Abstract
Dissecting folliculitis of the scalp (or dissecting cellulitis or perifolliculitis capitis abscedens et suffodiens of Hoffman) is a rare inflammatory scalp condition (Otberg and Shapiro, Fitzpatrick’s dermatology. New York: McGraw-Hill, 2019; Branisteanu et al., Rom J Morphol Embryol 50(4):719–724, 2009). This disease belong to follicular occlusion triad (Oakley and Marrison, Follicular occlusion syndrome. DermNet New Zealand Trust (online serial), 2014). Here we present a 17-year-old male patient with a dissecting folliculitis. He also was obese and has a habit of smoking every day.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
A 17-year-old Indonesian male was referred to the Department of Dermatology and Venereology with painful nodules with coexisted scarring alopecia on the scalp. The lesions started on the vertex and spread to the occipitial area. The patient suffered from acne conglobata and obesity. He was a smoker.
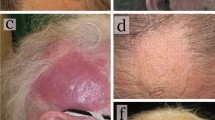
On physical examination painful, multiple, fluctuating, confluent nodules on the vertex and occipital scalp with coexisted scarring alopecia were observed (Fig. 46.1). Bacterial culture showed that Staphylococcus epidermidis. In histopathological examination, an extensive inflammatory reaction at the subcutaneous plane, causing disruption of subcutaneous adipose tissue, as well as at the perifollicular area in the upper dermis and around the sebaceous glands was observed (Fig. 46.2).
Histology shows an extensive inflammatory reaction at the subcutaneous plane (C), causing disruption of subcutaneous adipose tissue, as well as at the perifollicular area in the upper dermis (B) and around the sebaceous glands: (a) Inflammatory infiltrate consists mainly of lymphocytes (arrow) mixed with neutrophils and some plasma cells; inflammatory cells infiltrate the follicular epithelium (F) and are around sebaceous gland (S): (b) Granulomas containing histiocytes as well as giant cells (arrow head) (c) Box B and C in (a) indicates area of (b) and (c), respectively. Haematoxylin-eosin, bars (a) 500 μm, (b and c) 100 μm
Based on the case description, clinical picture, histopathological examination and bacterial culture the presented patient was diagnosed with dissecting cellulitis. He was initially treated with intralesional triamcinolone acetonide injections 10 mg/mL every four weeks and oral ciprofloxacin at 500 mg twice a day. After three months of treatment, clinical examination revealed a good clinical improvement, with hair regrowth (Fig. 46.3). Treatment was well tolerated, and no adverse effects were noted on the follow-up visits.
-
1.
Dissecting folliculitis.
-
2.
Folliculitis decalvans.
-
3.
Keloid.
-
4.
Cylindroma.
Dissecting cellulitis.
Discussion
Dissecting cellulitis is a rare, chronic, suppurative disease which predominantly occurs in black young men with the age range between 10 and 17 years. The disease belongs to the follicular occlusion triad. Follicular occlusion, androgens, seborrhea, secondary bacterial infections and abnormal host response to bacterial antigens seem to play an important role in pathogenesis of dissecting cellulitis. Moreover, the role of environmental factors including smoking, obesity, high carbohydrate diet, and humidity is also suggested [1,2,3,4].
Dissecting cellulitis is mostly found on the vertex and occipital areas. It is characterized by painful fluctuating and suppurative nodules, abscesses and sinuses with purulent discharge. Chronic and relapsing courses result in cicatricial alopecia [1,2,3,4,5,6].
Characteristic histopathological features of early stages of dissecting cellulitis include an intra- and perifollicular neutrophilic infiltrate with follicular occlusion along with lymphocytes, plasmocytes, eosinophils and giant cells [1, 6]. At more advanced stages the typical findings are sinus tracts lined by squamous epithelium, follicular perforation and perifollicular and deep dermal abscesses [1].
There is no consensus regarding the optimal management of dissecting cellulitis [6]. Chaw-Ning et al. proposed the therapeutic algorithm based on severity and activity of the disease (Fig. 46.4) [7].
The therapeutic algorithm for dissecting cellulitis according to Chaw-Ning et al. [7]. DC dissecting cellulitis
The first-line therapy includes topical and systemic antibiotics (such as erythromycin, tetracyclines, clindamycin, minocycline, cloxacillin, cephalosporin with or without rifampicin), intralesional corticosteroids, and oral prednisolone. In moderate to severe refractory disease, isotretinoin at a dose of 0.5–1 mg/kg/day, may be considered [1, 8,9,10,11]. Biologic agents, photodynamic or laser therapy are considered as the second-line therapeutic options in patients with moderate to severe refractory disease [10]. A X-ray epilation and surgical excision should be considered in patients with very severe disease [10].
Key Points
-
Dissecting folliculitis belongs to the follicular occlusion triad.
-
The role of environmental factors such as smoking, obesity, high carbohydrate diet, humidity in pathogenesis of dissecting cellulitis is suggested.
-
Dissecting cellulitis is mostly found on the vertex and occipital scalp and it is characterized by painful, fluctuating and suppurative nodules, abscesses and sinuses with purulent discharge.
References
Otberg N, Shapiro J. Fitzpatrick’s dermatology, vol. 2. 9th ed. New York: McGraw-Hill; 2019. p. 524–1536.
Branisteanu DE, Molodoi A, Ciobanu D, Badescu A, Stoica LE, Tolea I. The importance of histopathologic aspects in the diagnosis of dissecting cellulitis of the scalp. Rom J Morphol Embryol. 2009;50(4):719–24.
Oakley A, Marrison C. Follicular occlusion syndrome. DermNet New Zealand Trust (online serial). April 2014. Available from https://dermnetnz.org/topics/follicular-occlusion-syndrome
Diaz-Perez LM, Ramirez KE, Sanchez-Duenas LE. A new familial presentation of dissecting cellulitis: the genetic implications on scarring alopecias. JAAD Case Rep. 2020;6:705–7.
Plewig G. Hidradenitis Suppurativa/Acne Inversa/Dissecting Terminal Hair Folliculitis. Plewig and Kligman’s Acne and Rosacea. Cham: Springer Mature Switzerland AG; 2019. p. 1–46.
Elder DE, Elenitsas R, Johnson BL, Murphy GF. Lever’s histopathology of the skin. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 493–7.
Chaw-Ning L, Chen W, Chao-Kai H, Tzu-Teng W, Yu-Yun LJ, Chao-Chun Y. Dissecting folliculitis (dissecting cellulitis) of The scalp: a 66-patient case series and proposal of classification. J Dtsch Dermatol Ges. 2018;16:1–8.
Hintze JM, Howard BE, Donald C, Hayden RE. Surgical management and reconstruction of Hoffman’s disease (dissecting cellulitis of the scalp). Hindawi Publishing Corporation; 2016. p. 1–4.
Navarro-Trivino FJ, Almazan-Fernandez FM. Rodenas-Herranz T, Ruiz-Villaverde R. Dissecting cellulitis of the scalp successfully treated with topical resorcinol 15%. Wiley Online Library; 2020. p. 1–6.
Thomas J, Aguh C. Approach to treatment of refractory dissecting cellulitis of the scalp-systematic review. J Dermatolog Treat. 2019:1471–753.
Guo W, Zhu C, Stevens G, Silverstein D. Analyzing the efficacy of isotretinoin treating dissecting cellulitis: a literature review and meta-analysis. Drug R D. 2021;21(1):1–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Anum, Q., Tofrizal, Julia, D.S., Birawati, S. (2022). Dissecting Folliculitis of the Scalp. In: Waśkiel-Burnat, A., Sadoughifar, R., Lotti, T.M., Rudnicka, L. (eds) Clinical Cases in Scalp Disorders. Clinical Cases in Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-030-93426-2_46
Download citation
DOI: https://doi.org/10.1007/978-3-030-93426-2_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-93425-5
Online ISBN: 978-3-030-93426-2
eBook Packages: MedicineMedicine (R0)