Abstract
The aim to minimize mortality rates in polytrauma led to numerous investigations, calculations, and scoring systems to describe the individual patient risk. Patients react differently to the same injury. This reaction depends on the physiologic state, comorbidities, age, and numerous other factors. Several scoring systems aim to quantify the injury severity, the trauma load, and the physiologic response. In general, these scoring systems focus either on anatomic injury distribution, physiologic parameter, radiologic measures, or on any combination of the above. Some scores developed treatment recommendations, other sever for research purposes only. This chapter offers a detailed summary of definitions and scores in the initial assessment of polytrauma patients. It aims to highlighting strengths and limitations and discusses the complexity of defining polytrauma.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Polytrauma
- Severely Injured
- Score
- Definition
- Polytrauma Score
- Damage Control
- Safe definitive surgery
- Treatment recommendation
- Multiple injury
-
AIS, ISS, and NISS are anatomic scoring systems describing the injury distribution
-
Pathophysiologic-based scoring systems increase prediction of mortality at the cost of feasibility
-
Clinical scoring systems are intuitive at the cost of predictive capability
-
Polytrauma is more than the summary of injuries
-
Several different pathophysiological pathways should be taken into consideration during the initial assessment of polytrauma patient
1 Introduction
Treatment of polytrauma patients is complex and requires multidisciplinary approach [1,2,3,4]. Numerous studies investigate the treatment of polytrauma patient with the main goal to improve outcome and to minimize mortality rate. However, the main challenge that had to be overcome was the heterogeneity of polytrauma patients: injury distribution, pathophysiologic responses, and trauma systems. The Association for the Advancement of Automotive Medicine (AAAM) aimed to standardize the heterogeneity of anatomic injuries in polytrauma patients. Evaluating motor vehicle accidents, the AAAM established the Abbreviated Injury Scale (AIS). The AIS categorizes injury severity of each body region scaling from “0” (none) to “6” (not survivable). In 1974, Baker utilized the AUS to further calculate the Injury Severity Score (ISS) [5]. Osler presented a modification of the ISS, the new ISS (NISS) with slight modification of the ISS formula [6]. In the 1980s Advanced Trauma Life Support principles were developed aiming to minimize resources of trauma centers while standardizing the treatment of the severely injured patient [7,8,9]. Another 10 years later, in the 1990, Tscherne focused that the pathophysiologic response to trauma has a pivotal role and determines the outcome and mortality [10, 11]. These three concepts of defining and scoring a polytrauma patient define the treatment strategy and depend on individual situation:
-
1.
The anatomic injury distribution and injury severity
-
2.
The pathophysiologic response to trauma
-
3.
Logistics of trauma center
This chapter presents these most commonly used scoring systems, discusses advantages and disadvantages, and aims to summarize important key points in the initial assessment of polytrauma patients.
2 Anatomically Based Scoring Systems
2.1 Abbreviated Injury Scale (AIS)
The AIS is an anatomically based, consensus derived, scoring system that classifies individual injuries by body region. Each injury is grading according to severity and according to body region (Table 13.1). The AIS is not suitable for a prognostic evaluation of injuries but rather build the basis of calculating the ISS. Since the first publication the AIS is subject to constant improvements and updates [12,13,14]. After stratification according to the AIS, injuries are categorized as discrete variable: Injuries stratified as AIS 1 are not lethal, whereas stratification as AIS 6 is not survivable [13]. While categorizing single injuries according to the AIS body regions, the following points need to be taken into consideration:
-
AIS region “head” describes anatomic injuries of the neuro-cranium and the organs
-
AIS region “face” includes injuries to the viscero-cranium (facial bone)
-
Fractures of the orbita account to AIS region “head”
-
Injuries to the cervical spine account to AIS region “head”
-
Injuries to the thoracic spine account to AIS region “thorax”
-
Injuries to the lumbar spine account to AIS region “abdomen”
The categorization of isolated injuries is one initial assessment step of polytrauma patients. The AIS does not reflect the global injury severity nor has the AIS predictive capabilities, since the correlation of AIS scoring and mortality is not linear [15]. Following the suggestions of AIS 1980, a description of injury severity with the use of maximum AIS (MAIS) is possible [13]. The overall AIS is a remnant that should not be used based on missing objectivity and misinterpretation since the revision of 1980 [13].
2.2 Injury Severity Score (ISS)
Baker proposed a calculation to describe the anatomic injury severity that is based on the AIS [16]. This calculation aims to describe the total injury severity. The highest AIS of each of the six body regions is eligible for inclusion for calculating the ISS. The ISS is the sum of the square of the three most severely injured body regions:
It is important to recognize that the calculation of the ISS only includes one AIS per body region and a total of maximal three body regions. The ISS ranges from 1 point to 75 points. Of note, if any body region reaches 6 points on the AIS, the ISS is per definition 75.
The fact that only one AIS per body region, and maximum three body regions are taken into consideration, is one major drawback of the ISS. This might lead to underestimation of the injury severity [17]. This fact led to development of the NISS.
2.3 New Injury Severity Score (NISS)
Osler proposed the NISS in 1997 to address issues of underrepresentation of multiple extremity injury [6]. The calculation of the NISS is comparable to the ISS. The main difference is the inclusion of the three highest AIS independent of body region. This allows a multiple injured body region to contribute to the NISS. This might lead to an increase of total injury severity [12]. As a result, the NISS presents with higher sensitivity and specificity for predicting mortality compared with the ISS [18].
The ISS as well as the NISS is based on the classification of injuries according to AIS. This, however, lacks subjectivity and reproducibility [19, 20]. As a result, this leads to a wide observer variation that highlights a potential fallibility [21]. These mere anatomic based scoring systems represent an observation of acute injuries that miss individual pathophysiological reactions that base amongst others on age [22].
3 Pre-Hospital Scoring Systems
3.1 Revised Trauma Score (RTS)
Based on data from the Major Trauma Outcome Study (MOTS), Champion proposed the RTS that is one widely used pathophysiologic-based trauma score [23, 24]. The RTS includes three physiologic parameter including the vigilance, measured by the Glasgow coma scale (GSC) [25], the systolic blood pressure (RRsys), and the respiratory rate. Initially “capillary reperfusion” and “respiratory working load” were included in the RTS, measures that were omitted due to impracticability [26]. To calculate the RTS the following two steps are necessary:
-
1.
Coding each variable according the RTS value (Table 13.2)
-
2.
Weighing each RTS value with the following coefficient:
It is eminent that the RTS weighs the GCS highest, followed by the systolic blood pressure and the respiratory rate. According to the RTS the vigilance has the highest predictive value for mortality. The RTS ranges from 0 (death) to 78,408 (healthy). Further, a value of less than 4 points recommends a triage to a Level 1 trauma center [15]. The inclusion of the RTS into a logistic function calculates the direct survival probability [18]:
Despite its potential for triage recommendations the RTS is not well established in preclinical situation based on impracticability [15]. Further, the score calculation is based on values only in spontaneous breathing patient, not with values of patients under analog-sedation and intubation. Despite these limitations, the RTS’s capability of predicting mortality made it an essential part of the TRISS.
Evidence for use of the RTS is discussed in the literature, but there still is a lack of definitive evidence supporting its use as a primary triage tool and as a predictor of outcomes other than mortality [27]. Further, advancements of treatment strategies and polytrauma management led to a substantial decrease of mortality [4, 28, 29]. The calculated mortality rate based on the RTS is static and not adjustable to advancements of medical treatment. The RTS might therefore lead to an overestimation of mortality.
3.2 Trauma and Injury Severity Score (TRISS)
TRISS is one example of scoring system that combine the anatomic injury severity with pathophysiologic reactions. Boyd utilized the databank of Major Trauma Outcome Study (MTOS) to develop the TRISS [30]. In the TRISS, ISS represents injury severity and RTS the pathophysiologic changes. Further, TRISS differentiates blunt from penetrating trauma. TRISS calculations include coefficients that for RTS, ISS, age (≥55a), and a constant variable; the coefficients depend on the trauma mechanism (blunt versus penetrating) (Table 13.3).
In pediatric trauma, TRISS does not differentiate between blunt and penetrating trauma; the calculation of blunt trauma is used. If patients are under the age of 55 years, the age coefficient is set 0. TRISS values range from 0 to 1 and indicate the survival probability after trauma. Despite the incorporation of ISS and RTS, with the previously described limitations, the validated TRISS still presents limitations in case of multiple injuries of one body region or in cases of severe traumatic brain injury (TBI) [31].
3.3 Revised Injury Severity Classification RISC
RISC is a calculation based on the German Trauma registry [32]. The anatomic injury severity is based on NISS, AIS head, AIS extremity, and GCS. Physiologic parameters include partial thromboplastin time (PTT, sec.), base deficit (BE, mmol/L), RRsys below 90 mmHg, hemoglobin below 9 mg/dL, requirement of more than 9 packed red blood cells (pRBCs), as well as cardiopulmonary resuscitation (CPR) (Table 13.4). The coefficients are summarized and subtracted form 5. The resulting value Y is used for the calculation of the survival probability:
Comparing to the area under the curve (AUC) under the receiver operating curve (ROC) of TRISS (0.874), NISS (0.793), or ISS (0.777), the RISC presents with the highest AUC of 0.912 in the dataset of the German trauma registry. However, the RISC was developed based and validated on the dataset and needs validation in an external dataset or a prospective study. RISC based on calculation of data that were collected between 1993 and 2000 [33] leading to an overestimation of mortality rate. The update of RISC is based on calculations of data of the German trauma registry between 2010 and 2011 and led to the development of RISC II [33]; the internal validation is based on data collected in 2012. The following points were updated:
-
NISS was replaced by the highest two AIS
-
Gender is included in calculations
-
American Society of Anesthesiologists Score (ASA) is included
-
Injury mechanism is included
-
Pupil status is included
An external validation or a clinical study assessing predictive capability of the RISC II score would proof the value of RISC II and show potential limitations others than the included measures provide.
3.4 The AdHOC Score
The AdHOC score includes age, severity of head injury, oxygenation with acid-base parameter, and parameters of circulation [34]. It was developed on the data provided by the German trauma registry (TraumaRegistzerDGU®) and included patients ages 16 years and older, ISS of 9 points and higher that were admitted between 2012 and 2015 (development set). A dataset from patients admitted in 2016 served as an internal validation set. The AdHOC score provides a flow chart that assess whether any pathologic finding of the respected field (age, head injury, oxygenation, circulation) is present. Pathologic finding was defined as exceeding a predefined threshold. Thus, the patient might receive one point per field and a maximum of 4 points. The area under the receiver operating curve (AUROC) of the AdHOC score was 0.86 (95%CI 0.85–0.87) for the endpoint mortality. The thresholds and parameter are summarized in Table 13.5.
4 In-Hospital Scoring Systems
4.1 Early Appropriate Care (EAC) Protocol
The EAC protocol stratifies patients into low and high risk [35]. EAC recommends definitive surgery in patients stratified as low risk. THE EAC protocol is based on three measurements, all of which represent values of acid-base pathway: pH, BE, lactate. Patients with a pH of 7.25 or higher, BE of 5.5 and higher or lactate values below 4.0 are stratified as low risk. An external validation of this protocol revealed that patients stratified as high risk have significantly higher rate of early death and hemorrhagic shock, but the rate of patients who developed late in-hospital complications (e.g., pneumonia, sepsis, or multiple organ failure) did not differ among these groups [36].
4.2 Clinical Grading Scale (CGS)
The clinical grading system represents a summary of multiple publications and lists parameters indicative of four different pathophysiologic pathways [37]. Its level of evidence is based on expert knowledge (level IV) and has not been validated in a database. All recommendations rely on studies prior to 2005. The CGS aims to grade the polytrauma patients according to the condition into “stable,” “borderline,” “unstable,” and “in extremis.” This categorization based on the following pathophysiologic pathways: shock, coagulation, temperature, and soft tissue injuries. Based on the categorization of the polytrauma patient, a treatment recommendation is provided: early total care (ETC) in stable, or stable borderline patients, damage control orthopedic (DCO) in unstable or in extremis cases. Each pathophysiologic pathway is graded according to the highest grade per measure; the mean of all grades defines the patient’s condition.
4.3 Polytrauma Grading Score (PTGS)
The PTGS is based on calculation of the nation-wide German trauma registry [38]. It is based on in-hospital mortality rate. The score is based on blood pressure, BE, INR, NISS, pRBCs, and platelets. According to the measured value each measurement receives a score (Table 13.5). The sum of these scores defines the PTGS. Based on mortality rate, PTGS 0–5 indicate a stable condition, 6–11 a borderline condition, 12–20 and unstable condition, and 20 and higher points an “in extremis” condition.
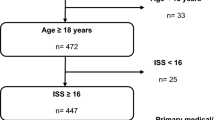
CGS, EAC, and PTGS have not been validated in a high quality prospective clinical study. The limitations and strengths have been presented based on validation on an external polytrauma dataset from one Level 1 trauma center [36]. Halvachizadeh demonstrated that the predictive capability of scoring systems (including mortality and in-hospital complications) increases when measures of several different pathophysiological pathways are included: shock, acid-base, coagulopathy, soft tissue injury, and anatomic injury severity. Figure 13.1 summarizes and compares scoring systems.
5 Summary of Scoring Systems
5.1 Pre-Hospital Scoring Systems
The Revised Trauma Score (RTS) is based on the degree of traumatic brain injury, as defined by the Glasgow Coma Scale (GCS) [25], blood pressure, and respiratory rate. Following the Major Trauma Outcome Study (MOTS), Boyed published the Trauma and Injury Severity Score (TRISS) aiming to combine anatomic injuries and physiologic responses after polytrauma [30]. The revised injury severity classification (RISC) [32] and the RISC II [39] are based on statistical analysis of a nation-wide trauma database. The AdHOC score aims to facilitate classification of trauma patients by summarizing pathologic finding of four pathophysiologic systems [34]. Further several scoring systems have been proposed that aim to provide treatment guideline.
5.2 In-Hospital Scoring Systems
The clinical grading score (CGS) aims to guide treatment strategies (damage control orthopedics, DCO versus safe definitive surgery, SDS) [37]. The early appropriate care (EAC) protocol bases definitive operability on lactate values [35]. Finally, the polytrauma grading score (PTGS) stratifies the stability of polytrauma patients based on mortality risk [38]. Roberts defined indications for damage control based on a scoping review and expert opinions [40]. These scoring systems are summarized in Table13.6.
6 Conclusion
The use of a combination of anatomic variables and variables from several pathophysiologic pathways is more precise in both defining the current state of polytrauma patients and in predicting the probability of developing complications. The assessment of polytrauma patients should be based on various factors rather than on one isolated aspect. Initial management of polytrauma patients ranges from damage control strategies to safe definitive surgery [2]. Several factors influence the decision-making including patient specific factors (age, comorbidities, physiologic status), and multiple disciplines (general surgeon, anesthesiologists, intensivists, orthopedic surgeon) [41, 42]. Based on several attempts to quantify injury severity and pathophysiologic responses it becomes eminent that scoring and defining polytrauma while giving treatment recommendations are challenging. The inclusion of several pathophysiologic pathways increases predictability for mortality and complication [36] that, however, increases complexity and decreases applicability in routine clinical practice. Observational injury descriptions are subject to high inter-, and intraobserver variability [16]. Statistical based calculations lead to complex and impractical scoring systems that include un-intuitive calculations [32, 39]. Clinical based scoring system is intuitive at the cost of decreased predictability of complications [36]. These limitations lead to an increasing number of literature investigating expert opinions on treatment strategies. Roberts summarized clinical and pathophysiological measured that lead to the recommendation of damage control surgery in polytrauma [43]. These measures include:
-
Injury patterns
-
Bleeding control
-
Amount of resuscitation provided
-
Degree of physiologic insult
-
Need for staged abdominal or thoracic wall reconstruction
The comprehensive list of measures indicative for damage control surgery is based on an expert panel and is peer reviewed. Yet, the indications represent extreme situations that are comparable to unstable or in extremis situations [36]. There still is a lack of high quality research providing measures indicative for safe definitive surgery in polytrauma patients. The outcome of polytrauma patients depends on comprehensive but precise diagnostic [44, 45] and on medical and surgical expertise. The clinical approach towards a polytrauma patient is based on the assessment of the severity of the polytrauma patient. The treating trauma team recognizes patient as a “polytrauma patient” and defines the next appropriate steps based on the clinical stability of the patient [2, 46,47,48]. In research, the precise definition of a polytrauma is essential to improve comparability and medical progress in this very heterogenic study-population (Fig. 13.2).
References
Pape HC, Champion HR. Patient assessment in polytrauma: current trends rely on multiple parameters to improve the prediction of complications and mortality. Injury. 2015;46(10):1875–7.
Pape HC, Halvachizadeh S, Leenen L, Velmahos GD, Buckley R, Giannoudis PV. Timing of major fracture care in polytrauma patients—an update on principles, parameters and strategies for 2020. Injury. 2019;50(10):1656–70.
Kaserer A, Casutt M, Sprengel K, Seifert B, Spahn DR, Stein P. Comparison of two different coagulation algorithms on the use of allogenic blood products and coagulation factors in severely injured trauma patients: a retrospective, multicentre, observational study. Scand J Trauma Resusc Emerg Med. 2018;26:9.
Stein P, Kaserer A, Sprengel K, Wanner GA, Seifert B, Theusinger OM, et al. Change of transfusion and treatment paradigm in major trauma patients. Anaesthesia. 2017;72(11):1317–26.
Baker SP, Oneill B, Haddon W, Long WB. Injury severity score—method for describing patients with multiple injuries and evaluating emergency care. J Trauma Injury Infect Crit Care. 1974;14(3):187–96.
Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma Injury Infect Crit Care. 1997;43(6):922–5.
Subcommittee A, American College of Surgeons’ Committee on T, International Awg. Advanced trauma life support (ATLS(R)): the ninth edition. J Trauma Acute Care Surg. 2013;74(5):1363–6.
Jayaraman S, Sethi D. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev. 2009;2:17.
First International Conference on Emergency Medicine. London, England, 14–18 April 1986. Abstracts. Arch Emerg Med. 1986;3(1):31–92.
Tscherne H. Unfallchirurgie. Tscherne H, Regel G. Trauma-Management. Berlin: Springer; 1997.
Tscherne H, Regel G. Tscherne Unfallchirurgie: trauma-management. Springer-Verlag; 2013.
Kulla M, Fischer S, Helm M, Lampl L. How to assess the severity of the multi-system trauma in the emergency-room—a critical review. Anasthesiol Intensivmed NotfMed Schmerzther. 2005;40(12):726–36.
Haasper C, Junge M, Ernstberger A, Brehme H, Hannawald L, Langer C, et al. The abbreviated injury scale (AIS). Unfallchirurg. 2010;113(5):366–72.
Palmer CS, Franklyn M, Niggemeyer LE. Abbreviated Injury Scale mapping between 1998 and 2008 versions: multiple maps, but no destination yet. J Trauma Acute Care Surg. 2012;73(4):1032.
Chawda MN, Hildebrand F, Pape HC, Giannoudis PV. Predicting outcome after multiple trauma: which scoring system? Injury. 2004;35(4):347–58.
Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Schroter C, Urbanek F, Fromke C, Winkelmann M, Mommsen P, Krettek C, et al. Injury severity in polytrauma patients is underestimated using the injury severity score: a single-center correlation study in air rescue. Eur J Trauma Emerg Surg. 2019;45(1):83–9.
Lefering R. Trauma score systems for quality assessment. Eur J Trauma. 2002;28(2):52–63.
Butcher NE, Enninghorst N, Sisak K, Balogh ZJ. The definition of polytrauma: variable interrater versus intrarater agreement—a prospective international study among trauma surgeons. J Trauma Acute Care Surg. 2013;74(3):884–9.
Maduz R, Kugelmeier P, Meili S, Döring R, Meier C, Wahl P. Major influence of interobserver reliability on polytrauma identification with the Injury Severity Score (ISS): Time for a centralised coding in trauma registries? Injury. 2017;48(4):885–9.
Zoltie N, Dedombal FT. The hit and miss of iss and triss. BMJ. 1993;307(6909):906–9.
Fatovich DM, Jacobs IG, Langford SA, Phillips M. The effect of age, severity, and mechanism of injury on risk of death from major trauma in Western Australia. J Trauma Acute Care Surg. 2013;74(2):647–51.
Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ. Trauma score. Crit Care Med. 1981;9(9):672–6.
Champion HR. Trauma score as a measure of physiological derangement after injury. Crit Care Med. 1982;10(6):420.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;304(7872):81–4.
Champion HR, Sacco WJ, Copes W. Simplification of the trauma score. J Trauma Injury Infect Crit Care. 1985;25(7):680.
Gabbe BJ, Cameron PA, Finch CF. Is the revised trauma score still useful? ANZ J Surg. 2003;73(11):944–8.
Long B, April MD, Summers S, Koyfman A. Whole body CT versus selective radiological imaging strategy in trauma: an evidence-based clinical review. Am J Emerg Med. 2017;35(9):1356–62.
Roberts DJ, Ball CG, Feliciano DV, Moore EE, Ivatury RR, Lucas CE, et al. History of the innovation of damage control for management of trauma patients: 1902–2016. Ann Surg. 2017;265(5):1034–44.
Boyd CR, Tolson MA, Copes WS. Evaluating trauma care—the triss method. J Trauma Injury Infect Crit Care. 1987;27(4):370–8.
Eichelberger MR, Bowman LM, Sacco WJ, Mangubat EA, Lowenstein AD, Gotschall CS. Trauma score versus revised trauma score in TRISS to predict outcome in children with blunt trauma. Ann Emerg Med. 1989;18(9):939–42.
Lefering R. Development and validation of the revised injury severity classification score for severely injured patients. Eur J Trauma Emerg Surg. 2009;35(5):437–47.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGU (TM): the Revised Injury Severity Classification, version II. Crit Care. 2014;18(5)
Knoepfel A, Pfeifer R, Lefering R, Pape HC. The AdHOC (age, head injury, oxygenation, circulation) score: a simple assessment tool for early assessment of severely injured patients with major fractures. Eur J Trauma Emerg Surg. 2020;48:411–21.
Nahm NJ, Moore TA, Vallier HA. Use of two grading systems in determining risks associated with timing of fracture fixation. J Trauma Acute Care Surg. 2014;77(2):268–79.
Halvachizadeh S, Baradaran L, Cinelli P, Pfeifer R, Sprengel K, Pape HC. How to detect a polytrauma patient at risk of complications: a validation and database analysis of four published scales. PLoS One. 2020;15(1):e0228082.
Pape HC, Giannoudis PV, Krettek C, Trentz O. Timing of fixation of major fractures in blunt polytrauma: role of conventional indicators in clinical decision making. J Orthop Trauma. 2005;19(8):551–62.
Hildebrand F, Lefering R, Andruszkow H, Zelle BA, Barkatali BM, Pape HC. Development of a scoring system based on conventional parameters to assess polytrauma patients: PolyTrauma Grading Score (PTGS). Injury. 2015;46(Suppl 4):S93–8.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGU™: the Revised Injury Severity Classification, version II. Crit Care. 2014;18(5):476.
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, et al. Indications for use of damage control surgery and damage control interventions in civilian trauma patients: a scoping review. J Trauma Acute Care Surg. 2015;78(6):1187–96.
von Ruden C, Buhren V, Perl M. Polytrauma management—treatment of severely injured patients in ER and OR. Z Orthop Unfallchir. 2017;155(5):603–22.
Pfeifer R, Heussen N, Michalewicz E, Hilgers R-D, Pape H-C. Incidence of adult respiratory distress syndrome in trauma patients: a systematic review and meta-analysis over a period of three decades. J Trauma Acute Care Surg. 2017;83(3):496–506.
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, et al. Indications for use of damage control surgery in civilian trauma patients: a content analysis and expert appropriateness rating study. Ann Surg. 2016;263(5):1018–27.
Huber-Wagner S, Lefering R, Qvick LM, Korner M, Kay MV, Pfeifer KJ, et al. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009;373(9673):1455–61.
Huber-Wagner S, Kanz KG, Hanschen M, van Griensven M, Biberthaler P, Lefering R. Whole-body computed tomography in severely injured patients. Curr Opin Crit Care. 2018;24(1):55–61.
Giannoudis PV. Surgical priorities in damage control in polytrauma. J Bone Joint Surg Br. 2003;85B(4):478–83.
Pape HC, Hildebrand F, Pertschy S, Zelle B, Garapati R, Grimme K, et al. Changes in the management of femoral shaft fractures in polytrauma patients: from early total care to damage control orthopedic surgery. J Trauma Injury Infect Crit Care. 2002;53(3):452–61.
Pape HC, Giannoudis P, Krettek C. The timing of fracture treatment in polytrauma patients: relevance of damage control orthopedic surgery. Am J Surg. 2002;183(6):622–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Halvachizadeh, S., Pape, HC. (2022). Polytrauma Scoring. In: Pape, HC., Borrelli Jr., J., Moore, E.E., Pfeifer, R., Stahel, P.F. (eds) Textbook of Polytrauma Management . Springer, Cham. https://doi.org/10.1007/978-3-030-95906-7_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-95906-7_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95905-0
Online ISBN: 978-3-030-95906-7
eBook Packages: MedicineMedicine (R0)