Abstract
-
Phenylalanine ammonia lyase (PAL) converts phenylalanine to ammonia and trans-cinnamic acid and can reduce phenylalanine concentrations in individuals with phenylketonuria (PKU).
-
Injectable pegvaliase (recombinant Anabaena variabilis PAL produced in E. coli conjugated with polyethylene glycol [PEG] to reduce immunogenicity (marketed as Palynziq®) has been shown to reduce blood phenylalanine concentrations in the majority of subjects with PKU in Phase 1, 2 and 3 clinical trials.
-
The most frequently reported adverse events are injection-site reactions, arthralgia, dizziness, and skin reactions. There is a risk of anaphylaxis. This requires premedication with histamine-receptor blockers and anti-inflammatory drugs and to have epinephrine available.
-
Long-term use of pegvaliase causes a persistent reduction of blood phenylalanine concentrations and a continued improvement of executive function measures.
-
Nutrition management of patients treated with pegvaliase focuses on increasing intact protein once blood phenylalanine is in the treatment range. This diet transition can be challenging for some patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
Phenylalanine ammonia lyase (PAL) converts phenylalanine to ammonia and trans-cinnamic acid and can reduce phenylalanine concentrations in individuals with phenylketonuria (PKU).
-
Injectable pegvaliase (recombinant Anabaena variabilis PAL produced in E. coli conjugated with polyethylene glycol [PEG] to reduce immunogenicity (marketed as Palynziq®) has been shown to reduce blood phenylalanine concentrations in the majority of subjects with PKU in Phase 1, 2 and 3 clinical trials.
-
The most frequently reported adverse events are injection-site reactions, arthralgia, dizziness, and skin reactions. There is a risk of anaphylaxis. This requires premedication with histamine-receptor blockers and anti-inflammatory drugs and to have epinephrine available.
-
Long-term use of pegvaliase causes a persistent reduction of blood phenylalanine concentrations and a continued improvement of executive function measures.
-
Nutrition management of patients treated with pegvaliase focuses on increasing intact protein once blood phenylalanine is in the treatment range. This diet transition can be challenging for some patients.
1 Background
Standard therapy for phenylketonuria (PKU) consists of a protein and phenylalanine-restricted diet for life [1]. If consistent adherence to this stringent dietary regimen decreases as a patient gets older, this will cause an increase in phenylalanine concentrations that can result in cognitive and executive dysfunction and psychiatric issues in the long term [2, 3]. Sapropterin, a synthetic form of tetrahydrobiopterin, can increase residual phenylalanine hydroxylase activity and decreases phenylalanine concentrations in about one-third of all patients with PKU when used in conjunction with diet [4, 5]. Individuals with the most severe forms of PKU usually do not respond to sapropterin and struggle to maintain a strict diet once they approach adult age. For this reason, additional therapies are being developed to treat PKU [4].
Pegvaliase (PEGylated recombinant [Anabaena variabilis] phenylalanine ammonia lyase [PAL]; marketed in the United States as PALYNZIQ™) is a novel enzyme substitution therapy administered via subcutaneous injection that lowers blood phenylalanine independently of diet [6, 7]. PAL (EC 4.3.1.24) is an enzyme not present in mammals that converts phenylalanine to ammonia and trans-cinnamic acid (Fig. 11.1) [8].
Degradation of phenylalanine to trans-cinnamic acid and ammonia by the enzyme PAL. Ammonia generated by PAL is converted to urea in the liver by the urea cycle. Trans-cinnamic acid is converted to benzoic acid by unknown processes. Benzoic acid is conjugated with glycine to form hippuric acid and excreted in urine [8]
Ammonia is removed by the urea cycle while trans-cinnamic acid is converted to benzoic acid by an unknown mechanism and, after conjugation with glycine by glycine N-acyltransferase, produces hippuric acid that can be excreted in urine [9]. Initial trials of oral PAL in humans yielded a modest decrease in blood phenylalanine concentrations [10]. Subsequent studies in animal models led to the development of a recombinant Anabaena variabilis PAL genetically modified to improve protease resistance and PEGylated to reduce immunogenicity (rAvPAL-PEG; pegvaliase) [11]. In a murine model of PKU deficient in PAH activity (BTBRPahenu2 [ENU2]), weekly subcutaneous administration of rAvPAL-PEG and, to a lesser extent, oral administration of PEGylated PAL, reduced blood phenylalanine concentrations over 3 months [11, 12]. Pegylation was essential to mask the bacterial protein and to allow persistent enzymatic activity.
2 Human Clinical Trials
Phase 3 trials for pegvaliase as enzyme substitution therapy for PKU began in 2013 and pegvaliase was FDA-approved on May 24, 2018 to reduce blood phenylalanine concentrations in adult patients with PKU with phenylalanine concentrations >600 μmol/L on existing management.
Phase 1 clinical trials in adult patients with PKU started in 2008 and demonstrated that a single subcutaneous dose of 0.1 mg/kg of pegvaliase reduced plasma phenylalanine concentrations [13]. Adverse events included injection-site reactions, dizziness, and rashes (local or generalized). No significant changes in safety laboratory tests were observed, but all patients developed antidrug antibodies. Blood PAL levels peaked about 5 days after drug administration with a mean 54% reduction in blood phenylalanine concentrations, with a nadir approximately 6 days after injection (Fig. 11.2a). There was an inverse correlation between drug and phenylalanine concentrations in plasma (Fig. 11.2b) [9]. Phenylalanine concentrations returned to near-baseline concentrations approximately 21 days after the single injection of rAvPAL-PEG.
Panel (a) Concentrations of plasma phenylalanine (filled circle) and rAvPAL-PEG (open squares) in subjects with phenylketonuria after one dose (time zero) of 0∙1 mg/kg of rAvPAL-PEG. Points are averages with the SD indicated in one direction. Panel (b) Correlation between plasma concentrations of rAvPAL-PEG and phenylalanine. Note the significant inverse correlation between plasma rAvPAL-PEG and phenylalanine concentrations in subjects with phenylketonuria who received a single dose of 0∙1 mg/kg of rAvPAL-PEG. The thick line represents the regression using all points with the parameters indicated. The lines are regression to individual subjects. These were all highly significant (p < 0∙01) except in Subject 5 where the regression was statistically significant (p < 0∙05). rAvPAL-PEG = pegvaliase [13]
3 Efficacy and Safety
Multiple Phase 2 studies examined the effects of repeated administration of pegvaliase to subjects with PKU (Table 11.1). The objective of these trials was to define the best way to progressively increase pegvaliase dosing, identifying the regimen producing the most rapid decrease in phenylalanine concentrations, while minimizing side effects. The three Phase 2 studies increased pegvaliase dosing very slowly (PAL-002) [7], then very rapidly (PAL-004) [7, 14] until an intermediate rate of dose increase was found acceptable (165–205) [15]. Most patients continued into a Phase 2 extension study (PAL-003) [15] to determine efficacy and safety over time [7]. Patients maintained consistent diets (many of them had unrestricted diets) with mean pretreatment baseline blood phenylalanine concentrations >1200 μmol/L (Fig. 11.3). There was a progressive decrease in plasma phenylalanine levels with time as the dosage of pegvaliase was increased (independent of whether the patients were initially started on a low dose (PAL-002, Fig. 11.3a) or high dose (PAL-004, Fig. 11.3b) of pegvaliase. In both cases, significant reductions of blood phenylalanine were seen once the weekly pegvaliase dose was increased to >80 mg per week and phenylalanine concentrations of <600 μmol/L were observed at a dose of 140–280 mg per week (Fig. 11.3). The Phase 2 data indicated that the dose of pegvaliase needs to be increased gradually to avoid severe reactions and that the majority of patients who continue dosing can expect a meaningful reduction of plasma phenylalanine concentrations with doses of 20 mg or 40 mg of pegvaliase per day. All patients developed antibodies against pegvaliase and the reduction in plasma phenylalanine was dependent on the individual immune response, the dose of drug, and the duration of therapy. The majority (81%) of Phase 2 subjects entering the long-term extension study achieved at least two consecutive blood phenylalanine concentrations ≤600 μmol/L after an average of 26 weeks of therapy [15, 16].
Mean blood phenylalanine concentration and pegvaliase dose over time in (a) PAL-002 and (b) PAL-004 continuing through PAL-003. Data are presented as mean (SE). Dotted line indicates transition of participants from the PAL-002 or PAL-004 studies to the PAL-003 study. Sample size reflects the participants with data available at the indicated time point and who had reached the time point at the time of the data cut; the study was ongoing at the time of this analysis [7]
Three Phase 3 studies evaluated the efficacy and safety of self-injection of pegvaliase in adults with PKU (165–301 [Prism301] and 165–302 [Prism302]), including a sub-study aimed at identifying changes in executive functioning caused by reduction of phenylalanine concentrations in adults (Prism003). A more recent trial (165–304) is evaluating the effect of higher doses of pegvaliase (up to 60 mg/day) on reduction of phenylalanine concentrations.
Since it was not possible to predict which patients would respond to pegvaliase with a reduction of phenylalanine concentrations without dose-limiting side effects, the pivotal trial was an 8-week double-blind, placebo-controlled randomized discontinuation trial in which subjects who had reduction of phenylalanine concentrations with proper induction therapy were randomly assigned to receive placebo, 20 mg or 40 mg per day of pegvaliase [6]. The administration of placebo and discontinuation of pegvaliase caused a significant increase of plasma phenylalanine concentrations (Fig. 11.4) from 504–564 μmol/L to 1173–1513 μmol/L in patients assigned to the placebo arm, but no significant increase in plasma phenylalanine was noted in patients receiving 20 or 40 mg per day of pegvaliase (Fig. 11.4) [6]. No significant changes in psychometric measures were observed in the 8 weeks of the randomized discontinuation trial [6].
Plasma phenylalanine concentrations in patients with phenylketonuria undergoing randomized discontinuation (RDT) of pegvaliase treatment. Baseline phenylalanine concentration ranged from 1109 to 1459 μmol/L in the different groups. Phenylalanine concentrations decreased to 504–564 μmol/L with open-label pegvaliase therapy. Discontinuation of pegvaliase and administration of placebo instead increased phenylalanine concentrations to 1164–1509 μmol/L after 8 weeks whereas continuation of pegvaliase at either 20 or 40 mg per day maintained phenylalanine concentrations at 559 μmol/L. Points represent the average of the patient population and are shown ± standard errors [6]
Continuation of therapy with pegvaliase further reduced phenylalanine concentrations in patients with PKU, with more than 60% of participants maintaining plasma phenylalanine concentrations <360 μmol/L after 24 months of therapy [16]. The reduction in phenylalanine concentrations was associated with a progressive improvement in ADHD scores in patients who displayed elevated scores at baseline (Fig. 11.5) [16]. Even though this part of the study was open label, the consistency of the continued improvement and the descriptions provided by patients were suggestive of a true effect.
Plasma phenylalanine concentration (continuous line) and investigator-rated ADHD RS-IV IA scores (dashed line) in participants with baseline scores >9 (inattention subgroup, N = 116). Sample size reflects participants with data available at study timepoint and who have reached study timepoint at data cut; study is ongoing. ADHD RS-IV IA Attention Deficit Hyperactivity Disorder Rating Scale IV inattention subscale, SE standard error [16]
In terms of safety, the Phase 3 study (165–205) demonstrated that weekly, low-dose introduction of treatment, followed by gradual dosage and frequency increases, was well tolerated, with hypersensitivity events limited to mild or moderate severity. The most common adverse events included hypersensitivity-type reactions consisting of injection-site reactions, skin reactions, and/or joint pains (Table 11.2) [14].
While hypersensitivity-type reactions were observed in nearly all subjects during initial drug administration, the reactions were generally mild to moderate and self-limited. The majority of subjects with these reactions were all successfully re-treated. The most common adverse events in long-term extension studies were injection-site reaction (72.5%), injection-site erythema (67.5%), headache (67.5%), and arthralgia (65.0%) [15]. Acute systemic hypersensitivity events, including potential events of anaphylaxis, were not associated with immunoglobulin E, and all events resolved without sequelae.
Adverse events were more frequent with initiation of therapy and dose escalation and were associated with anti-PEG antibodies in the first 24 weeks of therapy (Fig. 11.6) [15]. As antibody concentrations decreased, the frequency and severity of side effects improved. The use of premedications and the development of specific guidelines to deal with these side-effects improved the drug tolerability by subjects [17].
Frequency of hypersensitivity events (pink bars) and incidence of antibody positivity over time. Antibody positivity is calculated as the number of participants testing positive divided by the total number of participants at each study visit. All Phase 2 data are included. Sample size reflects participants with data available at study timepoint; study is ongoing. Abbreviations: IgG immunoglobulin G, IgM immunoglobulin M, PAL phenylalanine ammonia lyase, PEG polyethylene glycol, NAb neutralizing antibody [15]
4 Hypophenylalaninemia
The majority of subjects in PAL-003 had at least one blood sample where pegvaliase reduced phenylalanine concentrations below the normal range (≤30 μmol/L). No consistent association was found between these low concentrations and adverse effects. An increase in dietary protein and/or a reduction in the weekly dose of pegvaliase were found to be effective to normalize phenylalanine concentrations. Detailed studies about hypophenylalaninemia have not yet been published.
5 Immunogenicity
All subjects treated with pegvaliase developed antibodies against PAL and polyethylene glycol (PEG). Antidrug antibodies against PAL peaked by 6 months and then stabilized (Fig. 11.6). Most patients developed transient antibody responses against PEG, peaking by 3 months, then returning to baseline by 9 months (Fig. 11.6). Pegvaliase bound to antidrug antibodies formed circulating immunocomplexes that caused complement activation, with reduction of serum complement concentrations [18]. Complement activation was highest during early treatment and decreased with time. Plasma phenylalanine concentrations decreased with time as circulating immune complex concentrations and complement activation declined and pegvaliase dosage increased [18, 19]. Hypersensitivity adverse events were most frequent at the beginning of treatment and declined over time (Fig. 11.6). No subject with acute systemic hypersensitivity events tested positive for pegvaliase-specific IgE near the time of the event. IgE could not be detected even after depleting the IgG and IgM, immunoglobulins that could have prevented detection of IgE [20]. Laboratory evidence was consistent with immune complex-mediated type III hypersensitivity. There was no evidence of pegvaliase-associated immune complex-mediated end organ damage [19].
6 Practical Use of Pegvaliase in Phenylketonuria
Since commercial therapy with pegvaliase is relatively new, there is variation in the practice from clinic to clinic. This section describes the management of patients receiving pegvaliase therapy at University of Utah Metabolic Clinic.
Therapy for patients with PKU is individualized. Typically, pegvaliase therapy is reserved for adults with PKU who cannot maintain phenylalanine concentrations <600 μmol/L with available therapies. However, given the considerable constraints of the long-term PKU diet, more and more adults, including those responsive to sapropterin and those able to achieve consistent phenylalanine concentrations <360 μmol/L with diet, are attracted to pegvaliase therapy. Pegvaliase therapy requires education about its risks, proper drug administration, administration of premedications and rescue medications as necessary. Educational videos have been developed for patients and those living with them to explain proper procedures [17].
Based on the available immunogenicity data, pegvaliase induces a Type III hypersensitivity reaction, causing hypersensitivity adverse events that peak during induction/titration and decline over time as therapy is continued [18]. An induction, titration, and maintenance dosing regimen has been developed in our clinic with a schedule of events that patients need to understand and follow (Table 11.3).
At each clinic visit, the patient brings a 3-day diet record that is discussed with the dietitian, medical history is reviewed, and the patient is observed to self-inject the drug. Visits may be done virtually, including initial visits, if they are completed with the assistance of a home health nurse observing the injection and monitoring the patient for at least 60 minutes for severe reactions. The dose of pegvaliase is progressively increased until a response is observed. Levels of phenylalanine and tyrosine are monitored by plasma amino acids during clinic visits or by filter paper testing as per standard of care (at least once a month). The highest dose (60 mg per day) is usually necessary in patients with very elevated diagnostic phenylalanine concentrations (>3000 μmol/L) or with high antidrug antibody titers.
Because adverse events are common, patients are educated about possible side-effects, the need to have a responsible adult present for at least 1 hour after dosing in the first 16 weeks, and the requirement to carry auto-injectable adrenaline (epinephrine) [17, 18]. Risk mitigation strategies include premedication with H1-receptor antagonists (cetirizine 10 mg per day or fexofenadine 180 mg per day), H2-receptor antagonists (famotidine 20 mg per day), anti-inflammatory drugs (ibuprofen 600 mg per day with food). Premedications can typically be discontinued once the patient is on maintenance therapy and is free of reactions. Patients require close monitoring of adverse events and extending the titration period if hypersensitivity adverse events occur.
All patients are given contact information for the clinic with the number to call in case they suffer an adverse event. After hours, they are instructed to contact the geneticist/fellow on call. Adverse events should be promptly communicated with the clinic and summarized during in-person or remote visits. Hypersensitivity adverse events are usually managed by telemedicine using Benadryl or, rarely, steroids. In case of severe reactions, the patient is instructed to proceed to the closest emergency room.
If hypophenylalaninemia (phenylalanine <30 μmol/L) is observed, natural protein is increased by 10–20 g/day each week with a concurrent decrease in protein from medical food by 10–20 g/day, until reaching a goal protein intake with appropriate blood phenylalanine concentrations. Once diet is liberalized, but phenylalanine concentrations remain <30 μmol/L, the pegvaliase dose is decreased by 10%. Phenylalanine concentrations are measured about 2 weeks after each dose reduction until an increase of phenylalanine concentrations into the therapeutic range (45–360 μmol/L) is observed. Patients who continue therapy for a long time (>5 years) sometimes require dose reduction to maintain phenylalanine concentrations >0 μmol/L.
All patients are offered a neuropsychological assessment within 30 days of starting pegvaliase. Testing is repeated at approximately 12 months after starting therapy or after the patient reaches efficacy (phenylalanine concentrations <360 μmol/L), whichever comes first Current guidance suggests that pegvaliase is not to be used during pregnancy [17]; the label states that there is no data in humans and that the drug may cause fetal harm [21]. Despite this, the teratogenic effects of elevated blood phenylalanine on the fetus are well known [22] and the risks of the use of pegvaliase should be weighed against the risk of elevated phenylalanine concentrations. There is one case report of a successful outcome in a woman who continued pegvaliase during pregnancy [23]. Several women have discontinued pegvaliase prior to pregnancy, and with extensive education and support, were able to restart a phenylalanine-restricted diet and achieve blood phenylalanine in the treatment range for maternal PKU with successful pregnancy outcomes. It is unlikely that pegvaliase passes into breastmilk [24] and limited evidence from one case supports this [25]. If a woman is treated with pegvaliase during lactation, it is important to monitor maternal blood phenylalanine closely and avoid hypophenylalaninemia to ensure that the infant receives adequate phenylalanine for growth [21].
The safety and efficacy of pegvaliase has not been studied in the children younger than 16 years or in individuals over 65 years of age.
7 Nutrition Management of Patients with PKU Treated with Pegvaliase
Approved in 2018, Palynziq® (BioMarin, Novato, CA) or pegvaliase pqpz (pegvaliase) is an injectable enzyme substitution therapy for treating adults with PKU who have blood phenylalanine concentrations over 600 μmol/L while on other therapies [21], including diet and/or sapropterin dihydrochloride. While a phenylalanine-restricted diet has long been the primary mode of therapy for individuals with PKU, there is a shift to medical management that offers adults with PKU the possibility of attaining blood phenylalanine concentrations <360 μmol/L while consuming a “normal” diet (one that contains at least the recommended amount of protein from food sources). Nutrition management of patients on pegvaliase remains an important component of treatment, especially during the transition from a phenylalanine-restricted diet to a normal diet, and approaches to the nutrition management of these patients can be thought of in stages.
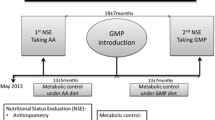
7.1 Nutrition Management During Pegvaliase Initiation and Titration
All patients starting pegvaliase should undergo a thorough nutrition assessment at baseline to establish the patient’s usual phenylalanine intake and nutrition status prior to a pegvaliase trial [17]. Nutrition assessment includes anthropometrics, nutrient analysis of dietary intake, as well as laboratory monitoring for patients with PKU as described in Chap. 10. Bone density and body composition assessments are recommended by some, as well as measures of food phobias and quality of life [26]. Measurements of inflammatory markers such as C-reactive protein and erythrocyte sedimentation rate may also be performed [27].
Detailed attention to the patient’s protein intake at baseline is especially important, including assessment of the amount and sources of protein in the diet. Adults with PKU may fall anywhere on the PKU diet spectrum, ranging from those who are taking medical food and restricting intact protein to those who have gone “off diet” and are eating a wide variety of foods. In the clinical trials, 15.7% of subjects were considered to be “on diet,” defined as taking at least 75 percent of protein from medical food [16]. However, most (57%) reported consuming some medical food in their diets, indicating that they were not on unrestricted diets [16]. Protein intake from medical food and/or intact sources should meet the DRI of 0.8 g/kg/d [28], and for patients consuming a vegan diet (without medical food), the requirement is slightly higher (0.9 g/kg/d) [17]. If protein intake goals are not met, nutrition counseling about the addition of medical food or high-quality sources of protein to the patient’s diet should be considered prior to commencing drug therapy.
Once it is established that the patient’s protein intake is adequate, the metabolic dietitian counsels them to maintain a consistent intake while the drug is initiated and titrated up to the target dose. This ensures that changes in blood phenylalanine can be attributed to the drug and not to a change in diet or lifestyle. Maintaining a consistent diet means avoiding drastic changes in food intake, such as adding high protein foods before being advised to or starting a weight reduction diet. Some clinics require patients to keep food records along with blood phenylalanine monitoring in order to verify that protein intake remains within 10% of baseline, as was required in the clinical trials [16], but the reliability of food records in assessing intake is limited [29].
Patients are counseled not to adjust their diets until the blood phenylalanine reaches the target range and the dietitian recommends a diet change. During the clinical trials, there was an increase over time in subjects’ mean protein intake [16, 25]; and while some of the increase was due to recommended changes, some was due to a tendency for subjects to add protein-containing foods before being counseled to do so.
Since pegvaliase therapy may take a year or longer before a reduction in blood phenylalanine is seen, the drug titration period is a good time to explore what the patient’s wishes are for the new diet, including food groups they wish to try or avoid, weight goals, interest in cooking, and any financial constraints.
The titration period is also a good time to discuss whether the patient has any food aversions or fears about adding new foods [17]. There are several tools available to assess food neophobias [30]. In a study of pegvaliase-treated patients who had been on a normal diet for at least 6 months, most reported low to moderate food neophobia, which correlated with increased enjoyment of food [31]. More research is needed to assess the degree of food phobias in this population as well as nutrition counseling approaches that address the emotional aspects of eating that may accompany a drastic change in diet.
During the initiation and titration phase, blood phenylalanine is monitored every 1–4 weeks [17]. Clinic approaches vary; monitoring too frequently can be discouraging if the time to respond to the drug is long, yet it is important to monitor blood frequently enough to capture a reduction in blood phenylalanine. Blood tyrosine is monitored with the same frequency and L-tyrosine is supplemented if postprandial blood phenylalanine is consistently low [17].
7.2 Nutrition Management During Diet Normalization
The goal of pegvaliase therapy is to allow a patient to maintain blood phenylalanine in the treatment range while consuming a normal diet [17]. A normal diet is considered to be one that meets or exceeds the DRI for protein [28] and does not contain medical food. For patients who have been restricting protein and/or are consuming a medical food, once the blood phenylalanine reaches the target range, intact protein is added to the diet and protein from medical food is decreased. Current guidance is to add intact protein once blood phenylalanine is 120 μmol/L or below [17]; however, some clinics counsel their patients to add intact protein to their diets when blood phenylalanine is under 240–360 μmol/L, especially if the drop in blood phenylalanine is abrupt, in order to prevent low blood phenylalanine.
Protein is added in increments of 10–20 g with monitoring of blood phenylalanine and subsequent increases in protein if blood phenylalanine remains in the treatment range or below [17]. Nutrition counseling about diet adjustments is highly individualized and depends on the patient’s blood phenylalanine concentration, clinic policy and patient preferences. Some dietitians counsel patients to add intact protein in larger increments (i.e., 40 g) if blood phenylalanine has dropped quickly, and for others, a slower approach is taken, especially if the patient’s blood phenylalanine does not fall below the physiologically normal blood phenylalanine concentration of 30 µmol/L [32].
Adding intact protein to the diet is challenging for some patients who have no or limited experience with eating high protein foods. Extensive nutrition counseling is crucial to help the patient transition to a new way of eating and includes individualized education about higher protein food options, counting protein to reach intake goals, food preparation and safety, grocery shopping and budgeting, and incorporating more protein in a healthy manner, to name a few. Also, some patients find it emotionally challenging to eat foods that were previously forbidden and may require more intensive counseling. Educational resources for teaching patients to increase protein in the diet are available at www.met-ed.net and www.gmdi.org.
For patients consuming medical food, an equal amount of protein from medical food is removed from the diet as intact protein is added [17]. For many with PKU, adherence to consuming the recommended amount of medical food has been a struggle during adulthood [33] and not having to consume it is a welcome change. But for others, medical food intake is associated with feeling full and well, and discontinuing it is not an easy transition. Moreover, medical food is a source of many nutrients other than protein equivalents, such as energy, tyrosine, vitamins and minerals, and a full assessment of nutrient intake is imperative as medical food is decreased. In addition, periodic monitoring of nutrition status is recommended (Chap. 10). Supplementation of vitamins and minerals may be necessary [17].
Supplementation of L-tyrosine is recommended if a patient’s postprandial blood tyrosine is consistently below 30 μmol/L. Blood tyrosine concentrations fluctuate diurnally, and a fasting blood tyrosine is more likely to be lower than a postprandial one [34]. During the pegvaliase clinical trials, supplementation with 1500 mg of L-tyrosine (500 mg tablets taken 3 times daily) was recommended [16]. Mean blood tyrosine remained normal throughout the study. It is expected that once a patient is consuming a high protein diet, tyrosine intake will be adequate. During commercial use of pegvaliase, one study indicated that 56 percent of patients had low fasting blood tyrosine, even after normalization of protein intake [31].
Hypophenylalaninemia, or low blood phenylalanine, defined as 2 or more blood phenylalanine concentrations below 30 μmol/L, was experienced by 35% of subjects in the Phase 3 pegvaliase clinical trials. Compared to the group of subjects who did not have low blood phenylalanine, subjects with low blood phenylalanine had a more rapid response to pegvaliase, experienced fewer adverse events, and discontinued the drug less frequently [35]. The only adverse event experienced more frequently in patients with low blood phenylalanine was alopecia [35]. However, alopecia occurred in both groups and patients with alopecia had new hair growth even when blood phenylalanine was low. The recommendation for patients whose blood phenylalanine falls below 30 μmol/L is first to normalize the diet with intact protein and then to lower the pegvaliase dose [17].
7.3 Nutrition Management After Diet Normalization
Nutrition counseling of a patient who is no longer on a restricted diet for PKU becomes less frequent and focuses on monitoring the patient’s intake and nutrition status. After a patient has normalized their diet, nutrition counseling is helpful, at least in the short term, to ensure that the patient’s protein intake continues to meet the DRI, weight status is appropriate and vitamin/mineral status is adequate. Guidance regarding healthful eating may be necessary; preliminary evidence shows that the diets of patients on pegvaliase do not meet healthy eating goals [31]. In the long term, the role of the metabolic dietitian for patients managed with pegvaliase remains to be seen.
References
Camp KM, Parisi MA, Acosta PB, Berry GT, Bilder DA, Blau N, et al. Phenylketonuria scientific review conference: state of the science and future research needs. Mol Genet Metab. 2014;112(2):87–122.
Bilder DA, Burton BK, Coon H, Leviton L, Ashworth J, Lundy BD, et al. Psychiatric symptoms in adults with phenylketonuria. Mol Genet Metab. 2013;108(3):155–60.
Viau KS, Wengreen HJ, Ernst SL, Cantor NL, Furtado LV, Longo N. Correlation of age-specific phenylalanine levels with intellectual outcome in patients with phenylketonuria. J Inherit Metab Dis. 2011;34(4):963–71.
Blau N, Longo N. Alternative therapies to address the unmet medical needs of patients with phenylketonuria. Expert Opin Pharmacother. 2015;16(6):791–800.
Blau N. Sapropterin dihydrochloride for the treatment of hyperphenylalaninemias. Expert Opin Drug Metab Toxicol. 2013;9(9):1207–18.
Harding CO, Amato RS, Stuy M, Longo N, Burton BK, Posner J, et al. Pegvaliase for the treatment of phenylketonuria: a pivotal, double-blind randomized discontinuation phase 3 clinical trial. Mol Genet Metab. 2018;124(1):20–6.
Burton BK, Longo N, Vockley J, Grange DK, Harding CO, Decker C, et al. Pegvaliase for the treatment of phenylketonuria: results of the phase 2 dose-finding studies with long-term follow-up. Mol Genet Metab. 2020;130(4):239–46.
Sarkissian CN, Gamez A. Phenylalanine ammonia lyase, enzyme substitution therapy for phenylketonuria, where are we now? Mol Genet Metab. 2005;86(Suppl 1):S22–6.
Hoskins JA, Holliday SB, Greenway AM. The metabolism of cinnamic acid by healthy and phenylketonuric adults: a kinetic study. Biomed Mass Spectrom. 1984;11(6):296–300.
Hoskins JA, Jack G, Wade HE, Peiris RJ, Wright EC, Starr DJ, et al. Enzymatic control of phenylalanine intake in phenylketonuria. Lancet. 1980;1(8165):392–4.
Sarkissian CN, Gamez A, Wang L, Charbonneau M, Fitzpatrick P, Lemontt JF, et al. Preclinical evaluation of multiple species of PEGylated recombinant phenylalanine ammonia lyase for the treatment of phenylketonuria. Proc Natl Acad Sci U S A. 2008;105(52):20894–9.
Sarkissian CN, Kang TS, Gamez A, Scriver CR, Stevens RC. Evaluation of orally administered PEGylated phenylalanine ammonia lyase in mice for the treatment of phenylketonuria. Mol Genet Metab. 2011;104(3):249–54.
Longo N, Harding CO, Burton BK, Grange DK, Vockley J, Wasserstein M, et al. Single-dose, subcutaneous recombinant phenylalanine ammonia lyase conjugated with polyethylene glycol in adult patients with phenylketonuria: an open-label, multicentre, phase 1 dose-escalation trial. Lancet. 2014;384(9937):37–44.
Zori R, Thomas JA, Shur N, Rizzo WB, Decker C, Rosen O, et al. Induction, titration, and maintenance dosing regimen in a phase 2 study of pegvaliase for control of blood phenylalanine in adults with phenylketonuria. Mol Genet Metab. 2018;125(3):217–27.
Longo N, Zori R, Wasserstein MP, Vockley J, Burton BK, Decker C, et al. Long-term safety and efficacy of pegvaliase for the treatment of phenylketonuria in adults: combined phase 2 outcomes through PAL-003 extension study. Orphanet J Rare Dis. 2018;13(1):108.
Thomas J, Levy H, Amato S, Vockley J, Zori R, Dimmock D, et al. Pegvaliase for the treatment of phenylketonuria: results of a long-term phase 3 clinical trial program (PRISM). Mol Genet Metab. 2018;124(1):27–38.
Longo N, Dimmock D, Levy H, Viau K, Bausell H, Bilder DA, et al. Evidence- and consensus-based recommendations for the use of pegvaliase in adults with phenylketonuria. Genet Med. 2019;21(8):1851–67.
Hausmann O, Daha M, Longo N, Knol E, Muller I, Northrup H, et al. Pegvaliase: immunological profile and recommendations for the clinical management of hypersensitivity reactions in patients with phenylketonuria treated with this enzyme substitution therapy. Mol Genet Metab. 2019;128(1–2):84–91.
Gupta S, Lau K, Harding CO, Shepherd G, Boyer R, Atkinson JP, et al. Association of immune response with efficacy and safety outcomes in adults with phenylketonuria administered pegvaliase in phase 3 clinical trials. EBioMedicine. 2018;37:366–73.
Larimore K, Nguyen T, Badillo B, Lau K, Zori R, Shepherd G, et al. Depletion of interfering IgG and IgM is critical to determine the role of IgE in pegvaliase-associated hypersensitivity. J Immunol Methods. 2019;468:20–8.
FDA. PALYNZIQ (pegvaliase-pqpz) injection, for subcutaneous use. Initial U.S. Approval 2018. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761079s000lbl.pdf.
Lenke RR, Levy HL. Maternal phenylketonuria and hyperphenylalaninemia. An international survey of the outcome of untreated and treated pregnancies. N Engl J Med. 1980;303(21):1202–8.
Boyer M, Skaar J, Sowa M, Tureson JR, Chapel-Crespo CC, Chang R. Continuation of pegvaliase treatment during pregnancy: a case report. Mol Genet Metab Rep. 2021;26:100713.
Pegvaliase [Internet]. Drugs and lactation database.
Rohr F, Burton BK, Longo N, Thomas J, Harding C, Rosen O, et al. Evaluating change in diet with Pegvaliase treatment in adults with phenylketonuria: results from phase 2 and 3 clinical trials. American College of Medical Genetics and Genomics Annual Meeting 2020.
Rocha JC, Bausell H, Belanger-Quintana A, Bernstein LB, Gokmen-Ozel H, Jung A, et al. Practical dietitian road map for the nutritional management of phenylketonuria (PKU) patients on pegvaliase treatment. Mol Genet Metab Rep. 2021;28:100771. https://doi.org/10.1016/j.ymgmr.2021.100771. PMID: 34094869; PMCID: PMC8167196.
Sacharow S, Papaleo C, Almeida K, Goodlett B, Kritzer A, Levy H, et al. First 1.5 years of pegvaliase clinic: experiences and outcomes. Mol Genet Metab Rep. 2020;24:100603.
Institute of Medicine (U.S.). Panel on Macronutrients., Institute of Medicine (U.S.). Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, D.C.: National Academies Press; 2005. xxv, 1331 p. p.
Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:e2014009.
Damsbo-Svendsen M, Frost MB, Olsen A. A review of instruments developed to measure food neophobia. Appetite. 2017;113:358–67.
Viau K, Wessel A, Martell L, Sacharow S, Rohr F. Nutrition status of adults with phenylketonuria treated with pegvaliase. Mol Genet Metab. 2021;133(4):345–51.
Bernstein LB, Rohr F. Palynziq in practice: one year after FDA approval (Survey) 2019.
Jurecki ER, Cederbaum S, Kopesky J, Perry K, Rohr F, Sanchez-Valle A, et al. Adherence to clinic recommendations among patients with phenylketonuria in the United States. Mol Genet Metab. 2017;120(3):190–7.
van Spronsen FJ, van Rijn M, Bekhof J, Koch R, Smit PG. Phenylketonuria: tyrosine supplementation in phenylalanine-restricted diets. Am J Clin Nutr. 2001;73(2):153–7.
Thomas J, Jurecki E, Lane P, Olbertz J, Wang B, Longo N, et al. Dietary intakes and adverse events in pegvaliase-treated phenylketonuria adults who had low blood phenylalanine levels. American College of Medical Genetics and Genomics Annual Meeting. 2020.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Longo, N., Andrews, A., Rohr, F. (2022). Medical and Nutrition Management of Phenylketonuria: Pegvaliase. In: Bernstein, L.E., Rohr, F., van Calcar, S. (eds) Nutrition Management of Inherited Metabolic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-94510-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-94510-7_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94509-1
Online ISBN: 978-3-030-94510-7
eBook Packages: MedicineMedicine (R0)