Abstract
Radiology–Pathology correlation is a critical component of the breast imager’s scope of work and has many important functions. Assessing concordance of radiology and pathology results provides an important safety net to prevent false-negative results. It also helps guide future management of the patient who encompasses both radiology and surgical follow-up. Critically, it is the law under the Food and Drug Administration and part of the Mammography Quality Standards Act (MQSA) Medical Outcome Audit. This chapter will reinforce procedural requirements of radiology–pathology correlation, discuss cases of radiology–pathology discordance, identify causes of radiology–pathology discordance, and highlight scenarios surrounding high-risk lesions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radiology–pathology correlation
- Radiology–pathology concordance
- Radiology–pathology
- iscordance
- Radiology–pathology correlation statement
- High-risk breast pathology
- False negative
- Van Nuys classification
- Breast cancer biomarkers
- Echogenic breast masses
-
1.
A 35-year-old woman presented with a palpable mass. The ultrasound-guided biopsy results showed fibroadenoma, which was thought to be concordant with imaging. Six months after the biopsy, the patient reported significant growth of the mass. On ultrasound exam, the mass had doubled in size compared to prior. The patient underwent a localized surgical excision.
At surgical excision, the pathology showed malignant Phyllodes tumor. Which of the following is true regarding radiology–pathology correlation? Radiology–pathology correlation should be performed on the following biopsy cases:
-
(a)
Cases with malignancy pathology.
-
(b)
Cases with benign pathology.
-
(c)
Cases when surgery is recommended.
-
(d)
Cases where the patient will return to screening mammography.
-
(e)
All cases.
-
(a)
-
2.
The radiology–pathology correlation statement that is placed on a benign biopsy should include the following:
-
(a)
A statement of concordance or discordance.
-
(b)
A clear recommendation for follow-up or return to screening.
-
(c)
A BIRADS classification.
-
(d)
a and b.
-
(e)
All of the above.
-
(a)
-
3.
One of the main reasons for performing radiology–pathology correlations is:
-
(a)
To prevent unnecessary surgery.
-
(b)
To decide when to order an MRI.
-
(c)
To limit the number of false negatives.
-
(d)
To increase the true positive rate.
-
(a)
-
4.
Which of the following is (are) true regarding false negatives?
-
(a)
False negative is defined as a test result that wrongly indicates that a patient does not have a disease.
-
(b)
Is a type I error.
-
(c)
Is a type II error.
-
(d)
A and B.
-
(e)
A and C.
-
(a)
-
5.
Which of the following is (are) an example(s) of a false-negative result?
-
(a)
An invasive ductal carcinoma diagnosed in a mass that was previously biopsied two years ago and had yielded a benign result.
-
(b)
An invasive ductal carcinoma diagnosed in the ipsilateral breast 10 months after a benign biopsy.
-
(c)
A benign biopsy that was deemed discordant with imaging and excision was recommended. On excision, the pathology showed invasive carcinoma.
-
(d)
A biopsy result showed ductal carcinoma in situ that underwent surgical excision. On excision, the mass was found to be invasive carcinoma.
-
(e)
All of the above.
-
(a)
-
6a.
A 60-year-old woman with no available prior mammograms was called back from screening mammogram for calcifications in the right lower inner quadrant. Diagnostic images of grouped amorphous calcifications among benign secretory calcifications are submitted below. The diagnostic mammogram was given a BIRADS 4B and a stereotactic biopsy was recommended. The pathology showed atypical ductal hyperplasia.
When performing radiology–pathology correlation for biopsied calcifications, what is required to conclude the pathology result is concordant with imaging findings?

-
(a)
A review of imaging to confirm that the histologic diagnosis explains the imaging findings.
-
(b)
That the specimen radiographs of a stereotactic biopsy specimen contain calcifications from the cluster identified on diagnostic mammogram.
-
(c)
There are post-biopsy changes and a decrease in the number of calcifications in the area of concern on post-procedure mammogram.
-
(d)
All of the above.
-
(a)
-
6b.
The following images are images from the stereotactic biopsy specimen and post-clip placement mammogram. What is your radiology–pathology correlation statement?

-
(a)
Concordant, follow-up mammogram in 6 months.
-
(b)
Concordant, recommend MRI.
-
(c)
Concordant, recommend surgical excision.
-
(d)
Discordant, recommend excision.
-
(a)
-
7.
All the following are examples of high-risk pathology for which surgical excision should be recommended except:
-
(a)
Sclerosing adenosis.
-
(b)
Atypical ductal hyperplasia.
-
(c)
Radial scar with atypia.
-
(d)
Flat epithelial atypia.
-
(e)
Atypical papillary lesion.
-
(a)
-
8.
The biopsy technique that has the highest rate of false negatives is:
-
(a)
Ultrasound core biopsy.
-
(b)
Stereotactic core biopsy.
-
(c)
MRI core biopsy.
-
(d)
Excisional biopsy.
-
(a)
-
9a.
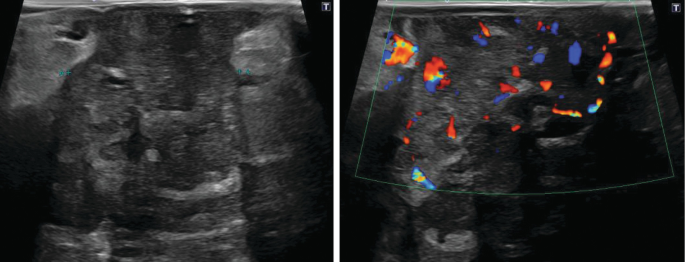
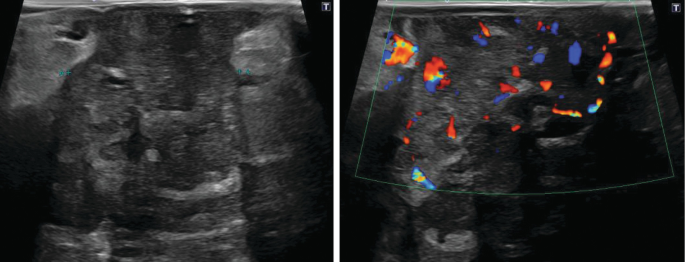
A 35-year-old breast-feeding female presents with breast erythema and tenderness in the peri-areolar region. Her ultrasound is shown below. What is the next best step?

-
(a)
Close follow up (in 6 months).
-
(b)
Mammogram.
-
(c)
Ultrasound-guided biopsy.
-
(d)
Ultrasound-guided drainage and antibiotics.
-
(a)
-
9b.
The most common bacteria causing breast abscess is:
-
(a)
Staphylococcus epidermidis.
-
(b)
Streptococcus pyogenes.
-
(c)
Staphylococcus aureus.
-
(d)
Peptostreptococcus.
-
(e)
Bacteroides.
-
(a)
-
10a.
A 35-year-old, non-breastfeeding woman presents with redness and pain in her right breast. Mammogram and ultrasound imaging is shown below. What is the differential diagnosis for this patient?

-
(a)
Infectious breast abscess.
-
(b)
Idiopathic granulomatous mastitis.
-
(c)
Inflammatory breast cancer.
-
(d)
Diabetic mastitis.
-
(e)
All of the above.
-
(a)
-
10b.
Percutaneous aspiration was attempted, and no fluid could be obtained. A biopsy was performed showing idiopathic granulomatous mastitis. Which of the following are true regarding this pathologic diagnosis?
-
(a)
Most commonly occurs in pre-menopausal women.
-
(b)
The etiology is unknown.
-
(c)
Imaging features can mimic malignancy.
-
(d)
Pathology shows chronic granulomatous inflammation composed of giant cells.
-
(e)
Has a high recurrence rate.
-
(f)
All of the above.
-
(a)
-
11a.
A 55-year-old woman presented with a growing palpable breast mass. Ultrasound images are shown.
Ultrasound core biopsy pathology showed malignant phyllodes tumor. What is your radiology–pathology correlations statement for this lesion?

-
(a)
Concordant— recommend ultrasound in 6 months.
-
(b)
Concordant—recommend excision.
-
(c)
Discordant—recommend excision.
-
(d)
Discordant—recommend MRI.
-
(a)
-
11b.
What is the method of metastasis for phyllodes tumors?
-
(a)
Hematogenous.
-
(b)
Lymphangitic.
-
(c)
Direct extension.
-
(d)
None of the above.
-
(a)
-
11c.
What is the most common location of metastasis of phyllodes tumor?
-
(a)
Axillary lymph nodes.
-
(b)
Bone.
-
(c)
Lungs.
-
(d)
None of the above.
-
(a)
-
11d.
If the pathology was benign phyllodes, what would be your concordance statement?
-
(a)
Concordant—recommend ultrasound in 6 months.
-
(b)
Concordant—recommend excision.
-
(c)
Discordant—recommend excision.
-
(d)
Discordant—recommend MRI.
-
(a)
-
11e.
What imaging characteristics are used to characterize benign from malignant phyllodes tumors?
-
(a)
There are no imaging characteristics that differentiate benign from malignant phyllodes.
-
(b)
Size.
-
(c)
Margins.
-
(d)
Internal cystic spaces.
-
(e)
Interval growth pattern.
-
(a)
-
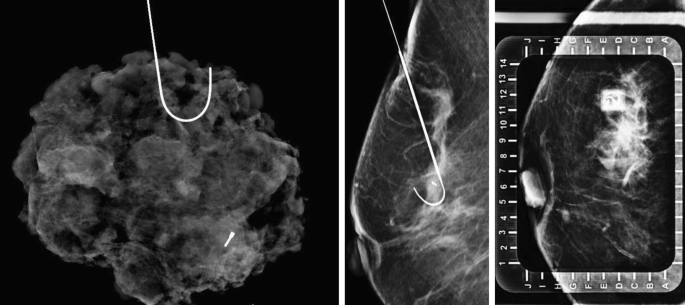
12a.
A 61-year-old woman presents for biopsy of the mammographic findings below. Her pathology returned as ductal carcinoma in situ. What is the most common mammographic finding if this was high-grade DCIS?

-
(a)
Non-calcified mass.
-
(b)
Architectural distortion.
-
(c)
Skin thickening and nipple retraction.
-
(d)
Fine pleomorphic or fine linear-branching calcifications.
-
(a)
-
12b.
What grading system is used to classify DCIS?
-
(a)
TNM classification.
-
(b)
Van Nuys classification.
-
(c)
Luminal Subtype.
-
(d)
Molecular Subtype.
-
(a)
-
12c.
What is the typical MRI enhancement pattern of this lesion?
-
(a)
Enhancing mass.
-
(b)
Focal enhancement in a regional distribution.
-
(c)
No enhancement.
-
(d)
Non-mass enhancement in a segmental distribution.
-
(a)
-
12d.
What are the most important risk factors for disease recurrence in DCIS?
-
(a)
Hormone receptor-positive status.
-
(b)
Post-excision positive margins and synchronous foci that were not excised.
-
(c)
Male gender.
-
(d)
Morphology of the calcifications.
-
(a)
-
13a.
A 20-year-old pregnant patient presents with a new palpable breast mass. Targeted ultrasound images are below. Which of the following is false regarding the evaluation of palpable breast masses in pregnancy?

-
(a)
Benign masses are more common than malignant masses.
-
(b)
Mammogram is contraindicated in pregnancy.
-
(c)
Most pregnancy-related malignancy is invasive ductal cancer.
-
(d)
Masses suspicious for malignancy in pregnant/lactating women should be biopsied despite the risk of milk fistula.
-
(a)
-
13b.
A biopsy of the above mass results in lactational adenoma. What is your radiology–pathology concordance statement for this biopsy?
-
(a)
Concordant—recommend surgical excision.
-
(b)
Concordant—recommend ultrasound follow up in 6 months.
-
(c)
Discordant—recommend MRI.
-
(d)
Discordant—recommend surgical excision.
-
(a)
-
13c.
Which of the following are false regarding lactational adenomas?
-
(a)
Usually presents as a palpable mass.
-
(b)
Ultrasound characteristics are commonly a circumscribed hypoechoic mass.
-
(c)
Can have imaging characteristics of a fibroadenoma.
-
(d)
The presence of interval growth during pregnancy necessitates excision.
-
(a)
-
14a.
A 73-year-old woman was called back for further evaluation from an abnormal screening mammogram. Spot mammogram and ultrasound images are provided below. This mass was biopsied. The pathology results were reported as papilloma with atypia. What is your radiology–pathology correlations statement?

-
(a)
Concordant—recommend surgical excision.
-
(b)
Concordant—recommend 6-month follow-up diagnostic mammogram.
-
(c)
Discordant—recommend MRI.
-
(d)
Discordant—recommend surgical excision.
-
(a)
-
14b.
This biopsied lesion underwent wire localization and excision. The excisional biopsy upstaged the pathology to 4 mm low-grade ductal carcinoma in situ, papillary and micropapillary types. No invasive component was identified. All margins were negative. Based on these pathology results, what TNM stage is the patient?
-
(a)
Stage 0.
-
(b)
Stage 1A.
-
(c)
Stage 2A.
-
(d)
Unable to determine.
-
(a)
-
15a.
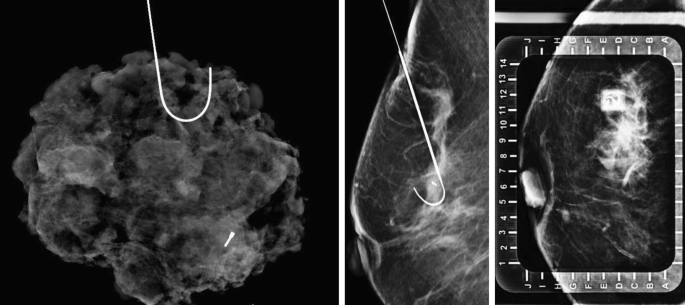
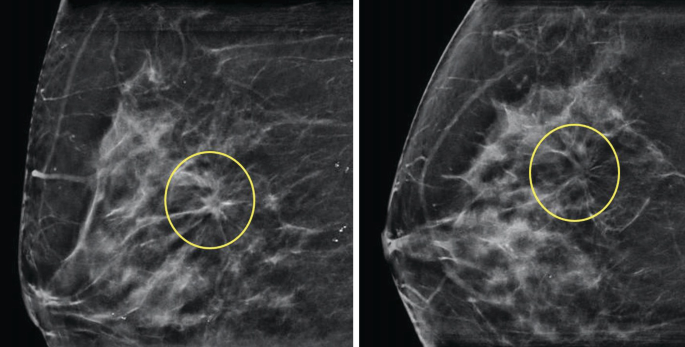
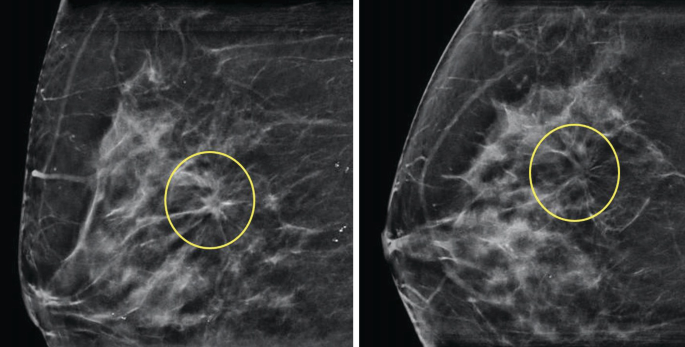
A 59-year-old woman called back for a screening mammogram for architectural distortion in the right breast. MLO and CC tomosynthetic 2D images are below respectively.

No sonographic correlation was identified. BIRADS 4 was given to the diagnostic workup, and a stereotactic core needle biopsy was performed. No specimen radiograph was obtained. Post-procedure mammograms are submitted below.

Pathology results showed focal microcalcifications in association with benign ducts. The radiology–pathology correlation for this biopsy is:
-
(a)
Concordant—recommend mammogram in 6 months.
-
(b)
Concordant—recommend mammogram and ultrasound in 6 months.
-
(c)
Discordant—recommend MRI.
-
(d)
Discordant—recommend surgical excision.
-
(a)
-
15b.
An excisional biopsy was performed showing invasive ductal carcinoma with lobular features. All of the following may explain architectural distortion on mammogram and be considered concordant except?
-
(a)
Radial scar.
-
(b)
Lobular carcinoma.
-
(c)
Post-surgical scar.
-
(d)
Ductal Carcinoma In situ.
-
(e)
Papilloma.
-
(a)
-
16a.
A 73-year-old woman was called back from screening mammogram for a new mass in the right breast. Diagnostic mammogram images and ultrasound are provided below. The below diagnostic workup was given a BIRADS 5—Highly suspicious and the mass underwent core needle biopsy. Pathology reported invasive lobular carcinoma. Of the mammographic findings below, what is the most common conventional mammographic finding of this pathology?

-
(a)
Irregular mass.
-
(b)
Pleomorphic calcifications.
-
(c)
Course, heterogeneous calcifications.
-
(d)
Circumscribed mass.
-
(a)
-
16b.
What is the most common ultrasound finding of invasive lobular carcinoma?
-
(a)
Dermal thickening with an ill-defined heterogeneous echogenicity.
-
(b)
An anechoic cystic mass with a vascular papillary projection from its wall.
-
(c)
An irregular mass with angular margins, hypoechoic, heterogeneous internal echoes, and posterior acoustic shadowing.
-
(d)
A circumscribed, isoechoic mass with no posterior acoustic features.
-
(a)
-
16c.
What is the next best step?
-
(a)
Lumpectomy with sentinel node biopsy.
-
(b)
MRI.
-
(c)
Neoadjuvant therapy.
-
(a)
-
17.
Which of the following description and associated BIRADS has the highest likelihood of a discordant pathology?
-
(a)
A stereotactic biopsy of heterogeneous calcifications (BIRADS 4) with pathology result of fibroadenoma.
-
(b)
An MRI biopsy of non-mass enhancement (BIRADS 4) with pathology result of DCIS.
-
(c)
An ultrasound mass with angulated margins (BIRADS 5) with pathology result of fibroadenoma.
-
(d)
A circumscribed mass on ultrasound (BIRADS 4) with pathology result of medullary carcinoma.
-
(a)
-
18.
Which of the following biomarkers are not routinely tested for on breast cancer biopsy specimens and excision specimens?
-
(a)
ER.
-
(b)
PR.
-
(c)
HER2.
-
(d)
PD-L1.
-
(e)
Ki-67 antigen.
-
(a)
-
19.
A 45-year-old woman with BRCA1 mutation underwent screening and diagnostic mammogram and screening breast MRI with images shown below. Because of the abnormalities, a stereotactic biopsy was performed. Based on the imaging findings, what is the most likely grade of her cancer?

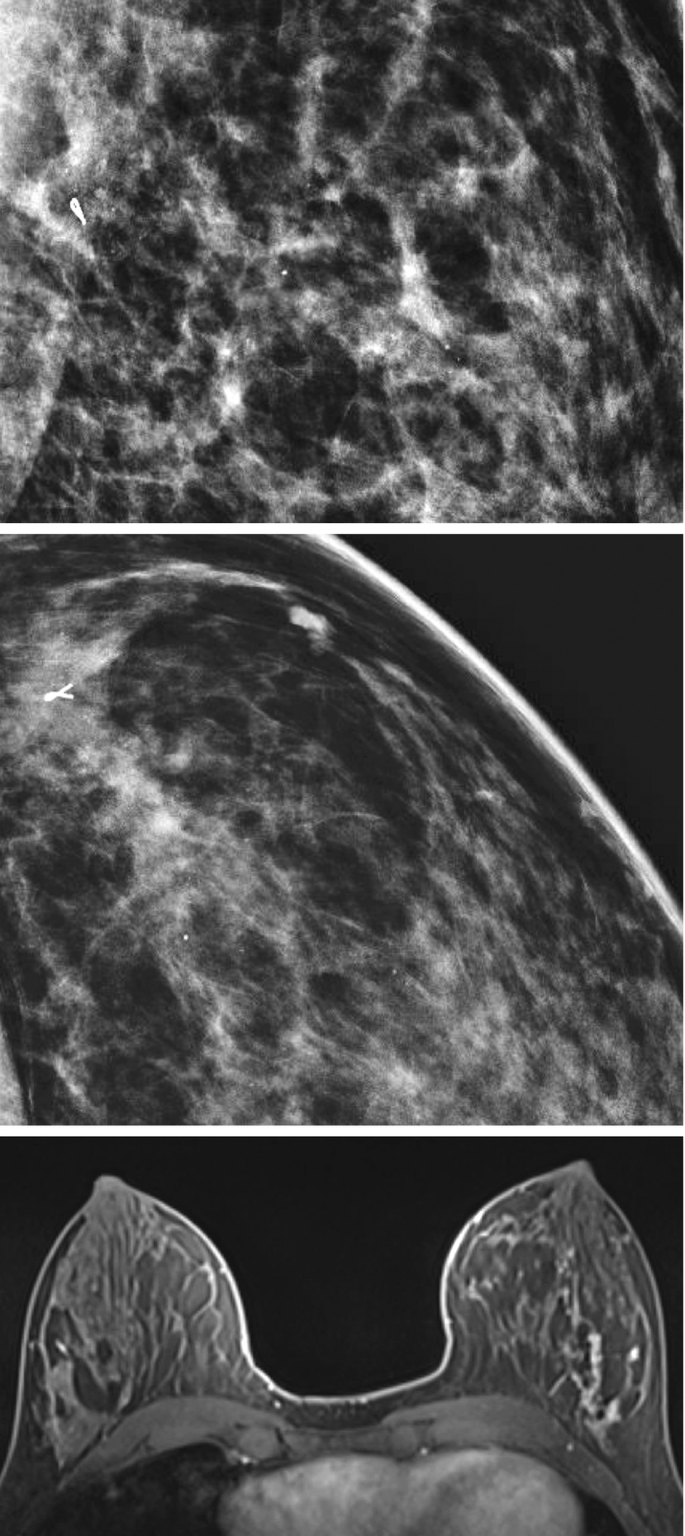
-
(a)
Low grade.
-
(b)
Intermediate grade.
-
(c)
High grade.
-
(d)
Benign findings.
-
(a)
-
20.
In BRCA 1 and BRCA 2 mutation carriers, what is the lifetime risk of developing breast cancer?
-
(a)
20%.
-
(b)
50%.
-
(c)
85%.
-
(d)
99%.
-
(a)
-
21a.
A 34-year-old female presenting with a new right breast palpable mass. Targeted ultrasound image is below:
What proportion of malignant lesions are isoechoic on ultrasound?

-
(a)
1/8.
-
(b)
3/4.
-
(c)
1/2.
-
(d)
1/3.
-
(a)
-
21b.
The echogenicity of a lesion on ultrasound is determined relative to what structure in the breast?
-
(a)
Fat.
-
(b)
Fibroglandular tissue.
-
(c)
Surrounding tissue.
-
(d)
Muscle.
-
(a)
-
21c.
If a mass in the patient’s fatty breast tissue was depicted on mammography but not detected on ultrasound, what is the next best step to assist in ultrasound visualization
-
(a)
Contrast-enhanced mammography.
-
(b)
MRI.
-
(c)
Tissue harmonic imaging.
-
(d)
Widen the dynamic range on ultrasound.
-
(a)
-
22a.
A 58-year-old woman who was called back from an abnormal screening mammogram. Diagnostic mammogram and ultrasound images are provided below. Which of the following pathologies can present as a circumscribed mass on imaging?

-
(a)
Mucinous carcinoma.
-
(b)
Medullary carcinoma.
-
(c)
Papillary carcinoma.
-
(d)
Invasive ductal carcinoma not otherwise specified.
-
(e)
All of the above.
-
(a)
-
22b.
The circumscribed mass above was biopsied and showed a circumscribed carcinoma composed of poorly differentiated cells. If the tumor were to show rapid growth over time, which subtype of circumscribed ductal carcinomas would this most likely be?
-
(a)
Mucinous carcinoma.
-
(b)
Medullary carcinoma.
-
(c)
Papillary carcinoma.
-
(d)
Invasive ductal carcinoma not otherwise specified.
-
(e)
None of the above.
-
(a)
-
23a.
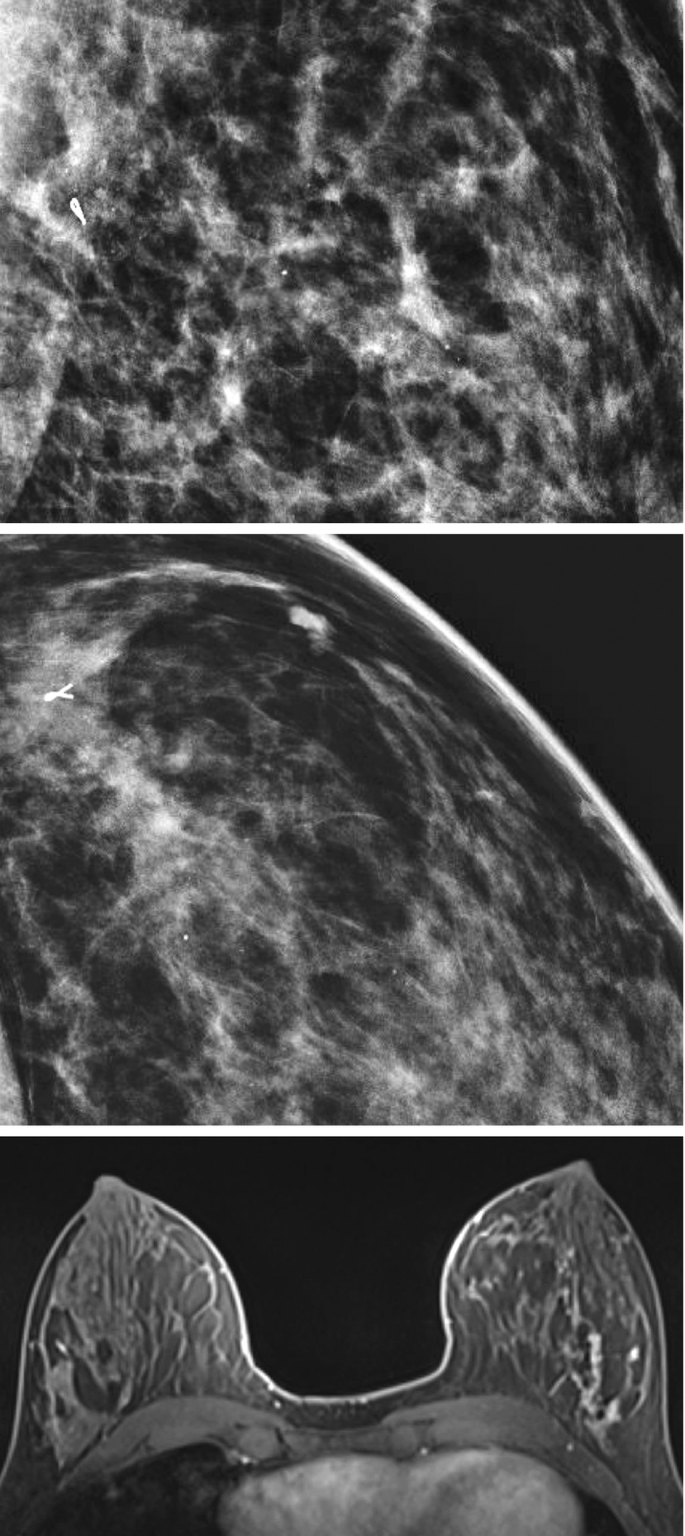
A 45-year-old female presents for screening mammography shown below, which showed a rapidly growing focal asymmetry in the right breast upper outer quadrant.

Additional magnification views and ultrasound were performed, as shown below.

Which of the following is false regarding hyperechoic breast masses?
-
(a)
An echogenic breast mass that is radiolucent on mammography is benign and does not need biopsy.
-
(b)
Most hyperechoic breast masses are benign.
-
(c)
Hyperechogenicity on ultrasound alone is enough to exclude malignancy.
-
(d)
The differential for hyperechoic breast masses includes benign and malignant etiologies.
-
(e)
None of the above.
-
(a)
-
23b.
Which of the following benign lesions can be hyperechogenic at ultrasound?
-
(a)
Lipoma.
-
(b)
Hematoma.
-
(c)
Silicone granuloma.
-
(d)
Galactocele.
-
(e)
Fat necrosis.
-
(f)
All of the above.
-
(a)
-
23c.
Based on the images above, what is the most likely diagnosis
-
(a)
PASH.
-
(b)
Phyllodes tumor.
-
(c)
Hamartoma.
-
(d)
Fibroadenoma.
-
(a)
-
23d.
The patient underwent biopsy of the lesion, which demonstrated PASH. When performing your radiology-pathology correlation, in which situations would surgical excision be recommended?
-
(a)
All cases of PASH should be excised.
-
(b)
PASH with atypia.
-
(c)
Rapidly growing in size.
-
(d)
Size greater than 5 cm.
-
(e)
B and C.
Answers
-
1.
e. All cases.
Radiology–Pathology correlation is required in all cases of percutaneous biopsy performed by a radiologist regardless of pathology or treatment plan. Determining concordance between imaging findings and histologic results is important because it guides the treatment plan, including the need to recommend surgical excision or short-term follow-up [1].
-
2.
d (A and B).
Radiology–pathology statement is included in the percutaneous biopsy report performed by the radiologist. In this statement, both concordance and a follow-up recommendation are required. A BIRADS assessment is not part of the radiology–pathology correlation statement [2].
-
3.
c. To limit the number of false negatives.
There are multiple reasons to perform radiology-pathology correlation, including regulatory compliance and data gathering for practice parameters. One of the main reasons to perform radiology-pathology correlation is limiting the number of false-negative biopsy results. A false negative result as defined by the National Cancer Institute is a test result that indicates a person does not have a specific disease or condition when the person does have the disease or condition. An example of this would be a benign biopsy result when the patient has cancer [3].
-
4.
e (A and C).
A false-negative test in interventional breast radiology is a breast biopsy that is initially histologically determined to be benign and later proven to be carcinoma at the same site. Type II error is a statistical term used to describe the acceptance of a null hypothesis that is in reality true. A type II error produces a false negative [3].
-
5.
b. An invasive ductal carcinoma diagnosed in the ipsilateral breast 10 months after a benign biopsy.
A False-Negative (FN) is tissue diagnosis of cancer within 1 year of a negative or benign examination. A false negative does not include cases with discordant or underestimation of disease if excisional biopsy is performed and cancer is identified without significant delay in diagnosis [4].
-
6a.
d. All of the above.
Radiology–Pathology correlation of calcifications requires all of the above [3].
-
6b.
c. Concordant, recommend surgical excision.

Atypical ductal hyperplasia (ADH) is a high-risk lesion, meaning it can underestimate the associated presence of underlying cancer. Up to 44% of ADH lesions diagnosed with a 14-gauge stereotactic biopsy turned out to be cancer on excisional biopsy [3]. Of the upgraded cases, 25% are associated with invasive carcinomas, and the remaining 75% are any grade DCIS [3]. In the above case, pathology was upgraded to DCIS upon surgical excision.
-
7.
a. Sclerosing adenosis.
High-risk lesions are pathologic diagnoses on core needle biopsy that are not malignant but can underestimate the presence of an associated cancer. They occur in approximately 10% of percutaneous biopsies and may require surgical excision [3]. For atypical ductal hyperplasia (ADH), a meta-analysis showed a pooled upgrade rate higher than 2%, and therefore excision is often recommended and pursued [5]. Although the management recommendations for radial scar and papillary lesions can be complex, the presence of atypia in the pathology specimen warrants excision [3].
-
8.
b. Stereotactic core biopsy.
One of the most important measures of biopsy accuracy is the false-negative rate. The literature reports a 4.0–22.2% false-negative rate for stereotactic core-needle biopsy using a 14-gauge needle vs. 0–3.3% for an 11-gauge needle [6]. Therefore, in stereotactic biopsies, it may be helpful to use an 11-guage needle or larger with vacuum assist [6]. MRI biopsy false negative rates have been reported as 0.6–2.4% [7, 8]. Ultrasound core biopsy false-negative rate is 2.4% [9]. Excisional biopsy has a 2.0% false-negative rate [6].
-
9a.
d. Ultrasound-guided drainage and antibiotics.
In a 35-year-old female patient who is lactating and has ultrasound findings typical for a breast abscess, it is appropriate to perform percutaneous drainage and treat with antibiotics.
There are many advantages to ultrasound-guided intervention:
-
Performed rapidly with local anesthesia in the ambulatory setting.
-
Lower rates of milk fistula.
-
No need to interrupt lactation.
-
Percutaneous drainage results in minimal to no scarring. US-guided drainage has a complication rate similar to or lower than surgical incision and drainage [10].
-
-
9b.
Staphylococcus aureus.
Most abscesses occur due to secondary bacterial infection from skin contamination. The most common pathogen by far is Staphylococcus aureus. Other bacterial causes include S. pyogenes, S. epidermidis, Peptostreptococcus, and Bacteroides. Less commonly, breast abscesses can occur from fungi, parasites, and mycobacterium including Tuberculosis, especially in certain geographic settings and patient populations. When you aspirate the collection, the fluid should be sent for gram stain and culture [10].
-
10a.
e. All of the above.
Common symptoms of breast infection include pain, redness, and warmth. However, it is important to consider the many causes of breast pain and erythema with these imaging findings, especially in non-lactating and older women. The differential includes breast abscess, inflammatory carcinoma, and noninfectious inflammatory processes including diabetic mastopathy, chronic idiopathic granulomatous mastitis, and immunologic diseases such as Churg-Strauss syndrome, amyloidosis, Wegener granulomatosis, and sarcoidosis [10].
-
10b.
f. All of the above.
Granulomatous mastitis is a rare disease that occurs in parous, pre-menopausal women with a history of lactation and is often associated with hyperprolactinemia. The exact etiology is unknown, but it has been postulated to stem from a local inflammatory response in connective tissue and has been shown to be associated with multiple factors, with established connections to pregnancy, lactation, and hyperprolactinemia. The most common presentation is a tender, palpable mass, with imaging features often mimicking malignancy thus biopsy is frequently performed. On ultrasound, findings include irregular masses, focal regions of inhomogeneity with hypoechoic or tubular/nodular structures, or parenchymal hypoechogenicity with posterior acoustic shadowing. Mammographic findings usually show a focal or global asymmetry, ill-defined breast masses, or negative findings; calcifications are rarely seen. Pathology shows noncaseating granulomatous inflammation centered in the lobules, with associated giant cells, leukocytes, macrophages, abscesses, and epithelioid cells. Infection, including mycobacterial and fungal pathogens, should be excluded. Treatment is controversial and varies by institution, ranging from surveillance in mild cases to oral steroid therapy, methotrexate or bromocriptine, and even surgery which is typically reserved for refractory or recurrent disease. Up to 50% of cases will recur, which can be reduced by immunosuppressive treatment until complete remission [3, 11].
-
11a.
b. Concordant—recommendation excision.
Phyllodes tumor classically presents as a rapidly enlarging mass in a woman in her fifth decade. It is a high-risk breast lesion and wide surgical excision is the preferred treatment. Incomplete excision of either a benign or malignant phyllodes tumor can result in local recurrence 15% of the time. Approximately 25% of phyllodes tumors are malignant [3].
-
11b.
a. Hematogenous.
Metastatic disease is common in phyllodes tumors. Metastatic disease has been reported in 13–40% of patients with phyllodes tumors. Unlike most other breast cancers, the method of spread is hematogenous [3].
-
11c.
c. Lungs.
The most common location for metastasis to occur from phyllodes tumor is the lungs [12, 13].
-
11d.
b. Concordant—recommend excision.
Phyllodes tumors of the breast account for 0.3%–1% of all primary breast tumors and constitute 2.5% of fibroepithelial tumors [3]. Phyllodes tumors are graded according to recommendations by the World Health Organization as benign, borderline, or malignant based on the presence of stromal cellularity, atypia, mitotic activity, and stomal overgrowth [14]. Surgical excision is required for all types of phyllodes tumors [3].
-
11e.
a. There are no imaging characteristics that differentiate benign from malignant phyllodes.
-
12a.
d. Fine pleomorphic or fine linear-branching calcifications.
Microcalcifications are found in 50–75% of DCIS [15]. Low-grade DCIS lesions are more likely than high-grade lesions to demonstrate non-calcified abnormalities on mammography, including asymmetry and mass. Fine pleomorphic or fine linear-branching calcifications have been noted in high-grade DCIS according to the WHO system of classification [15].
-
12b.
b. Van Nuys classification.
The Van Nuys classification system is the simplest and most reproducible classification system for classifying DCIS. It identifies three groups of DCIS lesions, differentiated first according to nuclear grade (low, intermediate, or high grade) and then with presence or absence of necrosis [15].
-
12c.
d. Non-mass enhancement in a segmental distribution.
Non-mass enhancement is the most common MRI finding of DCIS and is seen in 60–80% of cases [15]. A segmental distribution of this non-mass enhancement is the most common pattern and accounts for 33–77% of cases of DCIS [15]. Ductal, linear or regional distribution of non-mass enhancement are other commonly reported MRI findings. An enhancing mass is seen in 14–34% of cases and focal enhancement is seen in 1–12% [16].
-
12d.
b. Post-excision positive margins and synchronous foci that were not excised.
In DCIS, the most important risk factors for disease recurrence are post excision positive margins and synchronous foci that were not removed. In the National Surgical Adjuvant Breast Project, B-06 protocol, patients treated with excision followed by radiation therapy had a 6.9% recurrence, whereas those who did not undergo radiation therapy had a 22.7% rate of recurrence [16]. Gender and hormone receptor-positive status are not risk factors for disease recurrence. Adjuvant endocrine therapy has been shown to decrease the rate of recurrence by up to 50% in ER-positive tumors [17].
-
13a.
b. Mammogram is contraindicated in pregnancy.
Most masses that occur in pregnancy are benign and include benign lactational adenoma, fibroadenoma, galactocele, and abscess [3]. According to ACR appropriateness criteria, while ultrasound is the first indicated examination for pregnant and lactating women with palpable concerns, mammography is not contraindicated in pregnancy and the dose to the fetus is negligible (4-view mammogram is <0.03 mGy) [18]. NCCN guidelines state that mammogram with shielding can be done safely in pregnant women [18]. As always, discussion of risk and benefit should be performed with the patient prior to proceeding with mammogram. Also, lactation is not a contraindication for mammogram. Mammography in a diagnostic workup is important to identify findings of breast cancer such as microcalcifications. Milk fistula is an uncommon condition that occurs when there is an abnormal connection that forms between the skin surface and the duct in the breast of a lactating woman. This is more commonly associated with surgical intervention than percutaneous biopsy but can occur [19, 20]. However, 3% of breast cancers are coincident with pregnancy or lactation [3]. Therefore, if suspicious image findings are identified, a biopsy should be performed.
-
13b.
b. Concordant—recommend ultrasound follow up in 6 months.
Benign concordant lesions can be false-negative. For this reason, meticulous radiology-pathology concordance must occur by the radiologist performing the biopsy, with confirmation of appropriate sampling, correlation with clinical symptoms and breast cancer risk, and lesion radiologic features prior to biopsy with correlating pathologic results [3]. Recent studies have indicated routine screening is appropriate if the biopsy is benign and concordant [21]. Imaging follow-up can be performed at the discretion of the radiologist on the same imaging modality that guided the biopsy. This may occur more frequently in younger patients who would not be expected to have routine breast imaging if <40 years or if not on a high-risk screening schedule. If the lesion increases in size at follow-up, repeat biopsy or surgical excision can be considered [21].
-
13c.
d. The presence of interval growth during pregnancy necessitates excision.
Lactating adenoma is a solid, benign tumor diagnosed during pregnancy. It typically presents as a firm, painless palpable lump late in pregnancy or during lactation. On ultrasound, it has some similarities to fibroadenoma and appears as a well-circumscribed, hypoechoic mass that may contain echogenic bands (which are fibrotic bands seen on pathology). Interval growth is common and may represent change stimulated by hormonal alterations [3].
-
14a.
a. Concordant—recommend surgical excision.
The management of papilloma found on biopsy is controversial. In contrast to central papillomas, papillomas in the periphery of the breast are associated with epithelial proliferation, which can have atypical features. Atypia is thought to increase the risk of malignancy [3]. Papillary lesions without atypia have recently been shown in a prospective study to have an upgrade rate of just 1.7%, below the 2% threshold for probably benign findings and therefore if concordant imaging findings, may be considered safe to follow [22]. It is generally agreed that any papillary lesion with atypia, regardless of location, should undergo excision.
-
14b.
a. Stage 0.
Anatomic stage is based on the extent of cancer using T (extent of tumor), N (nodal disease), and M (distant metastasis) categories. When the primary tumor does not invade the basement membrane and only ductal carcinoma in situ is found, it is stage 0, or Tis, N0M0 [23].
-
15a.
d. Discordant—recommend surgical excision.
Architectural distortion is defined as distortion of the normal breast parenchyma architecture with no definite mass. It can be seen in both benign and malignant entities [3]. Architectural distortion has a high positive predictive value for malignancy in both screening and diagnostic 2D mammography, 10–67% and 60–83%, respectively [24]. The pathology of benign ducts does not explain the mammographic findings. Therefore, the radiology–pathology is discordant, and excision should be recommended secondary to the high positive predictive value of architectural distortion [24].
-
15b.
e. Papilloma.
Architectural distortion can be caused by invasive carcinoma, DCIS, radial scar, sclerosing adenosis, post-surgical scar, and post-radiation change. On mammography, papilloma can demonstrate a markedly dilated duct extending into the breast from the nipple with or without an associated mass. Ultrasound usually shows a solid mass within fluid-filled, dilated ducts. Solitary architectural distortion is not associated with papilloma [3].
-
16a.
a. Irregular mass.
Invasive lobular carcinoma (ILC) most commonly manifests as a mass with spiculated or indistinct margins on mammography (44–65%) [25]. Much less commonly, these cancers will present as round or circumscribed masses (1–3%) [25]. Architectural distortion is the second most common manifestation of invasive lobular carcinoma (10–34%) [25]. Reported microcalcifications associated with invasive lobular carcinoma vary (0–24%), however, is known to be less than with invasive ductal carcinoma [25].
-
16b.
c. An irregular mass with angular margins, hypoechoic, heterogenous internal echoes, and posterior acoustic shadowing.
Ultrasound is superior to mammography in identifying multicentric and multifocal diseases. The most common ultrasound manifestation of invasive lobular carcinoma is an irregular mass with indistinct, angular or spiculated margins, hypoechoic and heterogeneous internal echoes, and posterior acoustic shadowing. Other less common findings include circumscribed masses, focal shadowing without a discrete mass, and sonographically occultlesions [25].
-
16c.
b. MRI.
MRI should be performed in biopsy proven invasive-lobular carcinoma because it has been found to affect clinical management in 50% of cases, leading to changes in surgical management in 28% [25]. MRI is able to detect additional ipsilateral disease in 32% of cases and contralateral disease in 7% of cases that were not detected on mammography or ultrasonography [25].
-
17.
c. An ultrasound mass with angulated margins (BIRADS 5) with pathology result of fibroadenoma.
Ultrasound findings suggestive of cancer include an irregular shape, non-circumscribed margins (angular, indistinct, microlobulated, and spiculated), thick echogenic rim or halo, duct extension, or surrounding tissue changes, microcalcifications (in or out of a mass or intraductal), non-parallel orientation, or posterior shadowing. These descriptors are included in the ACR BI-RADS ultrasound lexicon. A fibroadenoma should have circumscribed margins without suspicious features [3].
-
18.
d. PD-L1.
ER, PR, HER2, and Ki-67 antigen are biomarkers that are tested consistently in invasive breast carcinoma due to their potential effect on prognosis and clinical management [17].
-
19.
c. High grade.
Linear enhancement is seen on MRI and calcifications on mammography most often correspond to high-grade carcinoma [26].
-
20.
c. 85%.
The lifetime breast cancer risk is as high as 85% for BRCA1 and BRCA2 mutation carriers. They also have a 50% risk of developing breast cancer by the age of 50 years [26].
-
21a.
d. 1/3.
Isoechogenicity is not classified as a suspicious finding for malignancy but is considered an indeterminate finding. It can be seen in both benign and malignant lesions. About one-third of breast carcinomas are isoechoic on ultrasound. Isoechogenicity can also be seen in usual ductal hyperplasia, atypical ductal hyperplasia, papillary apocrine metaplasia, adenosis, debris/cellularity in fibrocystic and benign proliferative conditions, fibroadenoma, and papilloma. In the above patient, ultrasound-guided core biopsy confirmed fibroadenoma, benign, and concordant [27].
-
21b.
a. Fat.
The echogenicity of a mass is assessed by its relationship to the echogenicity of fat in the breast [27].
-
21c.
c. Tissue harmonic imaging.
When a lesion is seen on mammogram in the fatty tissues but not identified on standard ultrasound, it is likely an isoechoic lesion. Tissue harmonic imaging uses nonlinear sound propagation that allows the processing of only the returned high-frequency harmonic signals and rejects echoes from fundamental frequencies. This technique improves lesion conspicuity on ultrasound by increasing tissue contrast and lateral resolution. Widening the dynamic range on ultrasound is not the next best step because a wide range allows isoechoic lesions to persist and remain undetectable. Contrast-enhanced mammography and MRI may be helpful but are not the next best step in evaluation [27]. Shown here is an example of the same finding with and without harmonics.

-
22a.
e. All of the above.
The well-differentiated invasive ductal carcinomas including mucinous, medullary, and papillary, can have a relatively circumscribed appearance on imaging. Invasive ductal carcinoma not otherwise specified can also present as a circumscribed mass, but typically has a poorer prognosis. Other circumscribed cancers of the breast include triple-negative breast cancer adenoid cystic carcinoma and malignant phyllodes tumor [28].
-
22b.
b. Medullary carcinoma.
Medullary carcinoma accounts for less than 2% of breast cancers [28]. It occurs more frequently in younger women and is characterized by rapid growth, often manifesting clinically with a palpable mass. The other lesions described above grow slowly in comparison to medullary carcinoma [28].
-
23a.
c. Hyperechogenicity on ultrasound alone is enough to exclude malignancy.
Echogenic breast masses are defined as a lesion that is hyperechoic in comparison with subcutaneous fat at ultrasound, in accordance with the BI-RADS ultrasound lexicon. On ultrasound, up to 5.6% of breast masses are reported to be echogenic of which most are benign [29]. Both benign and malignant etiologies can be echogenic. If a hyperechoic mass correlates with a well-delineated radiolucent mass at mammography, it does not need biopsy. One large study found that of 1849 lesions that were malignant, 9 (0.5%) were hyperechoic [30]. Therefore, although the vast majority of echogenic breast masses are benign, hyperechogenicity at US alone does not exclude malignancy [29].
-
23b.
f. All of the above.
The differential for hyperechoic breast masses is extensive.
Benign lesions that can be hyperechoic include:
Lipoma, angiolipoma, hematoma, seroma, fat necrosis, silicone granuloma, sebaceous or epidermal inclusion cyst, abscess, pseudoangiomatous stromal hyperplasia (PASH), galactocele or lactating adenoma, ductal ectasia, and apocrine metaplasia [29].
Malignant lesions that can be hyperechoic on ultrasound include:
Invasive ductal carcinoma, invasive lobular carcinoma, metastasis, lymphoma, and angiosarcoma [29].
-
23c.
a. PASH.
Pseudoangiomatous stromal hyperplasia (PASH) is a benign breast mass of unknown etiology. It usually presents in pre-menopausal women or post-menopausal women on hormone therapy, and can rapidly grow in size. On ultrasound, it appears as a mixed or hypoechoic mass with ill-defined borders but can also be hyperechoic. Mammography will demonstrate an oval mass, sometimes with well-circumscribed borders [3].
-
23d.
e. B and C.
A histological diagnosis of pseudoangiomatous stromal hyperplasia (PASH) is considered safe to manage conservatively with imaging follow-up. Because low-grade angiosarcoma can mimic PASH on biopsy, surgical excision is recommended in PASH with atypia and in cases of PASH with interval growth [3].
-
(a)
References
Ho CP, et al. Interactive case review of radiologic and pathologic findings from breast biopsy: are they concordant? How do I manage the results? Radiographics. 2013;33(4):E149–52.
Bassett LW, Mahoney MC, Apple SK. Interventional breast imaging: current procedures and assessing for concordance with pathology. Radiol Clin N Am. 2007;45:881–94.
Ikeda DM. Breast imaging: the requisites. 2nd ed. ELSEVIER MOSBY; 2004.
D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA, et al. ACR BI-RADS® atlas, breast imaging reporting and data system. 5th ed. American College of Radiology; 2013.
Schiaffino S, et al. Upgrade rate of percutaneously diagnosed pure atypical ductal hyperplasia: systematic review and meta-analysis of 6458 lesions. Radiology. 2020;294(1):76–86.
Jackman RJ, Marzoni FA, Rosenberg J. False-negative diagnoses at stereotactic vacuum-assisted needle breast biopsy: long-term follow-up of 1,280 lesions and review of the literature. Am J Roentgenol. 2009;192(2):341–51.
Hayward JH, Ray KM, Wisner DJ, Joe BN. Follow-up outcomes after benign concordant MRI-guided breast biopsy. Clin Imaging. 2016;40(5):1034–9.
Huang ML, Speer M, Dogan BE, Rauch GM, Candelaria RP, Adrada BE, Hess KR, Yang WT. Imaging-concordant benign MRI-guided vacuum-assisted breast biopsy may not warrant MRI follow-up. Am J Roentgenol. 2017;208(4):916–22.
Hyun Youk J, Kim EK, Kim MJ, Oh KK. Sonographically guided 14-gauge Core needle biopsy of breast masses: a review of 2,420 cases with long-term follow-up. Am J Roentgenol. 2008;190(1):202–7.
Trop I, et al. Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up. Radiographics. 2011;31:1683–99.
Pluguez-Turull CW, Nanyes JE, Quintero CJ, Alizai H, Mais DD, Kist KA, Dornbluth NC. Idiopathic granulomatous mastitis: manifestations at multimodality imaging and pitfalls. Radiographics. 2018;38(2):330–56.
Chaney AW, et al. Primary treatment of cystosarcoma phyllodes of the breast. Cancer. 2000;89(7):1502.
Barrio AV, et al. Clincopathologic features and long-term outcomes of 293 phyllodes tumors of the breast. Ann Surg Oncol. 2007;14:2961.
Tan PH, et al. Fibroepithelial tumors: WHO classification of tumors of the breast. Int Agency Res Cancer. 2012;4:414–147.
Yamada, et al. Radiologic-pathologic correlation of ductal carcinoma in situ. Radiographics. 2010;30:1183–98.
Mossa-Basha M, et al. Ductal carcinoma in situ of the breast: MR imaging findings with histopathologic correlation. Radiographics. 2010;30:1673–87.
Tirada N, et al. Breast cancer tissue markers, genomic profiling, and other prognostic factors: a primer for radiologists. Radiographics. 2018;38:1902–20.
diFlorio-Alexander RM, Slanetz PJ, Moy L, Baron P, Didwania AD, Heller SL, Holbrook AI, Lewin AA, Lourenco AP, Mehta TS, Niell BL, Stuckey AR, Tuscano DS, Vincoff NS, Weinstein SP, Newell MS. ACR appropriateness criteria® breast imaging of pregnant and lactating women. J Am Coll Radiol. 2018;15(11S):S263–75.
Schackmuth EM, Harlow CL, Norton LW. Milk fistula: a complication after core breast biopsy. Am J Roentgenol. 1993;161(5):961–2.
Larson KE, Valente SA. Milk fistula: diagnosis, prevention, and treatment. Breast J. 2015;22(1):111–2.
Monticciolo DL, Hajdik RL, Hicks MG, Winford JK, Larkin WR, Vasek JV Jr, Ashton BM. Six-month short-interval imaging follow-up for benign concordant Core needle biopsy of the breast: outcomes in 1444 cases with long-term follow-up. Am J Roentgenol. 2016;207(4):912–7.
Nakhlis F, Baker GM, Pilewskie M, et al. The incidence of adjacent synchronous invasive carcinoma and/or ductal carcinoma in situ in patients with intraductal papilloma without atypia on Core biopsy: results from a prospective multi-institutional registry (TBCRC 034). Ann Surg Oncol. 2021;28(5):2573–8.
Kalli S, et al. American joint committee on Cancer’s staging system for breast cancer, eighth edition: what the radiologist needs to know. Radiographics. 2018;38(7):1921–33.
Alshafeiy TI, et al. Outcome of architectural distortion detected only at breast tomosynthesis versus 2D mammography. Radiology. 2018;288(1):38–46.
Lopez JK, Bassett LW. Invasive lobular carcinoma of the breast: Spectrum of mammographic, US, and MR imaging findings. Radiographics. 2009;29:165–76.
Causer PA, et al. Breast cancers detected with imaging screening in the BRCA population: emphasis on MR imaging with histopathologic correlation. Radiographics. 2007;27:S165–82.
Kim MJ, et al. How to find an isoechoic lesion with breast US. Radiographics. 2011;31:663–76.
Harvey JA. Unusual breast cancers: useful clues to expanding the differential diagnosis. Radiology. 2007;242:683–94.
Gao Y, Slanetz PJ, Eisenberg RL. Echogenic breast masses at US: to biopsy or not to biopsy? Radiographics. 2013;33:419–34.
Linda A, Zuiani C, Lorenzon M, et al. Hyperechoic lesions of the breast: not always benign. Am J Roentgenol. 2011;196(5):1219–24.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chung, S.H., Cain, N., Roth, A. (2022). Pathology. In: Chow, L., Li, B. (eds) Absolute Breast Imaging Review. Springer, Cham. https://doi.org/10.1007/978-3-031-08274-0_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-08274-0_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08273-3
Online ISBN: 978-3-031-08274-0
eBook Packages: MedicineMedicine (R0)