. Catheter Cardiovasc Interv. 2014;83(6):E212–20.
Scheinert D, Micari A, Brodmann M, Tepe G, Peeters P, Jaff MR, et al. Drug-coated balloon treatment for femoropopliteal artery disease. Circ Cardiovasc Interv. 2018;11(10):e005654.
Thieme M, Von Bilderling P, Paetzel C, Karnabatidis D, Perez Delgado J, Lichtenberg M, et al. The 24-month results of the Lutonix global SFA registry: worldwide experience with Lutonix drug-coated balloon. JACC Cardiovasc Interv. 2017;10(16):1682–90.
Torsello G, Stavroulakis K, Brodmann M, Micari A, Tepe G, Veroux P, et al. Three-year sustained clinical efficacy of drug-coated balloon angioplasty in a real-world femoropopliteal cohort. J Endovasc Ther. 2020;27(5):693–705.
Singh H, Kirtane A, Moses J. AngioSculpt® scoring balloon catheter: an atherotomy device for coronary and peripheral interventions. Interv Cardiol. 2010;2:469–78.
Hwang CW, Levin AD, Jonas M, Li PH, Edelman ER. Thrombosis modulates arterial drug distribution for drug-eluting stents. Circulation. 2005;111(13):1619–26.
Tzafriri AR, Garcia-Polite F, Zani B, Stanley J, Muraj B, Knutson J, et al. Calcified plaque modification alters local drug delivery in the treatment of peripheral atherosclerosis. J Control Release. 2017;264:203–10.
Kronlage M, Werner C, Dufner M, Blessing E, Muller OJ, Heilmeier B, et al. Long-term outcome upon treatment of calcified lesions of the lower limb using scoring angioplasty balloon (AngioSculpt). Clin Res Cardiol. 2020;109(9):1177–85.
Korosoglou G, Lichtenberg M, Celik S, Andrassy J, Brodmann M, Andrassy M. The evolving role of drug-coated balloons for the treatment of complex femoropopliteal lesions. J Cardiovasc Surg. 2018;59(1):51–9.
Armstrong EJ, Kokkinidis DG. EDITORIAL: Eximo Medical’s B-Laser for infrainguinal peripheral artery disease: the new kid on the block for lesion preparation in complex peripheral interventions? Cardiovasc Revasc Med. 2020;21(1):93–5.
Tarricone A, Ali Z, Rajamanickam A, Gujja K, Kapur V, Purushothaman KR, et al. Histopathological evidence of adventitial or medial injury is a strong predictor of restenosis during directional atherectomy for peripheral artery disease. J Endovasc Ther. 2015;22(5):712–5.
Krishnan P, Tarricone A, Purushothaman KR, Purushothaman M, Vasquez M, Kovacic J, et al. An algorithm for the use of embolic protection during atherectomy for femoral popliteal lesions. JACC Cardiovasc Interv. 2017;10(4):403–10.
Shrikhande GV, Khan SZ, Hussain HG, Dayal R, McKinsey JF, Morrissey N. Lesion types and device characteristics that predict distal embolization during percutaneous lower extremity interventions. J Vasc Surg. 2011;53(2):347–52.
Dattilo R, Himmelstein SI, Cuff RF. The COMPLIANCE 360 degrees trial: a randomized, prospective, multicenter, pilot study comparing acute and long-term results of orbital atherectomy to balloon angioplasty for calcified femoropopliteal disease. J Invasive Cardiol. 2014;26(8):355–60.
Zeller T, Krankenberg H, Steinkamp H, Rastan A, Sixt S, Schmidt A, et al. One-year outcome of percutaneous rotational atherectomy with aspiration in infrainguinal peripheral arterial occlusive disease: the multicenter pathway PVD trial. J Endovasc Ther. 2009;16(6):653–62.
Zeller T, Langhoff R, Rocha-Singh KJ, Jaff MR, Blessing E, Amann-Vesti B, et al. Directional Atherectomy followed by a paclitaxel-coated balloon to inhibit restenosis and maintain vessel patency: twelve-month results of the DEFINITIVE AR study. Circ Cardiovasc Interv. 2017;10(9):e004848.
Kassimis G, Raina T, Kontogiannis N, Patri G, Abramik J, Zaphiriou A, et al. How should we treat heavily calcified coronary artery disease in contemporary practice? From atherectomy to intravascular lithotripsy. Cardiovasc Revasc Med. 2019;20(12):1172–83.
Brodmann M, Schwindt A, Argyriou A, Gammon R. Safety and feasibility of intravascular lithotripsy for treatment of common femoral artery stenoses. J Endovasc Ther. 2019;26(3):283–7.
Zeller T, Lopez L, Pigott JP. Acute outcomes with a novel plaque modification system in real-world femoropopliteal lesions. J Endovasc Ther. 2019;26(3):333–41.
Oriwo B, Abbas J, Lurie F. 2-year experience using FLEX catheter as a preparatory device for drug-coated balloon and/or balloon angioplasty. International symposium on endovascular therapy, Hollywood, FL; 2019.
Dexpert J-P, Hayoz D, Engelberger R, Krieger C, M-AR M, Periard D. Arterial preparation by longitudinal micro-incisions before balloon angioplasty of the superficial femoral and popliteal artery: acute and 12-month results. J Endovasc Ther. 2022;29(3):420–6.
Brodmann M, Keirse K, Scheinert D, Spak L, Jaff MR, Schmahl R, et al. Drug-coated balloon treatment for femoropopliteal artery disease: the IN.PACT global study de novo in-stent restenosis imaging cohort. JACC Cardiovasc Interv. 2017;10(20):2113–23.
Kinstner CM, Lammer J, Willfort-Ehringer A, Matzek W, Gschwandtner M, Javor D, et al. Paclitaxel-eluting balloon versus standard balloon angioplasty in in-stent restenosis of the superficial femoral and proximal popliteal artery: 1-year results of the PACUBA trial. JACC Cardiovasc Interv. 2016;9(13):1386–92.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pigott, J.P. (2022). Vessel Preparation with Longitudinal and Controlled-Depth Micro-Incisions. In: Shammas, N.W. (eds) Peripheral Arterial Interventions. Contemporary Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-031-09741-6_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-09741-6_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-09740-9
Online ISBN: 978-3-031-09741-6
eBook Packages: MedicineMedicine (R0)