Abstract
Since the computed microtomography (micro-CT) was invented at the end of the twentieth century, it has been one of the fastest-growing applications in the history of the dental researches. Especially, recent decades have seen the rapid development of micro-CT technology and imaging analyses software, and their widespread application from carious lesions, tooth resorption, periodontal disease, periapical pathology to dental implantology. In this chapter, we are going to have a comprehensive review in the development and application of micro-CT in dentistry, with a possible comparison with other 3D radiographic ways. At the end, the chapter will launch a prospect for further researches.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
15.1 General Introduction of Micro-CT and Nano-CT in Dentistry
Traditionally, the histology has long been a popular approach in dentistry research for resolving the interior microstructure of teeth and alveolar bone samples. It is feasible to get a two-dimensional resolution at the micron level by histological preparation of the materials, such as tissue cutting and chemical staining, but this is destructive and time-consuming. The biological sample cannot usually be utilized for further tests after the permanent changes that occur during histological preparation, such as serial sections, transparency, and dye penetration. As a result, researchers would benefit from an alternate technology that allows three-dimensional studies, such as X-ray microtomography (XMT, commonly known as micro-CT), to examine the internal structure of oral tissues without destroying or shrinking the samples [1, 2].
Radiology has made a breakthrough in the last 50 years, especially with computerized tomography (CT) and the later discovered magnetic resonance imaging (MRI) technique. CT, was discovered in 1972 and is being used routinely today. CT allows visualization of normal and abnormal soft tissue and bone tissues. It is also an ideal method for the determination of calcifications. CT applications in the head and neck region allow the evaluation of inflammation, cysts, benign and malignant tumors. It provides detailed visualization of the nasal cavity, lateral nasal wall, osteomeatal unit, and sinuses before functional endoscopic sinus surgery. Apart from this, it is useful in maxillofacial, reconstructive and orthognathic pre-surgery planning, dental implant applications, trauma, and temporomandibular joint (TMJ) diseases. Compared to conventional imaging methods of CT, it allows visualization of the structure desired to be examined without superposition of the surrounding tissues, high contrast resolution enabling two tissues with different physical densities to be separated from each other more easily, allowing tissue to be visualized in axial, coronal, and sagittal planes, absence of distortion and magnification. It has many advantages such as allowing determination of whether these lesions have a solid or liquid structure by density measurements in the presence of cysts or tumors. In addition, there are also disadvantages such as the need for contrast agent for imaging soft tissues, giving more radiation than conventional methods, and deterioration of image quality due to scattering of metallic objects in the image.
Computed microtomography (Micro-CT) devices can select the field of view (FOV) according to the size of the area to be examined, and in this way, higher resolution images can be obtained when working in smaller areas. Currently, in vitro and in vivo micro-CT devices are available, and the varying FOV ratios in these devices determine the area to be examined and the resolution to be obtained. Micro-CT systems use microfocal X-ray source and high resolution detectors to create 3D reconstructions of samples. The main parts of the device are the X-ray tube, a computer-controlled stepping motor that rotates the sample fixed on it at certain intervals, an image intensifier that concentrates the X-ray in the environment on the camera sensor, a CCD camera that converts the X-rays falling on it into image data, an image collector and a computer to control all the system.
The scanned object rotates on a bed while the system takes multiple X-ray shadow transition images from different angles. Using these shadow images, the reconstruction of the cross-sectional images of the object is processed and a three-dimensional model of the internal microstructure and density in the selected height range is created in the transition images. With reconstruction (reconstruction), internal morphological parameters can also be calculated. Traditional medical CT scanners allow three-dimensional imaging. The three-dimensional imaging of anatomical landmarks can be meaured without using sample preparation steps. The spatial resolution (resolution) of Medical Computed Tomographs (CT) is 1–2 mm, which corresponds to 1–10 mm3 voxel (three-dimensional pixel) size. Micro-CT, on the other hand, enable spatial resolution of less than 10 μm, reaching 1×10−6 mm3 voxel size. Micro-CT is currently used in biomedical research, materials science, pharmaceutical drug development and production, composites, dental research, electronic components, geology, zoology, botany, construction materials, paper production, and many other fields.
15.2 The Application of Micro-CT in Dentistry
In dentistry, there are a variety of samples that can be evaluated directly utilizing micro-CT. Mineralized tissues with a greater attenuation coefficient, such as teeth and bone, polymers, biomaterial scaffolds, and even high-density materials like metal implants and ceramics, are common examples of these samples. Micro-CT imaging can now be performed on soft tissues such as periodontal blood vessels that have been perfused with a contrast agent, as long as the contrast agent has a higher density than the surrounding tissue. With the rapid advancement of micro-CT systems over the last decade, the latest generation of systems, such as SkyScan nano-CT® and Phoenix nanotom®, now allow for even higher spatial resolution at the sub-micron level. Furthermore, in vivo imaging of small live animals has become available for long-term investigation of developmental deformities or pathology of the jaw.
15.2.1 Gap Formations for Dental Materials
Gaps and bubbles are imperfections in dental materials that impair their mechanical qualities. The gaps can be assessed for root canal therapy, but they can also be analyzed in dental composite replacement materials.
Although the composite structure has adequate mechanical properties at first, gaps can impair the repairs’ performance under fatigue loading. Internal gaps can impair the composite’s durability, which can lead to fracture and clinical failure in restorations. Furthermore, an increase in gaps in the composite mass, as well as further staining of the restoration, can result in higher water absorption (Fig. 15.1).
For prosthodontic restorations, the internal gap between restoration and abutment tooth is significant. Also, the gap on the finish line is a subject that has been widely evaluated. Due to the thickness of the gap between restoration and tooth, the strain of the cement is affected. And the improper thickness of cement gap may cause decementation, micro-leakage, and carious formation (Fig. 15.2).
Micro-organisms from gutta and outer coverings, or directly from the dentin can be important factors in root canal treatment and healing (Fig. 15.3). These factors have led and also demnaded for micro-leakage studies in endodontics (Figs. 15.4 and 15.5) [3, 4].
15.2.2 Evaluations in Implantology
Dental implants’ evaluations are another key application of micro-CT in dental research. A high-resolution 3D model of peri-implant bone created using micro-CT scanning could be used to assess treatment choices such as implant insertion techniques, antibiotics, antibacterial coatings, and anti-resorbing coatings on peri-implant bone remodeling and adaption (Fig. 15.6). Furthermore, in vivo micro-CT (e.g. SkyScan 1276) gives tiny animals a minimal radiation dosage with implant therapy, allowing for numerous scans in longitudinal preclinical research without the possibility of undesirable radiation-induced side effects.
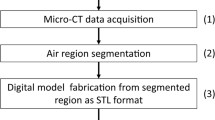
The region of interest where the bone-implant contact remains has gotten a lot of attention from researchers. It used to be a 2D histological investigation (Fig. 15.7), but it has now evolved into a 3D non-invasive method. Here is a diagram of how to choose 3D volumes of interest for morphometric analysis in the peri-implant bone region.
The 3D VOIs were mostly made up of trabecular bone, which was chosen using interpolated cross-sections and proprietary processing. In each section, irregular anatomic regions of interest (ROIs) can be created, excluding cortical bone in the ring-shaped ROIs and retaining only trabecular features for assessment. Following the recommendations of the American Society of Bone and Mineral Metabolism and Parfitt’s system, standard three-dimensional structural parameters of trabecular bone architecture could be estimated using CTAn on these VOIs [3,4,5].
Metal artefacts, which usually appear as strong streaks surrounding metallic objects, remain a barrier during imaging acquisition and segmentation, despite the numerous applications in the dental implant area. Examples of typical metal artifacts from screw-shaped Ti metal alloy implants include halo, shadow, and blurring effects generated by the material’s composition, the implant’s sharp-edged or perpendicular shape, and projection images from a single optical axis (Fig. 15.8a, b) [6].
Metal artefacts are caused by beam hardening, photon scattering, and photon starvation. According to the authors, implant materials made of pure Ti (titanium), biodegradable PLA (polylactic-coglycolic acid) collagen, or Mg can have relatively favorable imaging results, whereas heavy materials like Zr and Pt, which have higher atomic numbers and higher attenuation coefficients than body tissues, can cause serious imaging artifacts. As a result, obtaining high-contrast pictures is challenging, making it difficult to distinguish bone from implants (Fig. 15.9).
A morphometric quantification of peri-implant bone quality. From left to right, original cross-sectional gray image; manually rough selection of the ROI; binary ROI automatically generated by a custom processing algorithm based on thresholding segmentation for the implant protocols, excluding implant and cortical bone; binary segmentation of trabecular bone in this ROI, from which trabecular morphometric parameters were calculated
It is always recommended to scan the sample with metal implants at a high voltage, high filtering, a small rotation step, a high frame averaging value, and 360° full scan, round scanning to minimize metal artifacts. Furthermore, according to the current study, an optical axis method of spiral scanning with a unique optical axis will aid in the removal of these artefacts. Metal artifacts, it is also expected, will be decreased to a limited extent as a result of the current development of reconstruction algorism [7, 8].
15.2.3 Carious Formations
Micro-CT has been authorized and widely regarded as a more precise and dependable method of measurement than direct measurement, 3D scanning, or photography. As a result, when measuring the distance between internal and external structures in teeth, such as the crown, enamel, dentin, and pulp chamber, this imaging technique might be recognized as an accurate and valuable tool (Fig. 15.10). However, because of partial volume effects, a lower resolution micro-CT scanning with a pixel size of 10 m is not capable of resolving very thin enamel thicknesses of less than 100 m. As a result, it is usually best to choose a suitable pixel size for the evaluated objects before beginning the study project, which should be 10 times less than the true structure thickness [9].
Furthermore, micro-CT and associated data analysis tools may generate volume information more correctly and reliably. With this quantitative data, it is simple to examine the changes or differences that occurred before and after a specific therapy, such as caries excavation.
Another fascinating application is molar incisor hypomineralization (MIH), a structural aberration that affects the quality of tooth enamel and has far-reaching implications for the entire oral health system. Although the ethological elements are still unknown. The use of micro-CT to identify hypo-mineralized enamel in a non-destructive manner has been validated for onset of MIH, which will aid in understanding the pathology and clinical management of MIH lesions. If a density calibration technique is performed, Micro-CT can be used to quantify mineral density of enamel white spot lesions and dentin caries, either using default Hounsfield units or utilizing homogeneous porous hydroxyapatite (HA) phantoms with varying densities (Fig. 15.11).
15.2.4 Tooth Resorption
Micro-CT, in comparison to clinical cone beam CT, can not only give non-invasive 3D imaging of teeth, but also more exact measurements and higher contrast on the devoted anatomical components of teeth, which is especially important when investigating tooth internal/external resorption (Fig. 15.12). A study found that by comparing the morphological characteristics of the pulp cavity, the volume ratio at the horn, floor, and overall regions of the pulp chamber, and the diameters of the buccal and lingual orifices of the root canals between different study groups, it is possible to identify the morphological characteristics of the pulp cavity, the volume ratio at the horn, floor, and overall regions of the pulp chamber, and the diameters of the buccal and lingual orifices of the root canals.
It is worth noting that using higher image resolution allows you to see more features within and outside the tooth. This will inevitably result in unnecessary scanning time and resources being wasted. Despite this, the lack of consistency in scanning techniques may result in inconsistent outcomes. As a result, comparing micro-CT and Nano-CT images to identify the cut-off voxel size value for assessing root canal filling gaps is required. A voxel resolution of 11.2 m was defined as a cut-off value in micro-CT imaging for the evaluation of root canal filling gaps, according to a recent study [10].
15.3 Micro-CT Combination with Other Techniques
Due to the poor absorption contrast, it is difficult to visualize the soft tissues, including as blood vessels, periodontal ligaments, and nerve fibers, which is one of the main limitation of the micro CT technique. Contrast-enhanced micro-CT imaging has a growing demand and interest especially for invivo imaging. Superior imaging and quantification of 3D soft tissue under micro CT is now available because to these contrast enhanced agents. An example of such a contrast agent is Angiofil [11].
The virtual finite element analysis allows compression, bending, and screw pull-out tests to be performed directly from the 3D micro-CT dataset. With varying loadings or restorative materials, detailed and valid three-dimensional finite element models of tooth, implant, and peri-implant bone can be created. When this technology can able to process data more rapidily, there will be additions applictions for dental research [4, 12, 13] (Fig. 15.13).
Dual-energy CT is also described as an imaging technique that describes the major contrast changes caused by the staining period, the staining agent utilized, and the organ investigated. Two separate X-ray energy spectra (usually one high and one low energy) will be employed to gain further quantitative information on the accumulation of staining agents within the soft-tissue samples in 3D. For mouse heart and lung ex vivo, it showed shorter staining periods (many hours) and higher resolution contrast (Fig. 15.14).
By obtaining a resonance signal from the hydrogen nucleus, such as water in the bodily tissue, MRI investigates the target region. This imaging approach excels at resolving soft tissues and inflammatory processes without the use of a contrast agent. It is the ideal alternative for the research of TMJ location and morphology, skeletal physiology, tumors, and the healing of grafts, regardless of cost or availability Combining MRI and micro-CT to analyze the trabecular structure of human bone specimens and comparing it to bone mineral density in the prediction of bone strength is also achievable [14,15,16].
15.4 Future Projection for Micro-CT
Micro-CT, which was once a costly and unknown imaging tool, has now become a practical and routine application, particularly in the dentistry scientific field. Given that micro-CT can resolve a lot of fine structures of teeth and periodontal tissues in a non-invasive manner, it is a viable alternative to many traditional dental research methods. As a result, micro-CT data could be used to further investigate root canal anatomy in experimental endodontics, preclinical training in fundamental endodontic procedures, periapical and periodontal pathology, craniofacial skeletal structure and development, and peri-implant osseointegration, as well as a valuable mathematical modeling of tooth morphology in both healthy and pathological states.
However, it can only be used in in vitro human investigations and in vivo animal studies right now. With the development of micro-CT techniques, additional micro/nano-CT applications will be broadening the dental research, from millimeters to nanometers, from biological samples to material samples, from the lab bench to the chairside, for both research and industrial applications, without destroying dental samples.
References
Davis GR, Elliott JC. High definition X-ray microtomography using a conventional impact X-ray source. J Phys IV. 2003;104:131–4.
Davis G, Evershed A, Elliott J, Mills D. Quantitative X-ray microtomography with a conventional source. Dev X-Ray Tomogr. 2010;7:7804.
Parfitt AM, Drezner MK, Glorieux FH, et al. Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry nomenclature committee. J Bone Miner Res. 1987;2:595–610.
Magne P. Efficient 3D finite element analysis of dental restorative procedures using micro-CT data. Dent Mater. 2007;23(5):539–48.
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res. 2010;25:1468–86.
Huang Y, Van Dessel J, Liang X, Depypere M, Zhong W, Ma G, Lambrichts I, Maes F, Jacobs R. Effects of immediate and delayed loading on peri-implant trabecular structures: a cone beam CT evaluation. Clin Implant Dent Relat Res. 2014;16(6):873–83.
Alghamdi HS, Bosco R, van den Beucken JJJP, Walboomers XF, Jansen JA. Osteogenicity of titanium implants coated with calcium phosphate or collagen type-I in osteoporotic rats. Biomaterials. 2013;34(15):3747–57.
Bissinger O, Probst FA, Wolff K-D, Jeschke A, Weitz J, Deppe H, Kolk A. Comparative 3D micro-CT and 2D histomorphometry analysis of dental implant osseointegration in the maxilla of minipigs. J Clin Periodontol. 2017;44(4):418–27.
Olejniczak AJ, Grine F. Assessment of the accuracy of dental enamel thickness measurements using microfocal X-ray computed tomography. Anat Rec Pt A. 2006;288A:263–75.
Oi T, Saka H, Ide Y. Three-dimensional observation of pulp cavities in the maxillary first premolar tooth using micro-CT. Int Endod J. 2002;37(1):46–51.
Hlushchuk R, Zubler C, Barre S, Shokiche CC, Schaad L, Röthlisberger R, Wnuk M, Daniel C, Khoma O, Tschanz SA, Reyes M, Djonov V. Cutting-edge microangio-CT: new dimensions in vascular imaging and kidney morphometry. Am J Physiol Renal Physiol. 2018;314(3):F493–9.
Bona AD, Borba M, Benetti P, Duan Y, Griggs JA. Three-dimensional finite element modelling of all-ceramic restorations based on micro-CT. J Dent. 2013;41(5):412–9.
Almedia EO, Rocha EP, Junior ACF, Anchetia RB, Poveda R, Gupta N, Coelho PG. Tilted and short implants supporting fixed prosthesis in an atrophic maxilla: a 3D-FEA biomechanical evaluation. Clin Implant Dent Relat Res. 2015;17(Suppl 1):e332–42.
De Souza e Silva JM, Utsch J, Kimm MA, Allner S, Epple MF, Achterhold K, Pfeiffer F. Dual-energy micro-CT for quantifying the time-course and staining characteristics of ex-vivo animal organs treated with iodine- and gadolinium-based contrast agents. Sci Rep. 2017;7:17387.
Karatas OH, Toy E. Three-dimensional imaging techniques: a literature review. Eur J Dent. 2014;8(1):132–40.
Link TM, Majumdar S, Lin JC, Newitt D, Augat P, Ouyang X, Mathur A, Genant HK. Comparative study of trabecular bone properties in the spine and femur using high resolution MRI and CT. J Bone Miner Res. 1998;13(1):122–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Orhan, K., Akat, B., Celikten, B. (2022). Micro-CT in Dentistry. In: Delantoni, A., Orhan, K. (eds) Atlas of Dentomaxillofacial Anatomical Imaging. Springer, Cham. https://doi.org/10.1007/978-3-030-96840-3_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-96840-3_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96839-7
Online ISBN: 978-3-030-96840-3
eBook Packages: MedicineMedicine (R0)