Abstract
The introduction in the common practice of classification systems and the advent of new surgical technologies, greatly improved the outcome of patients affected by sub axial cervical spine injury although the standardization and uniformity in approaching the traumatized patient is still lacking. The ideal classification should be accurate in establishing the severity of the lesion, useful to guide the indication for treatment, but reliable and reproducible yet. Among the different classifications Allen and Ferguson, SLIC and AO are the most used worldwide. Allen and Ferguson is based on the presumed mechanism of injury, and, Although very old and based on x-ray only, it is surprisingly largely used still to date. AO is a morphological classification whose main objective is to provide users with a reliable and valid system that is highly reproducible in estimating the severity of the lesion. SLIC was the first to introduce a scoring system with the intent to guide the decision-making process. Due to the lack of guidelines, widely shared in the scientific community, the treatment of sub axial cervical spine injuries is based much more on individual surgeon experience and preference rather than on objective and reproducible treatment algorithms. What emerges from both the analysis of the literature and our experience is that there is not only valid surgery in all situations. Given the complexity of the injuries, individual cases must be well evaluated for the best solution.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Spinal cord injury
- Surgical treatment of cervical spine fractures
- Classification system of cervical spine fracture
Introduction
Epidemiology
Subaxial Cervical spine fractures and dislocations represent rare events accounting for approximately 7% of traumatic cervical injuries but often result in significant morbidity and death [1].
The mortality for patients with traumatic spinal cord injury (SCI) is markedly high, with rates ranging from 4 to 16.2% and 21.7 to 32.3% within 30 days and 1 year from admission respectively [2, 3].
The total frequency of SCI is estimated from 27 to 47 per million in the entire population and approximately 6% in polytraumatized patients; about 40% of patients may present some degree of neurological deficit due to spinal cord or nerve root injury [4]. In the literature a lower mortality was reported for surgically treated patients respect those conservatively treated [5].
There is generally a higher prevalence of cervical fracture among males, and significant predictors of cervical fracture seems to be: pelvic fracture, pelvic fracture combined with a fall and/or concurrent head injury, injury severity score >15, and age over 40 years [6, 7]. The main injury mechanism reported was a motor vehicle accident (MVA) followed by falls from height. Wang et al. [8] reported the most common mechanisms to be MVA in 33.1%, falls in 50.6%, and sports in 0.8%. Young et al. [4] sustained MVA, falls, motorcycle, bicycle, and pedestrian accidents as significant independent predictors of cervical spine injury and fractures.
Despite the overall low incidence of severe subaxial cervical fractures-dislocations, the correct classification and treatment of these patients still represents a topic of debate in literature. Therefore, the purpose of this chapter is to discuss the role of classifications to offer an easy and reliable method to establish the severity of injuries, and thereafter, to assist spinal surgeons in a correct treatment planning (conservative and/or surgical).
Classification Systems
Care protocols for polytraumatized patients (Prehospital Trauma Life Support and Advanced Trauma Life Support) that recommend maintaining a cervical collar until the presence of cervical injuries can be excluded, have been revealed strategically to reduce the incidence of complications after cervical injuries.
A correct injury pattern identification and classification could play a crucial role on the traumatized patient’s outcome. However, a proper evaluation, especially in a minor and peripheral hospital, is not always possible often due to poor equipment and the lack of a spinal surgeon available. In this scenario, an ideal classification system should be simple and reproducible, and able to transmit comprehensive information about diagnosis, prognosis and clinical/surgical management. Besides, it must allow the practitioners (often from different hospitals) involved in the multidisciplinary treatment of a polytrauma patient to speak a common language [9, 10].
Despite many systems were proposed to classify subaxial cervical spine trauma based on different criteria (morphological and/or pathogenic) [11, 12] to date, none of the classification was universally accepted; furthermore, many studies in the literature revealed the variability in severity assessment and management of traumatic spine injuries [13].
In the last decades, Magerl’s classification was most often used [14]. This classification exploded in a dizzying international success in the late 1990s, and rapidly replaced the older classification of Allen-Ferguson (AF) [15].
The most common classifications currently used are:
-
the Sub-axial Injury Classification (SLIC) and Severity Scale.
-
the AOSpine Subaxial Cervical Spine Injury classification system that represents, an upgrade of Magerl’s classification based on quite similar morphological features [16, 17].
Allen and Ferguson Classification
Firstly, published in 1982, Allen and colleagues devised a cervical spine injury classification system based on the traumatic mechanism they called mechanistic classification. The authors described six common patterns of indirect injury to the lower cervical spine, named phylogenies, based on radiographic pictures and supposedly involved traumatic forces (flexion/extension/compression/distraction). Each phylogeny was named according to the presumed attitude of the cervical spine at the time of failure and the initial, dominant mode of failure. Compressive flexion, vertical compression, distractive flexion, compressive extension, distractive extension and lateral flexion were the six phylogenies identified (Fig. 11.1).
Each pattern could be divided into stages according to the severity of musculoskeletal damage. A close correlation appeared to exist between the neurologic and musculoskeletal injury in each pattern [18].
The authors also point out that ligament injuries cannot always be evaluated with standard radiological examinations. However, such injuries can be indirectly detected by residual spinal displacement. In most cases the ligaments are injured by tension and/or shear forces but hardly by those in compression [19,20,21,22,23].
Among the various factors to be evaluated in case of cervical spine trauma, there were: residual malalignment and presence of neurologic injury. In contrast to instability, which indicates abnormal movement, malalignment implies a fixed abnormal relationship.
Another novelty introduced by this classification unlike the previous ones, in which it was argued that there was no strict correlation between the type of fracture and neurological injury [24]. Allen and his colleagues claim that higher stages are reflective of a more severe injury to the spine and predictably show a more severe cord involvement.
Magerl’s Classification
Unlike the previous one, Magerl’s classification was based on injury pathomorphological characteristics. Categories were settled according to the main mechanism of injury pathomorphological uniformity, and in consideration of prognostic aspects regarding healing potential.
The three main categories have a typical fundamental injury pattern defined by a few easily recognizable radiological criteria [14].
Emphasis was placed on the extent of the anterior and posterior elements involvement, with particular attention to soft-tissue injury, as well as ancillary bony lesions. Analysis of the injury pattern provides information on the pathomechanics of the injury and, at least, regarding the main mechanisms. In this classification, the loss of stability represents the key point for injuries classification, and the choice of treatment depends on it. The risk of neural injury seems to be primarily linked to the degree of mechanical instability. The dichotomous division between disco-ligamentous injuries and osseous lesions was set due to important prognostic and treatment differences in the two lesions. Because disco-ligamentous injuries had a poor healing potential, surgical stabilization and tension should be considered to avoid chronic instability [25].
The three main types of injuries are type A injuries, primarily caused by compression, type B by tension, and type C by axial torque corresponding to an increasing degree of injury instability. Thus, the severity of the injuries in terms of instability is expressed by its ranking within this classification system.
Subaxial Injury Classification (SLIC)
In 2007 a novel classification was published with the purpose to establish a system easy to remember and to apply in clinical practice guiding treatment decision-making in an objective and systematic manner.
Three main categories (injury morphology; disco-ligamentous complex integrity; and neurological status) were identified as important to injury description and a score were assigned according to the overall injury severity. Treatment options were assigned based upon threshold values of the severity score.
Three major injury characteristics were identified:
-
1.
injury morphology as determined by the pattern of spinal column disruption on available imaging studies.
-
2.
integrity of the disco-ligamentous complex (DLC) represented by both anterior and posterior ligamentous structures as well as the intervertebral disc.
-
3.
neurologic status of the patient.
Within each of the three categories, subgroups were identified and graded from the least to the most severe.
This is done according to the following categories:
-
1.
Spinal level,
-
2.
Injury level morphology,
-
3.
Bony injury description,
-
4.
Status of DLC with descriptors, i.e., presence of a herniated nucleus pulposus,
-
5.
Neurology,
-
6.
Confounders.
Bony injury descriptors include fractures or dislocations of the following elements: transverse process, pedicle, endplate, superior and inferior articular processes, unilateral or bilateral facet (subluxation/dislocation), lamina, spinous process, lateral mass, etc. Confounders include the following factors: presence of ankylosing spondylitis, diffuse idiopathic hyperostosis, osteoporosis, previous surgery, degenerative disease, etc.
This classification identifies three components of injury which represent the major and largely independent determinants of prognosis and management.
In this way, the SLIC severity scale is the first sub-axial trauma classification system to give up the anatomical and mechanical elements characterizing the other classifications in favor of injury morphology and clinical status. By building the system on injury patterns less severe to more severe, the SLIC severity scale helps to objectify both diagnosis and optimal management.
Practically, SLIC generates a score of severity that is helpful for the surgeon in the decision-making process. Score between 1 and 3 suggests conservative treatment while 5 or more recommends operative treatment.
Within the three categories of the SLIC system, integrity of the DLC is the most difficult to objectify. The Sub-axial Injury Classification (SLIC) and Severity Scale provides a comprehensive classification system for sub-axial cervical trauma, incorporating pertinent characteristics for generating prognoses and courses of management.
See Fig. 11.2 for calculating the score according to the SLIC system score.
AO Spine Subaxial Cervical Spine Injury Classification System
This classification was developed according to the criteria already used for AO group thoraco-lumbar (TL) junction fractures classification. The goal was to develop a comprehensive and simple classification system with high intra- and interobserver reliability [26].
The classification system describes injuries based on four criteria:
-
1.
morphology of the injury,
-
2.
facet injury,
-
3.
neurologic status,
-
4.
any case-specific modifiers.
Injuries are described by their level, followed by the morphologic type of the primary injury. The secondary injuries and modifiers are placed in parentheses (facet injury, neurologic status, and case specific modifiers).
According to morphology of the injury, AO Spine study group described three types:
“Type A” injuries are fractures that result from vertebral compression with intact tension band divided into five subtypes of increasing severity.
“Type B” injuries include failure of the posterior or anterior tension band by distraction forces with physical separation of the subaxial spinal elements while maintaining the alignment of the spinal axis without translation or dislocation.
“Type C” includes those injuries with displacement or translation of one vertebral body relative to another in any direction: anterior, posterior, lateral translation, or vertical distraction.
The second element analyzed was the morphology of facet injury according to an increasing grade of severity. The evaluation is strategic given the role of facet complex as a dominant stabilizer for axial rotation, and overall stability in association with the capsule, disc, and ligamentous structures [27, 28]. In case of multiple injuries of the same facet (for example, a small fracture and dislocation), only the highest injury is classified (dislocation). If both facets on the same vertebrae are injured, the right-sided facet injury is listed before the left sided injury if the injuries are of different subcategories. The “Bilateral” (BL) modifier is used if both facets have the same type of injury. If only facet injuries are identified (no A, B, or C injury), they are listed first after the level of injury. (For details of the main categories and subgroups, see AOSpine subaxial cervical spine injury classification system).
Neurological status is graded according to a six-part system like the system described for the TL classification:
-
N0—neurologically intact
-
N1—transient neurologic deficit that has completely resolved by the time of clinical examination (usually within 24 h from the time of injury)
-
N2—radiculopathy
-
N3—incomplete spinal cord injury
-
N4—complete spinal cord injury
-
NX—neurology undetermined—used to designate patients who cannot be examined due to head injury or another condition which limits their ability to complete a neurological examination such as intoxication, multiple traumas, or intubation/sedation.
-
The symbol “+” is the only difference with TL classification introduced to identify ongoing cord compression in the setting of incomplete neurologic deficit or nerve injury.
Additional modifiers created to describe unique conditions relevant to clinical decision making are as follows:
-
M1—posterior capsuloligamentous complex injury without complete disruption,
-
M2—Critical disk herniation [29],
-
M3—Stiffening/metabolic bone disease [i.e., Diffuse Idiopathic Skeletal Hyperostosis (DISH), Ankylosing Spondylitis (AS), Ossification of the Posterior Longitudinal Ligament (OPLL) or Ossification of the Ligamentum Flavum (OLF)]. This modifier describes conditions that may argue either for or against surgery for those patients,
-
M4—Signs of vertebral artery injury [30].
Treatment
The choice of best treatment in case of cervical spine injury is the logical consequence of estimation of severity of the lesion according to the correct evaluation of many clinical, morphologic elements. All the proposed classification has been aimed to give the most reliable system of grading the severity of the lesion and suggest an algorithm of treatment. Suspicion of traumatic spinal instability due to cervical injury should guide spinal surgeons throughout the diagnostic process. Underestimating potential cervical spine instability could cause devastating spinal cord injury [31]. In fact, spinal surgeons are generally less worried of serious but stable bone lesions rather than soft tissue injuries (disc-ligamentous complex), potentially responsible for traumatic instability.
In case of cervical severe cervical trauma, it should be advisable to take a multidisciplinary approach from the emergency department to the final treatment decisions [32].
The first step is to accurately classify the injury according to the preferred classification system, estimate the severity of the lesions and differentiate between surgical and non-surgical cervical lesions. When surgical treatment is required, a careful assessment of priorities (polytrauma patients) and timing is essential, especially in the case of concomitant neurological injuries. Last, but not least, is the choice of the surgical approach and technique [33].
The goals of a surgical treatment must be neurologic decompression (in case of neurologic injury) and mechanical stabilization of the spine, to provide a correct spinal alignment and to obtain a solid spinal fusion [34]. Given the complexity of the issue, several methods of reduction-fixation of fractures and dislocations have been published in the literature. However a clear and universally accepted consensus on uniform or standardized methods of surgical approaches and techniques does not exist [35,36,37].
In this regard, classifications can play an important role in suggesting an anterior rather than a posterior or combined approach but are not useful for guiding the choice of specific surgical techniques. Therefore, even today, it is the surgeon’s experience and confidence with one approach over the other that guide and justify the final choice [38].
The timing of decompressive surgery, defined as the time elapsed from the trauma until the operation, and its influence on recovery after a neurologic damage deserve special considerations. In fact, the old concept that timing could be the most important factor for neurologic recovery remains a topic of debate. For many years, there have been no statistical differences in neurological outcomes after spinal cord injury in patients undergoing early or late surgery and, to date, a clearly accepted definition of early or late surgery is still lacking [32, 39]. Recent studies underlined that the difference between early and late surgery and their consequences on postoperative outcome are closely related to the physiopathology of SCI. In the literature there is no surgical procedure that can limit the primary damage while it is mandatory to prevent the secondary SCI, represented by vascular and biochemical changes (electrolytes modification, free radical production, serotonin, and catecholamine accumulation), edema formation and inflammation that appear within 72 h after spinal trauma [40, 41]. Therefore, on the basis of the data of the literature, it seems wise and appropriate to state that the neurological patient should be treated surgically as the general clinical condition and comorbidities can allow it and in any case within 72 h of the trauma [42].
Anterior Approach
The main advantages of the anterior approach to the cervical spine with respect to posterior are minor surgical trauma, reduced infection rate, minor bleeding, and minor postoperative pain. In addition, the anterior surgical approach frequently does not need long fusions which could be limited to one segment of motion, while the posterior approach often requires longer fusions [43].
One of the best indications for anterior approach is the presence of spinal cord compression due to posterior dislocation of bony fragments or disc hernia that allows surgeons to decompress the spinal canal by directly removing them.
Discussed is the anterior approach for facet dislocations with or without previous attempts to closed reduction. An attempt to close reduction for unilateral facet dislocations is sometimes recommended with gentle maneuvers in awake, alert, and cooperative patients.
According to the literature, approximately 50% success rate of a closed reduction has been reported. In the past, some cases of neurologic deterioration have been reported soon after closed maneuvers in which MRI was able to detect disc material inside the spinal canal.
After the first reports of dramatic neurologic complication, even though the occurrence of this event is quite rare, MRI has become strongly recommended for its high sensitivity for soft tissues [44]. Of course, based on the previous statement, any attempt of closed reduction should be performed only after MRI confirmation of the absence of any possible compression of the spinal cord due to disc herniated fragments or epidural hematoma [45, 46]. Spinal epidural hematoma frequently occurs in patients with spondylopathy, particularly in ankylosing spondylitis, after blunt trauma of the cervical spine so MRI is strongly recommended in these patients where the risk of spinal cord compression is very high and an urgent decompression of the spinal cord may be required [47].
Much more dangerous and not recommended are the attempts to reduce bilateral dislocations of the facets due to the simultaneous lesion of the disc and of the anterior and posterior longitudinal ligaments.
Recent literature has shown that in the case of bilateral facet dislocation, the anterior approach alone may not be sufficient due to the high risk of late kyphosis or hardware failure even years after surgery [48].
In these cases, due to the high instability of the lesion, the best indication is that of a combined anterior and posterior approach, in a single phase or, when contraindicated, in two phases, preferably starting from the posterior one.
The posterior approach is mandatory in the case of locked (irreducible) cervical facet dislocations, in the case of late or incorrect diagnosis, or in the case of failed attempts of reduction both closed and open.
Among disadvantages and complications of anterior approach, many patients complain transient laryngopharyngeal discomfort that disappears within 1–2 weeks, while permanent lesion for iatrogenic laryngeal nerve damage is reported as frequent complications of anterior approach especially with right access mostly used by neurosurgeons [49]. Radcliff et al. reported a 61.5% incidence of dysphagia after anterior surgery [50].
Posterior Approach
The most common and used worldwide posterior cervical column fixation technique is lateral mass screwing while the most demanding pedicle screwing technique is still limited to selected cases [51].
An effective cervical internal fixation system for lower cervical fracture-dislocation should provide immediate stabilization of the spine, correction of spinal deformity and limitation of use of external orthosis [52, 53]. Some posterior instruments widely used in the past (such as spinous process wiring, sublaminar wires and laminar hooks) are now completely abandoned due to the lower stability obtainable with these implants compared to those made with the screwing of lateral masses or pedicles [54, 55].
The lateral mass screw, nowadays, represents the gold standard in posterior cervical fixation for its relative safety and reliability in ensuring stability to the damaged spine. However, in a purely posterior column fixation, the resistance to pull-out forces may be limited. To reduce the risk of postoperative implant failure which, occasionally, can occur before fusion is achieved, some authors are used to apply a temporary external rigid collar after surgery. Rarely, stronger external immobilization, such as a halo vest, may be needed to protect the implant from failure particularly when, due to local factors, such as poor bone quality, it is difficult to make a strong and rigid structure [56].
Recently, the increasing availability of neuronavigation systems has given a new impulse to the use of cervical pedicle screw fixation [56]. Abumi et al. [54] first reported the results of pedicle screw fixation for traumatic lesions of the cervical spine in 1994.
Cervical pedicle screw fixation is a three-column fixation system with many biomechanical advantages. The results of biomechanical research demonstrate that the stability of cervical pedicle screw fixation is significantly higher than that of the lateral cervical mass and even superior to combined anterior and posterior fixation. Although cervical pedicle screws have a significantly lower loosening rate at the bone-screw interface as well as increased strength after fatigue testing, the main concern of surgeons is the accuracy of screw placement and the high risk of neurovascular injury. Currently, computer-assisted navigation systems are increasingly used to maximize the accuracy of screw placement [57]. which, in the literature, is between 16.8 and 97% [58] and minimizes the neurovascular damage that remains, however, the main concern in the use of this technique [59].
Unfortunately, given the high cost of navigation, its use is still limited and available only in the best equipped and reference centers for spinal surgery. Despite the lack of a clear guideline, shared among surgeons, the main indications for pedicle screwing are all cases where stronger fixation is required (i.e. osteoporotic patients), in case of major correction of severe traumatic deformities and in case of traumatic floating mass.
Combined Approach
The aim of a combined approach, in a single or two steps, is to achieve superior biomechanical stiffness by providing additional stability to the implants. Circumferential reconstruction has been found to provide maximum stability when applied in the subaxial cervical spine and cervicothoracic junction in case of severe disc-ligamentous complex lesion [60]. In literature, posterior fixation is recommended in case of previous anterior approach after extended corpectomy at more than two levels. In rare cases of severe spinal cord compression, when anterior and posterior decompression is required, the combined approach becomes mandatory despite the inevitable increased risk of complications due to the complexity of the procedure.
The decision to perform a combined approach is not an easy one and requires teams of experts, a proper preoperative assessment of the patient’s general condition capable of supporting a longer intervention and the availability of postoperative intensive care units because of greater surgical trauma, blood loss and increased risk of infection. It has also been reported that the change of patient’s position between the two steps of surgery can increase the risk of nerve injury [61].
Even the study of Yang and colleagues, states that in case of injuries that have a score equal to greater than 7, ranked according to score SLIC, it is advantageous to perform a double treatment [49].
Illustrative Cases
Case 1
Car accident. 45-year-old man arrived in hospital unconscious (GCS 3) and intubated for head trauma with skull fracture and subdural hematoma. Upon arrival the SLIC severity score was 5 suggesting an unstable lesion, as shown in CT scan (Fig. 11.3a). The widening of the anterior part of the intervertebral space suggests the disruption of the anterior longitudinal ligament and disc, without the need for MRI. For the coexistence of comorbidities, planned mono-segmental anterior arthrodesis was delayed and an external orthosis was applied. A new CT, carried out 2 weeks later, showed progression of the C6–C7 listesis (Fig. 11.3b) which confirmed the involvement of the whole disc-ligamentous complex. The careful interpretation of the images, acquired with high resolution CT, has allowed the recognition of clear signs, even if initially slight, highly suggestive of serious cervical injuries without the need of further investigation. An anterior approach was carried out (Fig. 11.4c, d). At surgery, the anterior longitudinal ligament was broken, and disc disrupted (Fig. 11.4a, b) as shown in intraoperative image.
(a) Anterior approach. Intraoperative images of the broken anterior longitudinal ligament (b) and of the plate (c, d) postoperative X-Ray in AP and lateral view. A titanium mesh has been inserted in the intervertebral space to fill the gap and maintain the lordotic alignment. A plate has been carefully shaped to adapt the segment morphology and fixed to the vertebral bodies with screws
Case 2
A 26-year-old woman hit by a vehicle was transferred to the hospital with no neurologic deficit. She reported cervical and thoracic trauma with pulmonary contusion. A chest drainage was applied for hemothorax. During the CT, she became tetraplegic. Behind the C6 vertebral body, a huge round mass was recognizable only on the soft tissue sequences (Fig. 11.5b). While no evidence of mass occupying space inside the spinal canal was recognizable on bone sequences, as show in Fig. 11.5a. No additional bony lesions were recognized. With the suspicion of epidural hematoma, in absence of more lesions, the patient underwent urgent anterior decompression surgery. Surprisingly, a complete tear of the anterior longitudinal ligament and intervertebral disc was detected. After the corpectomy, a huge disc fragment, compressing the spinal cord, was found, and removed (Fig. 11.6). A titanium MESH was used to replace the C6 vertebral body and stabilization was performed with a plate between C5 and C7. As the stabilization resulted not stable enough, an urgent, postoperative MRI was than requested of whole spine. MRI surprisingly demonstrated the coexistence of a serious damage of posterior tension band and, probably of the disc. Lesion of all ligamentous, which required a posterior decompression and arthrodesis (Fig. 11.7). After the results of MRI (Fig. 11.8a) all CT sequences acquired before the operation were reviewed (Fig. 11.8b). Underestimated facet subluxation of more than 50% of the joint were recognized despite they may be a sign of possible major injury to the disc-ligament complex. Assuming a major spine instability, a posterior cervical and thoracic stabilization was carried out 12 h after the first step. Lateral mass screw implant was performed in the cervical spine and a stable fixation was then carried out in the thoracic spine. During the operation a clear instability of the spine was detected with complete lesion of the supra- and inter-spinous ligaments, both joint capsule and subluxation of the facet joint. There was also, a hidden Dural lesion and a right foraminal vascular lesion with leakage of CFS fluid and bleeding with the acts of breath. A temporary mono-segmental fixation determined immediate cessation of the CFS leakage and bleeding. Finally, a definitive pedicles fixation, two levels above and below, was performed (Fig. 11.9). The patient fully recovered in a few months later.
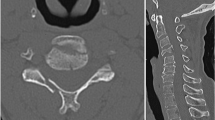
Case 3
67-year-old male, who fell from 3 m in height, arrived at the ER without neurological deficits despite slight numbness in the arms. CT showed C6–C7 spondylolisthesis (Fig. 11.10a) and bilateral dislocation of the facet (Fig. 11.10b, c). The lesion was judged to be severely unstable, and a posterior approach was performed a few hours after arrival (Fig. 11.10d, e). Although an attempted closed reduction is suggested in literature, as soon as possible after cervical injury. A surgical reduction was preferred due to the low collaboration of patient. Despite the open surgery, displacement reduction resulted particularly difficult requiring a partial resection of the lower facets. A long, multilevel fixation was carried out from C5 to T1 and given the optimal clinical condition of the patient, A single level of anterior arthrodesis (Fig. 11.10f, g) was performed 3 days later to accelerate clinical recovery.
Case 4
A 19-year-old boy, victim of a car accident, had suffered a dislocated C5 fracture (Fig. 11.11). On arrival in the emergency room, he had no strength or sensory deficits. The trauma mechanism was flexion-distraction, according to the Allen & Ferguson classification. Classifying the fracture according to SLIC the score was 5 pt. From the axial and coronal CT images the facet joint diastasis lesion is clear (Fig. 11.12a–d). The surgery was done via an anterior approach. Due to the young age of the patient, it was decided to perform surgery using autologous bone grafting to support rapid fusion. The alternative could have been a corpectomy of the C5 soma with expansion cage implantation. The X-ray at 3 months follow-up shows an excellent reduction of the fracture and good fusion of the bone graft (Fig. 11.13a, b).
Discussion
Subaxial cervical spine injury represent one of the most frequent cause of fracture-dislocations, which when not promptly treated can result in important cord lesions that reduce the quality of patients’ life. The incidence of neurological complications has been reduced thanks to first-aid rules on the scene or during transportation to the ER and thanks to the multidisciplinary management of patients with multiple injuries.
Further reduction of patients’ morbidity and mortality is due to the improvement of spine surgery, acknowledgement of spine’s injury anatomy, biomechanics and classifications that permitted more appropriate diagnosis and stadiation of the injuries.
Classifications’ common element is presenting the injuries in increasing order of severity, defined by a sum of various features.
There’s an amount of classification: during the last decades they became easier, more reliable and easier to reproduce.
Allen Ferguson (AF) classification, dating back to 1982, drew the attention to spine’s biomechanics and six different common mechanisms of trauma, so much to gain the definition of “a mechanistic classification”. It was extremely simple, based on X-rays, the only analysis available in that time, which, inevitable, tends to underestimate the severity of the injuries. Furthermore, there was no mention of neurologic involvement, so the authors concluded that medullary lesions’ risk increases with injuries’ gravity. Despite the absence in literature of a clear definition of instability, defined as “ethereal subject badly in need of rigorous definition”, in AF classification, instability was the main factor in treatment decision-making. They concluded that there was not enough instrument to decide whether to go for surgical or conservative treatment, despite being aware of ligaments’ low healing capacity. Surprisingly AF is still widely used in the world, in the common practice. Comparative studies with more recent classifications, showed AF has a good or even better reliability, despite its was conceived and based on x-ray only. Chhabra, in a questionnaire survey on expert opinion worldwide, observed that 38% declared they were using AF, 35% SLIC and only 5% CPISS [62].
SLIC classification and AO classification are the most used nowadays, both stressing out interpretation of lesions’ morphology.
In SLIC classification major emphasis has been put on the disk-ligament complex (DLC), considered as the main stabilizer of the joint, in fact facet subluxation >50% increases the injuries’ score. The involvement of DLC is not always clear using gold standard thin-layer CT, but MRI is sometimes helpful. The initial reliability assessment of the SLIC score was substantial but, among the three components of the classification, the lowest ICC was that of the DLC that confirms the difficulty in its assessment. The highest ICC was that of neurologic status.
Reproducibility is on the limits of every classification: inter and intra observer studies were conducted to demonstrate it. In 2010 Stone et al. [63] and later in 2013 Van Middendorp et al. [64] reported conflicting results on SLIC reliability: first authors reported an excellent inter and intrarater agreement for SLIC and a moderate interrater to an excellent intrarater agreement for AF, while Van Middendorp showed a moderate agreement on SLIC by internal validation studies, but an external validation study yielded a poor agreement.
So, worldwide multicentric studies show that the SLIC’s limit is reproducibility, instead of AF which seems to have a better reliability according to Kanagaraju [65].
In a recent study on multicenter observational survey on reliability and reproducibility for lower cervical spine injuries classification systems, an excellent agreement regarding management was observed among the experienced surgeons using SLIC while agreement among less experienced neurosurgeons was found 2 times less than that of experienced [66]. As advocated also by Vaccaro et al. [67], results showed that higher levels of experience may improve agreement of SLIC.
Subaxial cervical spine injury have heterogeneous morphologic features hence selecting the best surgical approach remains controversial. According to the perspective of many surgeons, they prefer to have a classification comprehensive, easy to use but more oriented to suggest the surgical indication. To achieve this aim, a further classification has been proposed recently with the aim to predict the failure of only anterior approach, called PLICS and measure the intra-interobserver reliability [49]. Anterior only approach is widely used but hardware failure and late cervical deformity are not rare and acceptable complications. In these cases, unstable injury due to not well recognized and estimated posterior elements lesion (bone and ligamentous complex) is the responsible of the complications. The issue is not new. Kotani et al. [68], Lee et al. [69] recognized the strategical importance of zygapophyseal joint and ligaments in conferring stability to the segment of motion. Longitudinal ligament lesion (anterior and posterior) and disc disruption were significantly associated with facet joint fractures and dislocation. The subtype analyses of lateral mass fractures demonstrated high rates of anterior translation in separation, split, and traumatic spondylolisthesis, as well as significant coronal malalignment in comminution and split types [62].
Unlike SLIC, AO classification is easier and with a better reliability and validity, again with the increasing gravity’s levels using a morphologic valuation. Urrutia et al. in 2016 compared agreement between AF and AO. The study demonstrated a significantly better inter-observer agreement with AO while the AF had insufficient inter-observer agreement and did not reach the minimum limit of agreement (k = 0.55) [70].
Nowadays, there’s the introduction of smartphone apps which are helpful to applying classification in clinical practice [71].
In 2021 Schroeder shows that treatment choice depends on experience and origin even in highly unstable injuries [72]. In fact, according to the literature, and also in our experience, there is no classification that includes all the elements that the therapeutic choice requires. Each of the classifications has some peculiar aspects that help the choice of the surgeon. Furthermore, the experience and preference of surgeons are still a bias in the choice of treatment, surgical approach, and techniques.
There is a need for further studies to improve the reliability of existing classifications by aiding communication between healthcare professionals, assisting in treatment decisions, and reducing errors due to misdiagnosis.
References
Torretti JA, Sengupta DK. Cervical spine trauma. Indian J Orthop. 2007;41:255–67.
Pearson AM, Martin BI, Lindsey M, Mirza SK. C2 vertebral fractures in the medicare population: incidence, outcomes, and costs. J Bone Joint Surg Am. 2016;98:449–56.
Dhall SS, Yue JK, Winkler EA, Mummaneni PV, Manley GT, Tarapore PE. Morbidity and mortality associated with surgery of traumatic C2 fractures in octogenarians. Neurosurgery. 2017;80:854–62.
Young AJ, Wolfe L, Tinkoff G, Duane TM. Assessing Incidence and risk factors of cervical spine injury in blunt trauma patients using the National Trauma Data Bank. Am Surg. 2015;81:879–83.
Fredø HL, Bakken IJ, Lied B, Rønning P, Helseth E. Incidence of traumatic cervical spine fractures in the Norwegian population: a national registry study. Scand J Trauma Resusc Emerg Med. 2014;22:78.
Hu R, Mustard CA, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976). 1996;21:492–9.
Clayton JL, Harris MB, Weintraub SL, Marr AB, Timmer J, Stuke LE, et al. Risk factors for cervical spine injury. Injury. 2012;43:431–5.
Wang H, Ou L, Zhou Y, Li C, Liu J, Chen Y, et al. Traumatic upper cervical spinal fractures in teaching hospitals of China over 13 years. Medicine (Baltimore). 2016;95:e5205.
Marcon RM, Cristante AF, Teixeira WJ, Narasaki DK, Oliveira RP, Barros Filho EP. Fractures of the cervical spine. Clinics. 2013;68(7):1455–61.
Schnake KJ, Schroeder GD, Vaccaro AR, et al. AOSpine classification systems (subaxial, thoracolumbar). J Orthop Trauma. 2017;31:S14–23.
Feuchtbaum E, Buchowski J, Zebala L. Subaxial cervical spine trauma. Curr Rev Musculoskelet Med. 2016;9:496–504.
Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52(8):1534–51.
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7(1):1–27.
Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201.
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7(1):1–27. https://doi.org/10.1097/00007632-198200710-00001.
Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, et al. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016;25(7):2173–84.
Anderson PA, Moore TA, Davis KW, Molinari RW, Resnick DK, Vaccaro AR, et al. Cervical spine injury severity score. Assessment of reliability. J Bone Joint Surg Am. 2007;89(5):1057–65.
Louis R. Fractures instables du rachis. III. L’instabilité. A. Les théories de l’instabilité [Unstable fractures of the spine. III.Instability. A. Theories concerning instability]. Rev Chir Orthop Reparatrice Appar Mot. 1977;63(5):423–5. French
Whitesides TE Jr. Traumatic kyphosis of the thoracolumbar spine. Clin Orthop. 1977;128:78–92.
Frisen M, Magi M, Sonnerup L, Viidik A. Rheological analysis of soft collagenous tissue-I. J Biomech. 1969;2:13–20.
Galante JO. Tensile properties of the human lumbar annulus fibrosus. Thesis. Acta Orthop Scand. 1967;Suppl 100:1–91.
Al K, Vulcan AP. Elastic deformation characteristics of the spine. J Biomech. 1971;4:413–29.
Lin HS, Liu YK, Adams KH. Mechanical response of the lumbar intervertebral joint under physiological (complex) loading. J Bone Joint Surg. 1978;60A:4i–55.
Barnes R. Paraplegia in cervical spine injuries. Proc R Soc Med. 1961;54(5):365–7.
Durbin FC. Fracture-dislocations of the cervical spine. J Bone Joint Surg Br. 1957;39-B(1):23–38. https://doi.org/10.1302/0301-620X.39B1.23.
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J, Shanmuganathan R, Fehlings M, Vialle L, AOSpine Spinal Cord Injury & Trauma Knowledge Forum. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38(23):2028–37. https://doi.org/10.1097/BRS.0b013e3182a8a381.
Nadeau M, McLachlin SD, Bailey SI, Gurr KR, Dunning CE, Bailey CS. A biomechanical assessment of soft-tissue damage in the cervical spine following a unilateral facet injury. J Bone Joint Surg Am. 2012;94:e156. https://doi.org/10.2106/JBJS.K.00694.
Rasoulinejad P, McLachlin SD, Bailey SI, Gurr KR, Bailey CS, Dunning CE. The importance of the posterior osteoligamentous complex to subaxial cervical spine stability in relation to a unilateral facet injury. Spine J Off J North Am Spine Soc. 2012;12:590–5. https://doi.org/10.1016/j.spinee.2012.07.003.
Vaccaro AR, Falatyn SP, Flanders AE, Balderston RA, Northrup BE, Cotler JM. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine. 1999;24:1210–7.
Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, Kandziora F, Fehlings MG, Dvorak MF, Aarabi B, Rajasekaran S, Schroeder GD, Kepler CK, Vialle LR. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016;25(7):2173–84. https://doi.org/10.1007/s00586-015-3831-3.
Zaveri G, Das G. Management of sub-axial cervical spine injuries. Indian J Orthop. 2017;51(6):633–52. https://doi.org/10.4103/ortho.IJOrtho_192_16.
Dobran M, Iacoangeli M, Nocchi N, Di Rienzo A, di Somma LG, Nasi D, Colasanti R, Al-Fay M, Scerrati M. Surgical treatment of cervical spine trauma: our experience and results. Asian J Neurosurg. 2015;10(3):207–11. https://doi.org/10.4103/1793-5482.161192.
Proietti L, Perna A, Ricciardi L, Fumo C, Santagada DA, Giannelli I, Tamburrelli FC, Leone A. Radiological evaluation of fusion patterns after lateral lumbar interbody fusion: institutional case series. Radiol Med. 2021;126(2):250–7. https://doi.org/10.1007/s11547-020-01252-5.
Krishna V, Andrews H, Varma A, Mintzer J, Kindy MS, Guest J. Spinal cord injury: how can we improve the classification and quantification of its severity and prognosis? J Neurotrauma. 2014;31(3):215–27. https://doi.org/10.1089/neu.2013.2982.
La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisalof the literature using a meta-analytical approach. Spinal Cord. 2004;42:503–12.
Skovrlj B, Steinberger J, Guzman JZ, Overley SC, Qureshi SA, Caridi JM, Cho SK. The 100 most influential articles in cervical spine surgery. Global Spine J. 2016;6(1):69–79. https://doi.org/10.1055/s-0035-1551652.
Harrop JS, Sharan A, Ratliff J. Central cord injury: pathophysiology, management, and outcomes. Spine J. 2006;6(6 Suppl):198S–206.
Mautes AE, Weinzierl MR, Donovan F, Noble LJ. Vascular events after spinal cord injury: contribution to secondary pathogenesis. Phys Ther. 2000;80:673–87.
Cotler JM, et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine. 1993;18:386–90.
Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxationor dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73:1555–60.
Gao W, Wang B, Hao D, Zhu Z, Guo H, Li H, Kong L. Surgical treatment of lower cervical fracture-dislocation with spinal cord injuries by anterior approach: 5- to 15-year follow-up. World Neurosurg. 2018;115:e137–45. https://doi.org/10.1016/j.wneu.2018.03.213.
Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg Br. 1992;74:224–7.
O’Dowd JK. Basic principles of management for cervical spine trauma. Eur Spine J. 2010;19(Suppl 1):S18–22.
Crim JR, Moore K, Brodke D. Clearance of the cervical spine in multitrauma patients: the role of advanced imaging. Semin Ultrasound CT MR. 2001;22:283–305.
Reindl R, et al. Anterior reduction for cervical spine dislocation. Spine (Phila Pa 1976). 2006;31:648–52.
Theodotou CB, et al. Anterior reduction and fusion of cervical facet dislocations. Neurosurgery. 2019;84(2):388–95.
Tamburrelli FC, Meluzio MC, Masci G, Perna A, Burrofato A, Proietti L. Etiopathogenesis of traumatic spinal epidural hematoma. Neurospine. 2018;15(1):101–7. https://doi.org/10.14245/ns.1834938.469.
Genitiempo M, Perna A, Santagada DA, Meluzio MC, Proietti L, Bocchi MB, Logroscino CA, Tamburrelli FC. Single-level Bryan cervical disc arthroplasty: evaluation of radiological and clinical outcomes after 18 years of follow-up. Eur Spine J. 2020;29(11):2823–30. https://doi.org/10.1007/s00586-020-06486-5.
Yang JS, Liu P, Liu TJ, Zhang HP, Zhang ZP, Yan L, Zhao QP, He BR, Tuo Y, Zhao YT, Huang DG, Hao DJ. Posterior ligament-bone injury classification and severity score: a novel approach to predict the failure of anterior-only surgery for subaxial cervical facet dislocations. Spine (Phila Pa 1976). 2021;46(4):209–15. https://doi.org/10.1097/BRS.0000000000003771.
Radcliff KE. What is the incidence of dysphagia after posterior cervical surgery? Spine. 2013;38(13):1082–8.
Joaquim AF, Tan L, Riew KD. Posterior screw fixation in the subaxial cervical spine: a technique and literature review. J Spine Surg. 2020;6(1):252–61. https://doi.org/10.21037/jss.2019.09.28.
Zhang HL, Zhou DS, Jiang ZS. Analysis of accuracy of computer-assisted navigation in cervical pedicle screw installation. Orthop Surg. 2011;3:52–6.
Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667–72.
Abumi K, Ito H, Taneichi H, Kaneda K. Transpedicular screw fixations for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28.
Karaikovic EE, Yingsakmongkol W, Gaines RW Jr. Accuracy of cervical pedicle screw placement using the funnel technique. Spine (Phila Pa 1976). 2001;26:2456–62.
Zhou F, Zou J, Gan M, Zhu R, Yang H. Management of fracture-dislocation of the lower cervical spine with the cervical pedicle screw system. Ann R Coll Surg Engl. 2010;92(5):406–10. https://doi.org/10.1308/003588410x12628812459616a.
Reinhold M, Magerl F, Rieger M, Blauth M. Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J. 2007;16:47–56.
Dhillon CS, Jakkan MS, Dwivedi R, Medagam NR, Jindal P, Ega S. Outcomes of unstable subaxial cervical spine fractures managed by posteroanterior stabilization and fusion. Asian Spine J. 2018;12(3):416–22. https://doi.org/10.4184/asj.2018.12.3.416.
Sribnick EA, Hoh DJ, Dhall SS. Traumatic high-grade cervical dislocation: treatment strategies and outcomes. World Neurosurg. 2014;82:1374–9.
Li P, Xue Y, Wang P, et al. Decompression via posterior-anterior approach and anterior fixation in treatment of fracture dislocation of the lower cervical spine with bilateral facet joints dislocation. Zhonghua Gu Ke Za Zhi. 2011;31:34–8.
Lan X, Xu JZ, Luo F, et al. Different surgical approaches for treatment of fracture and dislocation of the lower cervical spine. Zhonghua Chuang Shang Za Zhi. 2013;29:302–6.
Chhabra HS, Kaul R, Kanagaraju V. Do we have an ideal classification system for thoracolumbar and subaxial cervical spine injuries: what is the expert’s perspective? Spinal Cord. 2015;53(1):42–8. https://doi.org/10.1038/sc.2014.194.
Stone AT, Bransford RJ, Lee MJ, Vilela MD, Bellabarba C, Anderson PA, Agel J. Reliability of classification systems for subaxial cervical injuries. Evid Based Spine Care J. 2010 Dec;1(3):19–26. https://doi.org/10.1055/s-0030-1267064.
van Middendorp JJ, Audigé L, Bartels RH, Bolger C, Deverall H, Dhoke P, Diekerhof CH, Govaert GA, Guimerá V, Koller H, Morris SA, Setiobudi T, Hosman AJ. The subaxial cervical spine injury classification System: an external agreement validation study. Spine J. 2013 Sep;13(9):1055–63. https://doi.org/10.1016/j.spinee.2013.02.040.
Kanagaraju V, Yelamarthy PKK, Chhabra HS, Shetty AP, Nanda A, Sangondimath GM, Dutta Das K, Bansal ML, Mohapatra B, Patel N, Abel R, Tuli S, Barros T, Tandon V. Reliability of Allen Ferguson classification versus subaxial injury classification and severity scale for subaxial cervical spine injuries: a psychometrics study. Spinal Cord. 2019;57(1):26–32. https://doi.org/10.1038/s41393-018-0182-z.
Grin A, Krylov V, Lvov I, Talypov A, Dzukaev D, Kordonskiy A, Smirnov V, Karanadze V, Abdukhalikov B, Khushnazarov U, Airapetyan A, Dmitriev A, Kaykov A, Peyker A, Semchenko V, Aksenov A, Borzenkov A, Gulyy V, Torchinov S, Bagaev S, Toporskiy A, Kalandari A, Kasatkin D, Sytnik A, Lebedev V, Epifanov D, Hovrin D, Feniksov V, Choriev D. External multicenter study of reliability and reproducibility for lower cervical spine injuries classification systems-part 2: an analysis of the subaxial cervical spine injury classification and cervical spine injury severity score scale. Global Spine J. 2021 Jan;11(1):99–107. https://doi.org/10.1177/2192568219896546.
Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA Jr, Anderson P, Harrop J, Oner FC, Arnold P, Fehlings M, Hedlund R, Madrazo I, Rechtine G, Aarabi B, Shainline M, Spine Trauma Study Group. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007;32(21):2365–74. https://doi.org/10.1097/BRS.0b013e3181557b92.
Kotani Y, Abumi K, Ito M, Minami A. Cervical spine injuries associated with lateral mass and facet joint fractures: new classification and surgical treatment with pedicle screw fixation. Eur Spine J. 2005;14(1):69–77.
Lee SH, Sung JK. Unilateral lateral mass-facet fractures with rotational instability: new classification and a review of 39 cases treated conservatively and with single segment anterior fusion. J Trauma. 2009;66(3):758–67. https://doi.org/10.1097/TA.0b013e31818cc32a.
Urrutia J, Zamora T, Campos M, Yurac R, Palma J, Mobarec S, Prada C. A comparative agreement evaluation of two subaxial cervical spine injury classification systems: the AOSpine and the Allen and Ferguson schemes. Eur Spine J. 2016;25(7):2185–92. https://doi.org/10.1007/s00586-016-4498-0.
Ono AHA, Chang VYP, Rodenbeck EM, de Araujo AO, de Oliveira RG, Marcon RM, Cristante AF, Filho TEPB. Assessment of the accuracy of the AO Spine-TL classification for thoracolumbar spine fractures using the AO surgery reference mobile app. Global Spine J. 2021;11(2):187–95.
Schroeder GD, Canseco JA, Patel PD, Divi SN, Karamian BA, Kandziora F, Vialle EN, Oner FC, Schnake KJ, Dvorak MF, Chapman JR, Benneker LM, Rajasekaran S, Kepler CK, Vaccaro AR, AO Spine Cervical Classification Validation Group. Establishing the injury severity of subaxial cervical spine trauma: validating the hierarchical nature of the AO spine subaxial cervical spine injury classification system. Spine (Phila Pa 1976). 2021;46(10):649–57.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tamburrelli, F.C., Meluzio, M.C., Perna, A., Borruto, M.I., Genitiempo, M., Proietti, L. (2022). Cervical Spine Fractures and Dislocations, Classification and Treatment. In: Menchetti, P.P.M. (eds) Cervical Spine. Springer, Cham. https://doi.org/10.1007/978-3-030-94829-0_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-94829-0_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94828-3
Online ISBN: 978-3-030-94829-0
eBook Packages: MedicineMedicine (R0)