Abstract
Trauma and injuries represent a significant proportion of global mortality and continue to increase annually. Direct costs, such as medical and surgical interventions as well as indirect costs such as those of rehabilitation, missed work and mortality sum up the total economic burden of these injuries on society. Road traffic accidents remain to be a substantial cause of trauma in both developed and underdeveloped countries. Some studies suggest that despite sustained economic prosperity and improved healthcare, road traffic accidents continue to rise and cost nations as much as 3% of their gross domestic product annually. Along with other organizations, the World Health Organization has set out recommendations and proposed guidelines to improve road infrastructure, standardized vehicle safety regulations as well as speed regulations to combat the costs of these injuries. These preventative measures alongside preventative measures in the setting of osteoporosis have decreased the economic burden worldwide. Furthermore, the development and innovation of osteosynthesis over the last 60 years have decreased the economic costs on society and reduced the mortality associated with trauma and injuries.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Economic
- Cost of injury
- Road traffic accidents
- Mortality
- Trauma prevention
- Osteosynthesis
- fracture prevention
- trauma prevention
-
Understand the incidence and major causes of trauma and associated mortality.
-
Understand the direct and indirect costs of trauma on society.
-
Understand the utility and effectiveness of preventative measures in reducing the economic burden of trauma.
-
Understand and evaluate the disparity in road traffic safety across nations.
-
Understand the effectiveness of osteosynthesis in decreasing costs and mortality associated with trauma.
1 Introduction
Trauma and injuries are substantial causes of mortality and morbidity worldwide. It is estimated that over 5 million trauma related deaths occur on an annual basis [1, 2]. This represents 9.6% of global mortality and has been increasing over time [2]. The upward trend is largely attributed to a 46% increase in death due to road traffic trauma worldwide [2]. Alarmingly, despite their substantial economic burden, trauma accounts for 32% more deaths than tuberculosis, malaria, and HIV/AIDS combined (Fig. 2.1) [3]. Furthermore, trauma is the leading cause (40%) of death among young people (under 44 years of age) who often are economically essential members of society [4]. Furthermore, the Global Burden of Disease study group demonstrated that injuries account for 11.2% of disability adjusted life years (DALYs) worldwide [5]. Therefore, trauma and injuries are an economic burden due to healthcare expenditures as well as reduction in economic productivity of patients due to prolonged hospitalization, rehabilitation, disability and death [6].
2 Cost of Injury
The total economic burden placed on society by trauma can be divided into direct and indirect costs. Direct costs include health care expenses to the individual and health care system due to the traumatic events. Indirect costs include expenses related to the decline of productivity due to disability, rehabilitation, prolonged hospitalization and death. In Canada, the total cost of injury in 2010 was $26.8 billion with 59% calculated to be due to direct costs [6]. However, as indirect costs may be harder to estimate, it is possible this value could be even higher in reality. If current epidemiological trends continue, the Public Health Agency of Canada estimates that total costs related to trauma will rise by 180% in 2035 [6].
The distribution of direct costs to patients and the medical system vary from country to country due to public and private funding of medical care. Initial presentation to hospital usually activates a trauma team involving various physicians, nurses, social workers and coordinating staff. Often, medical or surgical interventions such as radiographic imaging, blood transfusions and utilization of operative and intensive care suites are required during the hospitalization period which include additional costs. Post hospitalization, costs of rehabilitation, prosthetics/aids, home care and medical prescriptions may also be endured. Data from the National Study on the Costs and Outcomes of Trauma of over 5000 moderate to severely injured patients who were treated and discharged from United States (US) hospitals was used to estimate overall treatment costs [7]. It was determined that the mean 1-year cost of trauma care per patient was $75,210 USD and about 58% of that cost was accrued during the initial hospitalization period [7]. Meanwhile, the estimated total direct annual treatment costs of US adult trauma was approximately $27 billion USD in 2005 [7]. These direct costs represent a significant financial burden to the healthcare system, the patient or private insurance depending on the method of funding.
Indirect costs of trauma care are much more difficult to quantify as they have variable and expansive effects for each individual. A nation’s economy can be severely affected when patients are unable to return to their pre-injury societal productivity. Studies have shown that only 60–66% of moderate to severely injured patients return to their full-time work duties [8, 9]. In the United States, an estimated $326 billion in loss of productivity costs occur annually due to trauma leading to missed work days [10]. Furthermore, costs incurred by patients with disabilities are severely underestimated in the literature as the loss of quality of life is a difficult intangible cost to quantify [11].
3 Implications of Economic Prosperity
Typically, economic improvements tend to lead to improvements of health indices within certain populations [12, 13]. Nonetheless, some studies have demonstrated an inverse relationship between injury rates and economic prosperity [12,13,14]. However, as road traffic trauma is one of the leading causes of injury, this may explain this effect. Despite conflicting literature, studies of developed countries indicate that sustained economic prosperity is associated with increased road traffic trauma, as more of the population would be able to afford to own and operate a motor vehicle [12, 13]. With regard to road traffic trauma, there has also been conflicting evidence regarding the association of increasing gasoline prices and rates of motor vehicle/motorcycle trauma [15, 16]. A Canadian study assessed the association of long-term economic prosperity and the resulting effect on trauma. Over a 16 year period of increasing mean annual gross domestic product (GDP), there was an increased risk of hospital admission due to trauma but no association was found with trauma mortality [14].
4 Prevention
Trauma can be divided into intentional and non-intentional injuries. Intentional injuries include those of self-inflicted harm, acts of violence towards self or others as well as combat related injuries. Non-intentional injuries such as falls, accidental fires, road traffic collisions and weather-related incidents tend to be more susceptible to preventative actions. Since trauma has significant costs to a country’s economy and expenses, many governments have placed substantial efforts in developing and implementing preventative measures to reduce incidence and resulting costs of trauma (i.e. United States has founded the United States National Center for Injury Prevention and Control). As countries look to cut costs on the medical expenses related to triaging and treating trauma, it has been suggested that resources would be better allocated with injury prevention as more than half of fatalities may have been prevented with better preventative measures prior to the injuries [17]. This is especially true in higher income countries where there are only marginal improvements in medical care systems compared to low to middle income countries [17]. The Children’s Safety Network, which is funded by the US Department of Health and Human Services, outlined a number of preventative measures (Table 2.1) and their associated societal cost savings in preventing trauma [18].
4.1 Road Traffic Injuries
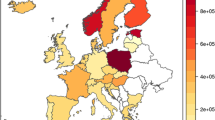
Along with over 5 million deaths, the WHO estimates over 20 million non-fatal injuries occur worldwide on annual basis due to road traffic injuries [3]. Furthermore, despite having only approximately 60% of the world’s motor vehicles, low and middle income countries account for 93% of road traffic fatalities [19]. Interestingly, even within countries of high income, those of lower socioeconomic status are more likely to be involved in road traffic trauma [3, 19]. These road traffic collisions can cost nations up to 3% of their GDP on an annual basis [19]. In 2017, the WHO created a report outlining worldwide recommendations of preventative actions against road traffic collisions that lead to trauma [20]. Their assessments focussed on improving speed regulation, infrastructure status and safety regulations.
Although the world’s fleet of motor vehicles is projected to double to over 2 billion by 2030, safety regulations across the world vary significantly and are non-existent in certain countries [21]. The United Nations (UN) World Forum for Harmonization of Vehicle Regulations is the group with the goal of unifying safety standards for all countries that include regulations on seat belts, frontal/side impact, child restraint anchorage points and pedestrian protection. A recent report indicated that over 40,000 fatalities, 400,000 severe injuries and $143 billion USD could be saved by 2030 in four Latin American countries if these regulations are abided by [22]. Furthermore, over 50% of roads assessed in 60 countries lacked basic infrastructure required for safe mobilization of pedestrians, cyclists and vehicle/motorcycle occupants. It was determined that merely improving the 10% highest risk roads in each of the 60 countries over the next 20 years would have the potential of preventing 3.6 million fatalities and over 40 million severe injuries [23].
4.2 Osteoporosis
Worldwide, one in three women and one in five men endure an osteoporotic fracture within their lifetime [24]. Hip fractures account for over half of osteoporotic fracture related costs as they are associated with a four-fold likelihood of requiring a long-term care facility posttreatment [25, 26]. This results in an expected annual direct cost of $25.3 billion USD by 2025 for the treatment of osteoporotic fractures in the US [27]. Overall, osteoporotic fractures result in direct medical costs as well as quality adjusted life years costs due to subsequent impairments. These include impairments to mobility, social wellbeing, physical function and quality of life [25].
In response to the increasing prevalence and economic burden of trauma with underlying osteoporosis, the American Society of Bone and Mineral Research and International Osteoporosis Foundation (IOC) have developed Fracture Liaison Services (FLS). These services are based on multidisciplinary care models that provide treatment and secondary prevention of osteoporotic injuries. They provide long-term monitoring, risk evaluation and fall prevention initiatives among many best practice guidelines developed [28]. These services have been extensively studied worldwide to assess their cost effectiveness across many settings. A recent systematic review demonstrated that FLS was cost effective in all countries studied (Australia, Canada, Japan, Sweden, Taiwan, United Kingdom and the United States of America) in comparison to standard of care or no treatment [29]. These programs also yielded cost savings in certain populations such as patients with prior hip fractures in the US. These savings were estimated to be $66,879 USD per lifetime/10,000 patients [25, 29]. Therefore, these economically and medically favourable services have demonstrated encouraging results and the IOC plans to further expand their implementation internationally.
5 Economical Impact of Osteosynthesis in Trauma Care
Prior to the visionary foundation of the Association of Osteosynthesis (AO) in 1958, the majority of fractures were treated conservatively in splints, casts and traction that resulted in significant immobilization for patients [30]. These Swiss founders established and popularized osteosynthesis for the treatment of long bone fractures to reduce hospital stay and time required until patients are able to return to work. It was only recently that studies evaluated the true economic impact of medical innovations in osteosynthesis. Eichler et al., performed a health economic evaluation of femur, tibia and radius fractures over a 60 year period (since the inception of AO) to estimate the health economic impact of innovations in osteosynthesis [31]. Within 17 high income countries, their modelling demonstrated total direct cost savings (Swiss Fracs) of $507 billion with tibia fractures, $272 billion with femur fractures, $69 billion with proximal femur fractures and $77 billion with radius fractures [31]. Furthermore, over 77.6 million years of life gained is estimated through the introduction of fracture osteosynthesis since its inception in 1958 to 2017 [31]. Despite limitations in the modelling design of the study, the impact of the AO founders’ innovation has not only yielded substantial improvements to the medical management of fracture care, but also staggering economic relief to nations worldwide. The example of osteosynthesis exemplifies the impact of medical innovation in reducing the economic burden due to trauma, and provides potential evidence that initially costly interventions may be more cost effective in the long term.
6 Conclusion
In conclusion, trauma and injuries are an immense economic burden on nations, healthcare providers and patients. This is due to healthcare expenditure and reduction in economic productivity of patients due to prolonged hospitalization, rehabilitation, disability and death. Numerous political and health organizations have set out initiatives to decrease this economic burden through innovation of healthcare delivery and products as well as preventative measures lowering the incidence of trauma.
Key Concepts and Take-Home Points
-
The total economic burden placed on society by trauma can be divided into direct and indirect costs. Direct costs include health care expenses to the individual and health care system due to the traumatic events. Indirect costs include expenses related to the decline of productivity due to disability, rehabilitation, prolonged hospitalization and death.
-
Road traffic collisions can cost nations up to 3% of their GDP on an annual basis.
-
Road traffic collisions are a major economic burden on all nations regardless of their economic prosperity and average socioeconomic status. Further improvements in road safety and regulations are needed to reduce these burdens.
-
Fracture Liaison Services are based on multidisciplinary care models that provide treatment and secondary prevention of osteoporotic injuries to decrease the potential economic burden of trauma.
-
The development and innovation of osteosynthesis over the past 60 years have substantially reduced the economic burden of trauma in terms of costs as well as mortality.
References
Kotagal M, Agarwal-Harding KJ, Mock C, Quansah R, Arreola-Risa C, Meara JG. Health and economic benefits of improved injury prevention and trauma care worldwide. PLoS One. 2014;9(3):e91862.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2095–128.
World Health Organization. Injuries and violence—the facts. Geneva; 2010.
Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374(9693):881–92.
Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223.
Parachute. The cost of injury in Canada; 2015. Available from: https://parachute.ca/en/professional-resource/cost-of-injury-report/.
Weir S, Salkever DS, Rivara FP, Jurkovich GJ, Nathens AB, Mackenzie EJ. One-year treatment costs of trauma care in the USA. Expert Rev Pharmacoecon Outcomes Res. 2010;10(2):187–97.
Holtslag HR, Post MW, van der Werken C, Lindeman E. Return to work after major trauma. Clin Rehabil. 2007;21(4):373–83.
Spreadborough S, Radford K, das Nair R, Brooks A, Duffy M. A study of outcomes of patients treated at a UK major trauma Centre for moderate or severe injuries one to three years after injury. Clin Rehabil. 2018;32(3):410–8.
Spicer R, Vallmuur K. Communicating consequences with costs: a commentary on Corso et al’s cost of injury. Inj Prev. 2015;21(6):432–3.
Haeusler JM, Tobler B, Arnet B, Huesler J, Zimmermann H. Pilot study on the comprehensive economic costs of major trauma: consequential costs are well in excess of medical costs. J Trauma. 2006;61(3):723–31.
Bishai D, Quresh A, James P, Ghaffar A. National road casualties and economic development. Health Econ. 2006;15(1):65–81.
van Beeck EF, Borsboom GJ, Mackenbach JP. Economic development and traffic accident mortality in the industrialized world, 1962–1990. Int J Epidemiol. 2000;29(3):503–9.
Roberts DJ, Das D, Mercado M, Vis C, Kortbeek JB, Kirkpatrick AW, et al. A booming economy means a bursting trauma system: association between hospital admission for major injury and indicators of economic activity in a large Canadian health region. Am J Surg. 2014;207(5):653–7; discussion 7–8.
Hyatt E, Griffin R, Rue LW 3rd, McGwin G Jr. The association between price of regular-grade gasoline and injury and mortality rates among occupants involved in motorcycle- and automobile-related motor vehicle collisions. Accid Anal Prev. 2009;41(5):1075–9.
Leigh JP, Geraghty EM. High gasoline prices and mortality from motor vehicle crashes and air pollution. J Occup Environ Med. 2008;50(3):249–54.
Stewart RM, Myers JG, Dent DL, Ermis P, Gray GA, Villarreal R, et al. Seven hundred fifty-three consecutive deaths in a level I trauma center: the argument for injury prevention. J Trauma. 2003;54(1):66–70; discussion -1.
Network CsS. A summary of cost outcome analysis for injury prevention programs; 2014.
World Health Organization. Road traffic injuries; 2020.
World Health Organization. Save Lives—a road safety technical package; 2017.
World Health Organization. Global status report on road safety; 2015.
Wallbank C, McRae-McKee K. The potential for vehicle safety standards to prevent deaths and injuries in Latin America. An assessment of the societal and economic impact of inaction; 2016.
World Road Association. Road safety manual: a manual for practitioners and decision makers on implementing safe system infrastructure; 2015.
Recker R, Lappe J, Davies KM, Heaney R. Bone remodeling increases substantially in the years after menopause and remains increased in older osteoporosis patients. J Bone Miner Res. 2004;19(10):1628–33.
Kanis JA, Borgström F, Compston J, Dreinhöfer K, Nolte E, Jonsson L, et al. SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos. 2013;8(1):144.
Tajeu GS, Delzell E, Smith W, Arora T, Curtis JR, Saag KG, et al. Death, debility, and destitution following hip fracture. J Gerontol A Biol Sci Med Sci. 2014;69(3):346–53.
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–75.
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, et al. Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24(8):2135–52.
Wu CH, Kao IJ, Hung WC, Lin SC, Liu HC, Hsieh MH, et al. Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int. 2018;29(6):1227–42.
Schlich T. Surgery, science and industry: a revolution in fracture care, 1950s–1990s. Palgrave Macmillan; 2002.
Eichler K, Höglinger M, Meier F, Knöfler F, Scholz-Odermatt SM, Brügger U, et al. Impact of osteosynthesis in fracture care: a cost comparison study. J Compar Effectiveness Research. 2020;9(7):483–96.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Atwan, Y., Schemitsch, E.H. (2022). Economic Aspects of Trauma Care. In: Pape, HC., Borrelli Jr., J., Moore, E.E., Pfeifer, R., Stahel, P.F. (eds) Textbook of Polytrauma Management . Springer, Cham. https://doi.org/10.1007/978-3-030-95906-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-95906-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95905-0
Online ISBN: 978-3-030-95906-7
eBook Packages: MedicineMedicine (R0)