Abstract
Cutaneous melanoma is dramatically increasing in frequency, and it represents quite an aggressive tumor when evolving to the metastatic stage. High-resolution ultrasound (US) is playing a growing role in assessing newly diagnosed cutaneous melanoma in the locoregional staging prior to the sentinel lymph node biopsy procedure and in the melanoma patient follow-up. Primary melanoma assessment with US requires a rigorous methodology to allow a sonographic measurement of tumor thickness adequately reflecting pathological measurement. Several challenging aspects exist. Appropriate equipment setting and adequate knowledge of the very peculiar way of spread of melanoma and the related grayscale and color Doppler features are mandatory. US can be valuable in assessing superficial melanoma metastases’ response to newly developed local or systemic therapies. Finally, US may guide percutaneous procedures in the melanoma patient, both diagnostic and therapeutic.
To the memory of Christiane Voit, passionate melanoma ultrasound expert
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cutaneous melanoma
- Lymph node
- Melanoma follow-up
- Melanoma metastasis
- Sentinel lymph node biopsy
- Ultrasound
- Color Doppler
- Elastography
Introduction
Most patients with early-stage (I and II) cutaneous melanoma have an overall favorable prognosis. Currently, 90% of the cases are diagnosed without metastasis, and their tumor-specific 10-year survival rate is 75–95% [1]. However, once melanoma has spread to visceral organs, this cancer rapidly becomes life-threatening. Despite significant improvements in the treatment of metastatic stage melanoma in the last years, survival is first of all improved by decreasing ultraviolet radiation exposure and increasing sun protection in the population, as well as by early detecting and appropriately managing skin-limited melanoma disease [2]. Diagnostic imaging, ultrasound (US) included, plays a minor role in the initial diagnosis of melanoma; however, high-resolution US is being studied to replace excision biopsy of cutaneous tumors [3]. Imaging plays a major part in the staging and follow-up of melanoma and the post-treatment assessment of metastatic disease [4]. The role of imaging is to help assess disease extent, formulate prognosis, establish treatment response, and detect recurrence.
This chapter focuses on the US findings and the US role in evaluating primary melanoma lesions, satellite/in-transit metastasis, and lymph node metastasis.
Epidemiological and Clinical Aspects of Cutaneous Melanoma
Prevalence and Mortality
Melanoma is a malignant proliferation arising from the pigment-producing melanocytic cells located in the skin. Melanocytic lesions are often benign (melanocytic nevi) and affect many individuals. Melanoma is the fifth most common cancer for men and is the seventh for women. Its incidence rate has continued to increase strongly worldwide, although the prevalence differs widely across the countries and among the various ethnicities. The annual incidence of malignant melanoma is 3–5/100,000 in Mediterranean European countries, 12–35/100,000 in North European countries, 20–30/100,000 in the USA, and 50–60/100,000 in Australia and New Zealand [1, 5]. The risk of developing a skin melanoma increases linearly after the age of 25 years until that of 50 years and then decreases. Melanoma may develop in childhood, although being quite rare. Women are more frequent in younger aged groups, while the males prevail from the age of 55 onwards [6].
The main risk factors for cutaneous melanoma include fair skin, excessive exposure to sunlight (particularly if high and intermittent), exposure to artificial ultraviolet radiation (phototherapy, tanning beds, etc.), history of sunburn in childhood or adolescence, a high number of common nevi or large congenital nevi, dysplastic nevi, family history of melanoma, and immunosuppression [6, 7]. Approximately 25% of melanomas arise on preexisting nevi, while 75% raise de novo.
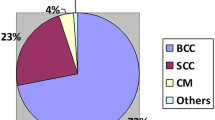
Although melanoma represents less than 5% of all types of skin cancer, it is responsible for most skin cancer-related deaths. It causes each year 9000 deaths in the USA and 55,500 deaths worldwide [8, 9]. Main prognostic factors include primary tumor depth at histology (Breslow thickness), ulceration of primary tumor, and status of regional lymph nodes at the moment of initial diagnosis [7].
Pathology and Classification: The Breslow Index
Cutaneous melanoma is a heterogeneous disease. The most common clinical and pathological subtype is superficial spreading melanoma, comprising around 41–70% of cases [1]. Other subtypes are nodular melanoma, lentigo maligna melanoma, acral lentiginous melanoma (including nail bed melanoma), amelanotic (achromic) melanoma, and desmoplastic melanoma [1, 7]. From the invasiveness point of view, melanoma is classified as in situ, when confined within the epidermis, or invasive, when melanocytes progressively invade the dermis [1]. Borderline lesions include Spitz nevi and dysplastic nevi. Atypical Spitz nevi are managed in the same way as melanoma. In a 2018 WHO conference [10], melanomas were divided into those etiologically related to sun exposure and those that are not, as determined by their mutational signatures, anatomic site, and epidemiology. Melanomas on the sun-exposed skin are further divided based on the surrounding skin’s histopathologic degree of associated solar elastosis. Low cumulative solar damage melanomas include superficial spreading melanomas, and high cumulative solar damage melanomas incorporate lentigo maligna and desmoplastic melanomas. The “nonsolar” category includes acral melanomas, some melanomas in congenital nevi, melanomas in blue nevi, Spitz melanomas, mucosal melanomas, and uveal melanomas.
Breslow index, i.e., the vertical tumor thickness measured at histological staining of the surgical biopsy specimen (histometry), represents the single most important prognostic factor for clinically localized cutaneous melanoma. It is a key aspect of patient management to establish the need and extent for primary tumor scar re-excision and the need for the sentinel lymph node biopsy (SLNB) procedure. The Breslow index is expressed in millimeters and is defined as the maximum distance between the top of the stratum granulosum of the epidermis and the deepest invasive tumor cell across the broad base of the tumor (dermal/subcutaneous) [11,12,13]. In the case of tumor ulceration, the measurement starts from the base of the ulcer. Deep, vertical extensions of the tumor, perpendicular to the base, are assumed to be periadnexal and are not included in the Breslow thickness. Variable degrees of inflammatory infiltrate, and associated nevi, can be encountered in combination with melanoma.
Patterns of Growth and Patterns of Spread
Most cutaneous melanomas evolve through two stages. In the first of these, the early lesions may be recognized as a pigmented macula or plaque, which expands more or less along the radii of an imperfect circle in the horizontal axis within the skin. In the subsequent phase, a tumor is formed that may infiltrate into the dermis or elevate the epidermis to form a nodule whose net direction of growth includes the vertical axis. Nodular melanoma starts as a bulging nodule from the beginning [1, 10].
Once grown, cutaneous melanoma has a particular modality of diffusion. Around 30% of metastasis are hematogenous, spreading to deep organs and having the skin as one of the main targets. In most cases, around 70% of metastasis happens via the lymphatic vessels. Using this pathway, melanoma cells may grow as dermal or subdermal nodules around the primary tumor or scar if the melanoma has already been removed. Nodules within 2 cm from the tumor are called satellite metastases. In other cases, melanoma lesions grow at a higher distance from the tumor, along the way to the regional lymph node station. These nodules are termed in-transit metastases. However, both satellitosis and in-transit metastasis represent an intralymphatic spread of the disease, for example, a stage III disease, and this categorization is not relevant in practice. Finally, the tumor may reach the regional lymph nodes. In some case, satellite/in-transit metastasis develops as isolated; in other cases, they are found in combination with metastatic lymphadenopathies, while finally, in some cases of metastasis, the majority goes straight to the lymph nodes, without combined satellite or in-transit lesions [1, 13].
Diagnosis and Management
Skin melanoma diagnosis is usually made clinically by the family doctor or the dermatologist. Dermoscopy improves the sensitivity and specificity of clinical assessment. Pathologic confirmation is mandatory and requires an excision biopsy with the removal of the entire primary lesion. In clinically suggestive lesions, a biopsy is performed at a full thickness to ensure that the lesion is not histologically transected at the deep aspect and it encompasses the entire breadth of the lesion with clinically negative margins [13]. However, at the same time, surgical margins must be narrow enough (usually 1–3 mm) to avoid impairment of the melanoma lymphatic basin before the SLNB procedure [5].
Histology is also necessary to determine the vertical thickness of the tumor (Breslow index), a key aspect in establishing further patient workup and final prognosis. The assessment of the tumoral thickness is essential to confirm the need for re-excision and to establish the width of the margin required. As a matter of fact, wider and deeper local excision is performed following initial biopsy to ensure complete removal of the lesion, confirm histologically clear margins, and reduce the risk of local recurrence [13]. Excision with safety margins of 0.5 cm for in situ melanomas, 1 cm for tumors with a Breslow thickness ≤2 mm, and 2 cm for thicker tumors is recommended [5].
In addition to re-excision, the SLNB procedure is performed for patients with melanomas thicker than 0.8 mm or melanomas thinner than 0.8 mm but ulcerated (i.e., melanomas pT1b, or higher) [5]. Radical, prophylactic (elective) lymphadenectomy is no longer an acceptable option, and SLNB is regarded as the current standard [5]. The introduction of SLNB, as an alternative to elective lymphadenectomy, has spared an unnecessary radical lymphadenectomy to around 80% of patients with no regional involvement [14, 15]. The SLN status is the strongest known prognostic marker [7, 13, 16]. Completion lymph node dissection (CLND) usually is performed after that for clinical (macroscopic) stage III disease on confirmation of lymph node invasion. It must be noted that, following the current guidelines, in the worst case, the patient undergoes surgery three times, first for SLN excision biopsy, then for re-excision of the primary tumor and SLNB, and finally for CLND.
Tips and Tricks of Cutaneous Melanoma US Examination
Technological Requirements
Scanners must be equipped with a high-resolution multifrequency linear transducer. Ideally, two linear probes should be available, differing in their footprint length and frequency range. Alternatively, a probe with a wide range of frequencies is advisable. A transmission frequency above 15 MHz is mandatory for primary melanoma and superficial metastasis (dermis). In comparison, frequencies between 7.5 and 15 MHz are needed for deeper abnormalities (subcutaneous layer and lymph nodes) [17, 18] (Fig. 10.1). The tiny dermal or subdermal lesions will be better displayed using higher frequencies, while small hypoechoic nodules will be confirmed or demonstrated as benign (epidermal inclusion cyst, postsurgical seroma, etc.) using higher frequencies (Fig. 10.2). A considerable amount of US gel or a standoff pad helps optimize the beam focalization [19, 20] (Fig. 10.3). This is particularly useful for the very superficial lesions close to the skin’s surface and is important not only for B-mode scanning but also for Doppler imaging and elastography assessment.
A skin-devoted preset should be present in the scanner. According to the ongoing findings, this baseline regulation will be modified during the examination dynamically. To maximize conspicuity, the beam is electronically focused immediately below the area of interest [21]. Special care is taken to regulate signal amplification and time-gain compensation curve [21, 22]. This avoids the development of artifactual echoes within anechoic structures and suppresses subtle echoes within hypoechoic structures. The time-gain compensation curve is adjusted to gradually increase with increasing depth and equalize the echogenicity of fatty tissues at all subcutaneous depths. It is essential to set the dynamic range. If it is too narrow, hypoechoic lesions appear anechoic, while if it is too wide, lesions may appear isoechoic and may not be detected on US. Total gain can accentuate the effects of an inappropriate dynamic range regulation [21].
Real-time, extended field-of-view (EFOV), or panoramic view images are obtained to display the area of interest comprehensively. EFOV scans may help improve image correlation during serial scanning and provide the surgeon with more readable and anatomically oriented images. These images are also helpful to measure the distance between multiple nodules or between a nodule of a given anatomic landmark [23].
Color Doppler imaging requires scanner settings adequate for detecting superficial slow flows. This includes high Doppler frequency, low pulse repetition frequency, low or null wall filter, and color gain raised immediately below the noise threshold [19, 20]. The color box is limited to the area of interest, and the beam focus is put just below it. The power Doppler mode, which is more sensitive to slow flows in most scanners, is preferred over the color Doppler mode [24]. Recently introduced, high-frame-rate modalities for microvasculature assessment are preferred, if available [19]. Care is taken to avoid excessive pressure of the transducer on the skin, which may suppress the flow signal from small and superficial lesions. Using a spacer or a considerable amount of gel is helpful to put the area of interest at the best depth inside the field of view, improving flow detection [25] (Fig. 10.4).
Primary Tumor Examination
During the primary melanoma US examination, the operator rotates the probe around its axis in 180 degrees clockwise and counterclockwise to check the entire surface of the tumor and reveal the maximal diameter and thickness of the melanoma [26]. The transducer must be held in a very gentle way. Flattening of the tumor by excessive probe compression must be avoided, both for B-mode display and for Doppler display. A large amount of sonographic gel is recommended.
It is very important to measure tumor thickness using a rigorous and standardized way [27]. Depth is regulated by focusing the field of view on the first couple of centimeters. Electronically zoomed scans are advisable. The beam focus must be single and put just below the tumor. B-mode gain and time-gain compensation curves must be regulated to achieve the best contrast. The measure is tracked using the electronic calipers on a frozen, clear image, in a perfectly perpendicular way, at the point of the maximal tumor vertical extent. Measuring the thickness three times and calculating the mean value are advisable. The thin echogenic epidermis line above the tumor is excluded from the measurement since US cannot differentiate the various epithelial layers inside.
Using radiofrequency signals obtained with a single-element focused transducer, Andrekute et al. [28] were able to make the tumor boundaries more noticeable and adopt an automated measurement of melanocytic skin tumor thickness. Automatically measured US thickness correlated significantly better than manually measured US thickness with the Breslow index.
Locoregional Examination
A patient’s surgical history should be known in detail before performing a sonographic scan. The clinical’s report of the physical examination should also be available. The patient must be questioned regarding any change felt at self-palpation.
A skin area of 5–10 cm around the in-site primary melanoma, or around its postsurgical scar, is scanned to detect any satellite [17, 29]. The transducer is subsequently moved along the presumable course of the lymphatic vessel lesion toward the regional lymphatic region, mainly in a transverse probe orientation [30, 31]. This is to identify in-transit metastases. In patients with torso melanomas, the cutaneous portion toward the axillae (with the patient both supine and sitting on the bed) and the inguinal regions are scanned. In subjects with melanoma of the limbs, the skin toward the regional lymphatic station, at least at the level of the compartment (anterior or posterior) where the primary lesion is located, is explored. Aside from what is displayed on the screen, it is also important to note any subtle irregularity felt while moving the probe over the skin.
All nodal regions are explored with the patient supine. A sitting position is helpful to evaluate the supraclavicular, nuchal, and retroauricular lymph nodes. In trunk melanomas, the supraclavicular and axillary nodes, as well as the deep pectoral and infraclavicular nodes, are investigated. When the primary melanoma site is in the head or neck, the cervical stations and the supraclavicular stations are explored bilaterally. In upper limb and upper trunk melanomas, the supraclavicular and infraclavicular stations are included. When the primary melanoma is at the level of the limbs, the status of both axillary and inguinal lymphatic basins is, respectively, investigated. The contralateral (axillary or inguinal) lymphatic basin is also examined, although contralateral lymphadenopathies are quite rare in extremity melanomas. Contralateral lymph nodes represent a useful reference since any significant relevant difference between the two sides is regarded as suspicious [17, 32].
All nodal stations must be scanned widely since the lymph nodes can be located quite eccentrically. Particularly after SLNB and CLND, the lymphatic drainage can encounter considerable changes, which must be considered during patient follow-up. In the neck, not only the anterior and laterocervical stations but also all possible sites of spread are explored, including nuchal, retroauricular, and intraparotid nodes. In the case of facial melanoma, the cheeks and anterior submental region are explored in addition to the neck stations. At the axilla level, the cavity, both medially and laterally to the main vessels, is examined. The posterior column toward the latissimus dorsi muscle, the beginning of the upper arm, the subaxillary region, and the mammary prolongation are also included. The inguinal region is scanned for both superficial and deep nodes, medially and laterally to the femoral vessels, extending the scan to the crural region toward the thigh and above the ligamentum inguinale to the suprainguinal portion of the anterior abdominal wall. An attempt should also be made to evaluate the most superficial external iliac nodes.
To rule out any interval lymphadenopathy (i.e., any non-regional lymphatic station placed along the pathway of the melanoma spread), the epitrochlear area in patients with primary melanoma located in the forearm or hand and the popliteal fossa in patients with the primary tumor in the leg or foot are scanned [33,34,35].
Once a lymph node is identified, careful assessment is needed to understand if metastatic involvement is present or not. Attention is paid to “cut” the lymph node along its long axis since an oblique view may raise a mistaken idea of asymmetric cortical thickening. Sometimes lymph nodes, particularly the fatty ones, have an irregular, lobulated shape, which may lead to an erroneous image interpretation or an incorrect measurement. The size of the abnormal lymph nodes is measured according to two perpendicular planes. Measurement includes the maximum lesion diameter (lesion length or longitudinal diameter) and the maximal diameter perpendicular to the former (lesion thickness or transverse diameter). Their ratio, i.e., the longitudinal-to-transverse diameter ratio (L/T), is calculated.
Primary Cutaneous Melanoma: US Findings
Primary melanoma appears as a markedly hypoechoic lesion infiltrating the dermis [24]. It is of note that the same applies to all superficial and deep melanoma locations, and it is due from one side to the hypercellularity of the lesions, as for many other tumors, and from the other side to the very echo reflexivity of melanin [4]. The tumor is homogeneous or near homogeneous with few low-level echoes inside [22, 36]. The shape is usually oval, jagged, or linear, but it can be quite asymmetric, with portions of different thicknesses [26, 37]. Tumor thickness correlates with tumor shape, being maximal in oval lesions, intermediate in jagged lesions, and low in linear lesions. The ratio between the maximal diameter and the maximal thickness is low in oval tumors, intermediate in jagged tumors, and high in linear tumors [26] (Figs. 10.5 and 10.6).
The margins are usually sharp. The thin echogenic line of the epidermis is always recognizable over the melanoma lesion unless tumor ulceration is present. In the latter case, the epidermis may be irregular or discontinuous, and increased echogenicity of the surrounding subcutaneous tissue may be found [24, 38]. In most cases, particularly in nodular lesions, the tissues deeper to the tumor exhibit a homogeneous acoustic enhancement. Unlike skin carcinomas, posterior acoustic shadowing is not encountered in melanoma lesions [4, 36].
Very thin melanomas may not be recognizable at all [24]. This is particularly in sun-exposed areas of older people in which the physiologic subepidermal hypoechoic band is significant and masquerades the tumor.
In most cases, on color or power Doppler, flows can be identified within the tumor, proving that a slow-flow setting has been adopted. Vascularization is usually medium to high in intensity, anarchic, and multipolar [4, 26, 36] (Figs. 10.7, 10.8, and 10.9). Botar Jid et al. found significant correlations between the Breslow index, the degree of vascularization, and the number of vascular pedicles [39]. Thin tumors may exhibit low or absent vascularization.
Cutaneous melanoma is moderately to strongly stiff at strain elastography [3, 26, 40]. However, this finding is not specific, shared by most cutaneous malignancies [4]. The elastography stiffness ratio was high in oval-shape melanomas (3.26), intermediate in jagged melanomas (2.76), and low (2.40) in linear melanomas [26]. Botar Jid et al. [39] showed a strong correlation between the strain elastography qualitative appearance and the vascularization of primary melanoma, as well as between the strain elastography qualitative appearance and the number of vascular pedicles. The relations between tumor appearance at strain elastography and tumor thickness at US, the lesion-to-dermis strain ratio, and the lesion-to-hypodermis strain ratio have proven statistically significant [3].
Role of US in Primary Cutaneous Melanoma
Differential Diagnosis
At the present moment, it is not the role of US to obtain a noninvasive diagnosis of melanoma, i.e., to differentiate it from clinically overlapping lesions, such as basal/squamous cell carcinoma, nevus, keratosis, lentigo, capillary thrombosis, and pigmented histiocytic fibroma [41]. A Cochrane review published in 2018 [42] identified 20 datasets for diagnosing melanoma using high-resolution US (20 MHz or more). Derived sensitivities were at least 83% for the detection of melanoma; the combination of three features (lesions appearing hypoechoic, homogenous, and well defined) demonstrated a 100% sensitivity in two studies, with a specificity of 33% and 73%, respectively. Given the between-study heterogeneity, unclear to low methodological quality, and limited volume of evidence, the authors stated that they could not draw any implications for practice. The article concluded that insufficient data are available on the potential value of US in the diagnosis of melanoma. However, again, it must be highlighted that melanoma diagnosis is not at present the focus of US.
In clinical practice, the most frequent issue is to differentiate melanoma from atypical nevi. The US appearance basically overlaps since both nevi and melanoma lesions are mainly hypoechoic, relatively homogeneous, symmetrical, and usually well delimited from the adjacent dermis. Junctional nevi are very thin, while dermal nevi are thicker.
US features that can assist in the differential diagnosis between benign pigmented lesions and melanoma include location, echogenicity, homogeneity, shape, margins, increased posterior echogenicity, and back shadowing. Melanomas have been generally described as more homogeneous with well-defined margins than other lesions [43]. Harland et al. [44] employed objective measures of acoustic shadowing, intralesional sound reflection, and surface sound reflectance characteristics. They reported melanoma as being less attenuating than benign lesions and more homogeneous than seborrheic keratoses. Additionally, the ratio between tumor diameter and tumor thickness is higher in melanoma compared to benign skin abnormalities [36].
In addition to B-mode criteria, also vascularization may be useful in suspecting a malignant lesion since the detection of intralesional flows increases the probability of a melanomatous nature. However, despite a good specificity, flow detection has not proven enough sensitivity till now. This is due to the inability of Doppler techniques, particularly with the equipment available in the past years, to demonstrate the presence of a vascular signal in thin melanomas. The conspicuity for malignancy is strong when vascular signals are detected in a hypoechoic lesion thicker than 2 mm. Conversely, the absence of flow signals in a lesion less than 2 mm in thickness does not enable benignity to be confirmed.
Preliminary experiences using strain elastography are encouraging. In the series from Hambardzumyan and Hayrapetyan [36], the stiffness of the 26 melanomas was 2.95 ± 0.18, being significantly higher than the group of 35 patients with benign skin abnormalities (0.96 ± 0.59).
US contrast media have been employed by some researchers [41] to differentiate melanoma from benign pigmented lesions. No data are available as of now.
Measuring Tumor Thickness
US measurement of primary melanoma thickness (so-called sonometry) has shown a variable correlation with the Breslow index according to the various studies published through the years [45,46,47]. Older articles using lower frequency transducers had a nonoptimal correlation, while more recent studies with better-performing scanners and probes obtained more valuable results [19]. Some authors have suggested that the accuracy of sonometry would be improved by using probes of very high frequency, up to 100 MHz, but these transducers are not available in all diagnostic centers [48, 49]. Interestingly, a US scan at 12–15 MHz can reliably differentiate primary melanoma thicknesses of greater than 1 mm from those of 1 mm or less [50].
The correlation between US measurement and Breslow index is high but not ideal, particularly for lesions <1 mm in thickness. US tends to overscore the primary melanoma thickness [22]. This is also because US measures the tumor in vivo while the pathologist performs their measurement on a dehydrated and fixed material [24]. Subtumoral inflammatory infiltrates and associated nevi may also explain discrepancies since US cannot distinguish the different components of the lesion [11]. The difference in the speed of sound through melanoma and normal tissue may be another explanation for the US overestimation of tumor thickness [51].
Preliminary experiences have been reported on the use of US as an alternative to excision and re-excision for tumor management. Caput et al. recently published a retrospective series of 99 melanoma patients imaged using 20-MHz US [52]. In 78 subjects, the tumor was removed in a single step, basing the width of the excision on the thickness as measured with US. In five cases, this resulted in excessive margins, and in two cases, the margins were insufficient. The conclusion was that measuring the thickness of melanoma with US makes it possible to remove the tumor in a single step instead of two steps, achieving adequate margins in at least 82% of cases.
At least US-based measurement could represent a valuable complementary tool in case of lesions that are large and/or located in challenging anatomic sites such as the face or acral, in which excision biopsy may be precluded.
Prognosis
Aside from the diagnosis of melanoma, the amount of vascularization has proven to have a prognostic value, correlating with the risk of lymph node involvement and the 5-year survival [53, 54].
Cutaneous Melanoma Staging
The eighth edition of the American Joint Committee on Cancer (AJCC) staging system for cutaneous melanoma was published in 2017 [16, 55].
The T categorization basically relies on two criteria, vertical tumor thickness (Breslow index) and presence or not of ulceration (i.e., full-thickness absence of the epidermis above any portion of the tumor with an associated host reaction). This is because primary tumor thickness and ulceration are by far the strongest predictors of melanoma-specific survival. T1 includes tumors ≤1.0 mm. Subcategories are T1a for tumors <0.8 mm and T1b for tumors <0.8 mm but ulcerated or 0.8–1.0 mm tumors. The T2 category includes tumors between 1.1 and 2.0 mm, without ulceration (T2a) or with ulceration (T2b). T3 tumors range between 2.1 and 4.0 mm, not ulcerated (T3a) or ulcerated (T3b). T4 tumors are >4.0 mm in thickness, classified as T4a if nonulcerated and T4b if ulcerated [16, 55].
The N category riles on the involvement or not of regional lymph nodes and non-nodal locoregional sites. The latter include microsatellites (microscopic cutaneous or subcutaneous metastases found adjacent or deep to the tumor on pathological examination), satellites (clinically evident cutaneous or subcutaneous metastases occurring within 2 cm of the tumor), and in-transit metastases (clinically evident cutaneous and/or subcutaneous metastases identified at a distance more than 2 cm in the region between the tumor and the first echelon of regional lymph nodes).
N0 means that no regional metastases are detected. N1 category is assigned if only one lymph node is involved or if any in-transit, satellite, or microsatellite metastasis with no combined nodal metastasis is found. N2 means that two or three lymph nodes are involved, or any in-transit, satellite, or microsatellite metastasis is seen jointly with a metastatic lymph node. Finally, N3 is applied when more than three metastatic lymph nodes are present, if any in-transit, satellite, and/or microsatellite metastasis is found together with more than one metastatic lymph node, or in the case of matted lymph nodes, any number. Like the T parameter, the N one has several subcategories, but this is beyond the purpose of this chapter [16, 55].
The M parameter is M0 in the absence of distant metastasis and M1 in the presence of distant metastasis. M1 includes four categories. M1a is important from the point of view of this chapter since it refers to metastasis to the skin, soft tissue including muscle, and/or non-regional lymph node [16].
Clinical staging includes microstaging of the primary melanoma—as a standard practice, after biopsy of the primary melanoma—and clinical/radiologic assessment for regional and distant metastases, as well as biopsies, performed to assess for regional and distant metastases, as appropriate [16]. When T is T1a and N is N0, the clinical group stage is IA. When T is T1b or T2a and N are N0, the disease stage is IB. When T is T2b or T3a and N are N0, the stage is IIA. When T is T3b or T4a and N are N0, the stage is IIB. When T is T4b, and N is N0, the stage is IIC. When N is N1 to N3, the stage is III (whatever the T parameter is). Finally, when M is M1, i.e., one or more distant metastasis is present, the stage is IV, whatever the T and the N parameter will be.
For low-risk melanomas (pT1a), no additional investigations are necessary. In the other stages, pT1b-pT4b, US for locoregional metastasis and/or computed tomography (CT) or positron-emission tomography (PET-CT) scans represent options for tumor extension assessment before surgical treatment and SLNB [5].
The Sentinel Lymph Node Biopsy
Conceptual Aspects
Regional lymph nodes represent the most frequent site of metastasis in the melanoma patient. The sentinel lymph node (SLN) is the first lymph node draining a given skin area and consequently the first one reached by the tumor cells in a given lymphatic station. If the SLN is free from tumor invasion, the probability of involvement of the other lymph nodes, the non-sentinel lymph nodes, is quite low. The opposite is in the case of SLN involvement. The status of the SLN at surgical excision biopsy is consequently the most powerful predictor of outcome in patients with early-stage melanoma [13, 56]. The risk of regional lymph node recurrence after a negative SLNB result is ≤5 [57].
Description of the Procedure
Lymphoscintigraphy with radioactive nanocolloid is employed to map preoperatively the lymphatic drainage of the cutaneous melanoma toward the lymph node station [58] (Fig. 10.10). In addition, the vital blue dye can be injected intradermally, allowing the surgeon to follow it till the SLN [13]. In the triple technique, lymphoscintigraphy is undertaken within 24 h of the SLNB procedure, patent blue is injected during surgery, and handheld γ-probe detection of technetium-99 sulfur colloid is employed during surgery [13] (Fig. 10.11). The dissected SLN is stained with hematoxylin-eosin and, if needed, with immunohistochemical markers for S100 protein, Sox10, and HMB45 antigen, to detect the presence of metastatic deposits. The morbidity of SLNB is 10%, and the false-negative rate is 4–20% [15].
A SLN metastasis is seen in less than 5% of patients with melanoma <0.8 mm in thickness and 5–12% of patients with melanoma ranging from 0.8 to 1.0 mm in thickness. Therefore, SLNB is offered to patients with a T1b primary tumor, particularly when other adverse prognostic parameters are also present, and not to subjects with a T1a tumor [59]. Subjects with positive SLN excision represent about 20% of all patients with intermediate-thickness primary melanoma [60]. The 10-year melanoma-specific survival in these stage III patients is significantly lower than among the SLN-negative patients for intermediate-thickness melanomas [56]. The SLN tumor burden is classified according to the Rotterdam criteria (largest tumor deposit <0.1 mm or 0.1–1.0 mm or >1.0 mm). It significantly influences the prognosis of melanoma since subjects with SLN metastasis <0.1 mm have good survival rates, although still at higher risk of recurrence if compared to subjects with a negative SLNB [61, 62]. False-negative SLNBs may result from deficiencies in nuclear medicine, surgery, or pathology [63, 64].
Post-SLNB Patient Management
By now, the SLNB is thought to be a surgical staging procedure with diagnostic and prognostic significance only since its therapeutic role in patient survival is not confirmed [15, 60, 65]. The study named MSLT-I did not demonstrate a significant therapeutic advantage of SLNB over observation concerning melanoma-specific survival [56].
Most surgeons continue to recommend a complete lymph node dissection (CLND) in subjects with a positive SLNB, although its real impact on mortality is now intensely debated [5, 13]. CLND removes any additional lymph nodes in that given lymphatic station. The non-sentinel lymph nodes turn out to be histologically tumor positive in 8–33% of cases [66, 67]. Non-sentinel lymph node metastasis has been shown to represent an independent prognostic factor [68]. CLND improves staging and regional disease control, although its survival benefit is unproven [69, 70]. Active nodal basin surveillance with the US and adjuvant therapy is now offered to patients with a positive SLNB as an alternative to CLND. This is particularly the case of SLN micrometastasis. CLND may still be reasonable in the setting of high tumor burden in the SLN, a greater number of positive SLNs, and/or adverse histologic features in the primary cutaneous melanoma [7, 13, 69]. In any case, before performing a CLND, a detailed whole-body investigation is mandatory to avoid unnecessary surgery.
US and the SLNB
US scanning cannot replace the SLNB excision. However, US can help decrease the number of subjects to be submitted to the SLNB, which is an expensive, invasive (general anesthesia and surgical morbidity), and logistically demanding procedure [62, 71] (Fig. 10.12).
Heterogeneous results on the pre-SLNB US screening of lymph nodes have been published [14]. This is also due to the different quality of the scanners through the years, the addition or not of Doppler imaging to grayscale scanning, the different diagnostic criteria adopted, and the training of the operators [72]. Significant experience is required to distinguish efficaciously normal from metastatic lymph nodes, and specific expertise is needed. Some studies [73] have shown that US is not sufficiently sensitive in the pre-SLNB assessment of the lymph nodes. The US false negatives are mostly due to the false negative due to micrometastasis. However, it is interesting to note that US false negatives are associated with a lower tumor burden and better overall survival [74].
Chai and co-workers evaluated 325 patients before the SLNB procedure [73]. US showed 34% sensitivity, 86% specificity, 36.5% positive predictive value, and 84% negative predictive value. Sensitivity and specificity improved somewhat with increasing Breslow depth. Sensitivity was highest for the neck, but specificity was highest for the groin. In a limited study cohort, US proved more accurate than PET-CT in detecting metastatic lymph nodes before the SLNB procedure [75]. In the retrospective study by Olmedo et al. [76], US was 46% sensitive and 76% specific for the detection of unpalpable, metastatic lymph nodes in patients with melanoma (≥T1b). Use of US avoided SLNB in 6% of patients. False negatives were significantly more common in patients over 60 years and in melanomas <2 mm in thickness. The staging protocol with US and SLNB had a lower cost-effectiveness ratio than the protocol with SLNB alone (8095.24 Euros versus 28,605.00 Euros).
There are two main strategies suggested to improve the rather low sensitivity of pre-SLNB US. The first one is the systematic use of fine needle aspiration cytology (FNAC) on any suspicious or indeterminate lymph node identified at US scanning of the regional lymphatic station. In the study by van Rijk [77], the sensitivity and specificity of pre-SLNB US were 34% and 87%, respectively. In combination with FNAC, this was 5% and 100%, respectively. This yield was judged insufficient for US to be used as a routine diagnostic tool in selecting patients eligible for SLNB. As an alternative, some authors reported, although in a small series, the effective use of US contrast media in assessing the lymph nodes before SLNB [78]. The second possibility for improving US accuracy consists of the so-called targeted US, where US and FNAC are performed after lymphoscintigraphy, once the nuclear medicine physician has already identified the SLB and marked it on the skin [79,80,81,82,83,84]. The study from Voit and others that targeted US plus FNAC yielded a sensitivity of 51% and a specificity of 99% [84]. Oppositely, Sanki and collaborators had a 97% specificity for pre-SLNB-targeted US and a 24% sensitivity [79]. Pre-SLNB screening with targeted US and FNAC is regarded as cost effective, also saving patients from unnecessary surgery and the consequent undesired morbidity [85]. The real problem is the actual number of patients benefiting from this approach. Additionally, it must be kept in mind that the practice of targeted US requires an optimal organization (US and FNAC performed in the time slot between lymphoscintigraphy and surgery), with many different operators working together. It must be kept in mind that, even doing so, US will continue to miss micrometastases.
A Cochrane review published in 2019 [86] evaluated 11 studies on the pre-SLNB US. The summary sensitivity of US alone was 35%, and specificity was 94%. Combining US with FNAC revealed a summary sensitivity of 18 and specificity of 100%. When these data were translated to a hypothetical cohort of 1000 people eligible for SLNB, 237 of whom had nodal metastases (median prevalence), the combination of US with FNAC potentially allowed 43 people with nodal metastases to be triaged directly to adjuvant therapy rather than having SLNB first. This, at the cost of two people with a false-positive result and consequently with incorrect management. The authors concluded that imaging with US combined with FNAC before SLNB might identify around one-fifth of those with nodal disease, but that confidence intervals were found wide, and further work was regarded as necessary to establish the real cost-effectiveness.
In addition to pre-SLNB screening, US of regional lymph node station/s may be used to monitor the patients eligible for SLNB but who did not undergo this procedure or in whom the SLNB was technically unsuccessful [13].
Satellite, In-Transit, and Lymph Node Melanoma Metastasis: US Findings
US Imaging of Satellite/In-Transit Metastasis
Satellite and in-transit metastases, as well as hematogenous melanoma metastases to the skin, appear as solid nodules, hypoechoic relative to the surrounding fat, with a dermal or subcutaneous location [87] (Fig. 10.13). Marked hypoechogenicity is due to hypercellularity and too low sound reflection of melanin and not due to tumor necrosis [17, 37]. The shape is round, oval, or lobulated, and the contour is usually sharp [38]. Most lesions have a homogeneous internal echotexture. Sometimes, particularly in nodules larger than 6 mm, tiny fluid areas are encountered. Margins are well defined, being slightly irregular only in relatively larger lesions. Nodules frequently exhibit a good sound-wave transmission (Fig. 10.14). The combination of marked hypoechogenicity and dorsal acoustic enhancement may mimic a cystic-like change, such as a seroma.
Solivetti et al. [31] detected 95 satellite or in-transit lesions in 63 patients with a mean number of nodules ranging from 1 to 4. Six patients had multiple lesions arranged along the same lymphatic, the largest one being the farthest from the primary tumor site. Size ranged from 4 to 17 mm (mean, 8 mm), with only four lesions exceeding 1 cm in diameter. Since in-transit nodules grow along the lymphatic ducts, sometimes it is possible to note a hypoechoic band entering the metastasis on one side and exiting on the other, which is the direct image of the dilated duct filled with melanoma cells (“tail sign”). Sometimes the tumor cell-filled lymphatic channel connects multiple aligned in-transit metastases (“string sign”) [88] (Fig. 10.15).
Melanoma metastases show a variable degree of vascularization, ranging from scarce and peripheral to diffuse and intense [87, 89]. It should be noted that, although the presence of flow signals helps prove that a given abnormality is solid, the absence of vascularization does not help exclude melanoma metastasis. When a small subcutaneous lesion is found, possibly indicating a satellite or an in-transit nodule, detection of even minimal flow signals can allow proper differentiation from other abnormalities such as small seromas and cysts (Fig. 10.16). However, even using highly sensitive scanners and slow-flow settings, small melanoma metastases may not show any internal vascularity. In Solivetti’s study [31], 6 out of 53 lesions did not display any vascular signal inside, and only lesions larger than 7 mm in diameter showed vascularity at power Doppler imaging.
To date, there is no specific study on elastography assessment of in-transit melanoma metastasis. Anyway, as with most malignant soft-tissue lesions, melanoma metastases are stiff at strain elastography assessment [90, 91]. This high stiffness can be homogeneous or heterogeneous (Fig. 10.17).
US Imaging of Lymph Node Metastasis
The operator should be adequately aware of the sonographic appearance of normal, reactively enlarged, involutivity enlarged (fatty metamorphosis), inflammatory (acute and chronic lymphadenitis), and neoplastic lymph nodes. He or she should also be aware that the appearance of normal lymph nodes may differ between the various lymphatic stations (neck, axilla, and inguinal region). For example, axillary and inguinal lymph nodes may show a wavy subcapsular sinus (horseshoe lymph node), while normal neck lymph nodes may exhibit a small and eccentric hyperechoic sinus or an absent sinus [14].
Lymph node assessment is based on analyzing the size, shape, border, internal echotexture, and vascularization (Fig. 10.18). Several features indicating malignancy have been described, and the operator should always look for a combination of grayscale and Doppler findings [79, 92]. A systematic review showed how the various published series on melanoma nodal metastasis using US employed quite heterogeneous criteria. In some articles, the diagnostic criteria were not even described [72].
Suspicious changes in a lymph node. Marked, asymmetric cortical thickening with small hilum (a). Limited but asymmetric cortical thickening (b). Cortical thickening with focal tumor deposits (c). Marked, symmetric cortical thickening with small hilum (d). Infiltration of the peri-nodal fat tissue (e). Round lymph node with small hilum (f). Round lymph node with absent hilum (g)
Lymph node size by itself is not relevant. Clearly, a lymph node with a nonspecific appearance (e.g., with a slightly thickened cortex) becomes more suspicious if it is also large. Small lymph nodes may sometimes appear round or show a loss of hilar hyperechogenicity or cortical thickening. However, they will still be considered benign if these changes are not marked. Instead, the same changes would be considered suspicious in a large lymph node. The shape of the lymph node is suspicious when oval and even more when round shaped (“balloon shaped”) while more reassuring if elongated [93]. Some authors consider an L/T ratio <2 suspicious, whereas others consider an L/T ratio <1.5 suspicious [22, 72]. A threshold of 1.5 increases the rather low specificity of the size criterion.
More relevance must be given to cortical changes, indicating an early stage of lymph node metastasis (Figs. 10.19 and 10.20). Lymphatic channel-borne tumor cells first reach the marginal sinus in the lymph node periphery. Consequently, metastatic foci grow first within the cortex, extending subsequently into the rest of the node. Lymph nodes showing a diffuse but symmetric (circumferential) thickening of the cortex must be considered indeterminate. Instead, lymph nodes with asymmetric (unilateral) cortical thickening are highly suspicious of metastatic involvement. The more the thickness, the more the suspicion, particularly in the case of a hump-like cortex [75]. Lymph nodes with focal, eventually nodular, thickening of the cortex are overtly metastatic [92, 93]. This “nodule within the node” can be isoechoic or hypoechoic compared to the rest of the cortex. If hypoechoic, it virtually indicates partial metastasis, while if isoechoic, it is suspect, particularly if large and/or hypervascularized at Doppler imaging [22, 92, 93]. Focal metastasis may develop in lymph nodes that are very oblong, not just oval, with an evident echoic hilum and with a very thin cortex in all other areas, but that lymph node will still be confidently diagnosed as metastatic [94]. Other tumors produce focal protuberances of the lymph node contour, but these nodules are usually isoechoic to the remaining cortex. Melanoma may give rise to focal deposits, which are typically hypoechoic in comparison with the cortex (“echo-free island”) [95]. These focal changes can be further assessed with a targeted FNAC or contrast medium injection [96] (Figs. 10.21 and 10.22).
Together with evaluating the appearance of the cortex, changes within the central hyperechoic “hilum” must be considered. The hilar region can be displaced, reduced in size, overtly inhomogeneous, or totally replaced [97]. A small hilum can be a nonspecific finding, but hilar displacement by asymmetric or focal cortical thickening or partial or total substitution of the hilum with hypoechoic tissue indicates metastasis [92]. An appropriately set scanner frequently allows us to recognize a marked hypoechogenicity within melanoma metastasis involving part of or the entire lymph node. This low-level echotexture is rather typical of melanoma metastases. Various conditions can be associated with a round or oval nodular hypoechoic image within the soft tissues, including normal or abnormal vessels, dense scars, fluid collections (e.g., seromas, hematomas, and lymphoceles), cysts, abscesses, and benign tumors. Nevertheless, the patient’s history, combined with B-mode and color Doppler findings, usually allows adequate differentiation.
In a case in which the lymph node shows some subtle abnormality, such as a cortex that is slightly thicker than usual or slightly asymmetric, it can be helpful to look for similarly appearing lymph nodes in the same lymphatic basin as well as in the contralateral basin. Obviously, this is not a rigorous practice, but it is also evident that the suspicion of malignancy decreases considerably when similar changes are found in multiple nodes and mainly when these other lymph nodes are contralateral to the primary tumor (Catalano et al. 2010e).
Color and power Doppler imaging of any abnormal lymph node is mandatory. Benign lymph nodes show monopolar vascularization, with vessels entering the lymph node hilum and regularly distributing toward the periphery (without reaching the nodal cortex). In malignant lymph nodes, this “color hilum” is lost or displaced while multiple vessels penetrate the nodal capsule and enter the lymph node, distributing anarchically (capsular vascularization or “peripheral perfusion”) [15, 92, 93]. Doppler US is particularly helpful in some indeterminate circumstances, improving the operator’s confidence in suspecting malignancy. When a lymph node shows diffuse thickening of the cortex (i.e., a lower than usual size of the echoic hilum), detecting hilar vascularization decreases the suspicion, whereas an abnormal vessel distribution prompts further investigation. Also, when B-mode imaging shows isoechoic asymmetric thickening of the lymph node cortex or focal bulging of the cortex, Doppler techniques may show somewhat different vascularization of the suspected area, being more or less vascularized than the remaining portions of the lymph node or clearly showing capsular vessels directly related to that area (Catalano et al. 2010e).
Recent studies have investigated the role of elastography in the assessment of suspicious lymph nodes in melanoma patients. A significant correlation between lymph node stiffness and malignant involvement was demonstrated. Hinz [98] evaluated 36 patients scheduled for lymph node excision because of suspicious US findings or due to a planned SLNB procedure. At strain elastography, 90.5% of metastatic lymph nodes showed a pattern of 3, 4, or 5 (according to the percentage of high stiffness areas within the lymph node), while of all benign lymph nodes, 76% had a pattern of 1 or 2. The sensitivity and specificity of grayscale and power Doppler US were 81% and 76%, respectively; 90.5% and 76% for elastography; and 95% and 76% for the combined assessment. Ogata et al. evaluated 13 metastatic lymph nodes and 7 reactive lymph nodes in 12 melanoma patients [99]. Sensitivity and specificity were 100% and 71%, respectively, with a score cutoff value of 3; 92% and 100% for a score cutoff value of 4; and 77% and 57% for the B-mode US.
The contrast-enhanced US has proven effective in characterizing focal hypoechoic cortical changes within otherwise normal lymph nodes. In the study of Rubaltelli et al. [96] on 44 lymph nodes, the area of focal thickening showed a contrast enhancement similar to that of the remaining cortex in 29 cases, while it was hypoenhanced in the remaining 15 cases. Compared to FNAC, contrast-enhanced US yielded a 100% sensitivity and a 93.5% specificity.
Cutaneous Melanoma Follow-Up
As for any tumor, a surveillance strategy should be established based on the individual risk of recurrence. In the case of melanoma, however, patients undergo periodic follow-up not only to detect a tumor relapse but also to identify any new primary melanoma. Ninety percent of all melanoma metastases occur during the first 5 years after surgery. However, late metastasis does occur [1]. It is of note that up to 62% of local, satellite/in-transit, and regional nodal recurrences are detected by the patients themselves [100, 101]. Many others are found by physicians.
Melanoma recurrence may develop at the level of the primary tumor scar, in the skin around the scar and toward the regional lymph node station, at the level of the regional lymph nodes, or in the deep viscera (Figs. 10.23, 10.24, 10.25, 10.26, and 10.27). The latter aspect is beyond the purpose of this textbook. In the study by Franken, the first melanoma relapse type was local in 13% of cases, in-transit in 17%, in regional lymph nodes in 46%, and distant in 24% [101].
There is no international consensus on the intensity, timing, and length of surveillance in melanoma patients, as well as on the use of US in addition to medical history, clinical examination, and blood testing. Surveillance strategy should be stage specific and, as possible, patient tailored, according to the age, individual risk, etc. Follow-up rules vary worldwide, ranging in frequency from 2 to 4 times per year for 3 to 10 years [1, 13]. Closer monitorization is usually chosen in the first 5 years, while less intensity is generally adopted in the subsequent 5 years. Some centers do not use US at all, some others limit US to the regional lymph node station(s), and some others extend US to the scar, lymphatic basin, regional lymph node station(s), and even non-regional lymph node stations. Recent European multidisciplinary guidelines recommend US of lymph node station/s in the first 3 years after surgery [1]. US is more sensitive and more specific than palpation [22, 97, 102,103,104], although its benefit on patients’ survival is not proven. US appears to be the best imaging modality to detect lymph node disease compared to CT and PET-CT [1].
Accurate US investigation of melanoma patients, carefully exploring the regional lymph node station(s), the scar(s), and the skin in between, is time consuming [105]. Additionally, its real impact on patient survival is unclear. By analyzing two prospective cohorts of patients with early-stage melanoma (IB–IIA), Ribero et al. [106] found that, compared to clinical-based follow-up, US-based follow-up did not improve distant metastases-free survival, disease-free interval, nodal metastases-free survival, and melanoma-specific survival. The US-based follow-up did not increase the survival of patients in stage IB–IIA [107]. However, performing a US exam for assessing the lymph node status in melanoma patients with AJCC T1b stage and above is advisable according to the most recent international guidelines [1]. The introduction of the new treatments (targeted drugs and immunotherapies) may favorably impact the need for early diagnosis of recurrence in the future [13].
US is a sensitive and moderately specific method for evaluating superficial lymph nodes during the follow-up of melanoma patients. US is more accurate than palpation [13]. A single-center prospective study [108] evaluated with a physical exam and US a total of 6328 lymphatic drainage areas in 1288 melanoma patients at 4435 follow-up consultations. The sensitivity and specificity for US were 89% and 100%, respectively, and 71% and 100% for clinical examination. Clinical examination was least sensitive in the supraclavicular, axillary, and infraclavicular regions. US is superior to CT, PET, and PET-CT in detecting lymph node metastasis [109]. US follow-up is of particular value when nodal observation after positive SLNB is chosen as an alternative to CLND. In these subjects, although, again, the survival benefit is unproven, serial US scanning allows detection of tumor recurrence in the regional lymph node station.
FNAC has a high positive predictive value in cases with abnormal US findings. Solivetti et al. [110] evaluated 480 patients with skin tumors, mostly melanoma, undergoing US-guided FNAC of suspicious recurrent lymph nodes. Out of the 336 US-positive patients, 231 (69%) were positive at cytology. Of the 144 US negatives, 132 (92%) were FNAC negatives. Consequently, the negative predictive value of US was 92%, and the positive predictive value was 69%.
FNAC has a quite high accuracy in diagnosing melanoma metastatic to the skin. US plus FNAC is the first-line option in subjects with a clinically suspected mass and a history of melanoma [111, 112]. A 2013 meta-analysis of palpation and US-guided FNAC found a pooled sensitivity of 97% and a pooled specificity of 99% [112]. Causes for false-negative results include inadequate sampling, obesity, challenging areas for aspiration, intense fibrosis or a previous scar, small size, or poor circumscription of the suspicious lesion. The use of US guidance limits the significance of these factors. The most common cause of a false-positive result is a second malignancy, particularly in the case of a paucicellular smear. False-positive results may also occur due to overinterpretation of reactive fibroblasts as well as spindle cell lesions from nodular fasciitis and presence of atypical histiocytes, which may mimic melanoma cells [112]. US-guided FNAC is also useful in clinically misinterpreted melanoma metastases [113].
US Guidance for Diagnostic and Therapeutic Procedures
Real-time US represents the best guide to perform percutaneous procedures in the melanoma patient. Sonographically guided FNAC is more effective than palpation-guided FNAC [114]. Sonographic guidance reduces the number of false-negative results by indicating the most suspicious lymph node within a given station, by driving the needle toward small, not palpable, targets, and by showing that the needle tip is actually within the lymph node [22, 114]. US guidance is employed in a targeted way, directing the needle toward the most suspicious area of the lymph node, such as hypoechoic focal thickening of the cortex or the thickest and most vascularized area of the cortex. This allows avoiding areas at a greater risk of having a necrotic content, such as those with a very hypoechoic texture and without Doppler flow signals.
Usually, the freehand technique is employed, with small-diameter needles (21–22 gauge) attached to a 10-mL plastic syringe for superficial lesions and a 22-gauge spinal needle for deeper lesions (Catalano et al. 2010e). Some authors prefer using 25–27-gauge needles [14, 113]. The use of larger needles is not associated with a greater risk of tumor seeding, which is usually not found after lymph node FNAC in patients with melanoma; instead, a larger needle allows sampling of a slightly greater amount of material, consequently decreasing the need for sample repetition. An active aspiration is carried out when the needle tip is seen within the target. Some authors, however, rely on passive suction (capillarity) unless the target is very small [14]. To-and-fro, multidirectional needle movements inside the target are mandatory for an optimal result (Fig. 10.28).
If possible, FNAC samplings are extemporarily evaluated by the on-site cytopathologist from air-dried slides with rapid Romanowsky coloration. The puncture is repeated immediately in cases of indeterminate/unrepresentative smears or when there is a discrepancy between the clinical, sonographic, and cytologic findings. A definitive cytopathologic assessment from Papanicolaou staining will confirm the preliminary diagnosis (Figs. 10.29 and 10.30). The cytopathologic assessment includes immunocytochemical analysis, with special reference to the melanocyte marker HMB-45. Histologic assessment may be carried out for uncommon cases with indeterminate FNAC findings. As an alternative, some authors have employed core biopsy instead of FNAC to assess suspected lymph nodes in melanoma patients [115]. Sensitivity was 98% and specificity 100%.
US can be employed for presurgical targeting of melanoma metastases. In cases of deep and/or small locoregional metastasis, it is possible to mark the overlying skin with a pencil or, if necessary, to place a percutaneous guidewire preoperatively [116, 117]. A variety of guidewires are commercially available, some of which are repositionable once their placement is not in the ideally desired point, and some others not. The use of guidewire is also helpful in the case of melanoma lesions located in the proximity of vulnerable structures.
Electrochemotherapy is a local, nonthermal treatment combining electric pulses with intravenous or intratumoral injection of anticancer agents to obtain local tumor control. Electrochemotherapy is a safe and effective treatment, albeit basically palliative, for cutaneous and subcutaneous melanoma metastasis [118, 119]. Accurate positioning of electrodes within non-palpable nodules requires intraoperative US guidance [119, 120]. Solivetti et al. [105] evaluated 15 melanoma patients scheduled to be treated with electrochemotherapy for in-transit metastasis. US could detect all the 52 lesions, PET-CT 43% of them, and telethermography 28%. PET-CT also yielded a 4% false-positives rate.
Response to Treatment
New antiangiogenic and targeted treatments for metastatic melanoma require early assessment of response to treatment to discriminate between responding and non-responding patients. Classical dimensional criteria (RECIST 1.1) fit well for conventional chemotherapy, but the new drugs require a functional assessment since their effect on the lesions is first of inactivation and only in a second moment of coarctation. Some initial experiences with US contrast media in imaging in-transit melanoma metastasis led to interesting results on the lesion devascularization as an indicator of good response [41, 121].
Intratumoral immunotherapy is approved for stage IIIB–IV melanoma. RECIST does not allow US for lesion measurement because of operator dependence and difficulty with standardization. However, in practice, US may be the only choice for some subcutaneous lesions. Therefore, the newly developed itRECIST permits US measurement if no other lesions are available for quantitative assessment. When feasible, the same operator should perform the US at all visits using the same equipment and acquisition parameters, capturing lesion images in a similar orientation, with anatomic landmarks to align with preceding scans [122].
US of Cutaneous Melanoma: Challenging Aspects and Essential Requirements
In 2018, the European Cancer Organisation (ECCO) published the essential requirements for quality cancer care in melanoma patients [7]. Many challenges in melanoma care were identified by the panel of experts. Among these, those related to imaging, US included, were the following:
-
Insufficient knowledge of and experience in detection and treatment of satellite or in-transit metastasis.
-
Locoregional staging and follow-up with US techniques require updated scanners and specific operator expertise, which can lead to inter-observer variability in the US diagnosis of lymph node stations and varying outcomes of fine needle aspirations.
-
Underuse or overuse of diagnostic modalities, such as PET-CT, based on local availability or nonadherence to guidelines. The rate of metastatic cases among the patient population is relatively low. Extensive use of imaging modalities for staging and follow-up of early lesions may incur high costs, false-positive findings, radiation exposure, and potential contrast media-related toxicity and allergy.
The ECCO article [7] also listed a number of requirements believed to be essential by the experts. The recommendations concerning specifically radiological imaging, US included, were the following:
-
Radiologists must know the peculiar pattern of lymphatic spread of melanoma (satellitosis, in-transit metastasis, lymph node metastasis) and the modality of hematogenous diffusion (including uncommon sites of spread).
-
When performing/interpreting imaging studies, radiologists must be aware of patient history; knowledge is mandatory of the primary melanoma site, SLNB localization (if investigated), SLNB result, any prior or concurrent site of metastatic involvement, and any previous or ongoing treatment.
-
Radiologists must have interaction with the patient—as many superficial tumor localizations are self-palpated, any minimal symptom or finding must be considered.
-
Radiologists must have the latest equipment. This includes dermatology transducers (>15 MHz) and color Doppler mode for US, multidetector scanners (≥16 detector rows) for CT, high-magnetic-field scanners (≥1.5 T), liver-specific contrast media, diffusion-weighted imaging mode for magnetic resonance (MR), and workstations for CT and MR image processing.
-
High-resolution US with Doppler assessment is mandatory to detect locoregional metastasis. Two-phase liver acquisition (arterial phase and portal phase) CT is necessary to improve both the sensitivity and specificity in assessing liver lesions. Chest scans must include the neck base, while pelvic scans must encompass the inguinocrural region. MR imaging, particularly brain MR, must be performed in case of indeterminate or discrepant CT findings or when radiation therapy is planned.
-
Radiologists must have expertise in performing US- or CT-guided percutaneous procedures, including fine needle cytology, placement of presurgical guidewires, and aspiration of lymphoceles.
-
Radiologists assessing response to treatment must be made aware of ongoing therapy (immunotherapy, targeted therapy, isolated limb perfusion, chemoperfusion, electrochemotherapy, etc.). They must be familiar with peculiar phenomena related to innovative therapy (pseudo-progression, etc.) as well as with the main related complications.
Conclusions and Future Perspectives
Though several articles, albeit with nonuniform results, have been published through the years, US has not become a routine tool in the initial workup of primary cutaneous melanoma. The management is still based on primary tumor surgical biopsy and SLNB procedure [13, 56]. However, surgery-based management is a multistep approach. In the worst case, for example, melanoma thicker than 1 mm and positive SLNB, the patient undergoes surgery three times: primary tumor biopsy, re-excision plus SLNB, and CLND. From a theoretical point of view, US-based management would allow a single-step approach to be carried out in this subject. As a matter of facts, the US measurement of the primary tumor would show a thickness >1 mm while the regional lymphatic station US exploration (plus FNAC sampling) would demonstrate a positive lymph-node, prompting radical lymphadenectomy. Further studies are needed to understand if, and in what percentage of subjects, this management is feasible in clinical practice. However, a preliminary change in mentality is first needed.
US is playing a growing role in the locoregional staging, pre-SLNB nodal screening, and follow-up of patients with cutaneous melanoma. US of the locoregional lymph nodes is recommended for the initial workup of all primary cutaneous melanomas pT1b and higher [1]. Additionally, being more sensitive and specific than physical examination, US has been incorporated in most melanoma patient surveillance guidelines. US is also the method of choice in real-time guidance of percutaneous procedures such as FNAC, core biopsy, and presurgical guidewire placement. Finally, US is useful to monitor response to treatment in subjects with skin-limited melanoma metastasis.
To make US effective in a melanoma patient, state-of-the-art equipment, specific operator training, careful examination, and interdisciplinary cooperation are needed [13].
Abbreviations
- CLND:
-
Complete lymph node dissection
- CT:
-
Computed tomography
- EFOV:
-
Extended field-of-view
- FNAC:
-
Fine needle aspiration cytology
- L/T:
-
Longitudinal-to-transverse ratio
- PET:
-
Positron-emission tomography
- SLN:
-
Sentinel lymph node
- SLNB:
-
Sentinel lymph node biopsy
- US:
-
Ultrasound
References
Garbe C, Amaral T, Peris K, et al. European consensus-based interdisciplinary guideline for melanoma. Part 1: Diagnostics—update 2019. Eur J Cancer. 2020;126:141–58.
Hartman RI, Lin JY. Cutaneous melanoma: a review in detection, staging, and management. Hematol Oncol Clin North Am. 2019;33:25–38.
Botar-Jid CM, Cosgarea R, Bolboacă SD, et al. Assessment of cutaneous melanoma by use of very-high-frequency ultrasound and real-time elastography. AJR. 2016;206:699–704.
Catalano O, Alfabete Roldan F, Varelli C, et al. Skin cancer: findings and role of high-resolution ultrasound. J Ultrasound. 2019;22:423–31.
Michielin O, van Akkooi ACJ, Ascierto PA, et al. Cutaneous melanoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30:1884–901.
Leonardi GC, Falzone L, Salemi R, et al. Cutaneous melanoma: from pathogenesis to therapy (review). Int J Oncol. 2018;52:1071–80.
Wouters MW, Michielin O, Basitane E, et al. ECCO essential requirements for quality cancer care: melanoma. Crit Rev Oncol Hematol. 2018;122:164–78.
Guy GP Jr, Thomas CC, Thompson T, et al. Vital signs: melanoma incidence and mortality trends and projections - United States, 1982-2030. MMWR Morb Mortal Wkly Rep. 2015;64:591–6.
Schadendorf D, van Akkooi ACJ, Berking C, et al. Melanoma. Lancet. 2018;392:971–84.
Elder DE, Bastian BC, Cree IA, et al. The 2018 World Health Organization classification of cutaneous, mucosal, and uveal melanoma: detailed analysis of 9 distinct subtypes defined by their evolutionary pathway. Arch Pathol Lab Med. 2020;144:500–22.
Fernández Canedo I, de Troya MM, Fúnez Liébana R, et al. Preoperative 15-MHz ultrasound assessment of tumor thickness in malignant melanoma. Actas Dermosifiliogr. 2013;104:227–31.
Scolyer RA, Judge MJ, Evans A, et al. Data set for pathology reporting of cutaneous invasive melanoma: recommendations from the international collaboration on cancer reporting (ICCR). Am J Surg Pathol. 2013;37:1797–814.
Swetter SM, Tsao H, Bichakjian CK, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 2019;80:208–50.
Thompson JF, Haydu LE, Sanki A, et al. Ultrasound assessment of lymph nodes in the management of early-stage melanoma. J Surg Oncol. 2011;104:354–60.
Ulrich J, van Akkooi AJ, Eggermont AM, et al. New developments in melanoma: utility of ultrasound imaging (initial staging, follow-up and pre-SLNB). Expert Rev Anticancer Ther. 2011;11:1693–701.
Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma staging: evidence-based changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:472–92.
Catalano O, Voit C. Locoregional staging of melanoma. In: Wortsman X, GBE J, editors. Dermatologic ultrasound - clinical and histologic correlations. Berlin: Springer; 2014.
Wortsman X, Wortsman J. Clinical usefulness of variable-frequency ultrasound in localized lesions of the skin. J Am Acad Dermatol. 2010;62:247–56.
Catalano O, Wortsman X. Dermatology ultrasound. Imaging technique, tips and tricks, high-resolution anatomy. Ultrasound Q. 2020;36:321–7.
Wortsman X. Common applications of dermatologic sonography. J Ultrasound Med. 2012a;31:97–111.
Uematsu T, Kasami M, Kiyohara Y. B-mode ultrasound imaging, Doppler imaging, and real-time elastography in cutaneous malignant melanoma and lymph node metastases. Healthcare (Basel). 2013;1:84–95.
Uren RF, Sanki A, Thompson JF. The utility of ultrasound in patients with melanoma. Expert Rev Anticancer Ther. 2007;7:1633–42.
Catalano O, Sandomenico F, Siani A. Value of the extended field of view modality in the sonographic imaging of cutaneous melanoma: a pictorial essay. Dermatol Surg. 2010a;36:1300–4.
Wortsman X. Sonography of the primary cutaneous melanoma: a review. Radiol Res Pract. 2012b;2012:814396.
Corvino A, Sandomenico F, Corvino F, et al. Utility of a gel stand-off pad in the detection of Doppler signal on focal nodular lesions of the skin. J Ultrasound. 2020;23:45–53.
Hambardzumyan M, Hayrapetyan A. Ultrasound analytic criteria for diagnosing cutaneous malignant melanoma. J Dermatol Res. 2018;3:32–6.
Catalano O. Cancer measurement at ultrasound: state of the art. Ultrasound Q. 2017;33:116–24.
Andrekute K, Valiukeviciene S, Raisutis R, et al. Automated estimation of melanocytic skin tumor thickness by ultrasonic radiofrequency data. J Ultrasound Med. 2016;35:857–65.
Catalano O, Nunziata A, Saturnino PP, et al. Epitrochlear lymph nodes: anatomy, clinical aspects, and sonography features. Pictorial essay. J Ultrasound. 2010c;13:168–74.
Blum A, Schmid-Wendtner MH, Mauss-Kiefer V, et al. Ultrasound mapping of lymph node and subcutaneous metastases in patients with cutaneous melanoma: results of a prospective multicenter study. Dermatology. 2006;212:47–52.
Solivetti FM, Di Luca SA, Pirozzi G, et al. Sonographic evaluation of clinically occult in-transit and satellite metastases from cutaneous malignant melanoma. Radiol Med. 2006;111:702–8.
Catalano O, Siani A. Cutaneous melanoma: role of ultrasound in the assessment of locoregional spread. Curr Probl Diagn Radiol. 2010;39:30–6.
Catalano O, Setola SV, Vallone P, e t al. Sonography for locoregional staging and follow-up of cutaneous melanoma. J Ultrasound Med. 2010d;29:791–802.
Marone U, Caracò C, Chiofalo MG, et al. Resection in the popliteal fossa for metastatic melanoma. World J Surg Oncol. 2007;5:8.
Uren RF, Howman-Giles R, Thompson JF, et al. Interval nodes: the forgotten sentinel nodes in patients with melanoma. Arch Surg. 2000;135:1168–72.
Hambardzumyan M, Hayrapetyan A. Differential diagnosis of malignant melanoma and benign cutaneous lesions by ultrasound analysis. Sci Med J. 2020;2:2.
Catalano O, Voit C, Sandomenico F, et al. Previously reported sonographic appearances of regional melanoma metastases are not likely due to necrosis. J Ultrasound Med. 2011;30:1041–9.
Catalano O, Caracò C, Mozzillo N, et al. Locoregional spread of cutaneous melanoma: sonography findings. AJR. 2010b;194:735–45.
Botar Jid C, Bolboacă SD, Cosgarea R, et al. Doppler ultrasound and strain elastography in the assessment of cutaneous melanoma: preliminary results. Med Ultrason. 2015;17:509–14.
Hinz T, Wenzel J, Schmid-Wendtner MH. Real-time tissue elastography: a helpful tool in the diagnosis of cutaneous melanoma? J Am Acad Dermatol. 2011;5:424–6.
Chami L, Lassau N, Chebil M, Robert C. Imaging of melanoma: usefulness of ultrasonography before and after contrast injection for diagnosis and early evaluation of treatment. Clin Cosmet Investig Dermatol. 2011;4:1–6.
Dinnes J, Bamber J, Chuchu N, et al. High-frequency ultrasound for diagnosing skin cancer in adults. Cochrane Database Syst Rev. 2018;12:CD013188.
Bessoud B, Lassau N, Koscielny S, et al. High-frequency sonography and color Doppler in the management of pigmented skin lesions. Ultrasound Med Biol. 2003;29:875–9.
Harland C, Kale S, Jackson P, et al. Differentiation of common benign pigmented skin lesions from melanoma by high resolution ultrasound. Br J Dermatol. 2000;143:281–9.
Jasaitiene D, Valiukeviciene S, Linkeviciute G. Principles of high-frequency ultrasonography for investigation of skin pathology. J Eur Acad Dermatol Venereol. 2011;25:375–82.
Machet L, Belot V, Naouri M, et al. Preoperative measurement of thickness of cutaneous melanoma using high-resolution 20 MHz ultrasound imaging: a monocenter prospective study and systematic review of the literature. Ultrasound Med Biol. 2009;35:1411–20.
Piłat P, Borzęcki A, Jazienicki M, et al. Skin melanoma imaging using ultrasonography: a literature review. Postepy Dermatol Alergol. 2018;35:238–42.
Gamblicher T, Moussa G, Bahrenberg K, et al. Preoperative ultrasonic assessment of thin melanocytic skin lesions using a 100-MHz ultrasound transducer: a comparative study. Dermatol Surg. 2007;33:818–24.
Guitera P, Li LX, Crotty K, et al. Melanoma histological Breslow thickness predicted by 75-MHz ultrasonography. Br J Dermatol. 2008;159:364–9.
Music MM, Hertl K, Kadivec M, et al. Pre-operative ultrasound with a 12-15 MHz linear probe reliably differentiates between melanoma thicker and thinner than 1 mm. J Eur Acad Dermatol Venereol. 2010;24:1105–8.
Weichenthal M, Mohr P, Breitbart EW. The velocity of ultrasound in human primary melanoma tissue - implications for the clinical use of high-resolution sonography. BMC Dermatol. 2001;1:1.
Chaput L, Laurent E, Pare A, et al. One-step surgical removal of cutaneous melanoma with surgical margins based on preoperative ultrasound measurement of tumor thickness of the melanoma. Eur J Dermatol. 2018;28:202–8.
Lassau N, Koscielny S, Avril MF, et al. Prognostic value of angiogenesis evaluated with high-frequency and color Doppler sonography for preoperative assessment of melanomas. AJR. 2002;178:1547–51.
Lassau N, Lamuraglia M, Koscielny S, et al. Prognostic value of angiogenesis evaluated with high-frequency and colour Doppler sonography for preoperative assessment of primary cutaneous melanomas: correlation with recurrence after a 5 year follow-up period. Cancer Imaging. 2006;6:24–9.
Keung EZ, Gershenwald JE. The eighth edition American joint Committee on cancer (AJCC) melanoma staging system: implications for melanoma treatment and care. Expert Rev Anticancer Ther. 2018;18:775–84.
Morton DL, Thompson JF, Cochran AJ, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014;370:599–609.
Valsecchi ME, Silbermins D, de Rosa N, et al. Lymphatic mapping and sentinel lymph node biopsy in patients with melanoma: a meta-analysis. J Clin Oncol. 2011;29:1479–87.
Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127:392–9.
Wong SL, Balch CM, Hurley P, et al. Sentinel lymph node biopsy for melanoma: American Society of Clinical Oncology and Society of Surgical Oncology joint clinical practice guideline. J Clin Oncol. 2012;30:2912–8.
Gonzalez A. Sentinel lymph node biopsy: past and present implications for the management of cutaneous melanoma with nodal metastasis. Am J Clin Dermatol. 2018;19(Suppl 1):24–30.
Namikawa K, Yamazaki N, Nakai Y, et al. Prediction of additional lymph node positivity and clinical outcome of micrometastases in sentinel lymph nodes in cutaneous melanoma: a multi-institutional study of 450 patients in Japan. J Dermatol. 2012;39:130–7.
van Akkooi AC, Verhoef C, Eggermont AM. Importance of tumor load in the sentinel node in melanoma: clinical dilemmas. Nat Rev Clin Oncol. 2010b;7:446–54.
Karim RZ, Scolyer RA, Li W, et al. False negative sentinel lymph node biopsies in melanoma may result from deficiencies in nuclear medicine, surgery, or pathology. Ann Surg. 2008;247:1003–10.
Lam TK, Uren RF, Scolyer RA, et al. False-negative sentinel node biopsy because of obstruction of lymphatics by metastatic melanoma: the value of ultrasound in conjunction with preoperative lymphoscintigraphy. Melanoma Res. 2009;19:94–9.
Satzger I, Meier A, Hoy L, et al. Sentinel node dissection delays recurrence and prolongs melanoma-related survival: an analysis of 673 patients from a single center with long-term follow-up. Ann Surg Oncol. 2011;18:514–20.
Gershenwald JE, Andtbacka RH, Prieto VG, et al. Microscopic tumor burden in sentinel lymph nodes predicts synchronous nonsentinel lymph node involvement in patients with melanoma. J Clin Oncol. 2008;26:4296–303.
Reeves ME, Delgado R, Busam KJ, et al. Prediction of nonsentinel lymph node status in melanoma. Ann Surg Oncol. 2003;10:27–31.
Brown RE, Ross MI, Edwards MJ, et al. The prognostic significance of nonsentinel lymph node metastasis in melanoma. Ann Surg Oncol. 2010;17:3330–5.
Faries MB, Thompson JF, Cochran AJ, et al. Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med. 2017;376:2211–22.
Leiter U, Stadler R, Mauch C, et al. Complete lymph node dissection versus no dissection in patients with sentinel lymph node biopsy positive melanoma (DeCOG-SLT): a multicentre, randomised, phase 3 trial. Lancet Oncol. 2016;17:757–67.
Hocevar M, Bracko M, Pogacnik A, et al. The role of preoperative ultrasonography in reducing the number of sentinel lymph node procedures in melanoma. Melanoma Res. 2004;14:533–6.
Catalano O. Critical analysis of the ultrasonographic criteria for diagnosing lymph node metastasis in patients with cutaneous melanoma: a systematic review. J Ultrasound Med. 2011;30:547–60.
Chai CY, Zager JS, Szabunio MM, et al. Preoperative ultrasound is not useful for identifying nodal metastasis in melanoma patients undergoing sentinel node biopsy: preoperative ultrasound in clinically node-negative melanoma. Ann Surg Oncol. 2012;19:1100–6.
Pilko G, Zgajnar J, Music M, et al. Lower tumour burden and better overall survival in melanoma patients with regional lymph node metastases and negative preoperative ultrasound. Radiol Oncol. 2012;46:60–8.
Hinz T, Voth H, Ahmadzadehfar H, et al. Role of high-resolution ultrasound and PET/CT imaging for preoperative characterization of sentinel lymph nodes in cutaneous melanoma. Ultrasound Med Biol. 2013b;39:30–6.
Olmedo D, Brotons-Seguí M, Del Toro C, et al. Use of lymph node ultrasound prior to sentinel lymph node biopsy in 384 patients with melanoma: a cost-effectiveness analysis. Actas Dermosifiliogr. 2017;108:931–8.
van Rijk MC, Jelle Teertstra H, Peterse JL, et al. Ultrasonography and fine-needle aspiration cytology in the preoperative evaluation of melanoma patients eligible for sentinel node biopsy. Ann Surg Oncol. 2006;13:1511–6.
De Giorgi V, Gori A, Grazzini M, et al. Contrast-enhanced ultrasound: a filter role in AJCC stage I/II melanoma patients. Oncology. 2010;79:370–5.
Sanki A, Uren RF, Moncrieff M, et al. Targeted high-resolution ultrasound is not an effective substitute for sentinel lymph node biopsy in patients with primary cutaneous melanoma. J Clin Oncol. 2009;27:5614–9.
Starritt EC, Uren RF, Scolyer RA, et al. Ultrasound examination of sentinel nodes in the initial assessment of patients with primary cutaneous melanoma. Ann Surg Oncol. 2005;12:18–23.
Stoffels I, Dissemond J, Poeppel T, et al. Advantages of preoperative ultrasound in conjunction with lymphoscintigraphy in detecting malignant melanoma metastases in sentinel lymph nodes: a retrospective analysis in 221 patients with malignant melanoma AJCC stages I and II. J Eur Acad Dermatol Venereol. 2012;26:79–85.
Voit C, Kron M, Schäfer G, et al. Ultrasound-guided fine needle aspiration cytology prior to sentinel lymph node biopsy in melanoma patients. Ann Surg Oncol. 2006;13:1682–9.
Voit CA, van Akkoi AC, Schäfer-Hesterberg G, et al. Rotterdam criteria for sentinel node (SN) tumor burden and the accuracy of ultrasound (US)-guided fine-needle aspiration cytology (FNAC): can US-guided FNAC replace SN staging in patients with melanoma? J Clin Oncol. 2009;27:4994–5000.
Voit CA, Gooskens SL, Siegel P, et al. Ultrasound-guided fine needle aspiration cytology as an addendum to sentinel lymph node biopsy can perfect the staging strategy in melanoma patients. Eur J Cancer. 2014;50:2280–8.
van Akkooi AC, Voit CA, Verhoef C, et al. Potential cost-effectiveness of US-guided FNAC in melanoma patients as a primary procedure and in follow-up. Ann Surg Oncol. 2010a;17:660–2.
Dinnes J, Ferrante di Ruffano L, Takwoingi Y, et al. Ultrasound, CT, MRI, or PET-CT for staging and re-staging of adults with cutaneous melanoma. Cochrane Database Syst Rev. 2019;7:CD012806.
Nazarian LN, Alexander AA, Kurtz AB, et al. Superficial melanoma metastases: appearances on gray-scale and color Doppler sonography. AJR. 1998;170:459–63.
Corvino A, Corvino F, Catalano O, et al. The tail and the string sign: new sonographic features of subcutaneous melanoma metastasis. Ultrasound Med Biol. 2017;43:370–4.
Alexander AA, Nazarian LN, Capuzzi DM Jr, er al. Color Doppler sonographic detection of tumor flow in superficial melanoma metastases: histologic correlation. J Ultrasound Med. 1998;17:123–6.
Cohen J, Riishede I, Carlsen JF, et al. Can strain elastography predict malignancy of soft tissue tumors in a tertiary sarcoma center? Diagnostics (Basel). 2020;10:148.
Li S, Liu L, Lv G. Diagnostic value of strain elastography for differentiating benign and malignant soft tissue masses. Oncol Lett. 2017;14:2041–4.
Marone U, Catalano O, Caracò C, et al. Can high-resolution ultrasound avoid the sentinel lymph-node biopsy procedure in the staging process of patients with stage I-II cutaneous melanoma? Ultraschall Med. 2012;33:E179–85.
Voit C, van Akkooi AC, Schafer-Hesterberg G, et al. Ultrasound morphology criteria predict metastatic disease of the sentinel nodes in patients with melanoma. J Clin Oncol. 2010;28:847–52.
Tregnaghi A, De Candia A, Calderone M, et al. Ultrasonographic evaluation of superficial lymph node metastases in melanoma. Eur J Radiol. 1997;24:216–21.
Voit CA, Oude Ophuis CM, Ulrich J, et al. Ultrasound of the sentinel node in melanoma patients: echo-free island is a discriminatory morphologic feature for node positivity. Melanoma Res. 2016;26:267–71.
Rubaltelli L, Beltrame V, Tregnaghi A, et al. Contrast-enhanced ultrasound for characterizing lymph nodes with focal cortical thickening in patients with cutaneous melanoma. AJR. 2011;196:W8–12.
Saiag P, Bernard M, Beauchet A, et al. Ultrasonography using simple diagnostic criteria vs palpation for the detection of regional lymph node metastases of melanoma. Arch Dermatol. 2005;41:183–9.
Hinz T, Hoeller T, Wenzel J, et al. Real-time tissue elastography as promising diagnostic tool for diagnosis of lymph node metastases in patients with malignant melanoma: a prospective single-center experience. Dermatology. 2013a;226:81–90.
Ogata D, Uematsu T, Yoshikawa S, et al. Accuracy of real-time ultrasound elastography in the differential diagnosis of lymph nodes in cutaneous malignant melanoma (CMM): a pilot study. Int J Clin Oncol. 2014;19:716–21.
Francken AB, Bastiaannet E, Hoekstra HJ. Follow-up in patients with localised primary cutaneous melanoma. Lancet Oncol. 2005;6:608–21.
Francken AB, Shaw HM, Accortt NA, et al. Detection of first relapse in cutaneous melanoma patients: implications for the formulation of evidence-based follow-up guidelines. Ann Surg Oncol. 2007;14:1924–33.
Bafounta ML, Beauchet A, Chagnon S, et al. Ultrasonography or palpation for detection of melanoma nodal invasion: a meta-analysis. Lancet Oncol. 2004;5:673–80.
Machet L, Nemeth-Normand F, Giraudeau B, et al. Is ultrasound lymph node examination superior to clinical examination in melanoma follow-up? A monocentre cohort study of 373 patients. Br J Dermatol. 2005;152:66–70.
Voit C, Mayer T, Kron M, et al. Efficacy of ultrasound B-scan compared with physical examination in follow-up of melanoma patients. Cancer. 2001a;91:2409–16.
Solivetti FM, Desiderio F, Guerrisi A, et al. HF ultrasound vs PET-CT and telethermography in the diagnosis of in-transit metastases from melanoma: a prospective study and review of the literature. J Exp Clin Cancer Res. 2014a;33:96.
Ribero S, Podlipnik S, Osella-Abate S, et al. Ultrasound-based follow-up does not increase survival in early-stage melanoma patients: a comparative cohort study. Eur J Cancer. 2017;85:59–66.
Podlipnik S, Carrera C, Sanchez M, et al. Performance of diagnostic tests in an intensive follow-up protocol for patients with American joint Committee on cancer (AJCC) stage IIB, IIC, and III localized primary melanoma: a prospective cohort study. J Am Acad Dermatol. 2016;75:516–24.
Blum A, Schlagenhauff B, Stroebel W, et al. Ultrasound examination of regional lymph nodes significantly improves early detection of locoregional metastases during the follow-up of patients with cutaneous melanoma. Results of a prospective study of 1288 patients. Cancer. 2000;88:2534–9.
Xing Y, Bronstein Y, Ross MI, et al. Contemporary diagnostic imaging modalities for the staging and surveillance of melanoma patients: a meta-analysis. J Natl Cancer Inst. 2011;103:129–42.
Solivetti FM, Elia F, Santaguida MG, et al. The role of ultrasound and ultrasound-guided fine needle aspiration biopsy of lymph nodes in patients with skin tumours. Radiol Oncol. 2014b;48:29–34.
Covarelli P, Burini G, Barberini F, et al. The integrated role of ultrasonography in the diagnosis of soft tissue metastases from melanoma: preliminary report of a single-center experience and literature review. In Vivo. 2013;27:827–33.
Hall BJ, Schmidt RL, Sharma RR, et al. Fine-needle aspiration cytology for the diagnosis of metastatic melanoma. Systematic review and meta-analysis. Am J Clin Pathol. 2013;140:635–42.
Schäfer-Hesterberg G, Schoengen A, Sterry W, et al. Use of ultrasound to early identify, diagnose and localize metastases in melanoma patients. Expert Rev Anticancer Ther. 2007;7:1707–16.
Voit CA, van Akkooi AC, Eggermont AM, et al. Fine needle aspiration cytology of palpable and nonpalpable lymph nodes to detect metastatic melanoma. J Natl Cancer Inst. 2011;103:1771–7.
Bohelay G, Battistella M, Pagès C, et al. Ultrasound-guided core needle biopsy of superficial lymph nodes: an alternative to fine-needle aspiration cytology for the diagnosis of lymph node metastasis in cutaneous melanoma. Melanoma Res. 2015;25:519–27.
Shirley R, Uppal R, Vadodoria S, et al. Ultrasound-guided wire localisation for surgical excision of deep seated metastatic deposit of malignant melanoma. J Plast Reconstr Aesthet Surg. 2009;62:e411–2.
Voit C, Proebstle TM, Winter H, et al. Presurgical ultrasound-guided anchor-wire marking of soft tissue metastases in stage III melanoma patients. Dermatol Surg. 2001b;27:129–32.
Borgognoni L, Pasciteli L, Gerlini G, et al. Efficacy of electrochemotherapy in the treatment of cutaneous melanoma metastases and rare non-melanoma skin cancer. Anticancer Res. 2020;40:6485–92.
Kunte C, Letulé V, Gehl J, et al. Electrochemotherapy in the treatment of metastatic malignant melanoma: a prospective cohort study by InspECT. Br J Dermatol. 2017;176:1475–85.
Simioni A, Valpione S, Granziera E, et al. Ablation of soft tissue tumours by long needle variable electrode-geometry electrochemotherapy: final report from a single-arm, single-Centre phase-2 study. Sci Rep. 2020;10:2291.
Lassau N, Chami L, Peronneau P. Imaging of melanoma: accuracy of ultrasonography before and after contrast injection for diagnostic and early evaluation of treatments. Bull Cancer. 2007;94:93–8.
Goldmacher GV, Khilnani AD, Andtbacka RHI, et al. Response criteria for intratumoral immunotherapy in solid tumors: itRECIST. J Clin Oncol. 2020;38:2667–76.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Catalano, O. (2022). Ultrasound of Cutaneous Melanoma: Primary Tumor Assessment and Locoregional Staging. In: Wortsman, X. (eds) Textbook of Dermatologic Ultrasound. Springer, Cham. https://doi.org/10.1007/978-3-031-08736-3_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-08736-3_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08735-6
Online ISBN: 978-3-031-08736-3
eBook Packages: MedicineMedicine (R0)