Abstract
The data used by care teams managing high-risk, high-complexity procedural interventions are discussed. These teams use continuous surveillance of such data to achieve optimal outcomes. Examples of how selection risk is managed are highlighted. These concern patients with end-stage heart failure, severe pulmonary embolism, critical neurological injury, and solid organ transplantation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Although many factors influence the clinical outcomes of medical and procedural interventions, appropriate patient selection is probably the most important. Assessment and recognition of appropriate candidates for an intervention constitute a large part of procedural training.
This is especially important in procedural care as the mere performance of a procedure frequently influences expected outcomes in risk models. For example, the performance of percutaneous coronary intervention reduces expected mortality in risk models used by data-sharing organizations such as Vizient. It stands to reason that a mortality following such a procedure carries an even greater impact on overall risk-adjusted mortality for the population of patients subjected to the procedural intervention.
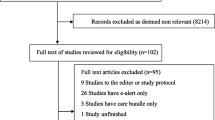
1 What Indicators Exist to Alert Medical Teams of the Need to Manage Selection Risk?
Not much is written in the literature about the management of selection risk. Transplant programs follow the success of transplant interventions by means of a CUSUM (cumulative sum) analysis, which is very sensitive to small changes over time. If a substantial movement in an adverse direction is observed, programs may pause to investigate where improvements can be made. In addition, they may reevaluate entry criteria and take less risk until the outcome trends improve. This process allows selection committees to err on the conservative side of patient selection to assure that benefit outweighs the risk in the cohort of patients under scrutiny.
Case review can serve a similar purpose. Programs can stay apprised of high selection risk by reviewing cases regularly, especially patients who have suffered an adverse outcome or long hospitalizations. Review should focus on the quality of preprocedural assessment and decision-making. In our own practice, mortality after elective surgery is reviewed 100%, as are mortalities that fall into the U.S. News & World Report diagnosis-related group (DRG). Patients with poor outcomes, whose preprocedural course identifies considerable risk, inform care teams of the need to strengthen the workup process, marshal additional care resources, and deepen cross-disciplinary decision support.
Our organization’s mortality oversight group reviews mortality trends across service lines and directs action when adverse trends are identified. Case selection for high-risk procedures is an important driver of risk-adjusted mortality and a focus of our group. During its work for the past 4–5 years, this group has intentionally and systematically requested and reviewed a grouping of reports from our medical informatics department. Examples are mortality by service line, mortality of patients presenting with sepsis or acquiring sepsis in hospital, and mortality of patients transferred from other health-care facilities. This coordinated and rigorous review process has helped identify the need for improvement efforts and supported necessary resources to effect these changes. These improvements have included more rigorous processes in cross-disciplinary input for case selection, care planning, and longitudinal coordination of care. This has greatly benefited our programs for the management of advanced heart failure, pulmonary embolism, extracorporeal membrane oxygenation, stroke, and intracranial bleeding.
Key Concept
Timely availability of outcome data allows teams managing high-risk interventions to adjust their processes, including the process for patient selection, so that optimal outcomes can be achieved.
2 Real-Life Examples of Managing Clinical Selection Risk
The following examples illustrate how clinical interventional programs at our organization have used data analyses and case review to improve care through data transparency, standardization, and multidisciplinary decision-making.
Advanced Cardiovascular Interventions
After a year of review for U.S. News mortalities in the specialty of cardiology and cardiac surgery, a pattern of selection risk became evident. Advanced heart failure patients (INTERMACS classification level 1) with cardiogenic shock have a substantially elevated mortality [1], likely related to the end-organ damage incident to cardiogenic shock. Careful patient selection processes are required to identify patients with cardiogenic shock who require percutaneous cardiac assist devices to reverse end-organ damage. We identified a number of cases for whom advanced heart failure interventional care was initiated and for whom a destination procedure such as heart transplant or mechanical heart was ultimately not appropriate. Instituting a clinical pathway for advanced heart failure allowed the introduction of cross-disciplinary decision-making at a much earlier stage in the patient’s therapeutic planning process. As a result, fewer patients died while supported by bridging or assist therapies prior to transplant or mechanical heart implantation. The clinical decision to embark on the advanced heart failure option is now reliably made with cardiac surgical, cardiology, and transplant specialty input. The survival score for the specialty increased during the years following this intervention (Fig. 6.1).
Pulmonary embolism (PE) outcomes improve when physicians representing the specialties that contribute to clinical and interventional management agree on a schema and process for a multidisciplinary approach. Over the past decade, major referral centers have organized pulmonary embolism rapid response teams (PERTs). While the overall impact of PERTs on mortality and functional outcome after major PE is still being investigated, PERTs have been demonstrated to improve access to advanced therapies for PE, such as catheter-directed thrombolysis [2, 3]. Our organization’s mortality oversight group identified an opportunity for improvement in this population. As a result, physician leaders from cardiology, cardiovascular surgery, emergency services, interventional radiology, pulmonary critical care, and hospital medicine agreed to establish a PERT. In addition, there was agreement on a clinical management algorithm and process by which the physicians on call for each specialty come together via a dedicated conference call prior to interventional management for PE (Fig. 6.2). After initiation of this call, which occurs on a 24/7 basis, the approach to interventional care for the patient with PE is agreed upon and implemented with input from all disciplines.
This multidisciplinary approach has allowed for the streamlined evaluation of patients and formulation of comprehensive treatment plans. It has facilitated the rapid mobilization of resources to provide the highest level of care to those patients with PE in need. At a national and international level, the PERT Consortium has been developed to unite the efforts of PERT teams across the United States and internationally. The purpose of the PERT Consortium is to serve the general public by undertaking activities to advance the status of PE care and promote research in the treatment of PE. The mechanisms to engage a multidisciplinary approach are proving to be an invaluable resource in the decision-making processes and treatment of high-risk PE patients. Our institution has joined this consortium to better serve the needs of our patients using a multidisciplinary approach.
Managing Clinical Risk in the Neurosciences
A similar review process exists for the specialties of neurology and neurosurgery. During mortality review, we identify patients who underwent percutaneous neurovascular or open neurosurgical procedures, with a view toward optimal selection. The recognition of significant comorbidity, coupled with ongoing life-threatening disease (such as hemodynamic instability), has led to rethinking the need to perform a neurointervention as a first resuscitative measure. We have also implemented a clinical evaluation unit designed to evaluate patients with devastating neurological injuries prior to admission. This adds value to a center like ours with a high volume of regional transfers. As we accomplished concurrent mortality reviews for patients with neurological disease, inpatient hospital deaths began to decrease (Fig. 6.3). In addition, the organization’s neuroscience service line has continued to rank among the top 50 hospitals in U.S. News. In Vizient, our neuroscience service line ranked at the 65th percentile in risk-adjusted mortality among comprehensive academic medical centers. Ochsner neuroscience risk-adjusted mortality was also lower than that of 7 of the 20 U.S. News Honor Roll hospitals in 2020.
Managing Clinical Risk in a Multiorgan Transplant Institute
Several mechanisms allow transplant programs to manage their risk. First, our transplant teams’ results are publicly available on the Internet. These results are not provided by the transplant programs themselves but come from a third party that assures 100% compliance with every process and outcome measure included. Second, the Centers for Medicare & Medicaid Services and the United Network for Organ Sharing (UNOS) mandate a quality program with internal audits for every transplant program.
Our teams have developed multiple dashboards to track our results in real time for risk management. The Scientific Registry of Transplant Recipients reports a 2.5-year rolling cohort of results; we can also look at each individual 6-month cohort. We share all the dashboards in real time with all our staff (Table 6.1). We hold monthly transplant council meetings and have each organ director present their own dashboard in depth. The entire transplant department has the opportunity to discuss the dashboards after each presentation. A recent example of improvement using this approach has been to assure complete documentation of pretransplant verification of ABO status.
We have also developed internal tools to stratify the risk of the recipients, which allows for appropriate donor and recipient selection. The CUSUM charts are one of many tools we use to manage risk. When adverse trends in outcome are noted, an in-depth investigation into possible causes is conducted.
Selection risk is evaluated, such as the quality of the donor organ, the age, major comorbidity, and retransplant status [4, 5]. The concept of recipient selection as a way to balance the risk of using a potentially marginal liver allograft has previously been addressed [6, 7]. Allografts with the highest risk, such as those with advanced age, prolonged ischemia times, or high fat content by liver biopsy, are matched with lower-risk recipients in an attempt to optimize outcomes.
Risk may also lie with the potential recipient. The technical complexity of liver transplant surgery substantially influences outcomes. Transplant outcomes are affected by recipient factors such as previous abdominal surgeries, central obesity, history of intra-abdominal infection, the presence and chronicity of ascites, and/or the presence and extension of portal vein thrombosis. Each of these factors can significantly impact operative physiological conditions that may compromise the conditions for organ reperfusion. Taking stock of these risk factors is key when considering marginal donor allografts since they may be more susceptible to challenging reperfusion conditions.
For more than 5 years, transplant surgeons at Ochsner Medical Center have been using a risk classification system so that the approach to manage risk is more standardized [8]. Patients listed for liver transplant are categorized by potential surgical complexity, based on the recipient’s surgical and medical history, physical examination, and cross-sectional imaging. Risk scores of A (low), B (moderate), or C (high) are assigned. The goal of this risk stratification system was to further understand the role of surgical complexity in transplant outcomes. In addition, we sought to facilitate donor–recipient matching and expedite the placement of marginal allografts. Team discussion of the potential recipient surgical risk classification is integral to the on-call workflow at the time of an organ offer.
Key Concept
Standardizing the recipient–donor match process in liver transplantation allows for better operative planning and resource utilization. As a result, patient and graft survival rates using marginal organs compare favorably with those achieved using organs according to conventional criteria.
Carefully taking into account the surgical complexity related to the recipient allows for better operative planning and resource utilization. When we stratify patients according to expected surgical complexity, we can predict operative risk more precisely (e.g., predicting operative time and transfusion requirements). This stratification allows our transplant team to match a higher-risk organ rapidly with a lower-risk recipient, thus expediting organ placement. It also allows us to achieve patient and graft survival rates using marginal organs that compare favorably with those achieved using organs according to standard criteria.
References
Shah SP, Mehra MR. Durable left ventricular assist device therapy in advanced heart failure: patient selection and clinical outcomes. Indian Heart J. 2016;68:S45–51.
Rosovsky R, Zhao K, Sista A, Rivera-Lebron B, Kabrhel C. Pulmonary embolism response teams: purpose, evidence for efficacy, and future research directions. Res Pract Thromb Haemost. 2019;3:315–30.
Kabrhel C, Rosovsky R, Channick R, Jaff MR, Weinberg I, Sundt T, Dudzinski DM, Rodriguez-Lopez J, Parry BA, Harshbarger S, Chang Y, Rosenfield K. A multidisciplinary pulmonary embolism response team: initial 30-month experience with a novel approach to delivery of care to patients with submassive and massive pulmonary embolism. Chest. 2016;150(2):384–93.
Nacif LS, Pinheiro RS, et al. Better selection criteria with prognostic factors for liver transplantation. Transplant Proc. 2018;50:766–8.
Findlay JY. Patient selection and preoperative evaluation for transplant surgery. Anesthesiol Clin. 2013;31:689–704.
Mateo R, Cho Y, Singh G, Stapfer M, Donovan J, et al. Risk factors for graft survival after liver transplantation from donation after cardiac death donors: an analysis of OPTN/UNOS data. Am J Transplant. 2006;6:791–6.
Grewal HP, Willingham DL, Nguyen J, Hewitt WR, Taner BC, et al. Liver transplantation using controlled donation after cardiac death donors: an analysis of a large single center experience. Liver Transpl. 2009;15:1028–35.
Humberto B, Cohen A, Loss G. Recipient selection in DCD liver transplantation. In: Donation after circulatory death (DCD) liver transplantation. Cham: Springer Nature; 2020. p. 121–36.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Loss, G., Cohen, A.J., Zweifler, R.M., Desai, S., Jenkins, J.S., Schubert, A. (2022). Managing Clinical Selection Risk. In: Schubert, A., Kemmerly, S.A. (eds) Optimizing Widely Reported Hospital Quality and Safety Grades. Springer, Cham. https://doi.org/10.1007/978-3-031-04141-9_6
Download citation
DOI: https://doi.org/10.1007/978-3-031-04141-9_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-04140-2
Online ISBN: 978-3-031-04141-9
eBook Packages: MedicineMedicine (R0)