Abstract
In this chapter, we lay out the challenges that women face when pursuing a research career in pediatrics, and in academic medicine generally. Specifically, we review the concept of the “leaky pipeline,” which reduces the numbers of women in the more senior research positions. We identify structural elements of an academic career in research, such as training, funding, and peer review publication process, and promotion may contribute to the leaky pipeline. Modifying these structural elements to eliminate existing gender bias is critical to “sealing the leak” in the pipeline.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
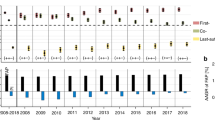
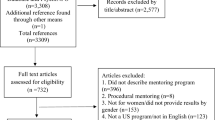
Research is the gold standard by which academic success is measured. There is no higher achievement in medicine than the Nobel Prize; up until 2014, only 16 women have ever received a Nobel Prize for their contributions to research [1]; seven additional have been awarded since then. But Nobel Prize winners are cultivated, through long years of training, and then graduated experiences as faculty and independent observers. The physician-scientist pipeline, as it is called for those who have a medical degree and pursue research-focused career, provides an orderly series of steps, from residency, to fellowship, to career development awards, through larger independent grants (Fig. 11.1) [2]. However, there is a concept called the “leaky pipeline,” [3] which describes the loss of diverse talent, particularly people from groups underrepresented in medicine and women, all along the physician-scientist pipeline. A study in the early 2000s found that there had been a steady decline in the percentage of women medical students who intended to pursue medical careers [4]; while we don’t have current data to see the percentage of women medical students who are interested in or contemplating a research career, the challenges in obtaining research funding can’t have helped.
NIH support for the physician-scientist pipeline https://acd.od.nih.gov/documents/reports/PSW_Report_ACD_06042014.pdf
Women have been vibrant contributors to medical research. Nobel Prizes in Physiology have gone to Gerty Cori, for her work on carbohydrate metabolism; Rosalyn Yalow, for developing the radioimmunoassay; and Dr. Francoise Barre-Sinoussi, for discovering the way that HIV is spread, among many others. Yet there have been other women scientists, such as Rosalind Franklin, whose critical contributions were undervalued or overlooked [5]. As a result, it is important to recognize as we discuss the role of women in pediatric research, that we don’t forget about the persistent bias and additional challenges met by physicians of color, and from other underrepresented backgrounds. The leaky pipeline is just as leaky, and perhaps more so, for these groups.
Funding
Training researchers and conducting research require funding. For training medical researchers, the federal government funds numerous programs throughout the training pathway, from medical school through faculty (Fig. 11.1). Pediatric researcher trainees are eligible for most, if not all, of these programs. In 2001, 10% of all pediatric residency graduates pursued a career in research, far below that of other specialties such as internal medicine [6, 7]. Pediatric research at the NIH is funded across institutes, and efforts are being made to harmonize pediatric research activities across the NIH, including improving training for pediatric researchers of the next generation. One such trans-NIH initiative (NIH is made up of 27 institutes and centers) is NIH Pediatric Research Consortium (N-PeRC), which was established in 2018 [8]. Concerns have been raised that the current NIH training funding mechanisms have privileged existing training programs over new programs, thus limiting the ability to diversify the funding pool [9]. The current proportion of women who comprise pediatric research training programs is not available.
Foundation grants provide an important source of funding for pediatric research trainees, as well as established faculty. Foundation grants can range from a few thousand to a few hundred thousand dollars. These funding mechanisms are incredibly important and often undervalued by the broader academic community because of both their size and their low or absent indirect cost funding to institutions. Yet, these funding mechanisms provide critical funding to smaller scope research projects, which are common among pediatric trainees as well as established faculty who are working on new or emerging areas that may be seen as high risk by federal agencies.
The goal standard of research accomplishment is to receive an NIH award. For the junior faculty, that award is often a career development award. For a mid-level faculty member, that is often an R01 award. The challenge with this standard is that it excludes pediatric researchers who do not conduct research that aligns with the mission of the NIH. This could potentially exclude areas in which women pediatric researchers may focus.
While the largest group of funded investigators by the NIH is physicians with an MD only (51%), MD/PhDs are significantly overrepresented in NIH grant funding compared to their overall numbers. While there are many routes to an MD/PhD, the NIH funds the Medical Scientist Training Program (MSTP) at 43 institutions, which supports almost 1000 trainees each year. In 2011, women made up 39% of MD/PhD applicants, 37% of matriculants, and 42% of graduates [2]. However, a deeper dive into gender in MSTP programs in 2018 found that women were more likely to apply to programs that were lower in U.S. News & World Report ranking [10]. MSTP trainees are far more likely to receive their PhD in a biological or physical science, rather than social sciences, health services research, or clinical informatics [2]. Increasing opportunities for MD/PhD candidates to obtain their doctorate in a more clinical field is an opportunity to appeal to a broader audience, including potentially more women.
While we can see the overall funding patterns for physicians and physician scientists, it’s more difficult to know how that is reflected within pediatrics. Since women make up a much larger share of graduating physicians, it should follow that they would have higher representation in grant funding. However, there are few data on whether this is the case. In fact, a study of a pediatric resident research grant program found that women asked for less money, and received lower scores than men, even controlling for advanced degrees (of which men had more) [11]. If these disparities are starting in training, they are likely to persist.
While the percentage of women MDs who are NIH research project grant holders has increased from 17% in the mid-1990s to 29% in 2014, this growth has actually been slower for MD/PhDs, who were also at 17% in the mid-1990s, and were at 22% in 2014 [2]. In 2012, the research project grant award rate was not different by gender, with men successful 23% of the time, and women successful 24% [2].
There are multiple reasons why women may be underrepresented in research grant awards. The physician-scientist pipeline is not forgiving; women who take time during residency or fellowship to care for children may find completing a project that may launch their career and stimulate their interest in research daunting, and mentors may dissuade them from taking this path. Academic careers are often less financially rewarding, and thus young women may pragmatically decide that a clinical career provides more security. Of course, these decisions are not only being made by women; it is likely that having a process that rewards and supports less traditional pathways and time off would also encourage more talented men to enter research careers. Alternatively, the system of K to R transitions has historically relied on sponsorship and mentorship, and we know that women often don’t get the same opportunities to engage with more senior faculty as men.
Publications
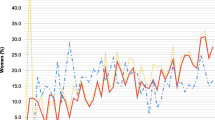
From 2000 to 2015, women increased from 32% of authors to 41% of authors in the Annals of Internal Medicine, though in 2016 only 16% were senior authors [12]. The field of pediatrics provides an interesting case study in authorship representation by gender. Pediatrics is one of only two specialties in medicine where the proportion of practicing physicians who are women is over 50%. In 2017, women were 72% of pediatric residents, 63% of practicing physicians, and 57% of academic pediatricians [13]. Fishman et al. (2017) [14] assessed the prevalence of authorship by women in three high impact pediatrics journals from 2001 to 2016, as well as editorial board membership. The overall proportion of women first authors increased from 40% to 58% (p < .001); the proportion of senior authors increased from 29% to 38% (P < .001) [14]. They concluded that women first authors are underrepresented in comparison to women junior faculty, while women senior authors are represented in number similar to women senior faculty. A more recent study examined the representation of women authors in perspective articles in high impact pediatric journals. The proportion of women first authors was 42%, and this was even lower among the authors of articles in journals where the perspectives were considered “scholarly” (15–44%), compared to “narrative” (53% vs. 66%) [15].
This disparity is even more apparent in other fields. A review of cardiovascular clinical trials published in high impact journals found that only 9% of first authors and 10% of last authors were women, and this was even more striking in large and procedurally oriented trials [16]. More recently, the COVID-19 pandemic has highlighted discrepancies in the ability of women to balance the increased child care demands of at-home schooling with the demands of an academic career, and in fact a 2020 report found that women’s shares of papers from 2019 to 2020 decreased by 14% for first author papers, 3% for senior author papers, and 5% for overall representation [17].
Women also lag in placement on editorial boards. The Fishman et al. (2017) article also assessed editorial board membership at the three high impact pediatric journals, and found that overall representation of women increased from 18% in 2001 to 40% in 2016 (p < .001).
As we look at the leaky pipeline to professor and leadership positions for women, we must recognize the role that research and scholarship play. Department chairs are often chosen for their research portfolios, rather than their management skills. Thus, fewer women choosing research careers will mean fewer being considered for these roles. There is certainly debate about whether physician-scientists make the best chairs, but to have gender equity in academic pediatrics, we must also consider the value of nonphysician scientists in leadership roles, and work to make research an attractive and viable option for women.
Training and Transition to Faculty
Fellowships
Most pediatric-focused fellowships involve a combination of clinical and research training. To complete training for many pediatric board specialties, individuals must engage in scholarly activity and produce a work product [18]. The options for activities vary, but research, grants, and published manuscripts are among them. There are research-focused fellowships available for pediatricians. One of the most well-known has been the Robert Wood Johnson Clinical Scholars Program (RWJ CSP) [19]. In recent years, this program has moved away from funding single MD development to funding team-based multidisciplinary model. A program run by alumnae of NCSP, National Clinician Scholars Program, has emerged to assume the mission of the original RWJ CSP [20].
In many cases, fellowship might be the first time that a trainee encounters the opportunity to lead a research project. Often fellowship is the time when a trainee has specific and substantial time set aside to spend focused time on research. Times vary by specific fellowship and across fellowship sites within a specialty. Admittedly, this time can be scheduled and “fit in” alongside other clinical duties like overnight calls, for example. This can create obvious challenges for women, who are often primary caregivers, with balancing workload and family responsibilities. The importance of mentorship to fellowship research success cannot be understated [21].
Early Faculty
Fellowship is also an important time in a physician researcher’s career because it provides the foundation upon which a future faculty position is built [22]. Navigating the search and negotiation of a junior faculty position can be challenging for any trainee. Women face additional hurdles related to their socialized approach to negotiation, as well as the culture’s reaction to their negotiation style [23]. It is critical that a faculty member who is committed to a physician-investigator career have the necessary administrative, capital, and mentorship resources to achieve their early career goals [24]. For example, start-up support, (i.e., institutional funds to provide for research-based activities such as faculty salary, research staff salary, non-personnel-related research costs) has been linked to increased success of NIH funding [25]. Unfortunately, studies outside of pediatrics have demonstrated that women faculty have been shown to be receive less institutional support, especially in the basic sciences [26]. The legacy of less institutional support for women researchers compounded with their caregiver roles has been shown to severely impact their productivity [27]. Similarly, flexible employment, including part time, for research intensive faculty is particularly relevant for women who may have the primary or majority role as caregiver in the home [29, 30].
Promotion
Progressing through the ranks of academic medicine can be a grind. While promotion is anchored in achievement in scholarship, the road can be fraught with challenges, both personal and professional, individual, and institutional. Physician-scientists Drs. Megan Moreno and Rachel Katzenellenbogen have encouraged women faculty to utilize the a socioecological (SEM) framework to plan and assess their career growth [28]. The SEM framework places the faculty member within larger contexts which include their mentors, colleagues, and teams, their academic environment, and their professional society. Within this framework, faculty can consider their academic achievement (e.g., publications, grants, etc.) as well as their support within and outside of their institution (e.g., mentorship, sponsorship, administrative and capital resources).
Research Leadership
After achieving success in leadership, some physician-investigators go on to leadership positions. Such leadership paths include dean positions (research, medical school), department chairs, vice chairs of research, or chief scientific/research officers of research institutes. However, as one moves through these ranks, the prevalence of women decreases [13]. Women’s representation among pediatric research professional societies is slightly better [13]. While progress has been made in the support of women pediatric researchers, there is room for continued improvement [31].
References
Modgil S, Gill R, Lakshmi Sharma V, Velassery S, Anand A. Nobel nominations in science: constraints of the fairer sex. Ann Neurosci. 2018;25(2):63–79. https://doi.org/10.1159/000481906.
National Institutes of Health. Physician-Scientist Workforce Working Group Report; 2014.
Goulden M, Mason MA, Frasch K. Keeping women in the science pipeline. Ann Am Acad Pol Soc Sci. 2011;638(1):141–62. https://doi.org/10.1177/0002716211416925.
Guelich JM, Singer BH, Castro MC, Rosenberg LE. A gender gap in the next generation of physician-scientists: medical student interest and participation in research. J Investig Med. 2002;50(6):7.
6 Women Scientists Who Were Snubbed Due to Sexism. Culture. Published May 19, 2013. Accessed August 13, 2021. https://www.nationalgeographic.com/culture/article/130519-women-scientists-overlooked-dna-history-science.
Committee on Pediatric Research. Promoting education, mentorship, and support for pediatric research. Pediatrics. 2001;107(6):1447–50. https://doi.org/10.1542/peds.107.6.1447.
McCabe LL. National Institutes of Health support for research and training: future of pediatrician scientists. Arch Pediatr Adolesc Med. 1998;152(9):839–42. https://doi.org/10.1001/archpedi.152.9.839.
NIH Pediatric Research Consortium (N-PeRC). https://www.nichd.nih.gov/. Accessed August 13, 2021. https://www.nichd.nih.gov/research/supported/nperc.
Rivkees SA. The missing link of NIH funding in pediatric research training program restructuring. Pediatrics. 2014;134(6):e1521–2. https://doi.org/10.1542/peds.2014-1100.
Bowen CJ, Kersbergen CJ, Tang O, Cox A, Beach MC. Medical school research ranking is associated with gender inequality in MSTP application rates. BMC Med Educ. 2018;18(1):187. https://doi.org/10.1186/s12909-018-1306-z.
Gordon MB, Osganian SK, Emans SJ, Lovejoy FH. Gender differences in research Grant applications for pediatric residents. Pediatrics. 2009;124(2):e355–61. https://doi.org/10.1542/peds.2008-3626.
Gayet-Ageron A, Poncet A, Perneger T. Comparison of the contributions of female and male authors to medical research in 2000 and 2015: a cross-sectional study. BMJ Open. 2019;9(2):e024436. https://doi.org/10.1136/bmjopen-2018-024436.
Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149.
Fishman M, Williams WA, Goodman DM, Ross LF. Gender differences in the authorship of original research in pediatric journals, 2001–2016. J Pediatr. 2017;191:244–249.e1. https://doi.org/10.1016/j.jpeds.2017.08.044.
Silver JK, Poorman JA, Reilly JM, Spector ND, Goldstein R, Zafonte RD. Assessment of women physicians among authors of perspective-type articles published in high-impact pediatric journals. JAMA Netw Open. 2018;1(3):e180802. https://doi.org/10.1001/jamanetworkopen.2018.0802.
Denby KJ, Szpakowski N, Silver J, Walsh MN, Nissen S, Cho L. Representation of women in cardiovascular clinical trial leadership. JAMA Intern Med. 2020;180(10):1382. https://doi.org/10.1001/jamainternmed.2020.2485.
Andersen JP, Nielsen MW, Simone NL, Lewiss RE, Jagsi R. COVID-19 medical papers have fewer women first authors than expected. eLife. 2020;9:e58807. https://doi.org/10.7554/eLife.58807.
Scholarly Activity | The American Board of Pediatrics. Accessed August 13, 2021. https://www.abp.org/content/scholarly-activity.
Voelker R. Robert wood Johnson clinical scholars mark 35 years of health services research. Medical News & Perspectives. 2007:2571–3.
National Clinician Scholars Program | NCSP National Clinician Scholars Program. Accessed August 13, 2021. https://nationalcsp.org/.
Steiner JF, Curtis P, Lanphear BP, Vu KO, Main DS. Assessing the role of influential mentors in the research development of primary care fellows. Acad Med J Assoc Am Med Coll. 2004;79(9):865–72. https://doi.org/10.1097/00001888-200409000-00012.
Saha S, Christakis DA, Saint S, Whooley MA, Simon SR. Perspectives a survival guide for generalist physicians in part 1. Getting Started. 1999;April
Sambuco D, Dabrowska A, DeCastro R, Stewart A, Ubel PA, Jagsi R. Negotiation in academic medicine: narratives of faculty researchers and their mentors. Acad Med. 2013;88(4):505–11. https://doi.org/10.1097/ACM.0b013e318286072b.
Saha S, Saint S, Christakis DA, Simon SR, Fihn SD. A survival guide for generalist physicians: preparing for the transition to junior faculty. J Gen Intern Med. 1999;April:750–5.
Connelly MT, Sullivan AM, Chinchilla M, et al. The impact of a junior faculty fellowship award on academic advancement and retention. Acad Med. 2017;92(8):1160–7. https://doi.org/10.1097/ACM.0000000000001541.
Sege R, Nykiel-Bub L, Selk S. Sex differences in institutional support for junior biomedical researchers. JAMA. 2015;314(11):1175. https://doi.org/10.1001/jama.2015.8517.
Carr PL. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129(7):532. https://doi.org/10.7326/0003-4819-129-7-199810010-00004.
Moreno MA, Katzenellenbogen R. Women rock science: a pocket guide for success in clinical academic research careers. Cham, Switzerland: Springer; 2019.
Alexander D, Boat T, Britto M, et al. Federation of Pediatric Organizations Task Force on women in pediatrics: considerations for part-time training and employment for research-intensive fellows and faculty. J Pediatr. 2009;154(1):1–3.e2. https://doi.org/10.1016/j.jpeds.2008.08.010.
Women Chairs of the Association of Medical School Pediatric Department Chairs. Women in pediatrics: recommendations for the future. Pediatrics. 2007;119(5):1000–5. https://doi.org/10.1542/peds.2006-2909.
Carr PL, Gunn CM, Kaplan SA, Raj A, Freund KM. Inadequate progress for women in academic medicine: findings from the National Faculty Study. J Women's Health. 2015;24(3):190–9. https://doi.org/10.1089/jwh.2014.4848.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wilson, K.M., Tarini, B.A. (2022). Research, Funding, and Publication for Women in Pediatrics. In: Spector, N.D., O'Toole, J.K., Overholser, B. (eds) Women in Pediatrics . Springer, Cham. https://doi.org/10.1007/978-3-030-98222-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-98222-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-98221-8
Online ISBN: 978-3-030-98222-5
eBook Packages: MedicineMedicine (R0)